- Department of Plastic Surgery, Kaohsiung Chang Gung Memorial Hospital and Chang Gung University College of Medicine, Kaohsiung, Taiwan
Many studies on the recurrence of pressure ulcers after surgical reconstruction have focused on surgical techniques and socioeconomic factors. Herein, we aimed to identify the risk factors of the associated comorbidities for pressure ulcer recurrence. We enrolled 147 patients who underwent pressure ulcer reconstruction and were followed up for more than three years. The recurrence of pressure ulcers was defined as recurrent pressure ulcers with stage 3/4 pressure ulcers. We reviewed and analyzed systematic records of medical histories, including sex, age, associated comorbidities such as spinal cord injury (SCI), diabetes mellitus (DM), coronary artery disease, cerebral vascular accident, end-stage renal disease, scoliosis, dementia, Parkinson's disease, psychosis, autoimmune diseases, hip surgery, and locations of the primary pressure ulcer. Patients with recurrent pressure ulcers were younger than those without. Patients with SCI and scoliosis had higher odds, while those with Parkinson's disease had lower odds of recurrence of pressure ulcers than those without these comorbidities. Moreover, the decision tree algorithm identified that SCI, DM, and age < 34 years could be risk factor classifiers for predicting recurrent pressure ulcers. This study demonstrated that age and SCI are the two most important risk factors associated with recurrent pressure ulcers following surgical reconstruction.
Introduction
The management of pressure ulcers is a significant challenge for healthcare professionals. Despite advances in information and technological progress for prevention, the recurrence of pressure ulcers is not rare (1–7). Many of these recurrent ulcers require prolonged time in wound care and even surgery management, both of which often result in costly procedures, lengthy hospitalizations, expensive dressing changes, and worsened quality of life for these people (8–13). To achieve successful surgical reconstruction, thorough preoperative wound care, patient compliance, control of comorbidities, professional postoperative support, and sufficient pressure relief are essential (14). Krause and Broderick suggested that lifestyle, exercise, and diet are protective mechanisms against the recurrence of pressure ulcers (15). Furthermore, lack of social support, inadequate pressure sore prevention knowledge (2, 5, 16, 17), unemployment, and residing in a nursing home (2, 12) have been considered important issues related to recurrence. Regarding demographic and medical factors, it has been reported that male sex, younger age, and a history of previous pressure sore surgery are associated with the recurrence of pressure ulcers (2, 12). However, as many studies describing recurrence after reconstruction have focused on socioeconomic factors (2, 17, 18), education (18), marital status (19), and surgical techniques (20–26), available data on factors associated with recurrence following surgical repair of pressure ulcers are rather limited.
In this study, we aimed to identify the risk factors associated with comorbidities of pressure ulcer recurrence following surgical reconstruction. In addition, we adopted the decision tree method, which is a machine learning model composed of decision rules based on optimal feature cutoff values that split independent variables into different groups in a hierarchical manner to predict an outcome (27–29), to explore the variables that could be used to identify individuals at risk of pressure ulcer recurrence following surgical reconstruction.
Materials and methods
This study was approved by the Institutional Review Board (IRB) of Chang Gung Memorial Hospital (approval number 201701802B0). The need for informed consent was waived according to IRB regulations because the study was designed for a retrospective analysis of the registered database. In this study, 147 bed-ridden patients who underwent reconstruction for pressure ulcers from 2007 to 2014 were enrolled and followed up for more than three years. The recurrence of pressure ulcers was defined as recurrent pressure ulcers with stage 3, full-thickness ulcer that might involve the subcutaneous fat, or stage 4, full-thickness ulcer with the involvement of the muscle or bone. The systematic records of medical histories, including sex, age, associated comorbidities such as spinal cord injury (SCI), diabetes mellitus (DM), coronary artery disease (CAD), cerebral vascular accident (CVA), end-stage renal disease (ESRD), scoliosis, dementia, Parkinson's disease, psychosis, autoimmune diseases, hip surgery, and locations of the primary pressure ulcer were reviewed. In this study, primary sacral pressure ulcers were treated with perforator flaps or rotation gluteal flaps, ischial pressure ulcers with muscle flaps (gluteal muscle or biceps femoris muscle) and skin flaps (rotation gluteal flap or posterior thigh flap), and trochanteric pressure ulcers with a gluteal rotation flap or pedicled anterolateral thigh flap.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics for Windows, version 20.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics were obtained by calculating the mean and standard deviation for continuous variables and the relative frequencies for categorical variables. These groups were compared using the chi-squared test for categorical variables with odds ratios (OR) and 95% confidence intervals (CIs). Student's t-test was used for the analysis of continuous variables. Statistical significance was set at p value < 0.05.
Decision tree classifier
The decision tree classification model was established by classification and regression tree (CART) analysis (30, 31) using the rpart function in the rpart package in R based on the Gini impurity index. CART analysis was used to search for the split on each variable to partition the data into two groups: one group of mostly “1s” (people who had sustained recurrent pressure ulcers) and another group of mostly “0s” (people who did not have recurrent pressure ulcers). The CART model identified the best overall split by iteratively testing all possible splits and creating a specified number of nodes until a further reduction in node impurity became impossible or the specified stopping criteria were reached (32–34). In this study, the complexity parameter (α) of the “cost-complexity” pruning method is set to 0.001. The complexity parameter (α) indicated a measure of how much additional accuracy a split must add to the entire tree to warrant additional complexity. A confusion matrix was used to determine the performance of the decision tree model for the presence of recurrent pressure ulcers. Accuracy, sensitivity, specificity, and area under the curve (AUC) of the receiver operating characteristic (ROC) curve were measured.
Results
Of the enrolled 147 patients, 46 had recurrent pressure ulcers. As shown in Table 1, among these patients, SCI was the most common associated comorbidity (n = 31, 67.4%), followed by DM (n = 21, 45.7%), CVA (n = 8, 17.4%), and scoliosis (n = 8, 17.4%). Among the patients without recurrence, DM was the most common associated comorbidity (n = 39, 38.9%), followed by CVA (n = 30, 30.0%), SCI (n = 24, 23.8%), and Parkinson's disease (n = 16, 15.8%). Patients with recurrent pressure ulcers were significantly younger than those without recurrence (55.7 ± 17.4 vs. 62.8 ± 17.4, respectively, p = 0.023). Patients who had SCI and scoliosis had significantly higher odds of recurrence of pressure ulcers than those without (SCI, OR = 6.63, 95% CI = 3.08–14.29; scoliosis, OR = 10.42, 95% CI = 2.12–51.31). In contrast, those patients who had Parkinson's disease had significantly lower odds of recurrence of pressure ulcers than those without (OR = 0.12, 95% CI = 0.02–0.92). There were no significant differences in sex, location of ulcer, and associated comorbidities, such as DM, CAD, CVA, ESRD, hip surgery, dementia, psychosis, and autoimmune diseases.
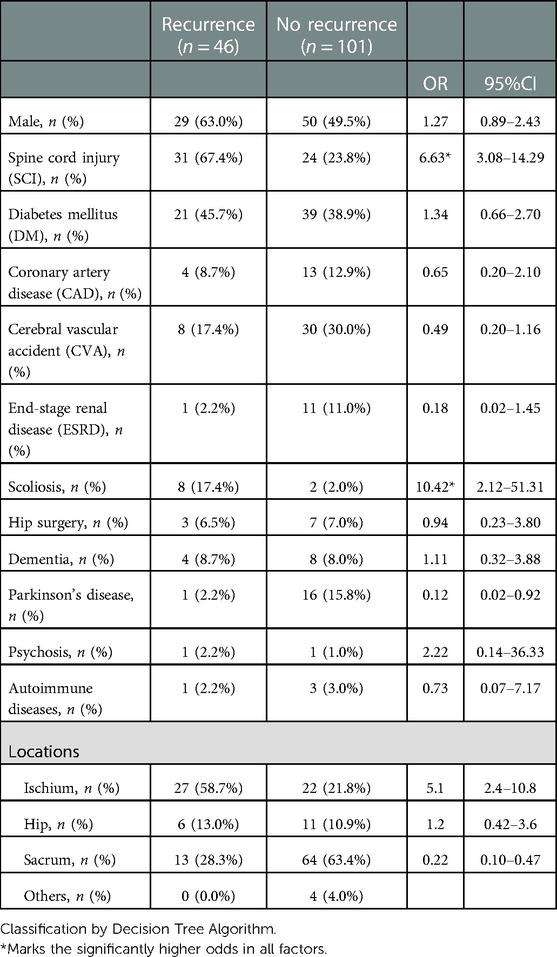
Table 1. Characteristics of patients with and without recurrence of pressure ulcer following reconstruction.
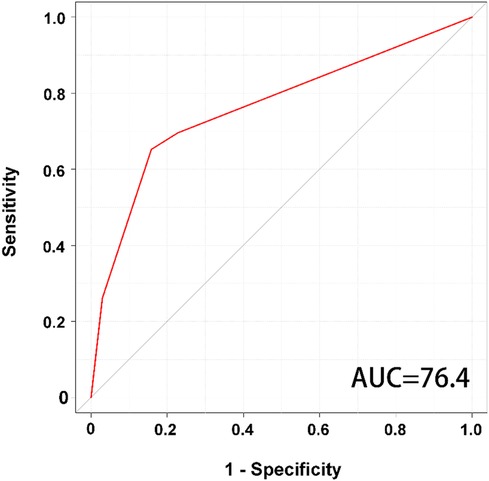
According to the classification by the decision tree algorithm, three groups of patient characteristics (SCI, DM, age < 34 years) with a high risk of recurrent pressure ulcers were identified (Figure 1). The presence or absence of SCI in the DT model was identified as a variable for the initial split. Among patients with SCI, 69% had recurrent pressure ulcers and 31% did not. Among patients with SCI, the presence or absence of DM was identified as a variable in the second split. For this node, 80% of patients with DM had recurrent pressure ulcers. An age of less than 34 years served as the third split for patients without DM. For this node, 58% of patients aged < 34 years had recurrent pressure ulcers. With all variables in the model, the decision tree algorithm achieved an accuracy of 78.23% (sensitivity of 65.22% and specificity of 84.16%). The decision tree model had an AUC of 0.764 for predicting the recurrence of pressure ulcers (Figure 2).
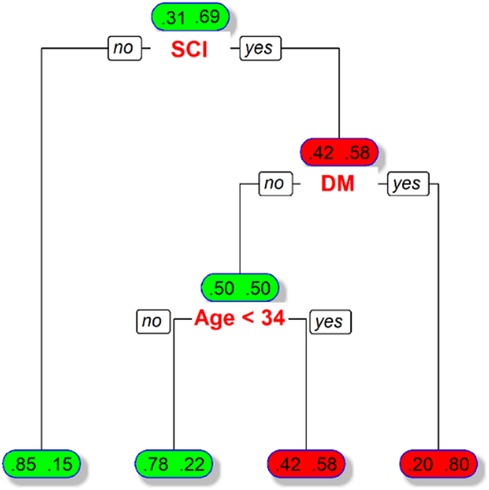
Figure 1. Illustration of decision tree model for predicting recurrence of pressure ulcers in the patients receiving reconstruction for pressure ulcer. Boxes denote the percentage of patients with discriminating variables from CART analysis. Patients with and without recurrence of pressure ulcers are indicated by the fractional number inside the right and left sides of the boxes, respectively.
Discussion
Authors should discuss the results and their interpretations from the perspective of previous studies and working hypotheses. The findings and their implications should be discussed in the broadest context possible. Future research directions may also be highlighted. This study demonstrated that patients with recurrent pressure ulcers were significantly younger and had a higher rate of sustaining SCI and scoliosis but a lower rate of Parkinson's disease than patients without recurrence. In addition, the decision tree algorithm identified that SCI, DM, and age < 34 years could be used as risk factor classifiers for predicting recurrent pressure ulcers.
This study recognized SCI as a risk factor, either from conventional comparisons or decision tree algorithms. Patients with SCI had a 6.6 times higher risk of pressure ulcer recurrence following surgical reconstruction. SCI has been recognized as a major risk factor for the recurrence of pressure ulcers (35, 36), and the recurrence rate can even be as high as 48 to 56% among these patients (5, 37). Furthermore, although older age might be responsible for delayed wound healing and was suggested to be a risk factor for the occurrence of pressure ulcers, this study recognized that younger age is a risk factor for the recurrence of pressure ulcers following surgical reconstruction. This is in accordance with the observation from some studies that younger age is associated with the recurrence of pressure ulcers (2, 12). One possible explanation is that pressure ulcer patients with SCI were generally much younger than those with other illnesses. Therefore, specific awareness is recommended for young and neurologically disabled patients following surgical treatment of pressure ulcers (5).
DM has been widely recognized as a risk factor for the development of pressure ulcers (38–40). However, in this study, there was no significant difference in the incidence of DM between the patients with and without pressure ulcer recurrence. We believe that the reason is that in the condition of multiple factors contributing to pressure ulcer recurrence, there were potential confounding factors in the analysis. Although individually weighted risk factors based on adequate statistical methods would be useful to assess the role of each risk factor in the development of pressure ulcers (41), this study is limited by its relatively small sample size for doing such work. In contrast, DM has been recognized by decision tree algorithms as a risk factor for the recurrence of pressure ulcers following surgical reconstruction. Machine learning methods may recognize a specific pattern to provide a useful classifier to make predictions for unseen data/objects (42, 43).
This study also demonstrated that patients with recurrent pressure ulcers were significantly younger and had a higher rate of sustaining scoliosis, but a lower rate of Parkinson's disease, than patients without recurrence. It had been reported that pelvic obliquity occurs secondary to scoliosis and results in increased instability of the hip on the high side and ischial decubitus ulcers on the low side (44). In a study of 166 patients who underwent 252 flap procedures, in addition to young age and oblique pelvis, scoliosis was recognized as a factor related to recurrence (45). The observed lower rate of Parkinson's disease in this study seemed to contradict the concept that the prevalence of pressure ulcers was markedly increased when Parkinson's coexisted (46) because the incidence of pressure ulcers is suggested to be inversely related to the amount of movement made during the night. Another large cohort study on more than 87,000 persons with pressure ulcers also revealed that Parkinson's disease was associated with the highest prevalence of pressure ulcers, although this study group did not include those patients following surgical reconstruction. In this study, the decision tree algorithm did not include scoliosis and Parkinson's disease as risk factor classifiers, which may be because of the sacrifice of pruning these relatively small numbers of patients in constructing a decision tree composed of a three-layer structure. Indeed, the reconstruction of more layers in the decision tree model may only increase the fair predictive power in this study (AUC of 0.764), and a decision tree model with too many layers or splits would make the model complex and difficult to use in the clinical setting.
The study was limited to a relatively small sample population to explore a disease influenced by multiple complex factors. Additional limitations of this study should be addressed. The first is selection bias associated with the retrospective study design. Second, socioeconomic factors and other potential factors such as nutritional status, being under- or overweight, anemia, vitamin deficiency, and arterial obstructive diseases were not analyzed or controlled in this study; therefore, some bias may exist. Third, the wound management, rehabilitation process, and activity may differ widely among these patients, which may have led to some bias in the analysis. Fourth, the recurrence of pressure ulcers was limited to those pressure ulcers with stage 3 or 4, because in such circumstances, a surgeon may need to determine whether to perform further reconstruction or allow the wound to heal secondarily. However, if the definition of pressure ulcer includes those with stage 1 and 2 pressure ulcers, the results may be different. Furthermore, the duration of each previous ulcer, the infectious status and pathology of the involved skin region, extension of previous ulcers, the type of spinal cord injury, and the bedridden time of the patients were unknown in this study, resulting in some potential bias in the comparison of the outcome. Whether the study results of bed-ridden patients in this study could be generalized to those who had different ambulatory status require further investigation. In addition, a longer follow-up time of more than three years, as performed in this study, may also impact the analysis of the results. Finally, the study was limited to a single center with a relatively small number of studied patient population, and patient injury characteristics may vary from those observed at other institutions, thereby limiting the generalizability of the findings.
Conclusions
This study demonstrated that age and SCI were the two most important risk factors associated with recurrent pressure ulcers following surgical reconstruction.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Institutional Review Board (IRB) of Chang Gung Memorial Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
Conceptualization, P-YL. and C-HH; methodology, Y-HY; validation, C-CW; investigation, CC; resources, NFM; writing—original draft preparation, Y-JT; writing—review and editing, C-HL; supervision, P-YL. and C-HH. All authors contributed to the article and approved the submitted version.
Funding
This research was funded by Chang Gung Memorial Hospital, grant number CORPG8L0631.
Acknowledgments
We appreciate the help with the statistical analysis extended by the Biostatistics Center, Kaohsiung Chang Gung Memorial Hospital.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bennett L, Kavner D, Lee BY, Trainor FS, Lewis JM. Skin stress and blood flow in sitting paraplegic patients. Arch Phys Med Rehabil. (1984) 65:186–90.6712437
2. Disa JJ, Carlton JM, Goldberg NH. Efficacy of operative cure in pressure sore patients. Plast Reconstr Surg. (1992) 89:272–8. doi: 10.1097/00006534-199202000-00012
3. Hentz VR. Management of pressure sores in a specialty center. A reappraisal. Plast Reconstr Surg. (1979) 64:683–91. doi: 10.1097/00006534-197964050-00014
4. Mandrekas AD, Mastorakos DP. The management of decubitus ulcers by musculocutaneous flaps: a five-year experience. Ann Plast Surg. (1992) 28:167–74. doi: 10.1097/00000637-199202000-00007
5. Relander M, Palmer B. Recurrence of surgically treated pressure sores. Scand J Plast Reconstr Surg Hand Surg. (1988) 22:89–92. doi: 10.3109/02844318809097940
6. Wyllie FJ, McLean NR, McGregor JC. The problem of pressure sores in a regional plastic surgery unit. J R Coll Surg Edinb. (1984) 29:38–43.6707991
7. Bennett G, Dealey C, Posnett J. The cost of pressure ulcers in the UK. Age Ageing. (2004) 33:230–5. doi: 10.1093/ageing/afh086
8. Buntine JA, Johnstone BR. The contributions of plastic surgery to care of the spinal cord injured patient. Paraplegia. (1988) 26:87–93. doi: 10.1038/sc.1988.17
9. Charlifue S, Lammertse DP, Adkins RH. Aging with spinal cord injury: changes in selected health indices and life satisfaction. Arch Phys Med Rehabil. (2004) 85:1848–53. doi: 10.1016/j.apmr.2004.03.017
10. Fuhrer MJ, Garber SL, Rintala DH, Clearman R, Hart KA. Pressure ulcers in community-resident persons with spinal cord injury: prevalence and risk factors. Arch Phys Med Rehabil. (1993) 74:1172–7. doi: 10.1016/S0003-9993(23)00010-2
11. Langemo DK, Melland H, Hanson D, Olson B, Hunter S. The lived experience of having a pressure ulcer: a qualitative analysis. Adv Skin Wound Care. (2000) 13:225–35.11075022
12. Sprigle S, Chung KC, Brubaker CE. Reduction of sitting pressures with custom contoured cushions. J Rehabil Res Dev. (1990) 27:135–40. doi: 10.1682/jrrd.1990.04.0135
13. Yarkony GM. Pressure ulcers: a review. Arch Phys Med Rehabil. (1994) 75:908–17. doi: 10.1016/0003-9993(94)90117-1
14. Sørensen JL, Jørgensen B, Gottrup F. Surgical treatment of pressure ulcers. Am J Surg. (2004) 188:42–51. doi: 10.1016/s0002-9610(03)00290-3
15. Krause JS, Broderick L. Patterns of recurrent pressure ulcers after spinal cord injury: identification of risk and protective factors 5 or more years after onset. Arch Phys Med Rehabil. (2004) 85:1257–64. doi: 10.1016/j.apmr.2003.08.108
16. Baek SM, Williams GD, McElhinney AJ, Simon BE. The gluteus maximus myocutaneous flap in the management of pressure sores. Ann Plast Surg. (1980) 5:471–6. doi: 10.1097/00000637-198012000-00010
17. Rubayi S, Pompan D, Garland D. Proximal femoral resection and myocutaneous flap for treatment of pressure ulcers in spinal injury patients. Ann Plast Surg. (1991) 27:132–8. doi: 10.1097/00000637-199108000-00007
18. Saunders LL, Krause JS, Peters BA, Reed KS. The relationship of pressure ulcers, race, and socioeconomic conditions after spinal cord injury. J Spinal Cord Med. (2010) 33:387–95. doi: 10.1080/10790268.2010.11689717
19. Taghipoor KD, Arejan RH, Rasouli MR, Saadat S, Moghadam M, Vaccaro AR, et al. Factors associated with pressure ulcers in patients with complete or sensory-only preserved spinal cord injury: is there any difference between traumatic and nontraumatic causes? J Neurosurg Spine. (2009) 11:438–44. doi: 10.3171/2009.5.Spine08896
20. Allman RM, Laprade CA, Noel LB, Walker JM, Moorer CA, Dear MR, et al. Pressure sores among hospitalized patients. Ann Intern Med. (1986) 105:337–42. doi: 10.7326/0003-4819-105-3-337
21. Exton-Smith AN, Sherwin RW. The prevention of pressure sores. Significance of spontaneous bodily movements. Lancet (London, England). (1961) 2:1124–6. doi: 10.1016/s0140-6736(61)91033-9
22. Gosnell DJ. Pressure sore risk assessment: a critique. Part I. The Gosnell scale. Decubitus. (1989) 2:32–8.2775472
23. Higgins JP, Orlando GS, Blondeel PN. Ischial pressure sore reconstruction using an inferior gluteal artery perforator (IGAP) flap. Br J Plast Surg. (2002) 55:83–5. doi: 10.1054/bjps.2001.3713
24. Pers M. Plastic surgery for pressure sores. Paraplegia. (1987) 25:275–8. doi: 10.1038/sc.1987.51
25. Schryvers OI, Stranc MF, Nance PW. Surgical treatment of pressure ulcers: 20-year experience. Arch Phys Med Rehabil. (2000) 81:1556–62. doi: 10.1053/apmr.2000.17828
26. Stotts NA, Paul SM. Pressure ulcer development in surgical patients. Decubitus. (1988) 1:24–30. doi: 10.1097/00006527-198900940-00009
27. Farion K, Michalowski W, Wilk S, O'Sullivan D, Matwin S. A tree-based decision model to support prediction of the severity of asthma exacerbations in children. J Med Syst. (2010) 34:551–62. doi: 10.1007/s10916-009-9268-7
28. Zintzaras E, Bai M, Douligeris C, Kowald A, Kanavaros P. A tree-based decision rule for identifying profile groups of cases without predefined classes: application in diffuse large B-cell lymphomas. Comput Biol Med. (2007) 37:637–41. doi: 10.1016/j.compbiomed.2006.06.001
29. Kasbekar PU, Goel P, Jadhav SP. A decision tree analysis of diabetic foot amputation risk in Indian patients. Front Endocrinol (Lausanne). (2017) 8:25. doi: 10.3389/fendo.2017.00025
30. Chang LY, Wang HW. Analysis of traffic injury severity: an application of non-parametric classification tree techniques. Accid Anal Prev. (2006) 38:1019–27. doi: 10.1016/j.aap.2006.04.009
31. Ripley B. tree: Classification and regression trees. R package version 1.0-34. URL: http://CRAN.R-project.org/package=tree. 2013.
32. Guilbault RWR, Ohlsson MA, Afonso AM, Ebell MH. External validation of two classification and regression tree models to predict the outcome of inpatient cardiopulmonary resuscitation. J Viral Hepat. (2017) 32:333–8. doi: 10.1111/jvh.1261710.1177/0885066616686924
33. Shi KQ, Zhou YY, Yan HD, Li H, Wu FL, Xie YY, et al. Classification and regression tree analysis of acute-on-chronic hepatitis B liver failure: seeing the forest for the trees. J Viral Hepat. (2017) 24:132–40. doi: 10.1111/jvh.12617
34. Zimmerman RK, Balasubramani GK, Nowalk MP, Eng H, Urbanski L, Jackson ML, et al. Classification and regression tree (CART) analysis to predict influenza in primary care patients. BMC Infect Dis. (2016) 16:503. doi: 10.1186/s12879-016-1839-x
35. Marin J, Nixon J, Gorecki C. A systematic review of risk factors for the development and recurrence of pressure ulcers in people with spinal cord injuries. Spinal Cord. (2013) 51:522–7. doi: 10.1038/sc.2013.29
36. Bogie KM, Zhang GQ, Roggenkamp SK, Zeng N, Seton J, Tao S, et al. Individualized clinical practice guidelines for pressure injury management: development of an integrated multi-modal biomedical information resource. JMIR Res Protoc. (2018) 7:e10871. doi: 10.2196/10871
37. Tavakoli K, Rutkowski S, Cope C, Hassall M, Barnett R, Richards M, et al. Recurrence rates of ischial sores in para- and tetraplegics treated with hamstring flaps: an 8-year study. Br J Plast Surg. (1999) 52:476–9. doi: 10.1054/bjps.1999.3126
38. Kenneweg KA, Welch MC, Welch PJ. A 9-year retrospective evaluation of 102 pressure ulcer reconstructions. J Wound Care. (2015) 24(Suppl 4a):S12–21. doi: 10.12968/jowc.2015.24.Sup4a.S12
39. Nonnemacher M, Stausberg J, Bartoszek G, Lottko B, Neuhaeuser M, Maier I. Predicting pressure ulcer risk: a multifactorial approach to assess risk factors in a large university hospital population. J Clin Nurs. (2009) 18:99–107. doi: 10.1111/j.1365-2702.2008.02425.x
40. Thompson D. A critical review of the literature on pressure ulcer aetiology. J Wound Care. (2005) 14:87–90. doi: 10.12968/jowc.2005.14.2.26735
41. Halfens RJ. Risk assessment scales for pressure ulcers: a theoretical, methodological, and clinical perspective. Ostomy Wound Manage. (2000) 46:36–40. 42-34.11189546
42. Du AX, Emam S, Gniadecki R. Review of machine learning in predicting dermatological outcomes. Front Med (Lausanne). (2020) 7:266. doi: 10.3389/fmed.2020.00266
43. Nagendran M, Chen Y, Lovejoy CA, Gordon AC, Komorowski M, Harvey H, et al. Artificial intelligence versus clinicians: systematic review of design, reporting standards, and claims of deep learning studies. Br Med J. (2020) 368:m689. doi: 10.1136/bmj.m689
44. Bassett GS, Weinstein SL, Cooper RR. Long-term follow-up of fascia lata transfer for the paralytic hip in myelodysplasia. J Bone Joint Surg Am. (1982) 64:360–5. doi: 10.2106/00004623-198264030-00005
45. Lefèvre C, Bellier-Waast F, Lejeune F, Duteille F, Kieny P, Le Fort M, et al. Ten years of myocutaneous flaps for pressure ulcers in patients with spinal lesions: analysis of complications in the framework of a specialised medical-surgical pathway. J Plast Reconstr Aesthet Surg. (2018) 71:1652–63. doi: 10.1016/j.bjps.2018.07.007
Keywords: risk factor, recurrence, pressure ulcer, surgical reconstruction, decision tree model
Citation: Tsai Y-J, Lin C-H, Yen Y-H, Wu C-C, Carvajal C, Molte NF, Lin P-Y and Hsieh C-H (2023) Risk factors for pressure ulcer recurrence following surgical reconstruction: A cross-sectional retrospective analysis. Front. Surg. 10:970681. doi: 10.3389/fsurg.2023.970681
Received: 16 June 2022; Accepted: 23 January 2023;
Published: 3 March 2023.
Edited by:
Marta Imamura, Universidade de Sao, BrazilReviewed by:
Fatih Zor, Wake Forest University, United StatesYalcin Kulahci, Wake Forest University, United States
© 2023 Tsai, Lin, Yen, Wu, Carvajal, Molte, Lin and Hsieh. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pao-Yuan Lin cGFveXVhbjkyMTlAZ21haWwuY29t Ching-Hua Hsieh bTkzY2hpbmdodWFAZ21haWwuY29t
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Yueh-Ju Tsai
Yueh-Ju Tsai Cen-Hung Lin
Cen-Hung Lin Ching-Hua Hsieh
Ching-Hua Hsieh