- 1Department of Plastic and Reconstructive Surgery, Chungnam National University Hospital, Daejeon, Republic of Korea
- 2Department of Plastic and Reconstructive Surgery, College of Medicine, Chungnam National University, Daejoen, Republic of Korea
- 3Department of Plastic and Reconstructive Surgery, Chungnam National University Sejong Hospital, Sejong, Republic of Korea
The free flap is a versatile option for reconstruction of soft tissue defects around the ankle. In patients with poor lower leg circulation, arterial insufficiency is one of the complications that can occur immediately after vessel anastomosis during free flap surgery. The authors were able to improve blood circulation in the flap by using modified turbocharging method in which another perforator was anastomosed to the distal end of the main pedicle.
Purpose
Soft tissue defects around the ankle are a challenge for reconstructive surgery. If the defect size is small in the lower one-third of the lower limb or around the ankle, local flaps such as a reverse sural flap or a propeller flap can be tried. However, if the defect is large, it is often necessary to perform a free flap (1). The arterial insufficiency is often encountered after anastomosis of the perforator and pedicle, especially in the case of poor blood circulation in the lower legs (2). The authors performed an anterolateral thigh (ALT) free flap to reconstruct a defect around the ankle in a patient with poor blood circulation in the lower limb. After vessel anastomosis, arterial blood flow was not achieved with the flap, and arterial insufficiency could be improved by performing anastomosis with the distal end of the pedicle on the remaining perforator.
Case review
A 72-year-old male patient visited the hospital with the right tibiofibular fracture. One day after visiting the hospital, the orthopedic department applied closed reduction and external fixation, and one week later, open reduction and internal fixation was performed. Skin necrosis occurred in the ankle area, and after the implementation of the debridement, soft tissue defect occurred and was referred to a plastic surgery clinic (Figure 1).
ALT free flap was planned and computed tomography angiography was performed. In the reading, there was diffuse atherosclerosis, both distal superficial femoral arteries, and the blood supply below the ankle was not smooth. After peripheral angiogram and balloon angioplasty, occlusion of the anterior tibial artery (ATA) was recanalized.
After 5 days, ALT free flap was performed. It was decided to include two perforators of Flap and dissection was performed (Figure 2). The distal perforator was more reliable and descending branch of lateral circumflex femoral artery (DB-LCFA) was dissected, but the preserving proximal perforator was not connected to the DB-LCFA (Figure 2). The ATA of the recipient site and the proximal of DB-LCFA were anastomosed, but blood supply to the flap was not smooth. Salvage methods were tried to improve blood flow, but circulation in the flap was not observed. At this time, the author connected the remaining proximal perforator to the distal end of the DB-LCFA to secure additional blood supply. The blood supply improved, and the surgical site recovered without any complications (Figure 3).

Figure 2. Intra operative photo. Two perforators and DB-LCFA are observed. * distal perforator; † proximal perforator; ‡ DB-LCFA. DB-LCFA descending branch of lateral circumflex femoral artery.
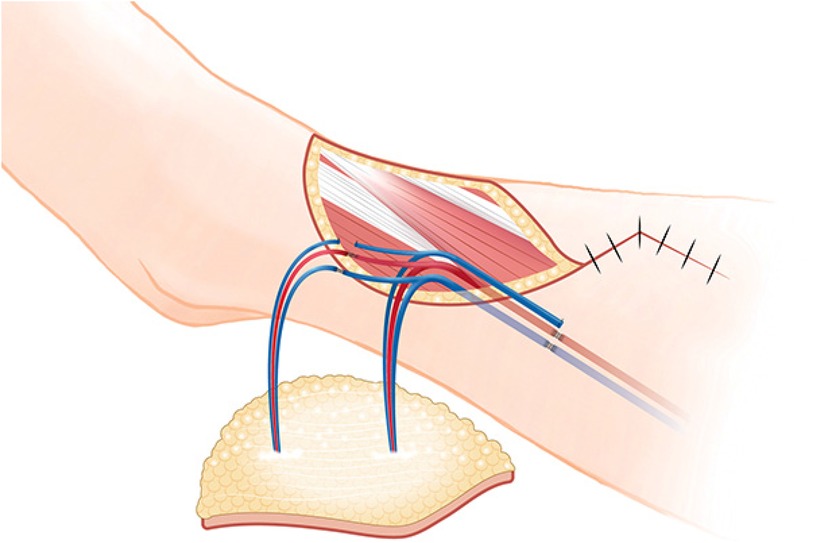
Figure 3. Schematic diagram of surgery. After pedicle anastomosis, the proximal perforator was anastomized with the distal end of DB-LCFA. DB-LCFA descending branch of lateral circumflex femoral artery.
Discussion
Vascular compromise occurs because of hematoma, thrombosis, vessel spasm, vascular kinking, and technical errors (2, 3). If blood flow is not confirmed immediately after vessel anastomosis, arterial anastomosis is reopened, followed by heparin flushing, warm saline irrigation, and reanastomosis (4). However, if there is no improvement and it is determined that the perforator was damaged during the flap harvesting process, it may be necessary to abandon the old flap and re-harvest a new flap. In this case, various salvage methods were used, but circulation did not improve, and an attempt was made to directly connect the sparing perforator to recipient vessel to improve blood flow, but it could not be performed due to the difference in vessel diameter between sparing perforator of flap and ATA. Surgeon tried to find the side branch of DB-LCFA and connect it with the sparing perforator (5), but could not find a suitable side branch. At this time, the author modified the turbocharging method and connected the remaining perforator to the distal end of the DB-LCFA.
Supercharging and turbocharging are surgical techniques for enhancing blood flow to the flaps. Supercharging connects one of the supply vessels of a flap to the vessels outside the flap. In contrast, turbocharging involves interconnection of supplying vessels of a flap. In the ALT free flap, the turbocharging method connects another perforator to the side branch of the DB-LCFA (5). However, in this case, since there was no suitable side branch to connect the perforator, it was decided to modify the traditional turbocharging method and connect the distal end of the DB-LCFA to another perforator (Figure 4). After modified turbocharging, the blood supply of the flap improved, and the patient was able to recover safely.
In this patient, blood supply was not smooth with a single perforator and the main pedicle did not have an adequate side branch, which was thought to be because the patient had long suffered from diabetic mellites, hypertension, and diffuse atherosclerosis.
Preoperative peripheral angiography revealed that the artery (ATA) at the trauma site was damaged. However, compared to the trauma area, the proximal vessel was not blocked even though it had stenosis, so it was thought that it could be sufficiently used as a recipient vessel for the free flap. It has been reported that 5%–25% of patients undergo early re-occlosuion after peripheral angiography (6). In the case of this patient, a cardiologist was also consulted to perform a free flap before early re-occlusion, and free flap surgery was performed 5 days after the procedure.
A perforator is commonly observed in the proximal position of the perforator commonly used in ATL free flap surgery, but if it is not necessary for surgery, it is sacrificed during dissection. In the case of this patient, a proximal perforator was sparing, expecting that the arterial circulation of the flap might not be good due to severe atherosclerosis. I was more concerned about stenosis and spasm of the harvest vessel (LCFA-DB) and skin perforator, so I prepared a second perforator. During flap dissection, the second perforator was not connected to the descending branch of LCFA. In retrospect, it is assumed that it was connected to another branch (possibly the transverse branch) of LCFA (7).
After the reconstruction surgery, the patient underwent plate and screw removal surgery at an orthopedic surgery center 6 months later and is undergoing rehabilitation treatment. Recently, a patient came back for the first time in almost two years, and there were no problems with the surgical site. The patient has been followed up for two years to date. There have been no signs of late necrosis.
Conclusion
If circulation is expected to be insufficient due to the large flap or atherosclerosis, using a modified turbocharging method by sparing the perforator is thought to be helpful for the success of the operation in ALT free flap.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Chungnam National University Hospital (2023-07-016). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YH: Writing – original draft. DK: Writing – review & editing, Data curation, Visualization. HKw: Supervision, Writing – review & editing. SK: Supervision, Writing – review & editing. SS: Supervision, Writing – review & editing. S-HO: Supervision, Writing – review & editing. J-hK: Supervision, Writing – review & editing. HY: Supervision, Writing – review & editing. HKy: Conceptualization, Investigation, Writing – original draft, Methodology.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by research fund of Chungnam National University Hospital and Chungnam National University.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. AlMugaren FM, Pak CJ, Suh HP, Hong JP. Best local flaps for lower extremity reconstruction. Plast Reconstr Surg Glob Open. (2020) 8(4):e2774. doi: 10.1097/GOX.0000000000002774
2. Chiu YH, Chang DH, Perng CK. Vascular complications and free flap salvage in head and neck reconstructive surgery: analysis of 150 cases of reexploration. Ann Plast Surg. (2017) 78(3 Suppl 2):S83–8. doi: 10.1097/SAP.0000000000001011
3. Stepanovs J, Ozoliņa A, Rovīte V, Mamaja B, Vanags I. Factors affecting the risk of free flap failure in microvascular surgery. Proc Latv Acad Sci B Nat Exact Appl Sci. (3917) 70(6):356–64. doi: 10.1515/prolas-2016-0039
4. Barhoum F, Tschaikowsky K, Koch M, Kapsreiter M, Sievert M, Müller S, et al. Successful free flap salvage surgery with off-label use of alteplase: a case report, review of the literature and our free flap salvage algorithm. Int J Surg Case Rep. (2020) 75:398–402. doi: 10.1016/j.ijscr.2020.09.035
5. Jeong SH, Koo DY, Moon KC, Dhong ES, Han SK. The turbocharged wide anterolateral thigh perforator flap to reconstruct massive soft tissue defects in traumatized lower extremities: a case series. Front Surg. (2022) 9:991094. doi: 10.3389/fsurg.2022.991094
6. Visona A, Tonello D, Zalunardo B, Irsara S, Liessi G, Marigo L, et al. Antithrombotic treatment before and after peripheral artery percutaneous angioplasty. Blood Transfus-Italy. (2009) 7(1):18–23.19290075
Keywords: turbocharging, anterolateral thigh, soft tissue defect reconstruction, perforator flap, salvage technique
Citation: Ha Y, Kim D, Kwon H, Kim S, Song SH, Oh S-H, Kim J-h, Yang HJ and Kyung H (2024) Anterolateral thigh free flap using modified turbocharging method: a case report. Front. Surg. 11:1273843. doi: 10.3389/fsurg.2024.1273843
Received: 7 August 2023; Accepted: 26 August 2024;
Published: 1 October 2024.
Edited by:
Benedetto Longo, University of Rome Tor Vergata, ItalyReviewed by:
Jose M. Lasso, Hospital General Universitario Gregorio Marañón, SpainDimitris Tatsis, Aristotle University of Thessaloniki, Greece
Seokchan Eun, Seoul National University Bundang Hospital, Republic of Korea
Copyright: © 2024 Ha, Kim, Kwon, Kim, Song, Oh, Kim, Yang and Kyung. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hyunwoo Kyung, aHdreXVuZ0BnbWFpbC5jb20=
 Yooseok Ha
Yooseok Ha Donghyun Kim1
Donghyun Kim1 Hyunwoo Kyung
Hyunwoo Kyung
