
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 15 August 2023
Sec. Cardiovascular Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1236734
Retrograde catheter-induced coronary artery dissection during percutaneous coronary intervention is an exceedingly rare occurrence, and the likelihood of it extending into the aorta is even more uncommon. Typically, surgical treatment involves aortic root replacement combined with coronary artery bypass grafting. However, in this particular case, a meticulous approach was employed. By carefully guiding wires into the true lumens and placing stents in the proximal left main and left anterior descending arteries, the immediate complications were averted by obstructing the retrograde flow in the false lumen. Subsequently, an off-pump coronary artery bypass was performed using the left internal mammary artery to the left anterior descending artery, without the need to manipulate the aorta. This approach resulted in a short operation time and the absence of any other complications.
Advances in cardiovascular interventional technology and stent materials are promoting an increase in the number of percutaneous coronary intervention (PCI) procedures and the number of patients undergoing complex, high risk PCI treatments. Among the catheter-induced coronary artery dissections (CICADs) that can occur during PCI, type A aortic dissection following the retrograde extension of a coronary artery dissection is one of the most life threatening and dramatic complications (1). In general, depending on the patient's condition, treatment typically requires emergency surgical procedures such as aortic root replacement accompanied by coronary artery bypass grafting. Additionally, critical care measures are implemented, including intubation, pacemaker stimulation to address bradycardia, infusion of inotropic drugs, utilization of an intra-aortic balloon pump, and potentially employing extracorporeal life support (2).
The elderly woman who experienced a mid-left anterior descending (LAD) arteries dissection during PCI underwent a successful rescue and repair procedure using a combination of two approaches. The procedure involved a PCI in the left main (LM) to mid-LAD arteries, followed by an emergency off-pump coronary artery bypass graft (OPCAB) utilizing the left internal mammary artery (LIMA) to LAD.
A 78-year-old woman was brought to our hospital with elevated cardiac enzymes. On admission, the electrocardiogram showed no ST elevation, but right bundle branch block; transthoracic echocardiography (TTE) showed moderate to severe hypokinesis at the anterior apex and the apical septal wall. Computed tomography (CT) showed neither aortic dissection nor pericardial effusion. With the diagnosis of non-ST elevation myocardial infarction, diagnostic coronary angiogram was performed and showed no stenosis or thrombus in LM, but diffuse, irregular, up to 85% stenosis from proximal to distal LAD and diffuse, irregular, up to 70% stenosis in the proximal to distal right coronary artery (RCA). When a mid-LAD dissection and retrograde aortic dissection appeared during PCI (Figure 1A), the PCI was carried out from LM to mid-LAD. However, once we confirmed that the balloon and stent would not pass the mid to distal LAD lesion, we proceeded with emergency OPCAB. Perioperative transesophageal echocardiography showed the flap of the proximal aortic dissection (Figure 2A). Median sternotomy was performed under general anesthesia, and there was moderate pericardial adhesion of unknown cause. Cardiopulmonary bypass (CPB) was considered unnecessary due to the absence of retrograde flow to the aorta in the operative field. Because the right and left saphenous veins were both <1 mm in diameter, saphenous vein to RCA bypass graft was not performed. LIMA to LAD OPCAB was performed, and an excellent result was obtained on the flow meter. Operation time was 89 min and anesthesia time was 125 min. The estimated blood loss was 700 ml. Postoperative TTE showed normal left ventricle global systolic function without definite regional wall motion abnormality. Postoperative CT revealed a small remnant intramural hematoma, and the LAD stent was visible (Figure 2B). The postoperative course was good and the patient was discharged from our hospital on postoperative day 9.
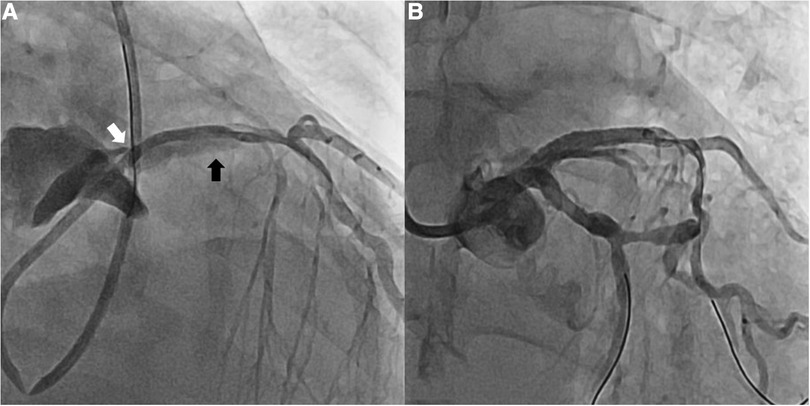
Figure 1. Coronary angiography. (A) Retrograde mid-LAD dissection (black arrow) and propagation to aortic dissection (white arrow) (B) Disappearance of mid-LAD dissection after PCI on LM to proximal LAD. LAD, left anterior descending artery; LM, left main coronary artery; PCI, percutaneous intervention.
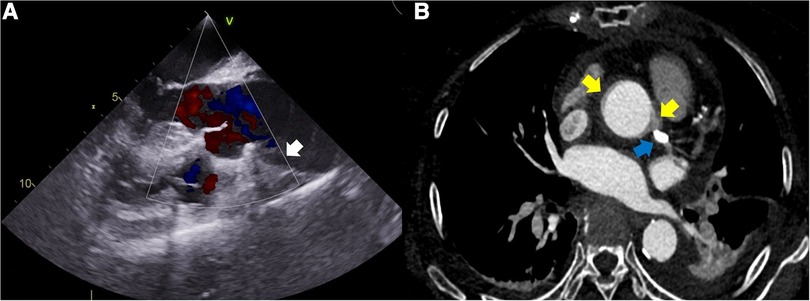
Figure 2. (A) Perioperative transesophageal echocardiography showing the flap of the proximal aortic dissection (white arrow). (B) Postoperative computed tomography showing a small remnant intramural hematoma (two yellow arrows) and the stent in the LAD (blue arrow). LAD, left anterior descending artery.
CICADs are rare but can be severe complications that may arise during PCI (1). While minor dissections are typically easier to handle, dealing with more complex dissections can be quite challenging. The preferred treatment approach involves immediate stenting when the wire is positioned within the true lumen and stent implantation is feasible (3). Globally, the occurrence rate of aortic dissection during PCI is extremely low, measuring less than 0.1%. However, there is a scarcity of available data regarding the natural progression of this condition and its long-term outcomes (4). Rylski and his colleagues reported that immediate surgical treatment, including replacement of the ascending aorta and selective repair of the aortic root and arch, yielded acceptable results after iatrogenic type A aortic dissection, similar to those following naturally occurring aortic dissection (5). Verevkin and his colleagues have also noted that iatrogenic type A aortic dissection should be considered a surgical emergency because of the concern for extension of the dissection (1). However, Costa and his colleagues have recently reported that prompt percutaneous closure of the dissection point of entry was effective in managing iatrogenic LM and aortic root dissection (6). In a case report presented by Hung and his colleagues, they described an iatrogenic aortocoronary dissection that occurred during a routine PCI for stable angina. To address this complication, the team carefully guided wires through the true lumen and successfully placed a stent to seal the dissection flap, leading to the prevention of immediate complications and the resolution of a large mural hematoma in the mid-ascending aorta. Utilizing computed tomography aortography to guide their decisions, they opted for a conservative approach to manage the residual aortic dissection (7). In our case, the patient was of advanced age and we were attempting to manage a retrograde aortic dissection by PCI with stenting from LM to LAD. An emergency OPCAB (LIMA to LAD) was performed on the same day because of severe calcification of the coronary arteries, especially from mid- to distal LAD, and failure to pass a coronary wire into the true lumen for revascularization. The operation went well without any events, and the patient was discharged on postoperative day 9.
In conclusion, the most effective approach to address iatrogenic type A aortic dissection during PCI remains a topic of ongoing debate. The required treatments can encompass a combination of PCI, emergency surgery, and intensive care, which are tailored to the individual patient's condition. Our report presented a detailed case that showcased the successful integration of PCI and emergency OPCAB, aiming to enhance the quality of care and management for patients encountering iatrogenic type A aortic dissection.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
The studies involving humans were approved by Eunpyeong St. Mary's Hospital at the Catholic University of Korea (Referral number: PC22ZESI0301). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
SA, supported by HL and JSC, performed the literature search and wrote the preliminary manuscript. JKK performed the surgery. IK and SA assisted in the surgery. All authors reviewed the manuscript draft and revised it critically on intellectual content. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Verevkin A, von Aspern K, Leontyev S, Lehmann S, Borger MA, Davierwala PM. Early and long-term outcomes in patients undergoing cardiac surgery following iatrogenic injuries during percutaneous coronary intervention. J Am Heart Assoc. (2019) 8(1):e010940. doi: 10.1161/JAHA.118.010940
2. Reinecke H, Fetsch T, Roeder N, Schmid C, Winter A, Ribbing M, et al. Emergency coronary artery bypass grafting after failed coronary angioplasty: what has changed in a decade? Ann Thorac Surg. (2000) 70(6):1997–2003. doi: 10.1016/S0003-4975(00)02172-X
3. Harding SA, Fairley SL. Catheter-induced coronary dissection: keep calm and don't inject. JACC Case Rep. (2019) 1(2):113–5. doi: 10.1016/j.jaccas.2019.07.002
4. Núñez-Gil IJ, Bautista D, Cerrato E, Salinas P, Varbella F, Omedè P, et al. Incidence, management, and immediate- and long-term outcomes after iatrogenic aortic dissection during diagnostic or interventional coronary procedures. Circulation. (2015) 131(24):2114–9. doi: 10.1161/CIRCULATIONAHA.115.015334
5. Rylski B, Hoffmann I, Beyersdorf F, Suedkamp M, Siepe M, Nitsch B, et al. Iatrogenic acute aortic dissection type A: insight from the German registry for acute aortic dissection type A (GERAADA)†. Eur J Cardiothorac Surg. (2013) 44(2):353–9. doi: 10.1093/ejcts/ezt055
6. Costa R, Brochado B, Silveira J, Carvalho Henrique C, Torres S. Successful percutaneous management of iatrogenic left main coronary artery and ascending aorta dissection. JACC: Case Rep. (2022) 4(7):415–7. doi: 10.1016/j.jaccas.2022.02.004
Keywords: LAD dissection, retrograde aortic dissection, percutaneous coronary intervention, catheter-induced coronary artery dissection, off-pump coronary artery bypass graft
Citation: Ahn S, Lee H, Choi JS, Moon Y, Kim I-S, Choi SY and Kang JK (2023) Left anterior descending artery dissection with retrograde aortic dissection during percutaneous coronary intervention: a case report. Front. Surg. 10:1236734. doi: 10.3389/fsurg.2023.1236734
Received: 8 June 2023; Accepted: 2 August 2023;
Published: 15 August 2023.
Edited by:
Vito Domenico Bruno, IRCCS Galeazzi Sant'Ambrogio, ItalyReviewed by:
Anshuman Darbari, All India Institute of Medical Sciences, India© 2023 Ahn, Lee, Choi, Moon, Kim, Choi and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Joon Kyu Kang amtrYW5nQGNhdGhvbGljLmFjLmty
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.