
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
EDITORIAL article
Front. Surg., 17 March 2023
Sec. Thoracic Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1176124
This article is part of the Research TopicNear-Infrared Fluorescence Guided Surgery: State of the evidence from a health technology assessment perspectiveView all 10 articles
Editorial on the Research Topic
Near-infrared fluorescence guided surgery: State of the evidence from a health technology assessment perspective
Indocyanine green is a fluorescent dye used in various medical applications, including thoracic surgery. Indocyanine green-based near-infrared fluorescence imaging can provide real-time visualization of the vascular and lymphatic structures, aiding in the identification of critical anatomical structures during thoracic surgeries (1–4).
Some potential applications of indocyanine green-based near-infrared fluorescence imaging in thoracic surgery include:
1. Pulmonary segmentectomy.Near-infrared fluorescence imaging using Indocyanine green can aid in the identification of segmental bronchi and vessels, which can help in the precise identification and preservation of pulmonary segments during segmentectomy. Due to the development of imaging technologies, there has been an increase in the discovery of small, nonpalpable lung nodules previously undetected. Long-awaited randomized controlled experiment JCOG0802 demonstrated that segmentectomy is superior to lobectomy for lung tumors 2 cm in size. Consequently, it is reasonable to predict that segmentectomies will replace lobectomies for stage IA illness (5). Before segmentectomies can be regarded as the standard of care for this subset of patients and widely adopted by thoracic surgeons, at least three pillars must be established: the non-inferiority of segmentectomy to lobectomy in terms of oncologic efficacy, the technical feasibility, and a good cost-effectiveness profile vis-à-vis the standard approach.Consequently, the tumor’s location is essential for thoracic surgeons undergoing segmentectomies. When nodules are discovered in peripheral segments or intersegmental planes, it is essential to examine the tumor’s location and segmental region to give radical surgical margins. Precise knowledge of the nodule and intersegmental plane is necessary to accomplish a complex segmentectomy (6).
2. Mediastinal lymph node dissection.Indocyanine green-based near-infrared fluorescence imaging can identify the lymphatic drainage of tumors in the mediastinum, allowing for more accurate identification and dissection of lymph nodes during surgery. After peritumoral injection, it can help identify sentinel lymph nodes and observe the lymphatic drainage path during lung resections, allowing for correct lymphadenectomy and N staging, or it can aid in the treatment of problems such as chylorrhea by locating the thoracic duct. Near-infrared fluorescence fluorescence-guided sentinel lymph node mapping can correctly identify the sentinel lymph node, allowing the discovery of micrometastases, providing accurate staging, and possibly improved survival. Using the so-called improved permeability and retention, a passive targeting effect 24 h after the injection of a hefty dose of near-infrared fluorescence can visualize even small pulmonary nodules, filling the vacuum following the loss of tactile input during VATS. Other fluorescent dyes are more specific for adenocarcinomas, although their usage is uncommon (7).
3. Identification of pulmonary nodules.Near-infrared fluorescence imaging using Indocyanine green can aid in the identification of small pulmonary nodules, which can be difficult to visualize with conventional imaging techniques. The indications and complications associated with fluorescence-navigated thoracoscopy have been summarized in a recent consensus study. Specifically, it may be a suitable method for identifying pulmonary nodules, intersegmental planes during thoracoscopic segmentectomy, and the surgical margin after excision. In contrast, given the low-quality evidence for the detection of sentinel lymph nodes, additional research is required to evaluate its role in this context. In addition, the panel of experts felt that fluorescence-guided thoracoscopic surgery could become a standard procedure for treating pulmonary lesions (8).
4. Assessment of pulmonary perfusion.Near-infrared fluorescence imaging using Indocyanine green can provide real-time visualization of pulmonary perfusion, which can help evaluate lung function and identify areas of impaired perfusion (1–4).
5. Thoracoscopic sympathectomy.Indocyanine green-based near-infrared fluorescence imaging can aid in the identification of the sympathetic chain during thoracoscopic sympathectomy, which can help reduce the risk of nerve injury (1–4).
Overall, Indocyanine green-based near-infrared fluorescence imaging has the potential to enhance the precision and safety of thoracic surgery by providing real-time visualization of anatomical structures and improving the accuracy of surgical interventions. Evidence for the safety and effectiveness of fluorescent imaging in thoracic surgery appears convincing, representing an excellent approach with minimal complications and contraindications. However, given the fundamental importance of a multidimensional assessment of health innovation to guide its diffusion and uptake across healthcare systems, additional research to clarify the managerial, economic, and cost-effectiveness impact of these options is still needed.
In this Research Topic for the Frontiers in Surgery Journal (Table 1), we present state-of-the-art on the clinical and patient-reported outcomes and organizational consequences of future improvements in fluorescence-guided surgery.
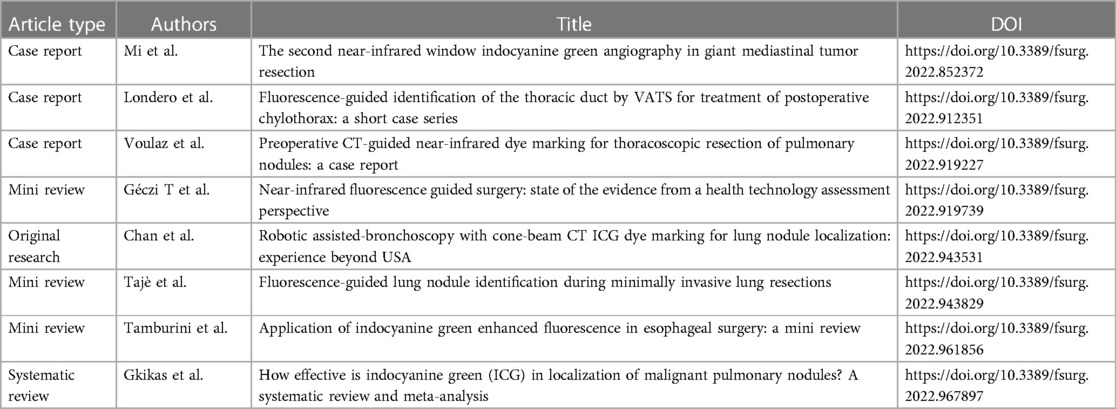
Table 1. Articles published within the research topic of Frontiers in surgery: near-infrared fluorescence guided surgery: state of the evidence from a health technology assessment perspective.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
This work was partially supported by the Italian Ministry of Health with Ricerca Corrente and 5 × 1,000 funds.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Yanagiya M, Hiyama N, Matsumoto J. Hybrid technique of virtual-assisted lung mapping and systemic indocyanine green injection for extended segmentectomy. Surg Case Rep. (2020) 6(1):273. doi: 10.1186/s40792-020-01052-z
2. He H, Zhao H, Ma L, Fan K, Feng J, Zhao R, et al. Identification of the intersegmental plane by arterial ligation method during thoracoscopic segmentectomy. J Cardiothorac Surg. (2022) 17(1):281. doi: 10.1186/s13019-022-02011-5
3. Yanagiya M, Amano Y, Hiyama N, Matsumoto J. Initial experience of virtual-assisted lung mapping utilizing both indocyanine green and indigo carmine. Gen Thorac Cardiovasc Surg. (2021) 69(6):1035–9. doi: 10.1007/s11748-020-01565-2
4. Chen-Yoshikawa T, Tanaka S, Yamada Y, Yuataka Y, Nakajima D, Ohsumi A, et al. P2.17-26 indocyanine green virtual assisted lung mapping (Icg-Val-map): anyone can perform a successful preoperative marking for a small lung nodule. J Thorac Oncol. (2019) 14(10):S894. doi: 10.1016/j.jtho.2019.08.1937
5. Saji H, Okada M, Tsuboi M, Nakajima R, Suzuki K, Aokage K, et al. Segmentectomy versus lobectomy in small-sized peripheral non-small-cell lung cancer (Jcog0802/Wjog4607l): a multicentre, open-label, phase 3, randomised, controlled, non-inferiority trial. Lancet. (2022) 399(10335):1607–17. doi: 10.1016/S0140-6736(21)02333-3
6. Bertolaccini L, Prisciandaro E, Spaggiari L. Commentary: we must constantly look at things in different ways. JTCVS Tech. (2021) 10:550–1. doi: 10.1016/j.xjtc.2021.08.016
7. Geczi T, Simonka Z, Lantos J, Wetzel M, Szabo Z, Lazar G, et al. Near-infrared fluorescence guided surgery: state of the evidence from a health technology assessment perspective. Front Surg. (2022) 9:919739. doi: 10.3389/fsurg.2022.919739
Keywords: near-infrared fluorescence guided surgery, lung cancer, thoracic surgery, health technology assessment, VATS
Citation: Bertolaccini L and Ciani O (2023) Editorial: Near-infrared fluorescence guided surgery: State of the evidence from a health technology assessment perspective. Front. Surg. 10:1176124. doi: 10.3389/fsurg.2023.1176124
Received: 28 February 2023; Accepted: 1 March 2023;
Published: 17 March 2023.
Edited and Reviewed by: Marco Scarci, Hammersmith Hospital, United Kingdom
© 2023 Bertolaccini and Ciani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Luca Bertolaccini bHVjYS5iZXJ0b2xhY2NpbmlAZ21haWwuY29t
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.