
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg. , 15 March 2023
Sec. Orthopedic Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.916694
 Hossein Saremi1*†
Hossein Saremi1*† Mohamadali seifrabiei2
Mohamadali seifrabiei2
Background: In the current study, we performed a systematic review and meta-analysis regarding the comparison of accuracy, sensitivity, and specificity of the techniques in diagnosing SSC tendon tears. Also, we performed a systematic review of the classification of SSC tendon tears.
Methods: English language, peer-reviewed journal publications from the first date available to March 2022 were extracted by searching PubMed and Web of Science databases. A forest plot was used to graphically show the results of pooled sensitivity, specificity, and accuracy of different diagnostic modalities.
Results: There were six studies on using MRI to diagnose subscapularis tendon tears, five studies on MRI, four studies on clinical examination, one on ultrasonography, and one on CT arthrography. Pooled sensitivity values for MRI, MRA, clinical examination, ultrasonography, and CT arthrography were 0.71 (CI: 0.54; 0.87), 0.83 (0.77; 0.88), 0.49 (0.31; 0.67), 0.39 (0.29; 0.51), and 0.90 (0.72–0.97), respectively. The pooled specificity values for MRI, MRA, clinical examination, ultrasonography, and CT arthrography were 0.93 (CI: 0.89; 0.96), 0.86 (0.75; 0.93), 0.89 (0.73; 0.96), 0.93 (0.88; 0.96), and 0.90 (0.69; 0.98), respectively. The pooled diagnostic accuracy values for MRI, MRA, clinical examination, ultrasonography, and CT arthrography were 0.84 (CI: 0.80; 0.88), 0.85 (0.77; 0.90), 0.76 (0.66; 0.84), 0.76 (0.70; 0.81), and 0.90 (0.78; 0.96), respectively.
Conclusion: According to our systematic review and meta-analysis, MR arthrography was the most accurate in diagnosing subscapularis tears. MR arthrography was the most sensitive, and MRI and ultrasonography were the most specific in detecting subscapularis tears.
The rotator cuff muscle group is formed by the subscapularis (SSC) muscle, supraspinatus muscle, infraspinatus muscle, and teres minor muscle at the posterior scapular region. The SSC muscle originates from the subscapularis fossa of the scapula, inserts into the lesser tubercle of the humerus, and is innervated by the superior and inferior subscapular nerves. The SSC muscle is the largest component of the aforementioned rotator cuff; it is responsible for the elevation and internal rotation of the shoulder and has a crucial role in stabilizing the glenohumeral joint (1). As the subscapularis tendon tear is a prevalent painful condition followed by a significant loss of function, timely diagnosis and management of this condition are of crucial importance (2). Until now, several classifications have been proposed by Fox et al., Lyons, Lafosse et al., and Touissant et al. (3–6). However, there is no consensus regarding the classification of this condition, which may hinder clinical evaluation, diagnosis, and management.
The most sensitive and specific clinical examinations to assess an SCC tendon tear are the lift-off test, the belly-press test, and the bear-hug test. Increased external rotation compared to normal shoulder rotation and weakness in internal rotation also help in the diagnosis (7). Although these tests are essential for the diagnosis of SSC tendon tears, various imaging modalities such as magnetic resonance imaging (MRI), computed tomography (CT) scanning, magnetic resonance arthrography (MRA), and ultrasonography (US) may also be indicated (8). Since the SCC plays a crucial role in shoulder function, evaluating diagnostic modalities is of great significance. Misdiagnosed SSC tendon tears may result in unbalanced force, persistent shoulder pain, and weakness even after cuff repair (9). The gold standard diagnostic test for SSC tendon tears is arthroscopy, which helps the physician precisely evaluate the humeral and glenoid aspects of the joint space (10). As arthroscopy is an invasive, technically demanding, and expensive technique, using the aforementioned clinical assessments and imaging modalities can replace the necessity of performing an arthroscopy to diagnose SCC tendon tears. While several studies have provided evidence-based guidelines for the examination, diagnosis, and management of SSC tendon tears, no previous systematic review and meta-analysis studies have evaluated the diagnostic accuracy of MRI, MRA, CT scanning, US, and clinical assessments in the diagnosis of SSC tendon tears. Also, as mentioned earlier in the manuscript, a consensus regarding the classification of SSC tendon tears is still lacking.
In the current study, we performed a systematic review and meta-analysis regarding the comparison of accuracy, sensitivity, and specificity of these techniques in diagnosing SSC tendon tears. Also, we performed a systematic review of the classification of SSC tendon tears.
We conducted a systematic review of the pieces of evidence for the diagnosis of subscapular tears with different diagnostic tools and studies on classification methods for subscapular tears. English language, peer-reviewed journal publications from the first date available to March 2022 were extracted by searching PubMed and Web of Science databases. The combination of the following search terms was used: subscapularis tear, diagnosis, and classification. After removing duplicate studies, the retrieved records were screened for title and abstract. The full text of eligible studies, selected from the previous step, was screened and reviewed. The data of interest were the sensitivity, specificity, and accuracy of different diagnostic tools in subscapularis tendon tears.
The eligible studies were observational studies (cross-sectional and cohort studies) on the diagnostic accuracy of imaging modalities and clinical assessments in subscapularis tendon tears. We excluded the studies that have one or more of the following criteria: (1) studies that were on rotator cuff tendons other than the subscapularis tendon (e.g., supraspinatus); (2) systematic reviews, meta-analysis studies, reviews, case reports, case series, and gray literature; (3) studies with no control group; (4) studies where the number of patients with subscapularis tendon tears was not specified; and (5) full text in any language other than English. For meta-analysis, we also excluded studies as reference tests other than arthroscopy (e.g., MRI or MR arthrography) because arthroscopy is the gold standard for diagnosing subscapularis tendon tears.
For data analysis, we used a meta package in R statistical software (version 4.1.1). The sensitivity, specificity, and accuracy of different diagnostic tests were calculated with a 95% confidence interval (CI). Sensitivity was considered as true-positive cases divided by total patients with a subscapularis tendon tear; specificity was considered as true-negative cases divided by total cases with an intact subscapularis tendon (confirmed by arthroscopy). Accuracy was considered as true-positive and true-negative cases divided by total subjects in the study. The random-effects model was used for calculating pooled sensitivity, specificity, and accuracy. In this study, subgroup analysis was used to report pooled sensitivity, specificity, and accuracy for different diagnostic tools. The forest plot was used to graphically represent the results of calculated pooled sensitivity, specificity, and accuracy for different subgroups. The I2 statistic was used to evaluate the heterogeneity in the included studies for each subgroup.
The flow diagram of selected studies is shown in Figure 1. After reming duplicate records, 305 studies retrieved from online databases were screened for title andabstract. Thirty-two studies accomplished the inclusion criteria for full-text review. Six studies were excluded, leading to a final inclusion of 26 studies. The characteristics of the selected studies are presented in Table 1. Among them, seven studies were on the classification of the subscapularis tendon tear and 19 studies were on the diagnosis of subscapularis tendon tear. One study was excluded from meta-analysis because the reference test was MRI and not arthroscopy. Eighteen studies were included in our meta-analysis, and of 2,593 total subjects, 892 had subscapularis tendon tears.
There were six studies on using MRI to diagnose subscapularis tendon tears, five studies on MRI, four studies on clinical examination, one on ultrasonography, and one on CT arthrography. As shown in Figure 2, the pooled sensitivity values for MRI, MRA, clinical examination, ultrasonography, and CT arthrography were 0.71 (CI: 0.54; 0.87), 0.83 (0.77; 0.88), 0.49 (0.31; 0.67), 0.39 (0.29; 0.51), and 0.90 (0.72–0.97), respectively. The I2 statistic for each subgroup is shown in Figure 2. The pooled specificity values for MRI, MRA, clinical examination, ultrasonography, and CT arthrography were 0.93 (CI: 0.89; 0.96), 0.86 (0.75; 0.93), 0.89 (0.73; 0.96), 0.93 (0.88; 0.96), and 0.90 (0.69; 0.98), respectively. The I2 statistic for each subgroup is shown in Figure 3. The pooled diagnostic accuracy values for MRI, MRA, clinical examination, and CT arthrography were 0.84 (CI: 0.80; 0.88), 0.85 (0.77; 0.90), 0.76 (0.66; 0.84), 0.76 (0.70; 0.81), and 0.90 (0.78; 0.96) respectively. The I2 statistic for each subgroup is shown in Figure 4.
Seven studies were found on the classification of subscapularis tendon tears (3–6, 29, 30). The different classification types are listed in Table 2.
To our knowledge, this is the first systematic review and meta-analysis comparing the accuracy of different methods in diagnosing subscapularis tears. Our systematic review and meta-analysis showed that MR arthrography and CT arthrography were the most accuracte in diagnosing subscapularis tears, with accuracy values of 85% and 90%, respectively. However, there was only one study on the diagnostic accuracy of CT arthrography, and one is not enough to conclude. MRA and CT arthrography were the most sensitive, with a sensitivity of 83% for MR arthrography and 90% for CT arthrography. Again, the results could not be reliable due to the low sample size in CT arthrography. MRI and ultrasonography were the most specific in detecting subscapularis tears, with a specificity of 93% for both of them. However, ultrasonography has much lower sensitivity, resulting in lower accuracy than MRI.
Clinical assessment and imaging studies are the two main methods for diagnosing subscapularis tendon tears (9). Generally, our meta-analysis showed that imaging studies are more accurate, sensitive, and specific than clinical assessment in the diagnosis of subscapularis tendon tears. However, clinical assessments could have high specificity in detecting such disorders. The patients may report weakness in internal rotation but is nonspecific of a subscapularis tendon tear. In our study, the clinical test used for the diagnosis of subscapularis tendon tear was the lift-off test; a previous meta-analysis of the lift-off test by Lädermann et al. showed that it has the highest accuracy among all clinical tests (31). However, clinical tests are subjective. The subscapularis tendon strength can be assessed by a dynamometer, which provides force comparison with the contralateral shoulder and objective values (9).
Ultrasonography is among other imaging techniques for the diagnosis of subscapularis tendon disorders . Although there are numerous studies on the accuracy of ultrasonography for diagnosing rotator cuff tendon tears particularly supraspinatus tendon tears, there are limited studies on the accuracy of ultrasonography in diagnosing subscapularis tendon tears (32). A meta-analysis conducted by Farooqi et al. on the diagnostic accuracy of ultrasonography for rotator cuff tears showed that ultrasonography has a more diagnostic accuracy for bicep tendon tears (93%) and supraspinatus tendon tears (83%) compared to subscapularis tendon tears (76%). However, ultrasonography is highly specific in detecting subscapularis tendon tears (93%) compared to other imaging modalities. Thus, a positive result could be considered for subsequent definitive diagnosis and management procedures such as arthroscopy, but a negative result needs more diagnostic tests to approve. Further studies on assessing the diagnostic accuracy of ultrasonography for subscapularis tendon tears are required to make more definitive conclusions.
MRI and MR arthrography are more reliable compared to ultrasonography or clinical assessment for the diagnosis of subscapularis tendon tears (33). A meta-analysis conducted by Malavolta et al. on the efficacy of MRI and MR arthrography in the diagnosis of subscapularis tendon tears showed that the pooled sensitivity and specificity of MRI and MR arthrography in the diagnosis of the subscapularis tendon tears were 68% and 90%, respectively. However, this study did not conduct a separate meta-analysis for MRI and MR arthrography (33). Our study is in line with this meta-analysis as the sensitivity of MRI and MR arthrography is lower than their specificity, which means that MRI and MR arthrography have lower false-positive cases than false-negative cases. Previous studies show that the diagnostic value of MRI is higher in a complete tear of the subscapularis tendon (Type 4 by the Lafosse classification) (16) and the tear of the other rotator cuff tendons (34). The relatively lower sensitivity of MRI and MR arthrography for subscapularis tendon tears than that for other rotator cuff tendons could be explained by its three-dimensional footprint topography of the humeral head, which is explained by Yoo et al. (30), or by some noninsertional types of subscapularis tears (35). $$$$The accuracy also increases with the higher expertise of the reviewer (36). On the other hand, the diagnostic accuracy of MRI and MR arthrography is not affected by the time elapsed from injury to perform the imaging study (16).
Considering the accuracy of each diagnostic tool is important to obtain good clinical and functional outcomes in the treatment of subscapularis tendon tears (37, 38), although treatment of elderly patients is often limited surgically due to the bad quality of the tissue. Hence, a shoulder replacement could be indicated (39).
Classifications of Lafosse (Figures 5A-E), Fox, Lyons, Martetschlager, and Toussaint are based on the insertion site lesions and according to anatomic data and arthroscopic lesion-related findings (3–6, 29). Yoo et al. described a classification based on a three-dimensional anatomic footprint (30). Dierckman’s classification was based on noninsertional tendinopathy of the subscapularis (40). None of the classifications included interstitial tears of the subscapularis tendon described by Saremi et al. (Figure 5F) (35).
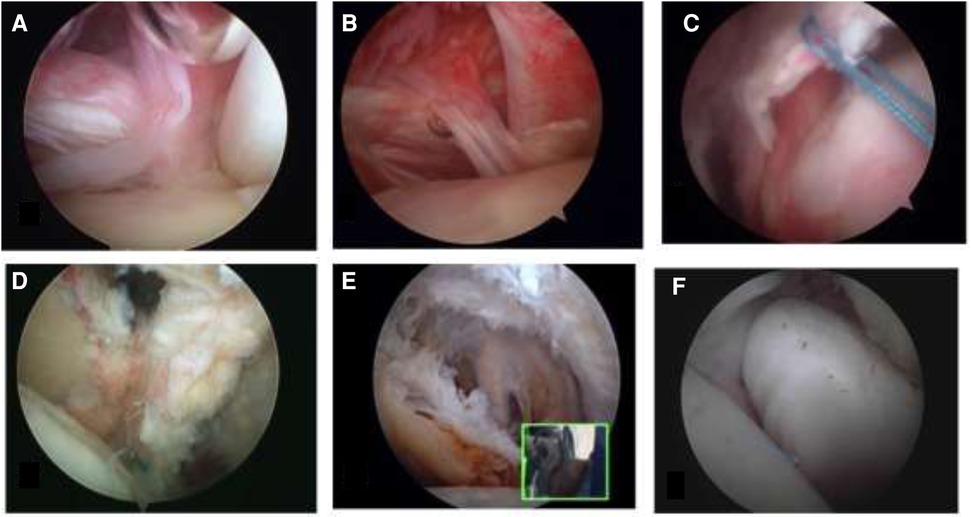
Figure 5. Arthroscopic view of the Lafosse classification of subscapularis tendon tears (A–D) (4), airbag sign, an arthroscopic finding of interstitial tears of the subscapularis tendon (35).
The main strengths of this study are as follows: (1) this is the first systematic review and meta-analysis comparing the accuracy of different methods in diagnosing subscapularis tears; (2) this study compared not only the different imaging modalities but also the accuracy of imaging modalities with clinical examinations; and (3) we conducted a meta-analysis of the sensitivity and specificity in addition to the accuracy of different diagnostic modalities.
The limitation of this study is that we did not compare the specific clinical tests, and we also did not compare complete and partial tears of the subscapularis tendon tear. However, adding another level of subgroups could have affected the possibility of conducting a meta-analysis.
According to our systematic review and meta-analysis, MR arthrography was the most accurate in diagnosing subscapularis tears, MR arthrography was the most sensitive, and MRI and ultrasonography were the most specific in detecting subscapularis tears. Further studies on assessing the diagnostic accuracy of ultrasonography and CT arthrography for subscapularis tendon tears are required to make more definitive conclusions.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
HS: drafted the manuscript, performed the literature search and drafted figures, edited the manuscript and supervised the whole study. MS drafted the manuscript, helped in correct literature search, contributed in data analysis and edited manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Aguirre K, Mudreac A, Anatomy KJ. Shoulder and upper limb, subscapularis muscle. [Updated 2021 Aug 7]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK513344/
2. Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: an anatomic and clinical investigation. Arthroscopy. (2008) 24(9):997–1004. doi: 10.1016/j.arthro.2008.04.076
3. Fox JA, Noerdlinger MA, Romeo AA. Arthroscopic subscapularis repair. Tech Shoulder Elbow Surg. (2003) 4(4):154–68. doi: 10.1097/00132589-200312000-00002
4. Lafosse L, Lanz U, Saintmard B, Campens C. Arthroscopic repair of subscapularis tear: surgical technique and results. Orthop Traumatol Surg Res. (2010) 96(8):S99–S108. doi: 10.1016/j.otsr.2010.09.009
5. Lyons RP, Green A. Subscapularis tendon tears. J Am Acad Orthop Surg. (2005) 13(5):353–63. doi: 10.5435/00124635-200509000-00009
6. Toussaint B, Barth J, Charousset C, Godeneche A, Joudet T, Lefebvre Y, et al. New endoscopic classification for subscapularis lesions. Orthop Traumatol Surg Res. (2012) 98(8 Suppl):S186–92. doi: 10.1016/j.otsr.2012.10.003
7. Barth J, Audebert S, Toussaint B, Charousset C, Godeneche A, Graveleau N, et al. Diagnosis of subscapularis tendon tears: are available diagnostic tests pertinent for a positive diagnosis? Orthop Traumatol Surg Res. (2012) 98(8 Suppl):S178–85. doi: 10.1016/j.otsr.2012.09.008
8. Ahmad ZY, Diaz LE, Roemer FW, Goud A, Guermazi A. Imaging review of subscapularis tendon and rotator interval pathology. Radiol Res Pract. (2022) 2022:4009829. doi: 10.1155/2022/4009829
9. Baverel L. Subscapularis tendon tears: Classification, diagnosis and repair, in recent advances in arthroscopic surgery. IntechOpen (2018).
10. Ek ET, Perret MC, Borbas P. Arthroscopic knotless repair of complete full-thickness tears of the subscapularis tendon through a single portal. Arthrosc Tech. (2020) 9(4):e439–43. doi: 10.1016/j.eats.2019.11.015
11. Khil EK, Choi JA, Lee E, Oh JH. Subscapularis (SSC) tendon tears: diagnostic performance and reliability of magnetic resonance arthrography (MRA) with arthroscopic correlation and comparison with clinical tests. Skeletal Radiol. (2021) 50(8):1647–55. doi: 10.1007/s00256-020-03697-1
12. Jung JY, Jee WH, Chun CW, Kim YS. Diagnostic performance of MR arthrography with anterior trans-subscapularis versus posterior injection approach for subscapularis tendon tears at 3.0 T. Eur Radiol. (2017) 27(3):1303–11. doi: 10.1007/s00330-016-4467-3
13. Oh DK, Yoon YC, Kwon JW, Choi SH, Jung JY, Bae S, Yoo J. Comparison of indirect isotropic MR arthrography and conventional MR arthrography of labral lesions and rotator cuff tears: a prospective study. Am J Roentgenol. (2009) 192(2):473–9. doi: 10.2214/AJR.08.1223
14. Choo HJ, Lee SJ, Kim OH, Seo SS, Kim JH. Comparison of three-dimensional isotropic T1-weighted fast spin-echo MR arthrography with two-dimensional MR arthrography of the shoulder. Radiology. (2012) 262(3):921–31. doi: 10.1148/radiol.11111261
15. Lee JH, Yoon YC, Jee S, Kwon JW, Cha JG, Yoo JC. Comparison of three-dimensional isotropic and two-dimensional. Conventional indirect MR arthrography for the diagnosis of rotator cuff tears. Korean J Radiol. (2014) 15(6):771–80. doi: 10.3348/kjr.2014.15.6.771. Epub 2014 Nov 7. PMID: 25469089; PMCID: PMC4248633.25469089
16. Saremi H, Yousefi S, Rastgari S, Seif Rabiei M. Accuracy of magnetic resonance imaging for subscapularis tendon tear comparison with arthroscopy. Adv Hum Biol. (2019) 9(3):236–40. doi: 10.4103/AIHB.AIHB_16_19
17. Atinga A, Dwyer T, Theodoropoulos JS, Dekirmendjian K, Naraghi AM, White LM. Preoperative magnetic resonance imaging accurately detects the arthroscopic comma sign in subscapularis tears. Arthrosc J Arthrosc Relat Surg. (2021) 37(10):3062–9. doi: 10.1016/j.arthro.2021.04.040
18. Lee JH, Rhyou IH, Ahn KB. Prediction of the anterior shoulder pain source by detecting indirect signs for partial articular subscapularis tendon tears through conventional magnetic resonance imaging. Knee Surg Sports Traumatol Arthrosc. (2021) 29(7):2297–304. doi: 10.1007/s00167-020-06259-z
19. Gyftopoulos S, O' Donnell J, Shah NP, Goss J, Babb J, Recht MP. Correlation of MRI with arthroscopy for the evaluation of the subscapularis tendon: a musculoskeletal division’s experience. Skeletal Radiol. (2013) 42(9):1269–75. doi: 10.1007/s00256-013-1669-5
20. Malavolta EA, Assunção JH, Guglielmetti CL, de Souza FF, Gracitelli ME, Bordalo-Rodrigues M, et al. Accuracy of preoperative MRI in the diagnosis of subscapularis tears. Arch Orthop Trauma Surg. (2016) 136(10):1425–30. doi: 10.1007/s00402-016-2507-8
21. Matsushita R, Yokoya S, Negi H, Matsubara N, Akiyama Y, Adachi N. Evaluation of subscapularis tendon tears of the anterosuperior aspect using radial-sequence magnetic resonance imaging. JSES Int. (2022) 6(1):97–103. doi: 10.1016/j.jseint.2021.08.005. PMID: 35141682; PMCID: PMC8811407
22. Bartsch M, Greiner S, Haas NP, Scheibel M. Diagnostic values of clinical tests for subscapularis lesions. Knee Surg Sports Traumatol Arthrosc. (2010) 18(12):1712–7. doi: 10.1007/s00167-010-1109-1
23. Somerville LE, Willits K, Johnson AM, Litchfield R, LeBel ME, Moro J, et al.. Clinical assessment of physical examination maneuvers for rotator cuff lesions. Am J Sports Med. (2014) 42(8):1911–9. doi: 10.1177/0363546514538390
24. Lin L, Yan H, Xiao J, He Z, Luo H, Cheng X, et al. The diagnostic value of magnetic resonance imaging for different types of subscapularis lesions. Knee Surg Sports Traumatol Arthrosc. (2016) 24(7):2252–8. doi: 10.1007/s00167-014-3335-4
25. Takeda Y, Fujii K, Miyatake K, Kawasaki Y, Nakayama T, Sugiura K. Diagnostic value of the supine napoleon test for subscapularis tendon lesions. Arthrosc J Arthrosc Relat Surg. (2016) 32(12):2459–65. doi: 10.1016/j.arthro.2016.04.034
26. Yoon JS, Kim SJ, Choi YR, Lee W, Kim SH, Chun YM. Medial subluxation or dislocation of the biceps on magnetic resonance arthrography is reliably correlated with concurrent subscapularis full-thickness tears confirmed arthroscopically. BioMed Res Int. (2018) 2018. doi: 10.1155/2018/2674061
27. Narasimhan R, Shamse K, Nash C, Dhingra D, Kennedy S. Prevalence of subscapularis tears and accuracy of shoulder ultrasound in pre-operative diagnosis. Int Orthop. (2016) 40(5):975–9. doi: 10.1007/s00264-015-3043-9
28. Asmar G, Goubier JN, Falcone MO. Improving the detection of subscapularis tears using a specific transverse CT arthrography image. Orthop Traumatol Surg Res. (2020) 106(6):1107–11. doi: 10.1016/j.otsr.2020.04.016
29. Martetschlager F, et al. A classification for partial subscapularis tendon tears. Knee Surg Sports Traumatol Arthrosc. (2021) 29(1):275–83. doi: 10.1007/s00167-020-05989-4
30. Yoo JC, Rhee YG, Shin SJ, Park YB, McGarry MH, Jun BJ, et al. Subscapularis tendon tear classification based on 3-dimensional anatomic footprint: a cadaveric and prospective clinical observational study. Arthroscopy. (2015) 31(1):19–28. doi: 10.1016/j.arthro.2014.08.015
31. Lädermann A, Collin P, Zbinden O, Meynard T, Saffarini M, Chiu JC. Diagnostic accuracy of clinical tests for subscapularis tears: a systematic review and meta-analysis. Orthop J Sports Med. (2021) 9(9):23259671211042011. doi: 10.1177/23259671211042011. PMID: 35146034; PMCID: PMC8822023.
32. Farooqi AS, Lee A, Novikov D, Kelly AM, Li X, Kelly JD 4th, et al. Diagnostic accuracy of ultrasonography for rotator cuff tears: a systematic review and meta-analysis. Orthop J Sports Med. (2021) 9(10):23259671211035106. doi: 10.1177/23259671211035106
33. Malavolta EA, Assunção JH, Gracitelli MEC, Yen TK, Bordalo-Rodrigues M, Ferreira Neto AA. Accuracy of magnetic resonance imaging (MRI) for subscapularis tear: a systematic review and meta-analysis of diagnostic studies. Arch Orthop Trauma Surg. (2019) 139(5):659–67. doi: 10.1007/s00402-018-3095-6
34. Furukawa R, Morihara T, Arai Y, Ito H, Kida Y, Sukenari T, et al. Diagnostic accuracy of magnetic resonance imaging for subscapularis tendon tears using radial-slice magnetic resonance images. J Shoulder Elbow Surg. (2014) 23(11):e283–90. doi: 10.1016/j.jse.2014.03.011
35. Saremi H. Interstitial tear of the subscapularis tendon, arthroscopic findings and technique of repair. Arch Bone Jt Surg. (2016) 4(2):177–80. PMID: 27200399; PMCID: PMC4852047.27200399
36. Malavolta EA, Assunção JH, Guglielmetti CL, de Souza FF, Gracitelli ME, Ferreira Neto AA. Accuracy of preoperative MRI in the diagnosis of disorders of the long head of the biceps tendon. Eur J Radiol. (2015) 84(11):2250–4. doi: 10.1016/j.ejrad.2015.07.031
37. Fama G, Tagliapietra J, Belluzzi E, Pozzuoli A, Biz C, Ruggieri P. Mid-term outcomes after arthroscopic “tear completion repair” of partial thickness rotator cuff tears. Medicina. (2021) 57(1):74. doi: 10.3390/medicina57010074. PMID: 33477332; PMCID: PMC7829759.33477332
38. Cigolotti A, Biz C, Lerjefors E, de Iudicibus G, Belluzzi E, Ruggieri P. Medium-to long-term clinical and functional outcomes of isolated and combined subscapularis tears repaired arthroscopically. Arch Med Sci. (2021) 17(5):1351. doi: 10.5114/aoms.2020.97714
39. Iacobellis C, Berizzi A, Biz C, Camporese A. Treatment of proximal humeral fractures with reverse shoulder arthroplasty in elderly patients. Musculoskelet Surg. (2015) 99(1):39–44. doi: 10.1007/s12306-014-0331-2
Keywords: subscapularis tendon tear, MRI, MR arthrography, ultrasonography, clinical examination, CT arthrography
Citation: Saremi H and seifrabiei M (2023) Subscapularis tendon tear classification and diagnosis: A systemic review and meta-analysis. Front. Surg. 10:916694. doi: 10.3389/fsurg.2023.916694
Received: 1 May 2022; Accepted: 23 January 2023;
Published: 15 March 2023.
Edited by:
Jaimo Ahn, University of Michigan, United States© 2023 Saremi and seifrabiei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hossein Saremi SG9zc2VpbnNhcmVtaS5zaG91bGRlckBnbWFpbC5jb20=
†ORCID Hossein Saremi orcid.org/0000-0002-2914-5110
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.