- 1Department for Orthopedic and Traumatology Surgery, University Hospital Bonn, Bonn, Germany
- 2Department for Orthopedic and Traumatology Surgery, University Hospital Wuppertal, Wuppertal, Germany
Background: Climate change and its consequences on our everyday life have also tremendous impacts on public health and the health of each individual. The healthcare sector currently accounts for 4.4% of global greenhouse gas emissions. The share of the emissions in the health care system caused by the transportation sector is 7%. The study analyses the effect of video consultation on the CO2 emissions during the Covid-19 pandemic in an outpatient clinic of the department of orthopaedics and traumatology surgery at a German university hospital.
Methods: The study participants were patients who obtained a video consultation in the period from June to December 2020 and voluntarily completed a questionnaire after the consultation. The type of transport, travel time and waiting time as well as patient satisfaction were recorded by questionnaire.
Results: The study comprised 51 consultations. About 70% of respondents would have travelled to the clinic by car. The reduction in greenhouse gas emissions of video consultations compared to a face-to-face presentation was 97% in our model investigation.
Conclusion: The video consultation can be a very important part of the reduction of greenhouse gas emissions in the health care system. It also saves time for the doctor and patient and can form an essential part of individual patient care.
1. Introduction
Climate change and its consequences on our everyday life have also tremendous impacts on public health and the health of each individual. In addition to the direct consequences of air pollution, such as respiratory diseases, the effects on health also include the indirect consequences of climate change, such as the spread of infectious diseases due to globalization, food shortages and consequently malnutrition and migration (1–3). For the year 2018, the European Environment Agency describes in its 2019 report that the premature death of 400,000 people in the EU is due to air pollution. This is explained by the increase in heart attacks (12%), lung cancer (11%) and strokes (11%) linked to air pollution. This concerns especially vulnerable people with pre-existing health conditions. By reducing greenhouse gas emissions, premature deaths also decrease (4–8).
The major part of greenhouse gases is produced by the combustion of fossil fuels. If their proportion in the atmosphere increases, this leads to an intensification of the greenhouse effect and thus to global warming. Greenhouse gases include carbon dioxide (CO2), methane (CH4), nitrous oxide (N2O2), chlorofluorocarbon (CFC) and water vapour (7). A CO2 equivalent (CO2e) is a measure of the global warming potential of a substance or the climate-damaging effect of an activity (1, 6). The healthcare sector currently accounts for 4.4% of global greenhouse gas emissions. According to the organisation “Health Care Without Harm” (HCWH), the EU's amount of global healthcare sector emissions is 12% (8). In Germany, the share of greenhouse gas emission in the health care sector is 5.2% of the total emission (5, 6). The share of greenhouse gas emissions in the health care system caused by the transportation sector is 7%, according to the data in the European Union (5, 6). In HCWH's analyses, the transport sector includes logistics, business travel and operational transport, which also includes the transport of patients and employees (9).
Some colleagues in different sectors of medicine, for example dermatology and urology, have shown that video consultations may reduce CO2 emissions. Studies in the medical specialty of orthopaedics and trauma surgery are still pending (10–12). The aim of the present study was to analyse the effect of video consultation on CO2 emissions using the specific situation during the covid-19 pandemic. We compared the estimated CO2 emissions in a 6-month period when conducting video consultations (VC) with that of a period with an exclusive face-to-face consultation in the outpatient clinic of the orthopaedics and traumatology surgery at a German university hospital.
2. Methods
2.1. Study participants
The study participants were patients who obtained a video consultation in the outpatient clinic of the department orthopaedics and traumatology surgery at a German university hospital in the period from June to December 2020 (Beginning of the Covid-19-pandemic in Germany) and voluntarily completed a questionnaire after the consultation. In the case of underage or mentally impaired patients (n = 2), the questionnaire as well as the supervision of the examination was carried out by the legally authorised person. The study comprised 51 consultations. The gender distribution was balanced in the patient collective (M:22; F:29, D: 1). The median age of the respondents was 51 years (2.7–87.9 years). In all cases of patients under 18 years of age, the consultation was conducted in the presence of the legal guardian, which also respond to the questionnaires. The video consultation are divided into spinal surgery, joint surgery, paediatric orthopaedics and accident surgery.
2.2. Study design and recruitment
All patients were sent an online questionnaire after the appointment. This questionnaire was anonymous and voluntary. It was divided into the following sections: personal data (age group, gender, place of residence), means of transport in case of face-to-face consultation (type of transport, journey), reason for the consultation (complaint region, type of consultation) and patient satisfaction. The response rate to the questionnaires was 60.71%. Only the data of those who had completed the questionnaire were analysed.
2.3. Calculation of Co2-emission
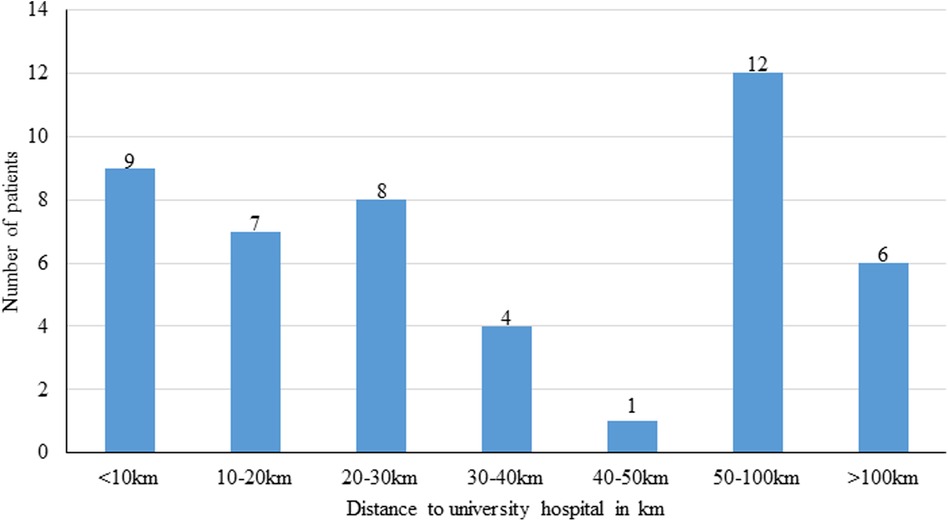
To calculate the greenhouse gas emissions, the route and the type of transport were considered. The calculation of the CO2 emissions was based on the data of the German Federal Environment Agency (4). These data sets include data on emissions of air pollutants from road traffic at regular intervals. This is published in the Handbook of Emission Factors (HBEFA). The German Federal Environment Agency has developed the computer programme TREMOD (Transport Emission Model) to calculate emissions for the period from 1960 to 2050. All passenger and freight transport modes are included in this calculation (13, 14). For our calculations, we used the estimates of the average emissions for transportation; assuming 143 g CO2e per person-kilometre for a journey by car (see Figure 1) (14).
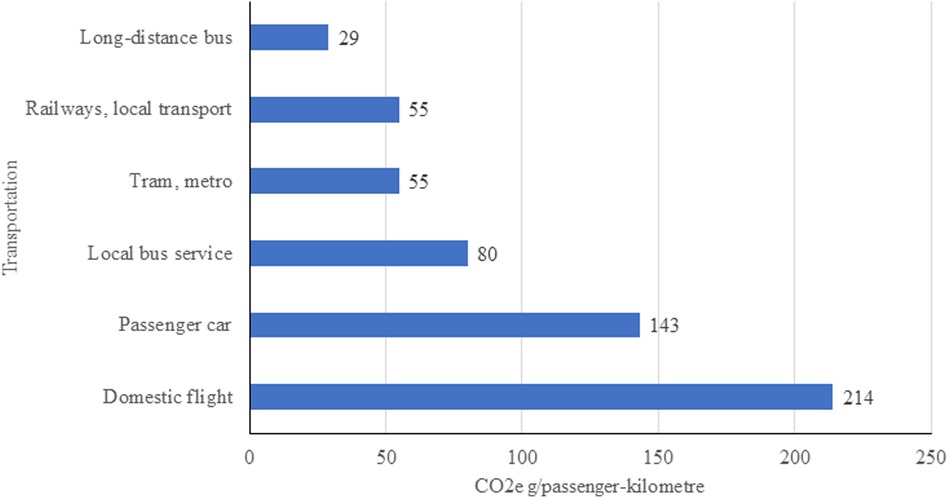
Figure 1. Co2e emission of transportation compiled after the German federal environment agency (6).
In order to adequately calculate the reduction of greenhouse gas emission, the emissions that occur during the performance of a video consultation were also considered (Figure 2). In particular, the power consumption of the data centres (server, storage systems, network and infrastructure) make up the majority of the emissions from video streaming (16, 17).
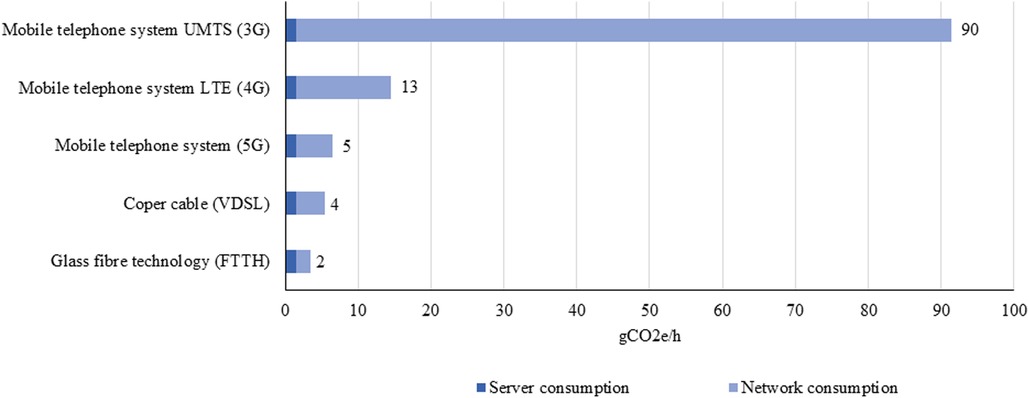
Figure 2. Co2e emission of data centre and network usage compiled after German federal environment agency (UBA) (15).
Fibre optic technology is environmentally most friendly with 2 g CO2e per hour of video streaming compared to the 3G network (UMTS “Universal Mobile Telecommunications System”) with 90 g CO2e (16, 17). In Germany, around 90 percent of households have access to “Very High Speed Digital Subscriber Line” (VDSL) connections with >50 Mbit/s (18). There are large differences between urban (>90%) and rural regions (43%) (19). Assuming that most German households have a VDSL connection, a 1-hour video consultation generates approx. 4 g CO2e per hour of video consultation (13, 18).
2.4. Outcomes
The primary endpoint of the study to evaluate the greenhouse gas emissions from a video consultation compared to the emissions from a face-to-face consultation. Secondary endpoints included satisfaction, time savings, and feasibility for different patients during a video consultation.
3. Results
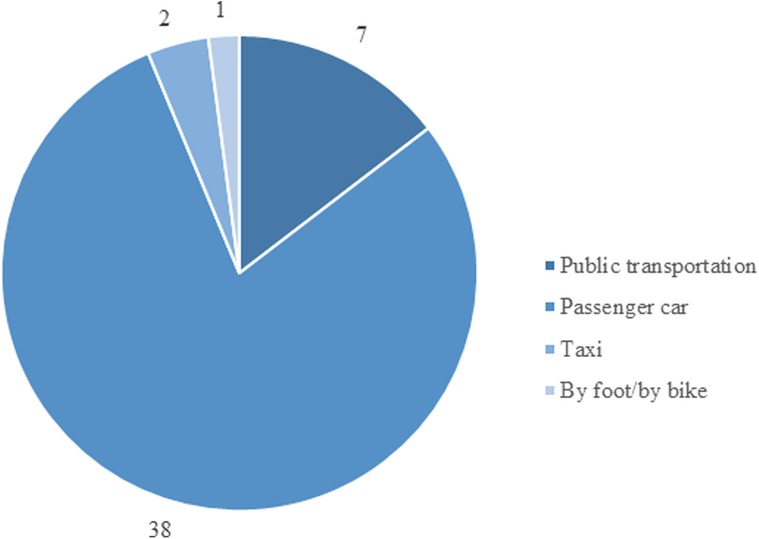
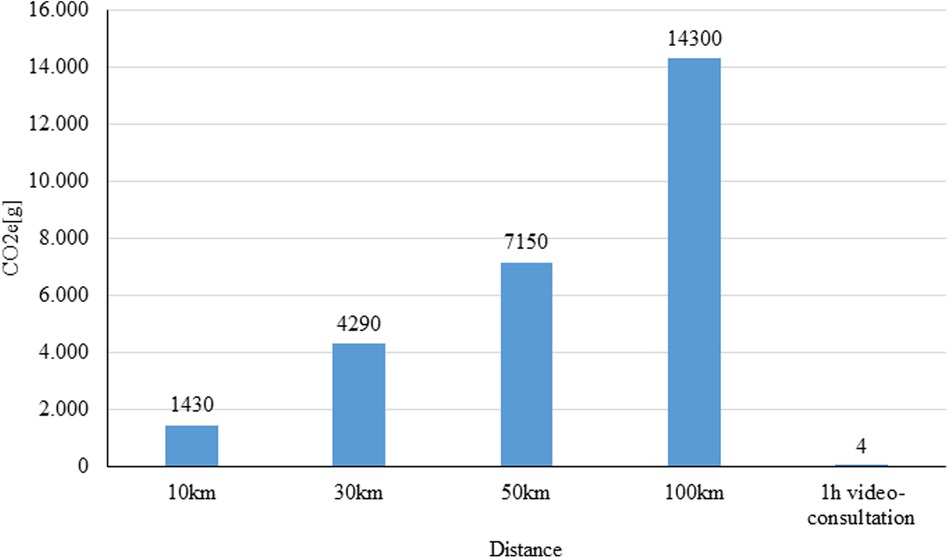
Among the 51 respondents 31% reported a travel distance less than 20 km to the clinic and 35% reported a travel distance of more than 50 km (Figure 3). The travel to the outpatient clinic would have taken less than 2 h for most patients (<1 h: n = 28; 1.5 h: n = 13; 2 h: n = 5; 2.5 h: n = 1; >3 h: n = 1). Most patients (74.5%) would have chosen to travel to the outpatient clinic by car. The search for a parking space would have taken about 30 min for most patients (64.7%). About 43.1% of the respondents were dependent on an accompanying person for a visit to our outpatient clinic. The most frequent reason (35.3%) for a consultation at the outpatient clinic was a follow-up. The majority of respondents (76%) conducted the video consultation at home and 9.8% at work. Many patients (43.1%) used their computer, 23.5% their tablet and 29.4% their smartphone for the consultation. On average, a video consultation lasted about 30 min. Two thirds of the respondents said that they would spend more than 2 h at every visit in an outpatient clinic for a face-to-face-appointment. A high percentage (84.3%) of the respondents were very satisfied or satisfied with the video consultation. Half of the respondents (n = 22) who completed a video consultation were dependent on an escort.
The data demonstrated a meaningful CO2 reduction, with a significant difference between the groups (p < 0.001). With reference to the data of the Federal Environment Agency, it was shown the implementation of the video consultation leads to a reduction in greenhouse gas emissions over 0.5 tons CO2e for the respondents compared to those patients traveling by car (Figure 4).
The most common reason for a video consultation was a follow-up for middle-aged patients with a journey to a special clinic in a distance of more than 30 km. A significant saving in emissions can be observed in patients who need to travel fort more than 10 km to the ambulance. The share of emissions by this group regarding the total emissions was 97.3%. Forty respondents would have driven to the outpatient department by car. On average, they would have to drive a distance of about 33 km (median 33.5 km; min 5 km, max 179 km). This would have resulted in around 0.5 tons CO2e. This is in contrast to 4 g CO2e used per one session of video consultation. The time the patient and the doctor were involved during the video consultation was included in the calculation. This resulted in a total of about 160 g of CO2e for all video consultations (Figure 5).
When 78.4% of the respondents would have travelled by car (incl. taxi), a total of 586,872 g CO2e would have be produced per return journey to the university's outpatient clinic. The high emission of patients who reported they would have use public transport to get to the clinic would have caused the emission of 15,299 g CO2e. Based on the current workload of the clinic's outpatient department with about 400 consultations per week, and assuming that about 20% of the consultations can also be performed online, it would significantly reduce greenhouse gas emissions.
4. Discussion
As one of the first estimates of the daily routine of the outpatient department for orthopaedics and trauma university hospital we have shown that, the implementation of video consultations can lead to a significant reduction in greenhouse gas emission. By running video consultations only, the German university clinic could reduce greenhouse gas emissions by 97% compared to face-to-face consultations. This result shows that there is a high potential for CO2 reduction in the implementation of video consultation.
The Federal Environment Agency of Germany estimated the total greenhouse gas emissions for Germany in 2019 to be about 810 GtCO2e. The emissions for the health care sector should have contributed about 42.12 GtCO2e (5.2% of national emissions) and the transport sector in the health care sector accounts for 2.95 GtCO2e (7% of emissions in the health care sector) (4, 6). Thus, reduction in this sector may significantly contribute to achieving the climate targets of Germany and the European Union. However, it is also important to mention that the use of digital media also has an impact on our environment through the power consumption of the servers and the use of rare earths for production. In addition, an electronic device have a limited lifespan and need to be replaced at regular intervals (16, 17). In order to make this technology even more environmentally friendly, demand-oriented planning should be aimed for. This includes the expansion of fibre optic cables, the sustainable operation of data centres and the economical use of mobile data transmission (16, 17).
Thanks to the video consultation, many patients can avoid potentially long journeys to a specialised university hospital for a second opinion or follow-up checks. A basic physical examination during a video consultation is possible or can be carried out by the general practitioner on site. Difficulties arise in particular with language barriers and pending imaging (e.g., sonography, x-ray diagnostics), where treatment may be delayed (20, 21). On the other hand, follow-up examinations in particular can be easily completed online, as the examiner is aware of the initial situation (22, 23). The video consultation also saves a lot of time for the patients and healthcare providers. On average, a video consultation lasts about 30 min. This is in contrast to the physical consultations, where the respondents reported a stay of about 2 h in our outpatient clinic with additional travel time (24, 25). The aim of the outpatient clinic is to avoid unnecessary in-person patient appointments and, if possible, to carry out a large part of the presentation by video consultation (26). The special challenge for orthopaedic patients is their limited mobility. Often these patients need an escort or help to get to the doctor. This is shown by the fact that half of the patients in our surveys were dependent on an escort. The video consultation can therefore also save the time for the escort.
In contrast to some other regions in Europe or Germany, the travel to a hospital in North Rhine-Westphalia (NRW) is within 8–12 min. for an ambulance and therefore comparatively short (27–29). In addition, there are many maximum-care hospitals in this region, so that a journey to a specialist is relatively short by European standards. For example, Buvik et al. describe distances of up to 250 km to a specialist in Norway (30). This is mainly due to the high population density and correspondent large number hospitals (344 in NRW as of 2017) (27, 30–32). The present study points out that the offer of a video consultation is a great advantage especially for patients who have a long journey (>50 km) to a specialised clinic. When talking about telecommunication, the still expandable access to the internet in the mainly rural regions should also be discussed. Patients in rural areas not only have to travel a long way to see specialists, but they also have limited opportunities for telemedicine. In Germany, less than 50% of the households in rural areas are connected to a data transmission rate of 50 Mbit/s or above (19). In order to increasingly establish telemedicine in Germany, this must be accompanied by an expansion of the digital infrastructure (13, 18, 33).
In their analysis of data from the National Health Service (NHS) UK, Wotton et al. divided the travel section into three groups: patient travel, visitor travel, staff travel and business travel. The total travel emissions were estimated to be about 49,000 tCO2e per year (34). This study showed, that over 40% of emissions due to travel were attributable to patient travel (34). Approximately one fifth was due to travel by healthcare workers. This shows the great potential for greenhouse gas reduction that exists in telehealth. Teleworking should also be expanded in the healthcare system. The SARS-CoV-2 pandemic has accelerated this development. The rapid changeover to video consultation would be possible because the telematic infrastructure had been intensified since a long time. On January 1st, 2016, the German Federal Ministry of Health stipulated the expansion of the digitalisation of medicine in the Social Code Book V in the “E-Health-Law”. In addition to the electronic doctor's letter and the electronic patient file, this also includes the offer of a video consultation. Telemedicine is one more step towards the digitalisation of medicine and thus towards more self-determined, individualised and modernised medicine. This obliges hospitals, health insurance companies and independent physicians to offer more telemedicine (20, 33, 35).
In addition to the reduction of greenhouse gas emissions from video consultation, the reduction of electricity consumption, waste production, and water pollution must also be considered to improve environmental protection (9–11). According to the HCWH report, the generation and distribution of electricity, gas and heat or cooling form the largest portion of greenhouse gas emissions in the healthcare system (9). In their analysis of emissions in the NHS, Conner et al. determined that 15% of emission is due to transport an another major part of emission (72%) by patient care is due to electricity consumption, waste production, and water pollution. Fathy et al. listed several possibilities for reduction of emissions such as the use of recycled paper, energy-inefficient office devices, or the use of water-saving systems, respectively (10). This shows where, apart from telemedicine, there is still a great potential for further consideration of environmental protection in medicine.
In various fields of medicine, such as urology and dermatology, studies have already been conducted on the influence of video consultation on emissions. Examples of this are the works of Croghan et al. and Fathy et al. (10, 35). Croghan et al. conducted more than 70% of their consultations in their clinic in the field of urology online in the context of the Corona pandemic. In their research, they showed that patients saved an average of 50 km of travel to the clinic, similar to our study. In accordance with our study, they showed that most savings occur when patients travel to the clinic by car (10, 35).
The present study refers exclusively to an outpatient clinic for orthopaedics and traumatology surgery. The feasibility must be adapted for different field of medicine (11, 22, 36). Due to the disease of the musculoskeletal system in orthopaedics and trauma surgery, recognition of instabilities, stiffening, degrees of movement etc. is essential. However, our study has shown that the video consultation can be used as a follow-up examination. The future aim should be to enable doctors and patients also to perform the initial examination as a video consultation. The video consultation should not be less qualitative and clinically informative than a face-to-face examination. The reason why in many cases colleagues still prefer a face-to-face presentation to a video consultation is the lack of standards and guidelines for the online examination of orthopaedic trauma surgery of patients. Currently, many working groups are trying to establish a standardised form for clinical diagnostics via video consultation (22, 23).
The video consultation offers the possibility of changing the daily routine at the clinic through the possibility of a work from home. In this way, the profession of doctor can be integrated into the modern, digital workplace. According to the research report of the German Federal Ministry of Labour and Social Affairs, mobile working leads to a significantly higher level of employee satisfaction (37). In addition, the doctors’ commute can be reduced, which can lead to a further reduction in CO2 emissions. This was not yet analysed in the study, as the doctors were in the hospital during the video consultation.
Since the protection of public health is the most important task of the health care system and CO2 emissions have such a great impact on public health, the reduction of emissions in terms of transportation, energy consumption, waste production and water pollution is of fundamental importance (9, 10, 38).
5. Limitations
One point of criticism of the study could be the imprecise data on the data transfer rate of the patients, but a significant expansion of the telecommunication infrastructure can be expected in the metropolitan areas. In rural regions, access to broadband connections is often not available (18). It should also be noted here that the age group between 40 and 65 is particularly well represented. The reason for this is likely the lack of digital competence among the elderly and geriatric patient group. However, this patient group represents the majority of the patients in most departments. In addition, it should be mentioned in the projections that the transport sector in the health care system not only includes the travel of patients, but also other types of transport, such as the travel of staff, visitors, etc (2). Video consultation cannot be carried out for all consultations because in some cases a personal examination is indispensable. A disadvantage of the digital consultation is the lack of possibilities for physical examinations in the case of musculoskeletal diseases. In addition, direct diagnostic imaging is not possible, which can lead to a delay in the correct treatment. Also, in the case of language barriers, video consulting can only lead to limited results.
6. Conclusion
In our study, we have shown that conducting a video consultation leads to a 97% reduction in greenhouse gas emissions compared to a face-to-face presentation in our model investigation of an outpatient clinic of orthopaedics and traumatology surgery. Video consultations are an important step towards more environmental protection in medicine by significantly reducing greenhouse gas emissions. The video consultation can be an important part of the reduction of greenhouse gas emissions in the health care system, it also saves time for the doctor and patient and is an important part of individual patient care.
So far, there are no guidelines and standards for the digital examination of orthopaedic and trauma surgery patients in Germany; these will have to be worked out in the near future.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethikkommission an der Medizinischen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn. The patients/participants provided their written informed consent to participate in this study.
Author contributions
EMA, TRJ, JB, JJR, MB, TMR, KW, CB and KK contributed conception and design of the study, EMA, TRJ, TMR, KW and KK designed the questionnaires. EMA, JB, JJR and MB analysed the questionnaires. EMA wrote the first draft of the manuscript and prepared the figures. All authors contributed to manuscript, revision, read and approved the submitted version.
Funding
Funding by the University Hospital of Bonn.
Acknowledgments
The authors would like to thank the team of the Department of Orthopaedics and Traumatology Surgery of the University Hospital of Bonn.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Barrett B, Charles JW, Temte JL. Climate change, human health, and epidemiological transition. Prev Med. (2015) 70:69–75. doi: 10.1016/j.ypmed.2014.11.013
2. McMichael AJ, Woodruff RE, Hales S. Climate change and human health: present and future risks. Lancet. (2006) 367:859–69. doi: 10.1016/S0140-6736(06)68079-3
3. Tennison I, Roschnik S, Ashby B, Boyd R, Hamilton I, Oreszczyn T, et al. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. (2021) 5:e84–92. doi: 10.1016/S2542-5196(20)30271-0
4. Umweltbundesamt. Treibhausgas-Emissionen in Deutschland (2022). Available at: https://www.umweltbundesamt.de/daten/klima/treibhausgas-emissionen-in-deutschland#emissionsentwicklung.
5. Gonzalez E. Air quality in Europe. Luxembourg: Publications Office of the European Union (2020). 1160.
6. Karliner J. Health care’s climate footprint: how the health sector contributes to the global climate crisis and opportunities for action 2019. ARUP (2020). p. 48.
7. European Commission. Greenhouse gas emissions - raising the ambition (2021). Available at: https://ec.europa.eu/clima/eu-action/climate-strategies-targets/2030-climate-energy-framework_de.
8. Schneider M, Karmann A, Braeseke G. Politische Handlungsempfehlungen. Umweltbundesamt (2020). p. 13.
9. WHO. Climate change and health (2021). Available at: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health.
10. Fathy R, Nelson CA, Barbieri JS. Combating climate change in the clinic: cost-effective strategies to decrease the carbon footprint of outpatient dermatologic practice. Int J Womens Dermatol. (2021) 7:107–11. doi: 10.1016/j.ijwd.2020.05.015
11. Connor A, Lillywhite R, Cooke MW. The carbon footprint of a renal service in the United Kingdom. QJM. (2010) 103:965–75. doi: 10.1093/qjmed/hcq150
12. Purohit A, Smith J, Hibble A. Does telemedicine reduce the carbon footprint of healthcare? A systematic review. Future Health J. (2021) 8(1):e85–e91. doi: 10.7861/fhj.2020-0080
14. Umweltbundesamt. Emissionsdaten (2022). Available at: https://www.umweltbundesamt.de/themen/verkehr-laerm/emissionsdaten.
15. Umweltbundesamt. Video-Streaming: Art der Datenübertragung entscheidend für Klimabilanz (2020). Available at: https://www.umweltbundesamt.de/presse/pressemitteilungen/video-streaming-art-der-datenuebertragung.
16. Schödwell B. Kennzahlen und Indikatoren für die Beurteilung der Ressourceneffizienz von Rechenzentren und Prüfung der praktischen Anwendbarkeit (2018).
17. Köhn M, Gröger J, Stobbe L. Energie- und Ressourceneffizienz digitaler Infrastrukturen Ergebnisse des Forschungsprojektes "Green Cloud-Computing". Umweltbundesamt (2020).
18. Bundesnetzargentur. Breitbandatlas (2021). Available at: https://www.bundesnetzagentur.de/DE/Fachthemen/Telekommunikation/Breitband/breitbandatlas/start.html.
19. Bundesminiterium für Verkehrkehr und digital Infrastruktur. Breitband-verfuegbarkeit-mitte-2020. Bundesminiterium für Verkehrkehr und digital Infrastruktur (2020). p. 20.
20. Bundesministerium für Gesundheit. E-Health (2022). Available at: https://www.bundesgesundheitsministerium.de/service/begriffe-von-a-z/e/e-health.html.
21. Makhni MC, Riew GJ, Sumathipala MG. Telemedicine in orthopaedic surgery: challenges and opportunities. J Bone Joint Surg Am. (2020) 102:1109–15. doi: 10.2106/JBJS.20.00452
22. Welle K, Täger S, Hackenberg RK, Markowetz A, Schildberg FA, Burger C, et al. Die untersuchung der hand in der videosprechstunde. Z Orthop Unfall. (2021) 159:202–8. doi: 10.1055/a-1304-3593
23. Jansen T, Gathen M, Touet A, Goost H, Wirtz DC, Burger C, et al. Telemedizinische wirbelsäulenuntersuchung während der COVID-19-pandemie. Z Orthop Unfall. (2021) 159:193–201. doi: 10.1055/a-1283-7160
24. Dullet NW, Geraghty EM, Kaufman T, Kissee JL, King J, Dharmar M, et al. Impact of a university-based outpatient telemedicine program on time savings, travel costs, and environmental pollutants. Value Health. (2017) 20:542–6. doi: 10.1016/j.jval.2017.01.014
25. Kabir K, Goost H, Gathen M, Scheidt S, Wimmer M, Täger S, et al. Prozessanalyse der ambulanten behandlung unfallchirurgischer patienten an einer universitären poliklinik. Unfallchirurg. (2020) 123:507–16. doi: 10.1007/s00113-020-00809-3
26. Holderried M, Schlipf M, Höper A, Meier R, Stöckle U, Kraus TM. Chancen und risiken der telemedizin in der orthopädie und unfallchirurgie. Z Orthop Unfall. (2018) 156:68–77. doi: 10.1055/s-0043-116941
28. Völker S. Die inanspruchnahme der ambulanten notfallversorgung in westfalen-lippe: eine medizingeographische studie. Gesundheitswesen. (2019) 81:471–7. doi: 10.1055/s-0043-119082
29. van den Heuvel D, Veer A, Greuel H-W. Geriatrische versorgungsstrukturen in deutschland. Der geriatrische versorgungsverbund als bedarfsgerechte weiterentwicklung. Z Gerontol Geriat. (2014) 47:13–6. doi: 10.1007/s00391-013-0570-0
30. Buvik A. Cost-effectiveness of telemedicine in remote orthopedic consultations: randomized controlled trial. J Med Internet Res. (2019) 21(2):e11330. doi: 10.2196/11330
31. Deutsche Krankenhausgesellschaft. Bestandsaufnahme zur Krankenhausplanung und Investitionsfinanzierung in den Bundesländern. Deutsche Krankenhausgesellschaft (2019).
32. Isfort M. Entwicklung_Gesundheitsberufe_NRW_2015_web. Bundesministerium für Gesundheit (2016). p. 354.
33. Bundeärztekammer. Hinweise und Erläuterungen zu § 7 Abs. 4 MBO-Ä–Behandlung im persönlichen Kontakt und Fernbehandlung. Deutsches Ärzteblatt (2019).
34. Wootton R, Tait A, Croft A. Environmental aspects of health care in the Grampian NHS region and the place of telehealth. J Telemed Telecare. (2010) 16:215–20. doi: 10.1258/jtt.2010.004015
35. Croghan SM. Time, cost and carbon-efficiency: a silver lining of COVID era virtual urology clinics? Ann R Coll Surg Engl. (2021) 103(8):599–603. doi: 10.1308/rcsann.2021.0097
36. Oliveira TC, Barlow J, Gonçalves L, Bayer S. Teleconsultations reduce greenhouse gas emissions. J Health Serv Res Policy. (2013) 18:209–14. doi: 10.1177/1355819613492717
37. Bundesministerium für Arbeit und Soziales. Verbreitung und Auswirkung von mobiler Arbeit und Homeoffice (2020).
Keywords: carbon footprint, telemedicine, video consultation, orthopaedic and trauma surgery, COVID-19
Citation: Arndt E-M, Jansen TR, Bojko J, Roos JJ, Babasiz M, Randau TM, Welle K, Burger C and Kabir K (2023) COVID-19 measures as an opportunity to reduce the environmental footprint in orthopaedic and trauma surgery. Front. Surg. 10:959639. doi: 10.3389/fsurg.2023.959639
Received: 18 July 2022; Accepted: 22 March 2023;
Published: 12 April 2023.
Edited by:
Savvas Lampridis, Hammersmith Hospital, United KingdomReviewed by:
Siegmund Lang, University Medical Center Regensburg, GermanyQiuyue Ding, Guizhou Provincial People's Hospital, China
Yongzhi Cui, Shanghai Jiao Tong University, China
© 2023 Arndt, Jansen, Bojko, Roos, Babasiz, Randau, Welle, Burger and Kabir. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eva-Maria Arndt ZXZhLW1hcmlhLmFybmR0QHVrYm9ubi5kZQ==
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Eva-Maria Arndt
Eva-Maria Arndt Tom Rainer Jansen
Tom Rainer Jansen Thomas Martin Randau
Thomas Martin Randau Kristian Welle
Kristian Welle