- Department of Cancer Therapy, The Affiliated Hospital of Qingdao University, Qingdao, China
Background: A peripherally inserted central catheter (PICC) is a specialized type of long-term intravenous catheter commonly employed for administering chemotherapy. The operation and management of PICC should exclusively be carried out by trained healthcare professionals equipped with the requisite knowledge of anatomy, procedural technique and patient care. Persistent left superior vena cava (PLSVC) is a vascular malformation which is typically asymptomatic in clinical presentation, almost always identified during invasive surgery or imaging examinations.
Case presentation: Herein, we detailed a case involving a breast cancer patient whose PLSVC was identified during the placement of PICC because of the negative P-wave in electrocardiogram (ECG). Subsequent examination, including chest x-ray imaging, postoperative enhanced CT of the chest, ECG, and consultation with an experienced imaging physician confirmed that the patient's variant type was PLSVC type I. 2160. Removal of the catheter was deemed unnecessary, as the catheter tip was appropriately positioned and no other concomitant cardiovascular malformations were detected.
Conclusion: The PLSVC is a vascular anomaly and is relatively uncommon within the general population. The operator should possess a thorough familiarity with the potential anatomical variations of left superior vena cava, and specialized case profile should be established for patients diagnosed with PLSVC.
Introduction
Cancer treatment approaches continue to evolve and optimize, including operation, chemotherapy, radiation therapy, etc. (1). Among these methods, chemotherapy holds a significant role, often integrated with other treatments to provide a comprehensive strategy. Chemotherapy agents can be administered through diverse routes, including oral administration, intravenous infusion, injections (subcutaneous or intramuscular), or even topical applications (creams or gels). A peripherally inserted central catheter (PICC) stands as a specialized type of long-term intravenous catheter, extensively employed for administering chemotherapy and other medical therapies (2). A PICC provides medium- to long- term central venous access, granting direct entry to larger blood vessels for dispensing chemotherapy agents, fluids, nutrition, and medications.
The operation and management of a PICC should exclusively be carried out by trained healthcare professionals who possess essential expertise in anatomy, procedural technique, and patient care (3). It is utmost importance to understand anatomical abnormality for the operator which can occur arise from genetic factor, developmental issue, congenital condition, or acquired disorder (4). In this context, we presented a case involving the finding of persistent left superior vena cava (PLSVC) during PICC placement.
Case presentation
A 64-year-old female patient was admitted to the hospital due to a 2 cm diameter tumor identified in her right breast. The pathology report from fine-needle aspiration indicated invasive ductal carcinoma in the right breast, grade 2. Subsequently, the patient underwent a successful right breast-conserving surgery along with a standard axillary dissection involving with sentinel node biopsy. The operation was effective and the patient's recovery had been favorable. A PICC placement was scheduled for subsequent postoperative chemotherapy. Prior to the operation, a comprehensive assessment of the patient's blood vessels and blood examination were performed. Throughout the operation, electrocardiogram (ECG) was employed to monitor vital signs and the positioning of the catheter tip. The patient was positioned supine, with the left arm abducted at a 90° angle from the body. Using B-ultrasound guidance, the puncture site on the left basilic vein was identified and marked on the body surface. The distance from the puncture site to the third intercostal space, down to the right sternoclavicular joint, was measured to provide an initial estimate of the catheter length. Following a thorough disinfection of the entire left arm using chlorhexidine and maintaining aseptic conditions, the basilic vein was punctured and the catheter inserted under B-ultrasound guidance. While advancing and retracting the catheter, dynamic monitoring of P-wave changes was conducted on lead II of the ECG. The ECG revealed a distinct deviation from the typical right superior vena cava (SVC) catheterization pattern. Specifically, at around the 34 cm, negative P-waves emerged instead of the expected positive P-waves. As the catheter continued its advance, the amplitude of these negative P-waves gradually intensified, eventually peaking before transitioning into a biphasic pattern with diminishing amplitudes. Around the 45 cm, the negative P-wave phenomenon ceased entirely. This abnormal phenomenon occurred repeatedly with repeated insertions of the catheter (Figure 1). A chest x-ray was taken to reconfirm the tip location and revealed that the catheter was positioned along the left paramediastinal border in proximity to the T8 vertebrae, rather than crossing the midline to access the right SVC (Figure 2). The subsequent postoperative enhanced CT demonstrated that the PLSVC could function normally within the SVC (Figure 3). The correlation of findings from chest x-ray imaging, postoperative enhanced CT, ECG, and consultation with a proficient imaging physician collectively confirmed the patient's specific anatomical variant as PLSVC type. 2160;. The vascular path was as follows: left upper brachial vein—left subclavian vein—PLSVC—CS—RA.
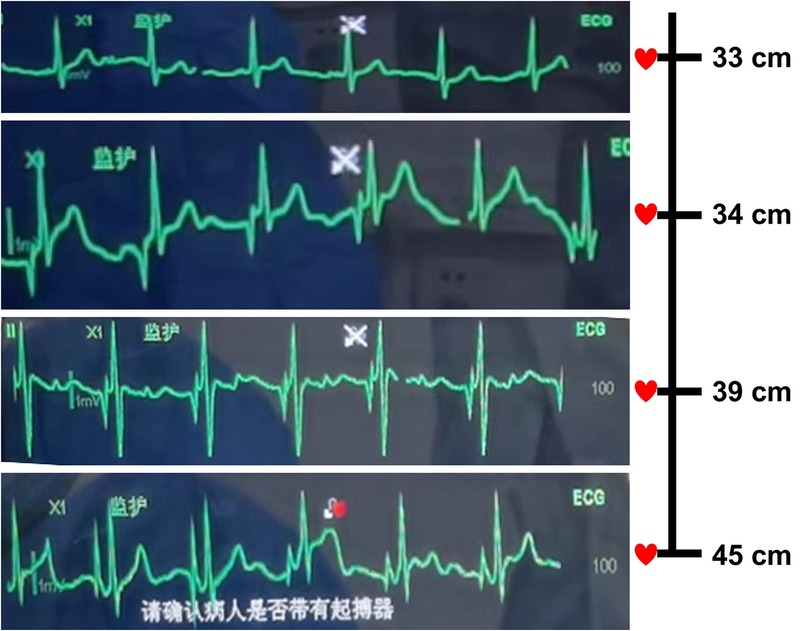
Figure 1. Electrocardiogram manifestation during the process of advancing and retreating the catheter. P-wave changes were dynamically observed on lead II of IC-ECG. IC-ECG showed that, at 33 cm, sinus rhythm with positive P-waves; at about 34 cm, negative P-waves instead of positive P-waves appeared. As the catheter continued to advance, the amplitude of the negative P-wave gradually increased and reached the maximum, and then the P-wave began to become biphasic and the amplitude decreased. At 45 cm, the negative P-wave disappeared completely. This phenomenon occurred repeatedly with repeated insertions of the catheter.
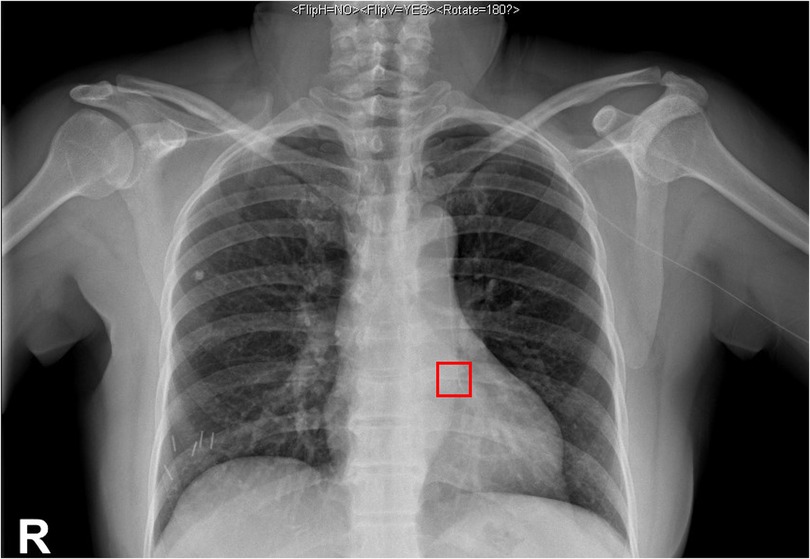
Figure 2. Chest x-ray findings. A chest x-ray was taken to confirm the tip location and showed that the catheter was positioned at the left paramediastinal border near the T8 vertebrae.

Figure 3. The postoperative enhanced CT of the chest. The postoperative enhanced CT of the chest showed that the diameter of the left superior vena cava is 11 mm, and compare the inner diameters of the PLSVC with the superior vena cava to ensure that the PLSVC could function normally.
After the acquisition of informed consent from both the patient and family, we re-adjusted the catheter tip position with the guidance of ultrasound. As the catheter neared the RA, it was gently retracted by approximately 3 cm, ensuring that the PICC's tip was appropriately lodged within the lower third of the left SVC. Moreover, a special case file was established emphasizing the catheter maintenance. The patient and her family received unique health education about the PICC. The patient was requested to visit the PICC specialist Outpatient Department weekly during chemotherapy period. The tip position was verified by x-ray imaging before each chemotherapy. Beside from routine maintenance, the left arm circumference, the length of the external portion of the PICC was measured, and any symptoms of the patient were documented. The patient experienced an uneventful recovery following six cycles of chemotherapy. The dwell time of this PICC was 192 days.
Discussion
Cancer treatment approaches have constantly evolved and been optimized over recent decades, encompassing different conventional and emerging therapies such as operation, chemotherapy, radiation therapy, and more. Among these, chemotherapy, involving the use of drugs to eliminate or impede the growth of cancer cells, stand as an important treatment option for cancer and is frequently integrated with other therapeutic methods to make a comprehensive strategy. Chemotherapy agents can be administered orally (pills or capsules), intravenously, or through other methods such as injections or topical applications. A PICC has been recognized as a favourable protocol for venous access in cancer chemotherapy.
A PICC involves the insertion of a catheter at a peripheral site (such as the arm), which is then advanced until its tip reaches the SVC just above its junction with the RA (2). This procedure can be performed either at the bedside or in a specialized intravenous room by trained individuals, including anesthesiologists, interventional radiologists, pediatricians, or specialized nurses (5). Given its path into the vena cava, a PICC dwelling time can be 390–575 days for infusion and blood sampling (2). By minimizing the need for repeated peripheral venous insertions, a PICC can significantly alleviate patient discomfort, pain, and anxiety. PICC-associated complications, such as thrombosis, stenosis, and infection have also been reported at relatively low levels (6). Therefore, PICC is the preferable choice for achieving intermediate to long-term venous access for medication, fluid therapy, blood sampling, and parenteral nutrition.
It is essential to be well-acquainted with the common anatomical variations in the venous system because they may lead to unusual discoveries either during PICC placement or on subsequent chest imaging. PLSVC is a vascular anomaly, in patients with which less research was reported about PICC implanted. The PLSVC is because of the persistence of the left anterior cardinal vein and the left common cardinal vein during embryonic development, which result in a persistent connection between the left brachiocephalic vein and the RA (7). The prevalence of PLSVC in the general population is approximately 0.3% to 0.5% and up to 10% among individuals with congenital heart disease (Table 1) (8). Typically asymptomatic, this malformation is often discovered incidentally, such as during the positioning of a central venous catheter placed from the left side of the body. In this study, we present a case involving the identification of PLSVC during the placement of PICC. The shared experience of this patient aimed to provide insights into variations in performing PICC for patient with this condition and highlight awareness about the importance of thoroughly examining venous anatomy before the procedure for patient safety and procedure success.
Based on distinct hemodynamic characteristics, PLSVC includes the following types (9, 10). In type I, the PLSVC drains into the RA through the CS, constituting approximately 90% of all PLSVC cases. When the catheter tip is correctly positioned, it can continue to be used because these patients have no other cardiovascular abnormalities (11). In type Ⅱ, similar to type I, the PLSVC also drains into the RA through the CS, however there is an additional patent connection to the left atrium, resulting in a right-to-left shunt. In type Ⅲ, the PLSVC directly drains into the left atrium and leads into right-to-left shunt. In type Ⅳ, CS atresia is observed, where the coronary sinus is blocked or non-existent. PLSVCs of Types II, III, and Ⅳ often exhibit varying degrees of cyanosis due to venous blood entering the left atrium and mixing with arterial blood (12). For patients with these three types of PLSVCs, the catheter should be removed (13). And these patients, who might have symptoms, such as cyanosis, syncope, reduced exercise tolerance, and progressive fatigue because of significant right to left cardiac shunting, should be referred to cardiothoracic surgery to receive treatments in two ways based on anatomy: PLSVC can be ligated if there is an adequate sized bridging vein, and PLSVC can be re-anastomosed to the CS if the bridging vein is not adequate in size or there is no right superior vena cava (9, 14).
For patients who had a recurring negative P-wave in lead Ⅱ of ECG during catheterization or for those patients whose catheter is positioned along the left side of the mediastinum on chest x-ray examination after catheterization, the possibility of PLSVC should be considered. This is attributed to the catheter's enter into the PLSVC and subsequently stimulates electrical impulses in advance, which is opposite to that of lead Ⅱ in body surface ECG; resulting in a negative P-wave appearing in lead II of the body surface ECG (15). And this negative P-wave, with a broad shape, is different from that occurs when the catheter enters the RA in patients with normal right SVC. As the catheter advances further, the amplitude of the negative P-wave diminishes, transitioning the P-wave into a biphasic configuration. This signifies that the catheter has now traversed the CS to enter the RA.
Catheter tip location is one of the primary focal points of the PICC procedure. During the placement of the catheter, when the maximum negative P-wave appears in the ECG, the catheter tip should be gently drawn back and fixed until the P/R ratio is approximately 50% of the maximum negative P-wave. This step aims to position the catheter tip accurately within the middle to lower segment of the PLSVC (16, 17). The PLSVC patient in this study was catheterized following the above-mentioned protocol, and subsequent confirmation of the catheter tip's accuracy was achieved through a chest CT scan conducted post-catheterization. The vital signs and clinical manifestations of the patients should be carefully observed during PICC operation, and timely identification and appropriate management of any complications related to the PICC are paramount. Finally, a special case file should be established to ensure safe PICC use in patients with PLSVC.
Conclusion
In conclusion, the PLSVC is a vascular anomaly and is relatively uncommon within the general population. The operator should possess a thorough familiarity with the potential anatomical variations of left superior vena cava, and specialized case profile should be established for patients diagnosed with PLSVC.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Ethics Committee of The Affiliated Hospital of Qingdao University. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants’ legal guardians/next of kin. Written informed consent was obtained from the minor(s)' legal guardian/next of kin for the publication of any potentially identifiable images or data included in this article.
Author contributions
SXP: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. YLZ: Data curation, Investigation, Methodology, Software, Writing – original draft. FF: Conceptualization, Formal analysis, Funding acquisition, Investigation, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Acknowledgments
We will thank the patient for the great help in this report.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hou S, Hasnat M, Chen Z, Liu Y, , Faran Ashraf Baig MM, Liu F, et al. Application perspectives of nanomedicine in cancer treatment. Front Pharmacol. (2022) 13:909526. doi: 10.3389/fphar.2022.909526
2. Westergaard B, Classen V, Walther-Larsen S. Peripherally inserted central catheters in infants and children—indications, techniques, complications and clinical recommendations. Acta Anaesthesiol Scand. (2013) 57(3):278–87. doi: 10.1111/aas.12024
3. Imburgio S, Johal A, Akhlaq H, Pannu V, Udongwo N, Mararenko A, et al. Persistent left superior vena Cava: an illustrative example. J Cardiothorac Vasc Anesth. (2023) 37(7):1336–7. doi: 10.1053/j.jvca.2023.03.038
4. Tang PT, Chan K. Isolated persistent left superior vena Cava. N Engl J Med. (2022) 386(9):879. doi: 10.1056/NEJMicm2113492
5. Sharpe E, Pettit J, Ellsbury DL. A national survey of neonatal peripherally inserted central catheter (PICC) practices. Adv Neonatal Care. (2013) 13(1):55–74. doi: 10.1097/ANC.0b013e318278b907
6. Naik VM, Mantha SSP, Rayani BK. Vascular access in children. Indian J Anaesth. (2019) 63(9):737–45. doi: 10.4103/ija.IJA_489_19
7. Leibowitz AB, Halpern NA, Lee MH, Iberti TJ. Left-sided superior vena cava: a not-so-unusual vascular anomaly discovered during central venous and pulmonary artery catheterization. Crit Care Med. (1992) 20(8):1119–22. doi: 10.1097/00003246-199208000-00009
8. Ouchi K, Sakuma T, Kawai M, Fukuda K. Incidence and appearances of coronary sinus anomalies in adults on cardiac CT. Jpn J Radiol. (2016) 34(10):684–90. doi: 10.1007/s11604-016-0574-y
9. Sonavane SK, Milner DM, Singh SP, Abdel Aal AK, Shahir KS, Chaturvedi A. Comprehensive imaging review of the superior vena Cava. Radiographics. (2015) 35(7):1873–92. doi: 10.1148/rg.2015150056
10. Nagasawa H, Kuwabara N, Goto H, Omoya K, Yamamoto T, Terazawa A, et al. Incidence of persistent left superior vena Cava in the normal population and in patients with congenital heart diseases detected using echocardiography. Pediatr Cardiol. (2018) 39(3):484–90. doi: 10.1007/s00246-017-1778-3
11. Kobayashi M, Ichikawa T, Koizumi J, Hashimoto J, Yamamuro H, Hara T, et al. Aberrant left brachiocephalic vein versus persistent left superior vena Cava without bridging vein in adults: evaluation on computed tomography. Ann Vasc Dis. (2018) 11(4):535–41. doi: 10.3400/avd.oa.18-00098
12. Ari ME, Dogan V, Ozgur S, Ceylan O, Ertugrul I, Kayali S, et al. Persistent left superior vena cava accompanying congenital heart disease in children: experience of a tertiary care center. Echocardiography. (2017) 34(3):436–40. doi: 10.1111/echo.13447
13. Gustapane S, Leombroni M, Khalil A, Giacci F, Marrone L, Bascietto F, et al. Systematic review and meta-analysis of persistent left superior vena cava on prenatal ultrasound: associated anomalies, diagnostic accuracy and postnatal outcome. Ultrasound Obstet Gynecol. (2016) 48(6):701–8. doi: 10.1002/uog.15914
14. Azizova A, Onder O, Arslan S, Ardali S, Hazirolan T. Persistent left superior vena cava: clinical importance and differential diagnoses. Insights Imaging. (2020) 11(1):110. doi: 10.1186/s13244-020-00906-2
15. Capasso A, Mastroianni R, Passariello A, Palma M, Messina F, Ansalone A, et al. The intracavitary electrocardiography method for positioning the tip of epicutaneous cava catheter in neonates: pilot study. J Vasc Access. (2018) 19(6):542–7. doi: 10.1177/1129729818761292
16. Shafi I, Hassan AAI, Akers KG, Bashir R, Alkhouli M, Weinberger JJ, et al. Clinical and procedural implications of congenital vena cava anomalies in adults: a systematic review. Int J Cardiol. (2020) 315:29–35. doi: 10.1016/j.ijcard.2020.05.017
Keywords: chemotherapy, peripherally inserted central catheter, ECG, persistent left superior vena cava, enhanced CT
Citation: Pan S-X, Zhang Y-L and Fang F (2024) Case Report: Persistent left superior vena cava: an incidental finding during peripherally inserted central catheter placement. Front. Surg. 10:1254937. doi: 10.3389/fsurg.2023.1254937
Received: 9 August 2023; Accepted: 13 November 2023;
Published: 3 January 2024.
Edited by:
Jon Ramm-Pettersen, Oslo University Hospital, NorwayReviewed by:
Francesco Patanè, Azienda Ospedaliera Ospedali Riuniti Papardo Piemonte, ItalyEmil Marian Arbanasi, Emergency County Hospital Targu Mures, Romania
© 2024 Pan, Zhang and Fang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Fang ZmFuZ2xpbmdxZGZ5QGhvdG1haWwuY29t
†This author has first authorship
 Shi-Xiang Pan†
Shi-Xiang Pan† Fang Fang
Fang Fang