- 1Department of General Surgery, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
- 2Department of Nursing, Shandong Provincial Qianfoshan Hospital, Shandong University, Jinan, China
Background: Prolapsing technique is a type of natural orifice specimen extraction surgery that can overcome the difficulty of precise transection of the distal rectum and subsequent anastomosis in a narrow pelvic space. Currently, protective ileostomy is widely utilized in low anterior resection for low rectal cancer, which may reduce the severe consequences caused by anastomotic leakage. The study aimed to combine the prolapsing technique with a one-stitch method of ileostomy and evaluate the surgical outcomes.
Methods: A retrospective analysis was conducted on patients with low rectal cancer who underwent protective loop ileostomy in laparoscopic low anterior resection between January 2019 and December 2022. The patients were divided into prolapsing technique combined with the one-stitch method of ileostomy (PO) group and traditional method (TM) group, and the intraoperative details and early postoperative outcomes of the two groups were measured.
Results: A total of 70 patients met the inclusion criteria, including 30 patients who underwent PO and 40 patients who underwent the traditional procedure. The PO group had a shorter total operative time than the TM group (197.8 ± 43.4 vs. 218.3 ± 40.6 min, P = 0.047). The time of intestine function recovery in the PO group was shorter than that in the TM group (24.6 ± 3.8 vs. 32.7 ± 5.4 h, P < 0.001). Compared with the TM group, the average VAS score was significantly lower in the PO group (P < 0.001). The incidence of anastomotic leakage in the PO group was significantly lower than that in the TM group (P = 0.034). The operative time of loop ileostomy was 2.0 ± 0.6 min in the PO group, which was significantly less than 15.1 ± 2.9 min in the TM group. Skin irritation was observed in 2 patients in the PO group and 10 patients in the TM group; therefore, there was a significant difference (P = 0.044).
Conclusion: This method is safe and feasible, which reduces the technical difficulty and achieves rapid postoperative recovery with few complications.
Introduction
Low rectal cancer generally refers to rectal cancer whose lower margin is within 5 cm from the dentate line (1). Currently, extra abnormal incision for specimen extraction and double-stapling technique are commonly used in the sphincter-preserving surgery (2). Natural orifice specimen extraction surgery (NOSES) is characterized by the removal of specimen from the natural orifice (anus or vagina), with better cosmetic effect, less postoperative pain, lower risk of incision infection, decreasing incidence of incisional hernia, and shorter length of hospital stay. Transanal prolapsing technique is a type of NOSES. In previous studies of NOSES, there may be risks of abdominal cavity contamination and tumor cell shedding during the process of placement of the anvil of circular stapler in the abdomen and fixation of it to the proximal colonic stump intracorporeally (3). In recent years, diverting ileostomy is widely used to protect high-risk anastomosis. In the conventional ileostomy, a stoma is constructed by using a supporting rod and suturing the intestine's wall transcutaneously or intracutaneously, which is associated with a prolonged duration of operation and a high incidence of stoma-related complications, such as peristomal skin disorders and mucocutaneous separation (4). We describe herein an ideal technique that combined prolapsing technique with the one-stitch method of ileostomy, avoiding abdominal cavity contamination and tumor cell shedding and reducing stoma-related complications, and compare the short-term outcomes with the traditional procedure.
Methods
Patient selection and variables
The patients with rectal cancer who underwent laparoscopic low anterior resection and protective loop ileostomy were collected from Shandong Provincial Qianfoshan Hospital between January 2019 and December 2022. The inclusion criteria were as follows: (1) a diagnosis of rectal adenocarcinoma by preoperative colonoscopic pathological examination, (2) the lower margin of the tumor was within 2–5 cm from the dentate line, (3) no intestinal obstruction or perforation, (4) no distant metastasis, (5) T2–T3 tumor on MRI, (6) rectal wall invasion account for less than 1/2 circumference, and (7) body mass index (BMI) of <30 kg/m2 (1). The exclusion criteria were as follows: (1) patients who underwent abdominoperineal resection or Hartmann's procedure, (2) radiation therapy or chemotherapy was performed before surgery, (3) the laparoscopic procedure was converted to open surgery, and (4) incomplete clinical and pathological data. According to the procedures of specimen extraction and protective loop ileostomy, all patients were divided into two groups, such the prolapsing technique combined with the one-stitch method of ileostomy (PO) group and the traditional method (TM) group.
The preoperative clinical variables of patients, such as sex, age, BMI, tumor distance from the dentate line, diabetes mellitus, and American Society of Anesthesiologists (ASA) grade, were recorded. The postoperative variables included operation time, estimated intraoperative blood loss, intestine function recovery, postoperative complications, and postoperative pain score. The pathologists determined the pathologic stage of rectal cancer and the quality of the total mesorectal excision (TME). A 10-point visual analog scale (VAS) was used to measure the intensity of the pain, with a high score indicating much pain. The VAS scores were collected on the first three postoperative days. The stoma-associated complications, such as necrosis, bleeding, stricture, retraction, prolapse, mucocutaneous separation, skin irritation, and parastomal hernia, were also investigated. Patients were followed up until ileostomy closure or 6 months after initial surgery. All included patients and their families signed a written informed consent. This study was approved by the hospital’s ethics committee. All operations were performed by the same group of surgeons.
Surgical procedures
The patient was placed in Lloyd-Davies position under general anesthesia. The pneumoperitoneum (12–14 mmHg) was performed with the five-hole method. The medial-to-lateral approach was used. The retroperitoneum was incised along the right side of the sigmoid mesentery. Toldt's gap was expanded, and the inferior mesenteric artery and vein were divided after clip placement. The rectum was mobilized to the level of the levator ani muscle, if necessary, to the level of the dentate line through the intersphincteric space.
In the PO group, the sigmoid mesentery was fully dissected, and the rectum approximately 10 cm proximal to the tumor was transected using a linear stapler (Endo GIA 60 mm, Covidien, United States). The anus was fully dilated. A sponge forceps was inserted through the anus to grasp the rectal stump under laparoscopic guidance, and the distal rectum was everted out transanally. The rectum was irrigated with diluted povidone-iodine and was then transected 1 cm–2 cm distally from lower margin of the tumor using a stapler (Endo GIA 60 mm, Covidien, United States, or CONTOUR, Ethicon, United States) (Figure 1A). The rectal stump was delivered back to the pelvic cavity.
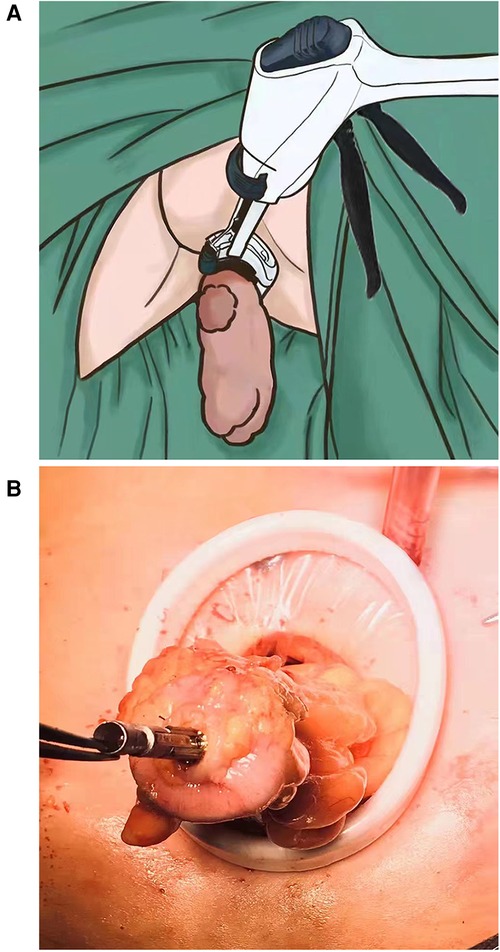
Figure 1. (A) Distal rectum was everted and transected under direct vision. (B) Anvil of circular stapler was placed in proximal stump and fixed with purse-string suture.
A 3.5–4 cm longitudinal rectus abdominis muscle-splitting incision was made in the right lower quadrant according to the appropriate stoma position. A wound retractor (small size; HangTian KaDi Technology R & D Institute, Beijing, China) that provided access to the abdominal cavity was attached at the incision. The colonic stump was exteriorized, the edge of it was removed, and purse-string suture was performed. The anvil of the stapler was placed in the proximal colon and fixed after tightening the purse string around the anvil (Figure 1B). Then, the colonic stump was sent back to the abdominal cavity. By covering the wound retractor by a glove, pneumoperitoneum was re-established. End-to-end anastomosis of the colon and rectum was completed using a circular stapler (EEA28, Covidien, United States) that was inserted through the anus.
The terminal ileum approximately 25–30 cm proximal to the ileocecal junction was exteriorized through the stoma incision and rotated 180° clockwise to ensure that the proximal limb was at the caudal side. A 3-0 polyglactin 910 suture (VCPB864D, Coated VICRYL Plus, Ethicon, United States) was used to sew into the skin 0.5–1.0 cm away from the incision midpoint at one side of the incision (Figure 2A). Then, the suture was passed through the avascular area of the ileal mesentery (Figure 2B) and subsequently sewed out from the opposite side of the incision at an equal distance (Figure 2C). Finally, the suture was passed through the avascular area of the mesentery to the original side (Figure 2D). The suture thread was tightened and knotted to fix the ileal stoma (Figure 2E). The intestinal wall was incised longitudinally about 1–2 cm in length (Figure 3A). The intestinal wall of the stoma would naturally turn over (Figure 3B).
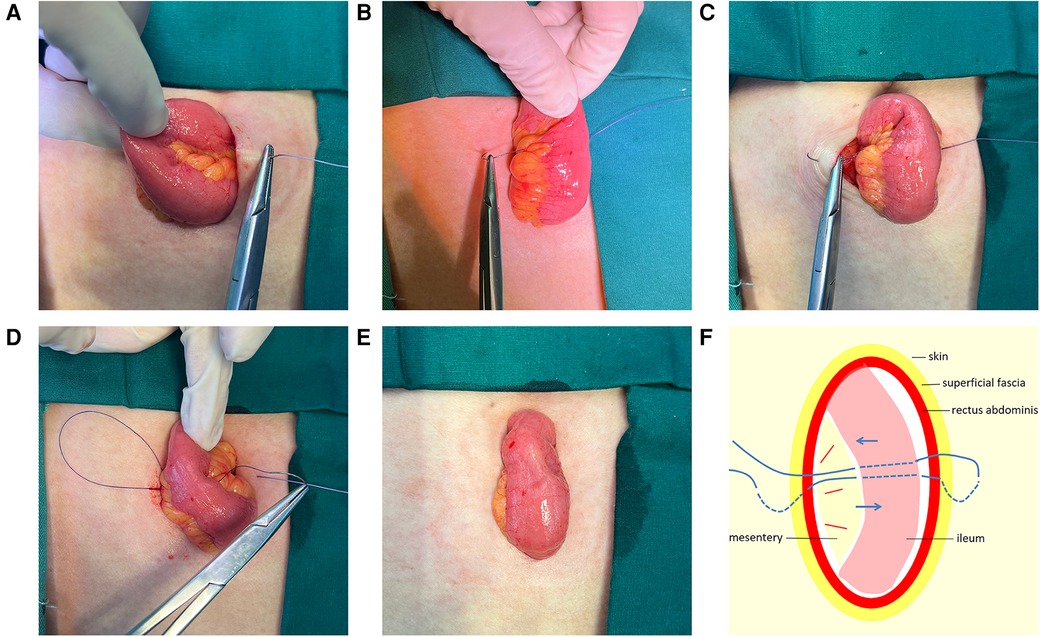
Figure 2. (A) Sew into the skin 0.5–1.0 cm away from the incision midpoint at one side of the incision. (B) Passed through the avascular area of the ileal mesentery. (C) Sew out from the opposite side of the incision at an equal distance. (D) Passed through the avascular area of the mesentery to the original side. (E) Thread was tightened and knotted to fix the ileal stoma. (F) A schematic diagram of the “one-stitch” method.
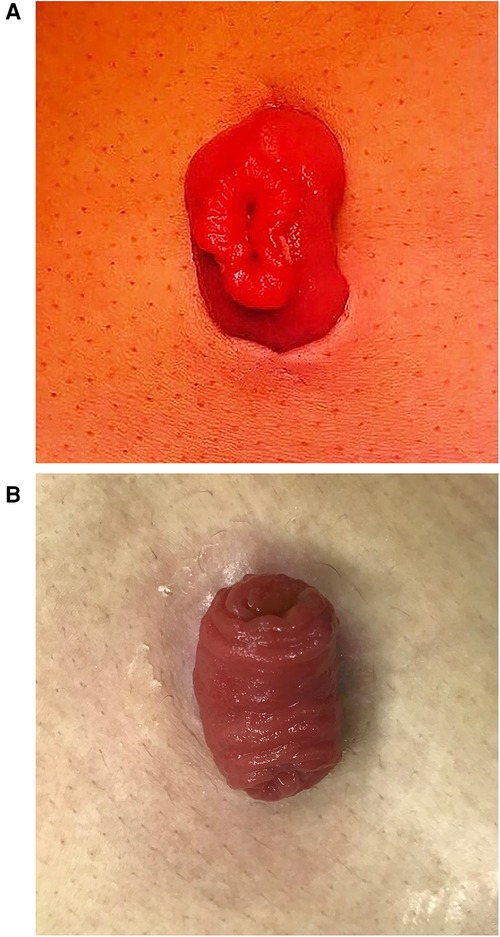
Figure 3. (A) The intestinal wall was incised longitudinally about 1–2 cm in length. (B) The intestinal wall of the stoma naturally turned over (1 month after surgery).
In the TM group, laparoscopic low anterior resection with end-to-end anastomosis was performed with a 5 cm abdominal midline incision for specimen extraction. An appropriate matching incision was established in the right lower quadrant. The seromuscular layer of the ileum was sutured intermittently in a circle with the peritoneum and the anterior rectal sheath using 3-0 polyglactin 910 suture, after which a plastic rod was placed as an ostomy bridge under the loop, half of the circumference of the antimesenteric portion of the bowel was opened, and the cut edges of the bowel were everted and fixed to the skin interrupted. After suturing the mucosal layer of the ileum transcutaneously, a 2–2.5 cm protrusion of the proximal limb was approximately achieved, and the stoma bag was placed.
Statistical methods
The data were presented as a number for categorical variables and the mean ± SD for continuous variables. Categorical variables were compared by using Chi-square analysis or Fisher's exact test, and continuous variables were compared by using Student's t-test. All P values were two-sided, and a P value less than 0.05 indicated a significant difference. All data analysis was performed using SPSS software version 22.0 (IBM Corp).
Results
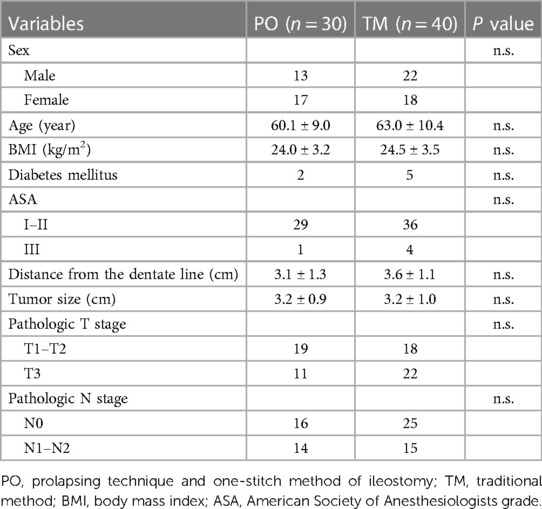
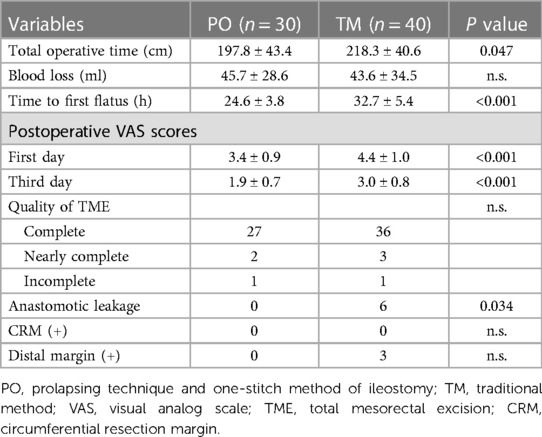
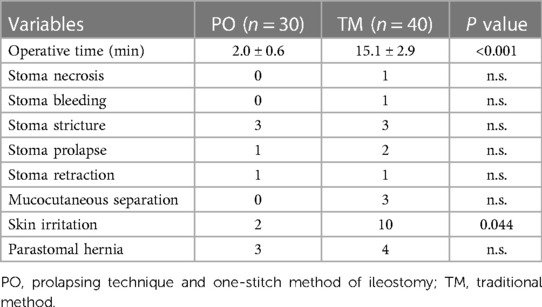
A total of 70 patients met the inclusion criteria, including 30 patients who underwent PO and 40 patients who underwent the traditional procedure. No statistically significant differences were reported between the two groups in terms of preoperative clinical characteristics, such as sex, age, BMI, tumor distance from the dentate line, diabetes mellitus, and ASA grade. No significant differences in intraoperative blood loss, postoperative tumor size, and tumor pathological stage were found between the two groups. The details were shown in Table 1.
The quality of the TME specimen was comparable in both groups. Two groups had no cases of positive circumferential resection margin. No patients with positive distal resection margin were identified in the PO group but four in the TM group, but the difference was not significant. The PO group had a shorter total operative time than the TM group (197.8 ± 43.4 vs. 218.3 ± 40.6 min, P = 0.047). The time of intestine function recovery in the PO group was shorter than that in the TM group (24.6 ± 3.8 vs. 32.7 ± 5.4 h, P < 0.001). Compared with the TM group, the average VAS score was significantly lower in the PO group (P < 0.001). Furthermore, anastomotic leakage (AL) occurred in six patients of the TM group, all of them were cured with conservative treatment. The incidence of anastomotic leakage in the PO group was significantly lower than that in the TM group (P = 0.034). The details are shown in Table 2.
The operative time of loop ileostomy was 2.0 ± 0.6 min in the PO group, which was significantly less than 15.1 ± 2.9 min in the TM group. Skin irritation was observed in 2 patients in the PO group and 10 patients in the TM group, and there was a significant difference (P = 0.044). No differences were found between the two groups when considering other stoma-related complications such as necrosis, bleeding, stricture, retraction, prolapse, mucocutaneous separation, and parastomal hernia (Table 3).
Discussion
Since NOSES was first reported by Franklin et al. (5) in 1993, a variety of new minimally invasive surgical techniques have been emerging. Based on the tumor location and the method for specimen extraction, Guan et al. (3) proposed practical NOSES techniques, including laparoscopic radical resection of low rectal cancer by the transanal prolapsing technique. Since there is no auxiliary incision in the abdominal wall and the abdominal cavity is not exposed, NOSES has a better minimally invasive surgical effects such as less postoperative pain, faster recovery of bowel function, and better cosmetic effects. The absence of auxiliary incision that needs to be sutured can reduce the operation time. Additionally, the prolapsing technique overcomes the difficulties in determining the precise transection line and transection of the rectum close to the anal sphincter in a narrow pelvic space. The everted rectum is transected under direct vision, avoiding multiple-stapler firings and reducing the risk of positive surgical margin.
One of the key technical difficulties of NOSES is the placement of the anvil in the proximal colon. The anvil can be usually inserted into the proximal colon through the rectum. Some surgeons also inserted the anvil into the abdominal cavity via the extended port hole (6) in the right lower quadrant. It is hard to fix the anvil to the proximal colon under total laparoscopy, as excellent skills of operation and team cooperation ability are required. At present, there are many kinds of fixation methods, such as extrusion (3), reverse puncture (7), snare ligation (8), and manual purse-string suture (9). Each method has its unique advantages and disadvantages. In this study, the modified anvil placement was extracorporeally performed by inserting the anvil after extraction of the proximal colon from the ileostomy incision, thus avoiding the risks of abdominal cavity contamination and tumor cell shedding or implantation metastasis during the process of placement of the anvil in the abdomen and fixation of it to the proximal colonic stump intracorporeally. In parallel, the purse-string suture method may lower the risk of anastomotic leakage caused by more intersections of staple lines and reduce the hospitalization costs owing to the reduced use of stapling cartridges. This technique is superior to the laparoscopic purse-string suture or snare ligation method in terms of simple operation and time savings. Moreover, compared with transanally pulling the proximal colon out, there is no need to fully mobilize the sigmoid colon or splenic flexure, which is more suitable for patients with short sigmoid colon or fatty mesosigmoid.
Anastomotic leakage remains the most severe complication of sphincter-preserving surgery for low rectal cancer and was reported to occur in about 10% (10) of patients after rectal cancer surgery. A systematic review and meta-analysis (11) including four RCTs and nine comparative studies with more than 2,000 patients showed that a diverting stoma may lower the rate of AL, additionally reducing the risk of reoperations significantly. The rate of diverting stoma after NOSES for low rectal cancer was even up to 77.2%–100% (6, 12). Patients who conform to the following criteria are encouraged to undergo protective ostomy: (1) patients with preoperative radiotherapy or intestinal obstruction; (2) the distance between the lower margin of the tumor and the anal verge <5 cm, especially <3 cm; and (3) poor patient's general status, including advanced age, malnutrition, hypoproteinemia, preoperative anemia, hypertension, diabetes, and other basic diseases associated with increased risk of AL (13). In this study, the new ostomy technique created a stoma, whose edge was in a shape of “8” via tightening the midpoints of the skin on both sides. The edge of the stoma was in complete contact with the intestinal wall that may reduce the occurrence of mucocutaneous separation. Furthermore, the continuous eversion of the intestinal mucosa after the opening of the stoma made the stoma protrude completely out from the skin in a “fungating” shape. The shape was “large at the top and small at the bottom,” which was beneficial to stoma care by using a smaller perforated stoma chassis. Because the ileum of the stoma was completely positioned in the bag, and the chassis could surround the bottom of the stoma closely, the one-stitch method could reduce the rate of peristomal skin disorders. The one-stitch method of ileostomy facilitated the postoperative care as there was no need of the supporting rod. As a result of the simplified suture process and reducing the number of stoma sutures, the operation time was shortened.
This study has some limitations. First, it was a retrospective single-institute analysis, and the sample size was small. Moreover, the current study design focused on the short-term efficacy, especially perioperative outcomes and stoma-related complications. Anal sphincter function was not preoperatively investigated, functional outcome was not well addressed because all study patients simultaneously underwent loop ileostomy at the time of rectal resection, and follow-up period was short. Third, we did not investigate oncologic outcomes. Due to the limitations of this study, the above conclusions need to be further validated by high-quality prospective controlled study with a large sample and long follow-up.
However, the rectal prolapsing technique is mainly applicable to patients with small tumor size. Routine protective ileostomy is not recommended only if there is a potentially high risk of AL. With the wide application of neoadjuvant chemoradiotherapy and the increase of patients at an early stage, the combination of rectal prolapsing technique and the one-stitch ileostomy could be an option for more cases.
Conclusion
Integration of prolapsing technique and the one-stitch method of ileostomy during laparoscopic low anterior resection is safe and feasible, which can simplify the operation and reduce the technical difficulty. Therefore, it could be an alternative to laparoscopic low anterior resection without the advancement of any special instruments or skills.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of Shandong Provincial Qianfoshan Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XL, YL, and MT collected and analyzed the data and wrote the main parts of the manuscript. XL, JC, and HT designed the study and completed the manuscript. MT provided the ostomy care. All authors contributed to the article and approved the submitted version.
Funding
This project was supported by Shandong Provincial Medicine and Health Science and Technology Development Plan (Grant No. 202004011539).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang X. Natural orifice specimen extraction surgery: colorectal cancer. Singapore: Springer (2018).
2. Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, Stryker SJ, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. (2004) 350(20):2050–9. doi: 10.1056/NEJMoa032651
3. Guan X, Liu Z, Longo A, Cai JC, Tzu-Liang Chen W, Chen LC, et al. International consensus on natural orifice specimen extraction surgery (NOSES) for colorectal cancer. Gastroenterol Rep (Oxf). (2019) 7(1):24–31. doi: 10.1093/gastro/goy055
4. Niu JW, Ning W, Zhou L, Pei DP, Meng FQ, Liu ZZ. Application of preventive flap-placement of terminal ileostomy in laparoscopic radical resection of low rectal cancer. Nat Med J China. (2019) 99(10):750–3. doi: 10.3760/cma.j.issn.0376-2491.2019.10.008
5. Franklin ME Jr., Ramos R, Rosenthal D, Schuessler W. Laparoscopic colonic procedures. World J Surg. (1993) 17(1):51–6. doi: 10.1007/BF01655705
6. Zhuo C, Liang L, Ying M, Li Q, Li D, Li Y, et al. Laparoscopic low anterior resection and eversion technique combined with a nondog ear anastomosis for mid-and distal rectal neoplasms: a preliminary and feasibility study. Medicine (Baltimore). (2015) 94(50):e2285. doi: 10.1097/MD.0000000000002285
7. Akamatsu H, Omori T, Oyama T, Tori M, Ueshima S, Nishida T, et al. Totally laparoscopic low anterior resection for lower rectal cancer: combination of a new technique for intracorporeal anastomosis with prolapsing technique. Dig Surg. (2009) 26(6):446–50. doi: 10.1159/000239761
8. Zhou ZQ, Wang K, Du T, Gao W, Zhu Z, Jiang Q, et al. Transrectal natural orifice specimen extraction (NOSE) with oncological safety: a prospective and randomized trial. J Surg Res. (2020) 254:16–22. doi: 10.1016/j.jss.2020.03.064
9. Saurabh B, Chang SC, Ke TW, Huang YC, Kato T, Wang HM, et al. Natural orifice specimen extraction with single stapling colorectal anastomosis for laparoscopic anterior resection: feasibility, outcomes, and technical considerations. Dis Colon Rectum. (2019) 60(1):43–50. doi: 10.1097/DCR.0000000000000739
10. Hasegawa H, Matsuda T, Arimoto A, Yamashita K, Nishi M, Takase N, et al. Does anastomotic leakage after rectal cancer resection worsen long-term oncologic outcome? Int J Colorectal Dis. (2020) 35(7):1243–53. doi: 10.1007/s00384-020-03577-z
11. Pisarska M, Gajewska N, Małczak P, Wysocki M, Witowski J, Torbicz G, et al. Defunctioning ileostomy reduces leakage rate in rectal cancer surgery-systematic review and meta-analysis. Oncotarget. (2018) 9(29):20816–25. doi: 10.18632/oncotarget.25015
12. Efetov SK, Tulina IA, Kim VD, Kitsenko Y, Picciariello A, Tsarkov PV. Natural orifice specimen extraction (NOSE) surgery with rectal eversion and total extra-abdominal resection. Tech Coloproctol. (2019) 23(9):899–902. doi: 10.1007/s10151-019-02058-y
Keywords: prolapsing technique, ileostomy, rectal cancer, natural orifice specimen extraction surgery, laparoscopy
Citation: Li X, Tian M, Chen J, Liu Y and Tian H (2023) Integration of prolapsing technique and one-stitch method of ileostomy during laparoscopic low anterior resection for rectal cancer: a retrospective study. Front. Surg. 10:1193265. doi: 10.3389/fsurg.2023.1193265
Received: 24 March 2023; Accepted: 16 May 2023;
Published: 31 May 2023.
Edited by:
Hiroki Hashida, Kobe City Medical Center General Hospital, JapanReviewed by:
Mikhail Danilov, A.S. Loginov Moscow Clinical Scientific Centre, RussiaWalter Brunner, Cantonal Hospital St. Gallen, Switzerland
Andreas Shamiyeh, AKh Linz, Austria
© 2023 Li, Tian, Chen, Liu and Tian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hu Tian dGlhbmh1NjU4NUAxNjMuY29t Min Tian bWludGlhbjEwMTZAMTYzLmNvbQ==
 Xiangmin Li
Xiangmin Li Min Tian
Min Tian Jingbo Chen1
Jingbo Chen1 Hu Tian
Hu Tian