- 1Department of Orthopaedic, The Affiliated Taizhou People’s Hospital of Nanjing Medical University, Taizhou, China
- 2Postgraduate School, Dalian Medical University, Dalian, China
- 3Department of Vascular Surgery, The Affiliated Taizhou People's Hospital of Nanjing Medical University, Taizhou, China
Introduction: Pedicle screw fixation (PSF) has been the standard therapy for the treatment of various spinal diseases. Although complications are identified regularly, iatrogenic vascular injury is one of the rare but life-threatening complications. In this literature, we describe the first case of inferior vena cava (IVC) injury during pedicle screw removal.
Case description: A 31-year-old man was treated by percutaneous pedicle screw fixation for an L1 compression fracture. After a year, the fracture healed well and hardware removal surgery was performed. During the procedure, the hardware on the right was removed unremarkably except for the L2 pedicle screw which slipped into the retroperitoneum because of the improper technique. The CT angiogram revealed the screw had breached the anterior cortex of the L2 vertebral body and penetrated the IVC. After multidisciplinary cooperation, the defect of IVC was reconstructed and the L2 screw was removed from the posterior approach in the end.
Result: The patient recovered well and was discharged after 3 weeks without further events. The removal of the contralateral implants was unremarkable at 7 months postoperatively. At the 3-year follow-up, the patient returned to his normal daily activity without any complaints.
Conclusion: Although pedicle screw removal is a rather simple procedure, severe complications may have occurred from this procedure. Surgeons should keep vigilant to avoid the complication noted in this case.
Introduction
The pedicle screw fixation (PSF) has been the standard therapy for the treatment of various spine diseases (1). However, there have been reports on undesired intraoperative and postoperative complications related to PSF (2). Iatrogenic vascular injury is one of the rare but life-threatening complication. Based on the literature, the incidence of large vessel injury caused by pedicle screws is 0.01% (3). Although the majority of pedicle screws related vascular complications occur during the intraoperative period from screw placement, they can also occur in a delayed period from pseudoaneurysm formation (4, 5).
Hardware removal is the most commonly performed orthopedic surgery, the procedure carries risks of unexpected complications (6, 7). According to the reports, the rate of its associated complication was 9.6% in a cohort of recently trained orthopedic surgeons in the United States (8). Although PSF related vessel injuries were well discussed in the literature (9, 10), to our knowledge, there are no reports describing the major vessel injury during pedicle screw removal.
Here, we present a case of inferior vena cava (IVC) injury secondary to the removal of the pedicle screw following percutaneous PSF in treating a thoracolumbar fracture.
Case description
A 31-year-old man was treated by percutaneous PSF for an L1 compression fracture. The implant was required to remove one year after the initial surgery without sign of hardware failure or loosening, and bone healing was achieved according to radiography (Figures 1A,B).

Figure 1. (A,B) anterior-posterior and lateral radiographs 1 year after percutaneous pedicle screw in L1. (C) Intraoperative fluoroscopy was taken and confirmed that the screw migrated anteriorly to the vertebral body. (D) Enhanced CT scanning of the abdomen found that the tip of the right L2 screw indented the IVC and left renal vein without blood extravasation.
Hardware removal surgery was performed in a prone position. During surgery, the caps on the right side was firstly loosened using a remover, and the caps and the rod were removed sequentially, then the pedicle screws of the T12 and L1 were removed unremarkably using the proper screwdriver. However, the removal of the right L2 pedicle screw was unsuccessful. With a limited view of minimal invasive incision, the screwdriver has never been able to fully fit the tail of the screw. After multiple attempts, the screwdriver seemed to fit. To enhance the sense of fit, the surgeon put forwarding pressure on the screw and rotated the screwdriver in a clockwise direction(in a wrong manner). Even worse, he suddenly felt that the screw was pushed into the retroperitoneum.
Intraoperative fluoroscopy was taken and confirmed that the screw migrated anteriorly to the vertebral body (Figure 1C). An endovascular team was emergently consulted. A contrast-enhanced computed tomography (CT) and computed tomography angiogram (CTA) of the abdomen was suggested to assess the extent of vascular injuries. The emergency contrast-enhanced CT and CTA revealed the L2 screw had breached the anterior cortex of the L2 vertebral body and penetrated the IVC but had not caused any extravasation of contrast. (Figure 1D).
The patient was hemodynamically stabilized by fluid resuscitation. Subsequently, a laparotomy was performed in a supine position by a vascular surgeon. The circumference of the IVC wall was evaluated. It was identified that the IVC was traversed, and the bilateral renal veins were also contorted by the screw. After carefully separating the blood vessels from screw, it was found that the IVC was completely punctured and there was a severe crush injury at the transition between the renal vein and the IVC. Vascular control above and below the level of injury was performed, and the screw was slowly backed out (Figure 2A). Finally, the defect of IVC was reconstructed using an artificial graft. (Figure 2B).
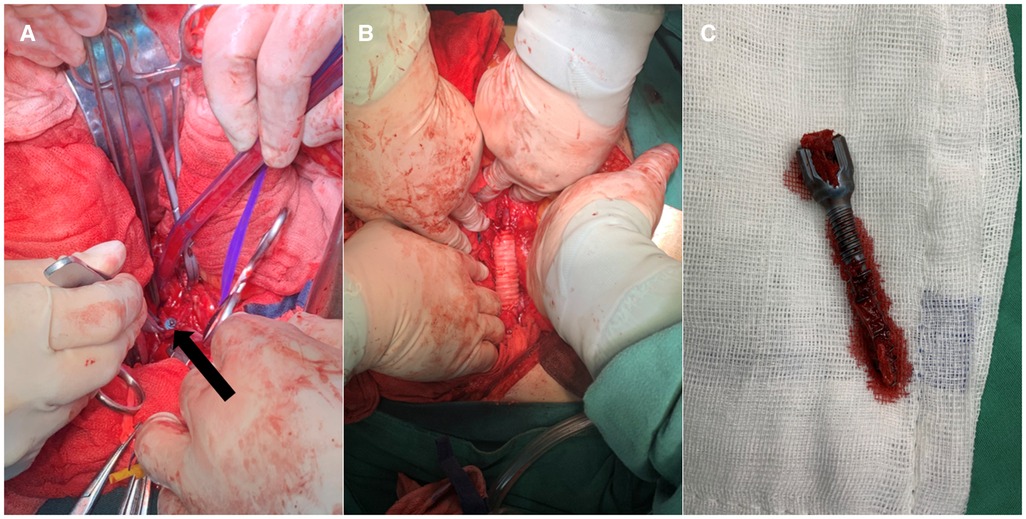
Figure 2. A View of the tip of the screw (black arrow) is exposed by the dissection flap of the IVC. (B) The defect of IVC was reconstructed using an artificial graft. (C) The right L2 pedicle screw was removed in the posterior approach.
Immediately following the abdomen incision was closed, the L2 screw was then removed from the posterior approach (Figure 2C). Considering the general condition of the patient, the removal of the contralateral implants was suspended. At the end of the procedure, he was transferred to the intensive care unit.
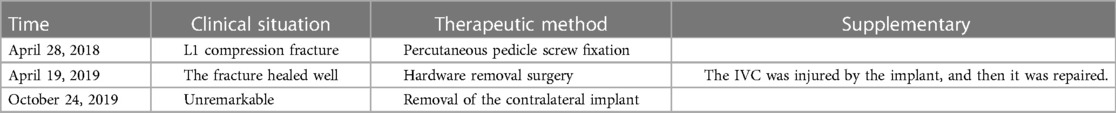
He recovered well and was discharged from our institution after 3 weeks without further event. At 7 months postoperatively visit, the removal of the contralateral implants was done with unremarkable. At the 3-year follow-up, the patient returned to his normal daily activity without any complaints. The diagnosis and treatment process of patient were showed in Table 1.
Discussion
PSF has developed into the standard therapy for the treatment of spine diseases (1). After temporary fixation, removal of screws is planned routinely. Although various complications were reported during pedicle screw removal (8), errant IVC injury is a rare but life-threatening complication. To the best of our knowledge, this is the first report of an IVC injury during pedicle screw removal.
Hardware removal remains a controversial topic in spine surgery after a successful fusion (11). Smits et al. reported that quality of life and patient satisfaction improved after implant removal in 108 patients who successfully treated thoracic lumbar fractures (7). Similarly, Chang-Hoon et al. believed that the segmental angular motion of patients can be restored after the removal of internal fixation, which could improve a series of related clinical symptoms (12). Alanay et al. found that after implant removal the rate of functional improvement and VAS decrease was 84%, and 50% respectively (6). However, in a retrospective study, Stavridis et al. found that only 12% of patients experienced complete remission of symptoms after the removal of pedicle screws (13).
Although whether to remove the pedicle screw was controversial, the procedure was still frequently performed. Its associated unexpected complications were occasionally reported. Crasto et al. reported a case of pneumothorax secondary to the broken bolt cutter jaw entering the pulmonary cavity during removal of hardware performed on the thoracolumbar spine, which resulted in the patient death (14). Vanichkachorn et al. described a case that underwent a potential for aorta injury during unsuccessful broken pedicle screw removal in the thoracolumbar spine (15). Fortunately, the laparotomy approach identified that the tip of the screw was closed to the aorta, and surrounding structures were intact. However, once the vascular injury occurred, fatal consequences to the patient will be faced.
Iatrogenic IVC injury is a rare but life-threatening complication. To our knowledge, there was only three pedicle screw related IVC injuries reported in the literature. Wang et al. reported a case of IVC tear which occurred during posterior spinal fusion surgery (16). The patient underwent emergent exploratory laparotomy, and the torn vessel was repaired, but the patient died after two weeks later due to multiple-organ failure. Yen et al. presented a case with an L-3 pedicle screw pushed into the retroperitoneum and then migrated to IVC (17). A percutaneous endovascular technique was given to successfully retrieve the screw. In 2019, Makino et al. using endovascular treatment successfully managed a case of IVC and lumbar artery injury caused by tap insertion for a pedicle screw during lumbar interbody fusion (18). The latter two iatrogenic injuries have occurred in older patients, and lack of attention to poor bone quality may be the cause of this catastrophic event. In the present case, although bone mineral density examination was not performed, the patient is a 31-year-old young man, and osteoporosis may not be considered. During surgery, with a limited view of minimal invasive incision, the surgeon of a two-year trainee in the field of spinal surgery had difficulties putting the screwdriver bound to the screw end. After multiple attempts, he clockwise turned the screwdriver with forwarding pressure (in a wrong manner), leading to unexpectedly penetrating the anterior wall of the vertebral body and injuring the IVC.
Injury of the vessel was associated with a mortality rate high of 50% due to its catastrophic hemorrhage occurred (19). CTA or digital subtraction angiography (DSA), the excellent options to assess the intact of large blood vessels, have been mentioned as the basis of handle for this kind of issue in the literature (20, 21). After evaluation, it is particularly important to treat it individually. A management algorithm, open vascular surgery or endovascular surgery, has been introduced to make the best clinical decisions for PSF related vessel injuries (22, 23). Direct suture, segmental aortic reconstruction, and endovascular stent graft (ESG) implantation are available options for the treatment of the lesions (24–26). It is important to note that screw removal should be performed in a setting with the capacity for well gaining vascular control. However, maintaining the screw in situ without removal is also an alternative option in certain circumstances. lin et al. reported a case in which the vascular replacement surgery was performed without removing the screw for the stability of the spine (27). A similar case was reported by Saila et al. (28). In addition, Kenneth et al. recommended that surgeons needed to assess the risk of hardware removal for no symptoms patients since they found that no sequelae were caused by the screw that connected to the vessel at a long-term follow-up (29).
Although numerous cases of large vascular injury by implant have been listed, sparse literatures regarding the systematic management tactics for this extremely condition (5, 20, 22–24). After reviewing a large body of literature, the author summarized as follows: Follow-up periodically should be the main manner for implant of adjacent vessels. In addition, the implant involving vascular injury should be removed preventative under the circumstance of safety. Furthermore, the vital signs of patients should be fully monitored during the implantation or removal of internal fixation, and when there is unexplained hemorrhage or even blood pressure drop severely, it is necessary to consider anatomy-related major vascular injury. CTA or DSA as the primary tasks should be fully evaluated as early as possible for the formulation of the appropriate management approach.
Conclusion
This present case suggested that although pedicle screw removal was a rather simple procedure, serious complications may arise from this procedure. Surgeons should keep vigilant to avoid the fatal complication noted in this case. Once it occurred during operation, an emergent diagnostic imaging scanning and an appropriate management approach are mandatory to make the best clinical decisions.
Data availability statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by Clinical Research Ethics Committee of the affiliated Taizhou people's hospital of Nanjing Medical University. The patients/participants provided their written informed consent to participate in this study.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ABH completed most of the writing work. SYF and ABH reviewed the literature and participated in the drafting of the manuscript. GJ, XD and HJL participated in patient management. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to acknowledge the patient for generously permitting the use of the data in this report.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Glaser J, Stanley M, Sayre H, Woody J, Found E, Spratt K. A 10-year follow-up evaluation of lumbar spine fusion with pedicle screw fixation. Spine (Phila Pa 1976). (2003) 28(13):1390–5. doi: 10.1097/01.Brs.0000067112.15753.Ad12838096
2. Katonis P, Christoforakis J, Kontakis G, Aligizakis AC, Papadopoulos C, Sapkas G, et al. Complications and problems related to pedicle screw fixation of the spine. Clin Orthop Relat Res. (2003) 411:86–94. doi: 10.1097/01.blo.0000068761.86536.1d
3. Parker SL, Amin AG, Santiago-Dieppa D, Liauw JA, Bydon A, Sciubba DM, et al. Incidence and clinical significance of vascular encroachment resulting from freehand placement of pedicle screws in the thoracic and lumbar spine: analysis of 6816 consecutive screws. Spine (Phila Pa 1976). (2014) 39(8):683–7. doi: 10.1097/BRS.000000000000022124480963
4. Been HD, Kerkhoffs GM, Balm R. Endovascular graft for late iatrogenic vascular complication after anterior spinal instrumentation: a case report. Spine (Phila Pa 1976). (2006) 31(22):E856–8. doi: 10.1097/01.brs.0000240761.13090.a917047534
5. Canaud L, Hireche K, Joyeux F, D’Annoville T, Berthet JP, Marty-Ane C, et al. Endovascular repair of aorto-iliac artery injuries after lumbar-spine surgery. Eur J Vasc Endovasc Surg. (2011) 42(2):167–71. doi: 10.1016/j.ejvs.2011.04.01121592826
6. Alanay A, Vyas R, Shamie AN, Sciocia T, Randolph G, Wang JC. Safety and efficacy of implant removal for patients with recurrent back pain after a failed degenerative lumbar spine surgery. J Spinal Disord Tech. (2007) 20(4):271–7. doi: 10.1097/01.bsd.0000211283.14143.ad17538350
7. Smits AJ, den Ouden L, Jonkergouw A, Deunk J, Bloemers FW. Posterior implant removal in patients with thoracolumbar spine fractures: long-term results. Eur Spine J. (2017) 26(5):1525–34. doi: 10.1007/s00586-016-4883-827864682
8. Kellam PJ, Harrast J, Weinberg M, Martin DF, Davidson NP, L C. Saltzman: complications of hardware removal. J Bone Joint Surg Am. (2021) 103(22):2089–95. doi: 10.2106/JBJS.20.0223134398858
9. Pesenti S, Bartoli MA, Blondel B, Peltier E, Adetchessi T, Fuentes S. Endovascular aortic injury repair after thoracic pedicle screw placement. Orthop Traumatol Surg Res. (2014) 100(5):569–73. doi: 10.1016/j.otsr.2014.03.02025023930
10. Kokotsakis J, Misthos P, Sakellaridis T, Farsaris D, Anagnostakou V, Spiliotopoulos K, et al. Emergent endovascular repair as damage control step of aortic injury after posterior spinal instrumentation. Ann Thorac Surg. (2010) 89(4):1304. doi: 10.1016/j.athoracsur.2009.07.08720338369
11. Hanson B, van der Werken C, Stengel D. Surgeons’ beliefs and perceptions about removal of orthopaedic implants. BMC Musculoskelet Disord. (2008) 9(73). doi: 10.1186/1471-2474-9-73
12. Jeon CH, Lee HD, Lee YS, Seo JH, Chung NS. Is it beneficial to remove the pedicle screw instrument after successful posterior fusion of thoracolumbar burst fractures? Spine (Phila Pa 1976). (2015) 40(11):E627–33. doi: 10.1097/BRS.000000000000087026091158
13. Stavridis SI, Bucking P, Schaeren S, Jeanneret B, Schnake KJ. Implant removal after posterior stabilization of the thoraco-lumbar spine. Arch Orthop Trauma Surg. (2010) 130(1):119–23. doi: 10.1007/s00402-009-0962-119727780
14. Crasto JA, Wawrose RA, Donaldson WF. Severe pulmonary injury leading to death during thoracic rod removal: a case report. Eur Spine J. (2020) 29(Suppl 2):183–7. doi: 10.1007/s00586-020-06591-532920690
15. Vanichkachorn JS, Vaccaro AR, Cohen MJ, Cotler JM. Potential large vessel injury during thoracolumbar pedicle screw removal. A case report. Spine (Phila Pa 1976). (1997) 22(1):110–3. doi: 10.1097/00007632-199701010-000189122774
16. Wang YR, Liu YC, Chung NC, Wu SZ, Chen MS, Ye XD, et al. Inferior vena cava tear during posterior spinal fusion surgery. Acta Anaesthesiol Sin. (2003) 41(2):89–92.12934424
17. Yen CY, Yang SC, Chen HS, Tu YK. Endovascular retrieval of a migrating pedicle screw within the inferior vena cava after instrumented spinal surgery: case report. J Neurosurg Spine. (2018) 28(2):215–9. doi: 10.3171/2017.5.SPINE1720829171788
18. Makino T, Kaito T, Sakai Y, Takenaka S, Yoshikawa H. Iatrogenic arteriovenous fistula and retroperitoneal hemorrhage after tapping of lumbar pedicle screws: a case report. JBJS Case Connect. (2019) 9(3):e0477. doi: 10.2106/JBJS.CC.18.0047731584906
19. Balachandran G, Bharathy KGS, Sikora SS. Penetrating injuries of the inferior vena cava. Injury. (2020) 51(11):2379–89. doi: 10.1016/j.injury.2020.08.02232838960
20. Liu L, Li N, Wang Q, Wang H, Wu Y, Jin W, et al. Iatrogenic lumbar artery injury in spine surgery: a literature review. World Neurosurg. (2019) 122:266–71. doi: 10.1016/j.wneu.2018.10.21930419401
21. Yan GW, Li HW, Yang GQ, Bhetuwal A, Liu JP, Li Y, et al. Iatrogenic arteriovenous fistula of the iliac artery after lumbar discectomy surgery: a systematic review of the last 18 years. Quant Imaging Med Surg. (2019) 9(6):1163–75. doi: 10.21037/qims.2019.05.1231367570
22. Mirza AK, Alvi MA, Naylor RM, Kerezoudis P, Krauss WE, Clarke MJ, et al. Management of major vascular injury during pedicle screw instrumentation of thoracolumbar spine. Clin Neurol Neurosurg. (2017) 163:53–9. doi: 10.1016/j.clineuro.2017.10.01129073499
23. Chan YC, Morales JP, Reidy JF, Taylor PR. Management of spontaneous and iatrogenic retroperitoneal haemorrhage: conservative management, endovascular intervention or open surgery? Int J Clin Pract. (2008) 62(10):1604–13. doi: 10.1111/j.1742-1241.2007.01494.x17949429
24. van Zitteren M, Fan B, Lohle PN, de Nie JC, de Waal Malefijt J, Vriens PW, et al. A shift toward endovascular repair for vascular complications in lumbar disc surgery during the last decade. Ann Vasc Surg. (2013) 27(6):810–9. doi: 10.1016/j.avsg.2012.07.01923541780
25. Gok M, Aydin E, Guneyli S, Akay A, Cinar C, Oran I. Iatrogenic vascular injuries due to spinal surgeries: endovascular perspective. Turk Neurosurg. (2018) 28(3):469–73. doi: 10.5137/1019-5149.JTN.19286-16.228191625
26. Koban O, Akar E, Öğrenci A, Yilmaz M, Dalbayrak S. Any instrument in a surgeon’s hand can be fatal: unusual iliac artery injury in lumbar spinal deformity surgery. World Neurosurg. (2020) 143:276–9. doi: 10.1016/j.wneu.2020.07.21732777398
27. Lin SH, Hu MH, Wu IH. A 13-year old spinal screw perforating into the thoracic aorta. Eur J Cardiothorac Surg. (2020) 57(3):607. doi: 10.1093/ejcts/ezz25532077479
28. Pillai ST, Schoenhagen P, Subrahmanyan L, Mukherjee SK, McNamara RL, Elefteriades J, et al. Aortic dissection associated with penetration of a spinal pedicle screw: a case report and review of the literature. J Card Surg. (2014) 29(3):377–81. doi: 10.1111/jocs.1232724707982
Keywords: pedicle screw, implant removal, iatrogenic vascular injury, inferior vena cava, case report
Citation: Fu S, Ju G, Dai X, Li H and Huang A (2023) Severe major vessel injury during peadicle screw removal: a case report. Front. Surg. 10:1187801. doi: 10.3389/fsurg.2023.1187801
Received: 16 March 2023; Accepted: 22 May 2023;
Published: 13 June 2023.
Edited by:
Harsh Deora, National Institute of Mental Health and Neuroscinces, IndiaReviewed by:
Vincent Nguyen, University of Southern California, United StatesMark G. Davies, The University of Texas Health Science Center at San Antonio, United States
© 2023 Fu, Ju, Dai, Li and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ai-Bing Huang aGFiMTY1QDE2My5jb20=
†ORCID Aibing Huang orcid.org/0000-0001-8224-5527
 ShengYu Fu
ShengYu Fu Gang Ju1
Gang Ju1 Aibing Huang
Aibing Huang