
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 30 October 2023
Sec. Visceral Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1289941
Objective: To determine the incidence and characteristics of Zuckerkandl's tubercle (ZT), and its relationship with recurrent laryngeal nerve (RLN) and the superior parathyroid gland (SPG) in the setting of total thyroidectomy.
Methods: A total of 421 patients (mean (min-max) age: 45.6 (18–78) years, 76.2% were females) who had total thyroidectomy were included in this prospective single-surgeon thyroidectomy series study. Patient demographics and thyroidectomy indications (benign and malignant) were recorded in each patient. The presence, grade and laterality of ZT, and its relationship with RLN and SPG were recorded during surgery.
Results: Most of the thyroidectomy indications (69.1%) were related to a malignant disease. The ZT was unrecognizable in 41(9.7%) of 421 patients. In 380 patients with identifiable ZT, the grade 2 (46.3%) ZT was the most common finding. Majority of ZTs (92.9%) were unilaterally located (right-sided: 64.9%; left-sided: 35.1%). In majority of the cases (83.2%), the RLN was found to lie medial to ZT. Overall, SPG was identified in close proximity to ZT in 66.6% of patients (Class 2 [0.5–1 cm from ZT] in 46.6% and Class 3 [<0.5 cm from ZT] in 20.0%). SPG was more likely to be identified in close proximity to ZT when the grade of ZT was higher, which was found to be located 0.5–1 cm from the ZT in 56.9% and 42.7% of grade 2 and grade 3 ZTs, respectively, and <0.5 cm from the ZT in 46.1% of grade 3 ZTs.
Conclusion: In conclusion, this prospective single-surgeon thyroidectomy series study indicates the likelihood of localizing the RLN medial to ZT, and the SPG in close proximity to ZT during total thyroidectomy operations. Hence, the ZT can be used as a reliable and constant landmark to localize both the RLN and the SPG during thyroid surgery, which enables minimizing the risk of iatrogenic injury to RLN, while ensuring a parathyroid-sparing thyroidectomy. The thyroid surgeon should have complete knowledge of thyroid gland anatomy and embryogenesis and should follow a careful and meticulous approach particularly for dissections around larger ZTs, given the increased likelihood of SPG and RLN to be in close proximity.
Thyroid surgery mandates the surgeons’ expertise and in-depth knowledge of the surgical anatomy and embryogenesis, due to considerable risk of complications such as injury to the recurrent laryngeal nerve (RLN), superior laryngeal nerve, or the parathyroid glands which may result in profound lifelong consequences for the patients (1–4).
The RLN shows great variability in its thickness, route and distal ramification (5, 6). In addition, rarely it may also be atypical in the form of the non-recurrent laryngeal nerve (NRLN), which occurs at an incidence ranging from 0.3% to 1.6% for the right and approximately 0.04% for the left, as considered to be by far more prone to intraoperative injury than the RLN (5–8). Hence, proper identification and preservation of the RLN and consideration of the potential variations are important for the safety of surgical procedures of the neck (9).
The direct inspection and complete exposure of RLN during thyroidectomy using the crucial anatomical landmarks such as inferior thyroidal artery, the ligament of Berry, thyroid cartilage and the Zuckerkandl's tubercle (ZT), has become the gold standard method to prevent the inadvertent injury to the nerve, while the parathyroid-sparing surgery is a routinely applied procedure in thyroidectomies to prevent the postoperative hypoparathyroidism (3, 4, 10–14).
The ZT, named by the Austrian anatomist Emil Zuckerkandl in 1902, is a posterolateral projection of the thyroid lobes, indicating the point of fusion between the ultimobranchial body and the main median thyroid process formed during the embryogenesis (15–17). ZT presents as a lateral projection from the lateral thyroid lobe with a close relationship to the extra-laryngeal termination of the RLN as well as to the superior parathyroid gland (SPG) (17–21).
Hence, serving a useful anatomical landmark for the location of both the RLN and the SPG, ZT is often described as “friend” of a thyroid surgeon, while its recognition is also considered important to ensure the complete removal of all thyroid tissue during total thyroidectomy (14, 17, 18, 20–26). Nonetheless, there is vast heterogeneity in the incidence, size and laterality of ZT reported in literature and its utility as a landmark in thyroid surgery has not been extensively investigated, particularly in terms of identifying SPG (1, 3, 4, 14, 17, 22, 23, 26).
This prospective single-surgeon study aimed to determine the incidence and characteristics of ZT and its relationship with RLN and SPG in the setting of total thyroidectomy, and thereby to evaluate its utility as a landmark to safely locate both the RLN and SPG during thyroid surgery.
A total of 421 patients (mean (min–max) age: 45.6 (18–78) years, 76.2% were females) who had total thyroidectomy accompanied with intraoperative exposure of RLN and SPG in relation to ZT were included in this prospective single-surgeon thyroidectomy series study conducted at a tertiary care general surgery clinic between June 2023 and June 2024. Patients who underwent thyroidectomy operations other than total thyroidectomy and those without intraoperative identification of RLN and/or SPG were excluded from the study.
The study was conducted in accordance with the ethical principles stated in the “Declaration of Helsinki” and approved by the Uludag University Clinical Research Ethics Committee (Date: 27/09/2019, Protocol No: 2019-15/1).
Patient demographics (age, gender) and thyroidectomy indications (benign and malignant) were recorded in each patient. All thyroidectomy operations were carried out by the same surgeon (E.G.). The presence, grade and laterality of ZT and its relationship with RLN and SPG were recorded during thyroid surgery.
ZT grade was assessed using the grading system described by Pelizzo et al. (18), including Grade 0 (unrecognizable), Grade 1 (slight thickening of lateral edge of thyroid lobe), Grade 2 (less than 1 cm) and Grade 3 (more than 1 cm). The laterality of ZT was recorded in those classified as Grade I–III (recognizable) ZTs (Figure 1).
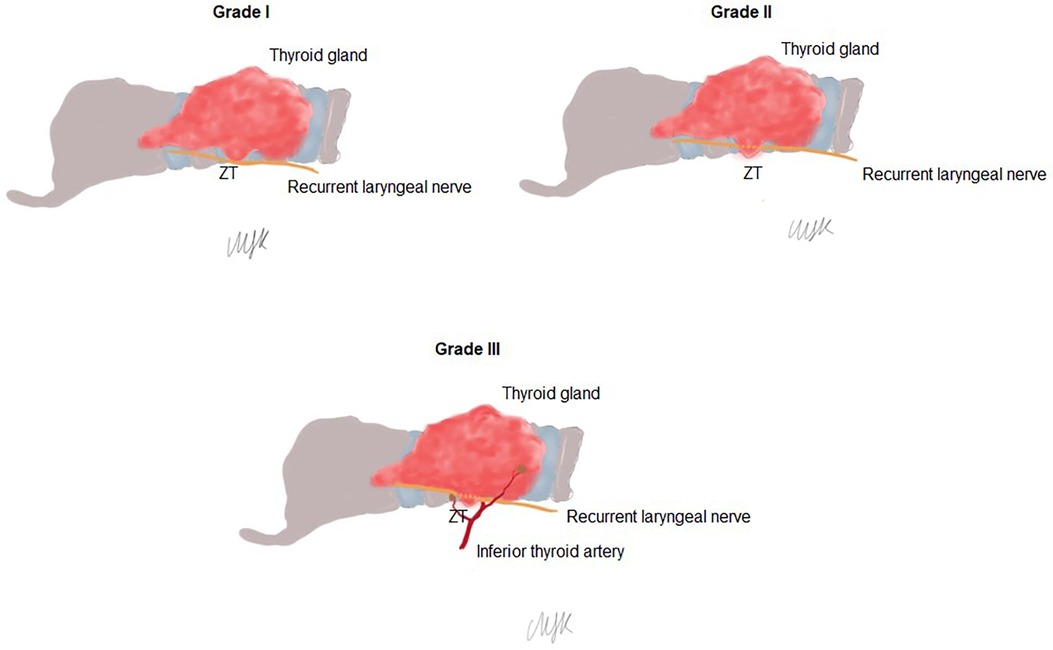
Figure 1. Grading of to Zuckerkandl's tubercle (ZT): Grade 1 (slight thickening of lateral edge of thyroid lobe), Grade 2 (less than 1 cm) and Grade 3 (more than 1 cm).
The running pathway of the RLN relative to ZT area was classified as medial to ZT, lateral to ZT and posterior to ZT.
The relationship between SPG and ZT was assessed using the classification system described by Prakash et al. (17). The position of SPG relative to ZT was categorized as Class 0 (2 cm from the ZT), Class 1 (1–2 cm from the ZT), Class 2 (0.5–1 cm from the ZT) and Class 3 (<0.5 cm from the ZT) (17) (Figure 2).
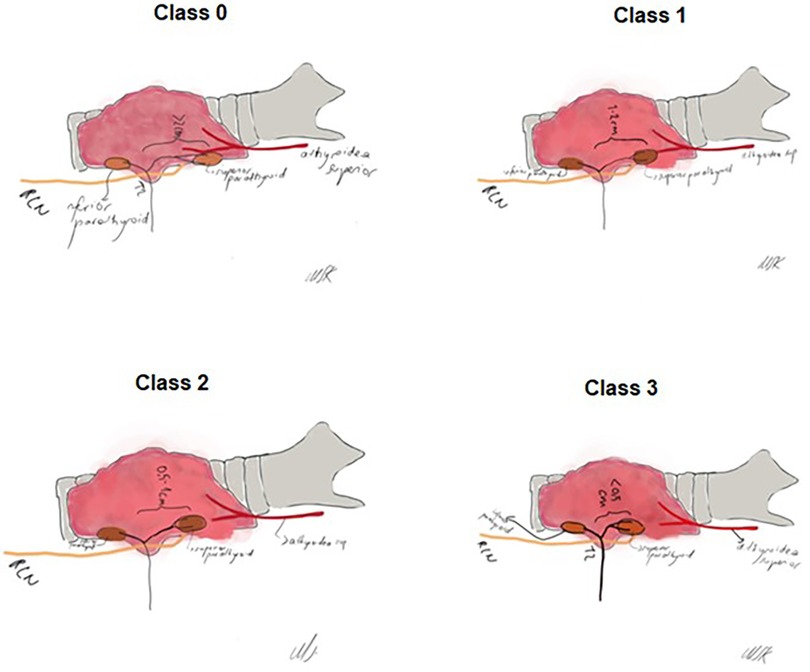
Figure 2. The course and position of superior parathyroid gland relative to Zuckerkandl's tubercle (ZT) as an anatomical landmark. Class 0 (2 cm from the ZT), Class 1 (1–2 cm from the ZT), Class 2 (0.5–1 cm from the ZT) and Class 3 (<0.5 cm from the ZT).
Statistical analysis was performed using IBM SPSS Statistics (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, version 22.0. Armonk, NY: IBM Corp). Descriptive statistics were reported including means and ranges for continuous variables and percentages for categorical variables. Data were expressed as mean (minimum–maximum) and percent (%) where appropriate.
Mean age of patients was 45.6 years (range, 18–78 years), 320 (76.2%) of 421 patients were females. Most of the thyroidectomy indications (69.1%) were related to malignant disease including papillary carcinoma in 54.9% of cases (Table 1).
The ZT was unrecognizable in 41 (9.7%) of 421 patients. In 380 patients with identifiable ZT, grade 2 (46.3%) ZT was the most common finding, followed by the grade 1 (22.8%) and grade 3 (21.1%) ZTs (Table 2, Figure 3).
Majority of ZTs (92.9%) were unilaterally located (right-sided: 64.9%; left-sided: 35.1%), while only 7.1% of ZTs were found to be bilateral (Table 2).
In majority of the cases the RLN was found to lie medial to ZT (83.2%), followed by lateral (12.7%) and posterior (3.9%) positions.
Overall, SPG was identified in close proximity to ZT in 66.6% of patients, including Class 2 (0.5–1 cm from ZT) pattern in 46.6% of patients and Class 3 (<0.5 cm from ZT) pattern in 20.0% of patients (Table 3, Figure 4).
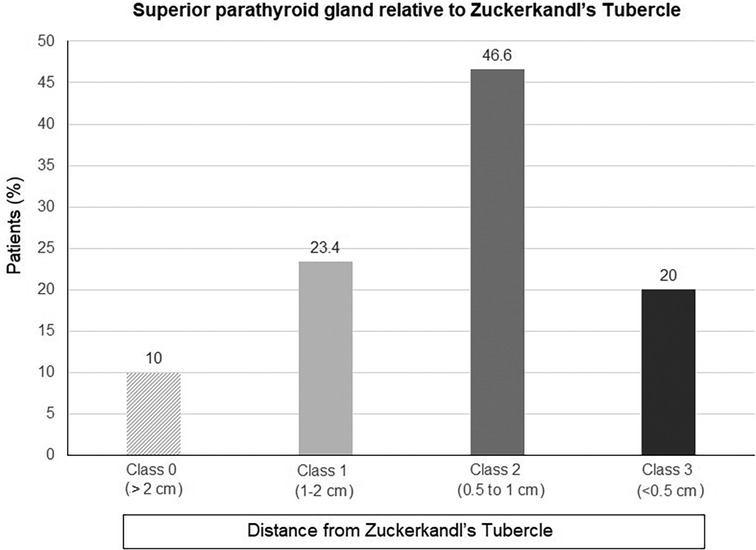
Figure 4. The relation between superior parathyroid gland and Zuckerkandl's tubercle in total thyroidectomy patients.
SPG was more likely to be identified in close proximity to ZT when the grade of ZT was higher. Accordingly, SPG was found to be located 0.5–1 cm from the ZT in 56.9% and 42.7% of grade 2 and grade 3 ZTs, respectively, and to be <0.5 cm from the ZT in 46.1% of grade 3 ZTs (Table 3, Figure 5).
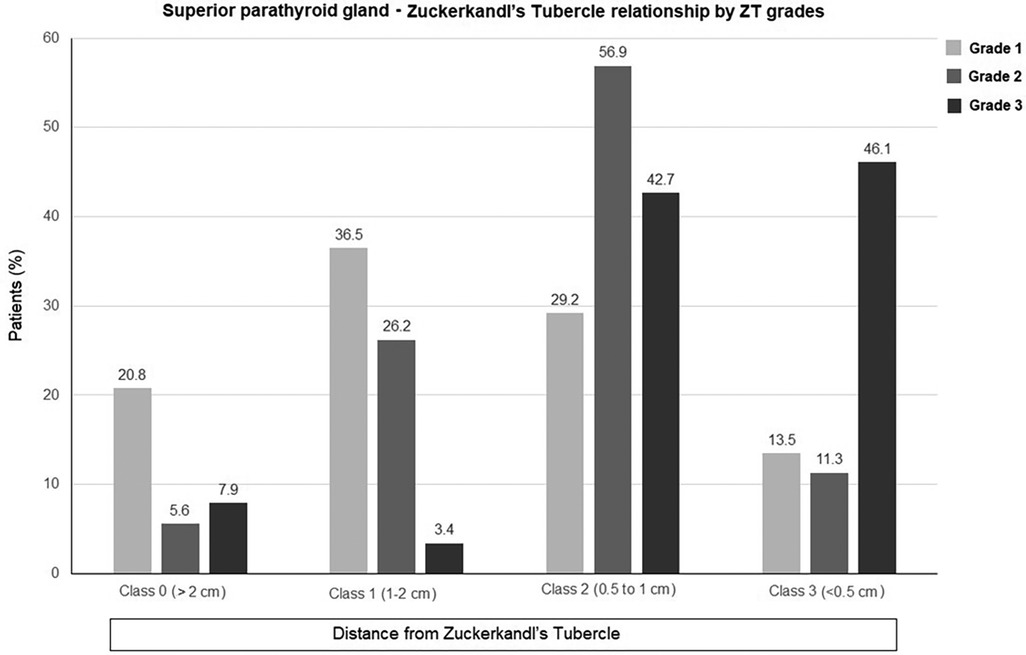
Figure 5. The relation between superior parathyroid gland and Zuckerkandl's tubercle by Zuckerkandl's tubercle grading in total thyroidectomy patients.
This prospective series of total thyroidectomies revealed that ZT was recognizable in majority of patients, as a landmark for locating both the SPG and RLN during the operation. ZT was predominantly unilateral with a predilection of a right-sided location in most of cases, and considered to be grade 2 in nearly half of patients. RLN was found to lie medial to ZT primarily. SPG was found to be in close proximity to ZT in most of patients, and the possibility of locating it nearby the ZT was increased by the advanced grade of ZT.
There is vast heterogeneity in the incidence of ZT reported in literature, which ranges from 7.0% to 90% in different thyroidectomy series depending on the geographical, genetic or ethnic factors as well as the use of accurate methodology in searching ZT during thyroidectomy (14, 17, 22, 23, 27–30). In our series, ZT was recognizable in majority (90%) of cases supporting its consideration of a constant landmark in locating RLN and SPG (14, 22, 23). Notably, in line with consistently reported predominance of grade 1–2 ZTs (18%–90%), nearly half of ZTs identified in our patients were grade 2 (<1 cm), which seems to emphasize the necessity for the surgeon's meticulous seeking and active effort to recognize ZT during the dissection (16, 17, 20, 21, 22, 23, 30–32).
In fact, the size of ZT is considered to be dependent not only on the amount of remnant lateral process tissue, but also on the pathology affecting the thyroid (17, 30, 33). The grade 3 ZT, with a reported incidence of 14% to 55% in thyroidectomy series, is suggested to be more commonly seen in enlarged thyroid glands with multinodular goitre, and considered to be a factor that can affect the completeness of thyroidectomy especially in less-experienced hands (14, 18, 20–24, 30). In this regard, the incidence of grade 3 ZTs (21.1%) in our patients seems consistent with the predominance of thyroidectomies performed for the malignant rather than benign indications in our series.
The predominantly unilateral location of ZT along with a two-fold higher incidence of right-sided vs. left-sided ZT (64.9% vs. 35.1%) in our patients support the data from previous thyroidectomy series indicated unilateral location of ZT in majority of patients along with a higher incidence on the right side (17, 21, 23, 26, 30–32). Likewise, in a series of 173 thyroid lobectomies from Turkey, ZT was reported to be recognizable in 73.4% of cases (grade 2 in 53.2%), and to be detected more frequently on the right vs. left side (78.2% vs. 68.6%) (17). In another study from Turkey in total and hemithyroidectomy series of 60 and 40 patients, respectively, ZT was identified in 66% of patients, and more commonly on the right vs. left side (61% vs. 38%) (21). The embryological difference of the two sides in relation to pharyngeal arches is considered to account for the more common presence of ZT on the right side, while the right-sided TZ is also suggested to be more consistently present in the setting of total thyroidectomy rather than the thyroid lobectomy (17, 32).
Theoretically, the ZT is considered to separate the parathyroid glands into the superior parathyroids and inferior parathyroids, and thus to serve as a pointer to SPG in thyroid surgery practice (18, 20, 30). In the current study, SPG was found to be in close proximity to ZT in most of patients, and the possibility of a closer relationship increased by the advanced grade of ZT. Similarly, in a study with 30 total thyroidectomy patients (10 with malignancies), SPG was found to be closely associated with ZT in majority of cases along with a strong relationship between the proximity of two structures and the ZT grade, indicating that the higher the grade of ZT, the closer the SPG to ZT (22). Also, in a study with 325 thyroidectomy patients (315 with malignancies), the authors noted that the smaller the size of ZT, the greater the distance between ZT and SPG (14).
Knowing that the SPG is more likely to be located in close proximity to a larger ZT seems to be a valuable information enabling the surgeon to take extra care when performing dissection around a larger grade ZT to preserve SPG (14, 22). Besides having a close proximity to the SPG, the larger ZT is also considered to make surgical dissection challenging at posterior site of the lateral lobes around the RLN and the inferior thyroid artery (21, 34).
The position of RLN relative to ZT in our patients support that RLN presents medial to ZT in majority of cases (80%–90%) and lies laterally in up to 10% (17, 20–22, 31, 35). Hence, ZT is considered a constant landmark pointing to the RLN, allowing easy identification of the nerve before it turns below the inferior cricothyroid articulation, if a careful and meticulous dissection is carried out around the ZT (17, 18, 23).
Majority of ZTs were unilaterally located in our series and was right-sided in most of cases. Nonetheless, ZT is considered a useful landmark to identify RLN bilaterally in studies reporting a higher incidence of bilateral ZTs (15%–25%, or even up to 90%) and/or equal incidence of right-sided and left-sided ZTs (14, 20–23). In addition, it should be noted that in thyroidectomies performed for malignant indications, RLN isolation may be challenging if the tumor extends to the ZT.
Albeit not detected in our series, NRLN is considered a rare but important anatomic variant associated with the five to six times higher risk of permanent nerve lesions in thyroid surgery (5, 6, 8). Indeed, the use of intraoperative neuro-monitoring (IONM) as an adjunct visual identification in thyroid surgery has been recommended, given that it allows the surgeon to recognize and differentiate true branches of RLN from sympathetic anastomoses, as well as the NRLN, during surgery (8, 36).
Overall, our findings indicate the utility of ZT as a reliable and constant anatomical landmark pointing to the RLN and the SPG during thyroidectomy, enabling to minimize the risk of inadvertent injury to the RLN as well the parathyroid injury (14, 17, 18, 21–27, 37). The careful and meticulous dissection around the tubercle thorough knowledge of the anatomy and embryogenesis of the thyroid gland is mandatory for safety of thyroid operations, given that the constant relationship of ZT with RLN and SPG may also cause a potential hazard for nerve and gland, or the presence a large ZT may also increase the risk insufficient surgery and complications, in the hands of inexperienced surgeons (1, 17, 18, 20, 21, 38, 39).
In conclusion, this prospective single-surgeon thyroidectomy series study indicates the likelihood of localizing the RLN medial to ZT, and the SPG in close proximity to ZT during total thyroidectomy operations. Hence, the ZT can be used as a reliable and constant landmark to localize both the RLN and the SPG, which enables minimizing the risk of iatrogenic injury to RLN while ensuring a parathyroid-sparing surgery with shorter operative time. Importantly, thyroid surgeons should have complete knowledge of thyroid gland anatomy and embryogenesis and should follow a careful and meticulous approach particularly for dissections around larger ZTs, given the increased likelihood of the SPG and the RLN to be in close proximity.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The Uludag University Clinical Research Ethics Committee (Date:27/09/2019, Protocol No: 2019-15/1). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
The author confirms being the sole contributor of this work and has approved it for publication.
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
The author would like to thank Melike Sema Kocbey for her valuable technical support for the preparation of illustrations.
The author declares that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Bhargav PR. Salient anatomical landmarks of thyroid and their practical significance in thyroid surgery: a pictorial review of thyroid surgical anatomy (revisited). Indian J Surg. (2014) 76:207–11. doi: 10.1007/s12262-013-0856-x
2. Christou N, Mathonnet M. Complications after total thyroidectomy. J Visc Surg. (2013) 150:249–56. doi: 10.1016/j.jviscsurg.2013.04.003
3. Patra A, Asghar A, Chaudhary P, Ravi KS. Identification of valid anatomical landmarks to locate and protect recurrent laryngeal nerve during thyroid surgery: a cadaveric study. Surg Radiol Anat. (2023) 45:73–80. doi: 10.1007/s00276-022-03054-y
4. Stefanou CK, Papathanakos G, Stefanou SK, Tepelenis K, Kitsouli A, Barbouti A, et al. Surgical tips and techniques to avoid complications of thyroid surgery. Innov Surg Sci. (2022) 7:115–23. doi: 10.1515/iss-2021-0038
5. Toniato A, Mazzarotto R, Piotto A, Bernante P, Pagetta C, Pelizzo MR. Identification of the nonrecurrent laryngeal nerve during thyroid surgery: 20-year experience. World J Surg. (2004) 28:659–61. doi: 10.1007/s00268-004-7197-7
6. Iorgulescu R, Bistriceanu I, Badanoiu D, Calin C, Capatana C, Iordache N. Non-recurrent inferior laryngeal nerve: case report and review of the literature. J Med Life. (2014) 4(Spec Iss 4):90–4.
7. Toniato A, Merante Boschin I, Pagetta C, Casalide E, Pelizzo M. A “pilot light” of the right non-recurrent laryngeal nerve, una spia del nervo non-ricorrente destro, surgical pathology, department of medical and surgical sciences, university of Padua, Italy. Acta Otorhinolaryngol Ital. (2010) 30:107–9.20559482
8. Guerreiro S, Lamas M, Candeias H, Eusébio R, Rocha V. The non-recurrent laryngeal nerve: an anatomical “trap”. Rev Port Endocrinol Diabetes Metab. (2014) 9:84–7. doi: 10.1016/j.rpedm.2014.05.001
9. Thomas AM, Fahim DK, Gemechu JM. Anatomical variations of the recurrent laryngeal nerve and implications for injury prevention during surgical procedures of the neck. Diagnostics (Basel). (2020) 10:670. doi: 10.3390/diagnostics10090670
10. Ngo Nyeki AR, Njock LR, Miloundja J, Evehe Vokwely JE, Bengono G. Recurrent laryngeal nerve landmarks during thyroidectomy. Eur Ann Otorhinolaryngol Head Neck Dis. (2015) 132:265–9. doi: 10.1016/j.anorl.2015.08.002
11. Mohebati A, Shaha AR. Anatomy of thyroid and parathyroid glands and neurovascular relations. Clin Anat. (2012) 25:19–31. doi: 10.1002/ca.21220
12. Uludağ M, Tanal M, İşgör A. A review of methods for the preservation of laryngeal nerves during thyroidectomy. Sisli Etfal Hastan Tip Bul. (2018) 52:79–91. doi: 10.14744/SEMB.2018.37928
13. Cho JN, Park WS, Min SY. Predictors and risk factors of hypoparathyroidism after total thyroidectomy. Int J Surg. (2016) 34:47–52. doi: 10.1016/j.ijsu.2016.08.019
14. Yun JS, Lee YS, Jung JJ, Nam KH, Chung WY, Chang HS, et al. The Zuckerkandl’s tubercle: a useful anatomical landmark for detecting both the recurrent laryngeal nerve and the superior parathyroid during thyroid surgery. Endocr J. (2008) 55:925–30. doi: 10.1507/endocrj.k08e-132
15. Zuckerkandl E. Nebst bemerkungen uber die epithelkorperchen des menschen. Anat Hefte. (1902) LXI:61–82.
16. Viveka S. Review of surgical anatomy of tubercle of Zuckerkandl and its importance in thyroid surgery. Chrismed J Health Res. (2018) 5:91–5. doi: 10.4103/cjhr.cjhr_107_17
17. Irkorucu O. Zuckerkandl tubercle in thyroid surgery: is it a reality or a myth? Ann Med Surg (Lond). (2016) 7:92–6. doi: 10.1016/j.amsu.2016.03.030
18. Pelizzo MR, Toniato A, Gemo G. Zuckerkandl’s tuberculum: an arrow pointing to the recurrent laryngeal nerve (constant anatomical landmark). J Am Coll Surg. (1998) 187:333–6. doi: 10.1016/s1072-7515(98)00160-4
19. Chevallier JM, Martelli H, Wind P. Surgical discovery of parathyroid glands and the recurrent laryngeal nerve. Application of well known embryological concepts in the operating room. Ann Chir. (1995) 49:296–304. (French).7668792
20. Gauger G, Delbridge LW, Norm P. Incidence and importance of the tubercle of Zuckerkandl in thyroid surgery. Eur J Surg. (2001) 167:249–54. doi: 10.1080/110241501300091363
21. Gurleyik E, Gurleyik G. Incidence and surgical importance of Zuckerkandl’s tubercle of the thyroid and its relations with recurrent laryngeal nerve. ISRN Surg. (2012) 2012:450589. doi: 10.5402/2012/450589
22. Prakash BG, Kamath KS, Rajesh B, Babu AR, Sandhya D. Extended surgical implication of tubercle of Zuckerkandl in total thyroidectomy. Indian J Otolaryngol Head Neck Surg. (2021) 73:147–51. doi: 10.1007/s12070-020-01854-5
23. Irawati N, Vaish R, Chaukar D, Deshmukh A, D'Cruz A. The tubercle of Zuckerkandl: an important landmark revisited. Indian J Surg Oncol. (2016) 7:312–5. doi: 10.1007/s13193-015-0482-0
24. Yalcin B, Poyrazoglu Y, Ozan H. Relationship between Zuckerkandl’s tubercle and the inferior laryngeal nerve including the laryngeal branches. Surg Today. (2007) 37:109–13. doi: 10.1007/s00595-006-3346-y
25. Singh P, Sharma K, Agarwal S. Per operative study of relation of Zuckerkandl tubercle with recurrent laryngeal nerve in thyroid surgery. Indian J Otolaryngol Head Neck Surg. (2017) 69:351–6. doi: 10.1007/s12070-017-1148-8
26. Gil-Carcedo E, Menéndez ME, Vallejo LA, Herrero D, Gil-Carcedo LM. The Zuckerkandl tubercle: problematic or helpful in thyroid surgery? Eur Arch Otorhinolaryngol. (2013) 270:2327–32. doi: 10.1007/s00405-012-2334-7
27. Page C, Cuvelier P, Biet A, Boute P, Laude M, Strunski V. Thyroid tubercle of Zuckerkandl: anatomical and surgical experience from 79 thyroidectomies. J Laryngol Otol. (2009) 123:768–71. doi: 10.1017/S0022215108004003
28. Kaisha WA, Saidi H. Topography of the recurrent laryngeal nerve in relation to the thyroid artery, Zuckerkandl tubercle, and berry ligament in Kenyans. Clin Anat. (2011) 24:853–7. doi: 10.1002/ca.21192
29. Gravante G, Delogu D, Rizzello A, Filingeri V. The Zuckerkandl tubercle. Am J Surg. (2007) 193:484–5. doi: 10.1016/j.amjsurg.2006.06.040
30. Sheahan P, Murphy MS. Thyroid tubercle of Zuckerkandl: importance in thyroid surgery. Laryngoscope. (2011) 121:2335–7. doi: 10.1002/lary.22188
31. Rajapaksha A, Fernando R, Ranasinghe N, Iddagoda S. Morphology of the tubercle of Zuckerkandl and its importance in thyroid surgery. Ceylon Med J. (2015) 60:23–4. doi: 10.4038/cmj.v60i1.7141
32. Mehanna R, Murphy MS, Sheahan P. Thyroid tubercle of Zuckerkandl is more consistenly present and larger on the right: a prospective series. Eur Thyroid J. (2014) 3:38–42. doi: 10.1159/000355823
33. Mirilas P. Grades of Zuckerkandl’s tubercle in normal thyroids. Surg Today. (2007) 37:918; (author reply 919–20). doi: 10.1007/s00595-007-3510-z
34. Freitas CAF, Paroni AF, Santos AN, Silva RJSD, Souza RO, Silva TFD, et al. Can the Zuckerkandl tubercle assist in the location of the inferior laryngeal nerve during thyroidectomies? Rev Col Bras Cir. (2019) 46:e2249. doi: 10.1590/0100-6991e-20192249
35. Pradeep PV, Jayashree B, Harshita SS. A closer look at laryngeal nerves during thyroid surgery: a descriptive study of 584 nerves. Anat Res Int. (2012) 2012:490390. doi: 10.1155/2012/490390
36. Donatini G, Carnaille B, Dionigi G. Increased detection of non-recurrent inferior laryngeal nerve (NRLN) during thyroid surgery using systematic intraoperative neuromonitoring (IONM). World J Surg. (2013) 37:91–3. doi: 10.1007/s00268-012-1782-y
37. Bagadiya P, Damor K. A prospective study: Zuckerkandl tubercle an important anatomical landmark in identification of recurrent laryngeal nerve in thyroid surgery. Int J Surg Sci. (2020) 4:130–3. doi: 10.33545/surgery.2020.v4.i3b.480
38. Koçak S, Aydintuğ S. Zuckerkandl’s tuberculum. J Am Coll Surg. (2000) 190:98–9. doi: 10.1016/s1072-7515(99)00231-8
Keywords: thyroidectomy, Zuckerkandl's tubercle, anatomical landmark, recurrent laryngeal nerve, superior parathyroid gland
Citation: Gurluler E (2023) The use of Zuckerkandl's tubercle as an anatomical landmark in identifying recurrent laryngeal nerve and superior parathyroid gland during total thyroidectomy: a prospective single-surgeon study. Front. Surg. 10:1289941. doi: 10.3389/fsurg.2023.1289941
Received: 6 September 2023; Accepted: 17 October 2023;
Published: 30 October 2023.
Edited by:
Giuseppe Cavallaro, Sapienza University of Rome, ItalyReviewed by:
Mehmet Kılıç, Eskişehir Osmangazi University, Türkiye© 2023 Gurluler. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ercument Gurluler Z3VybHVsZXJAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.