
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Surg., 10 July 2023
Sec. Visceral Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1164613
Hepatic angiomyolipoma (HAML) is a rare mesenchymal neoplasm that predominantly affects middle-aged women. In this study, we present a case of a 49-year-old woman with a giant HAML accompanied by spontaneous subcapsular rupture. The patient initially experienced nausea and abdominal distention, followed by an enlargement of the upper abdominal circumference. Laboratory examination revealed decreased serum hemoglobin, while tumor biomarkers were within normal ranges. Imaging studies, such as abdominal ultrasound and contrast-enhanced computed tomography (CT), demonstrated a large upper abdominal mass with heterogeneous density and hypervascularity. The tumor appeared to have invaded the left liver, raising concerns about possible malignancy. Subsequent positron-emission tomography/CT confirmed increased fluorodeoxyglucose uptake in the mass. Laparoscopic exploration revealed a protruding, well-encapsulated tumor from the left liver, exhibiting subcapsular hemorrhage. Surgical resection of the tumor and the left liver was performed, leading to a successful outcome.
Hepatic angiomyolipoma (HAML) is a rare hepatic mesenchymal neoplasm first reported in 1976 (1). It is generally composed of blood vessels and smooth muscle cells, and adipose tissue, with great variety in proportions (2). A review published in 2016 identified 292 patients with one or more HAML, and most of them are middle-aged women (1). Calame et al. (3) identified 10 HAML patients who had a spontaneous rupture in 2021. Here, we present a rare case of a patient who had a giant HAML with spontaneous subcapsular rupture.
A 49-year-old woman presented with a 6-month history of nausea and abdominal distention after meals, followed by an enlargement of the upper abdominal circumference. She had no symptoms of jaundice, abdominal pain, or constipation. Her laboratory examination showed decreased serum hemoglobin (78 g/L) and normal white blood cell counts. Tumor biomarkers, such as alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA), carbohydrate antigen 19-9 (CA19-9), and carbohydrate antigen 125 (CA125), were all negative. Abdominal ultrasound showed a slightly hyperechoic mass in the upper abdominal region, exhibiting echo heterogenicity, without obvious blood flow signal. Contrast-enhanced computed tomography (CT) revealed a 15 cm × 10 cm upper abdominal mass with heterogeneous density (Figure 1, dot lines: maximal size of the mass, 18.4 cm × 16.2 cm). The risk of malignancy is indicated by the mass potential invasion into the left liver. Blood supply was shown to come from the celiac trunk. The middle hepatic vein was compressed, and the left hepatic vein was not revealed. Positron-emission tomography (PET)/CT revealed a slightly increased 18F-fluorodeoxyglucose (FDG) intake, with a standardized uptake value (SUV) max of 2.4.
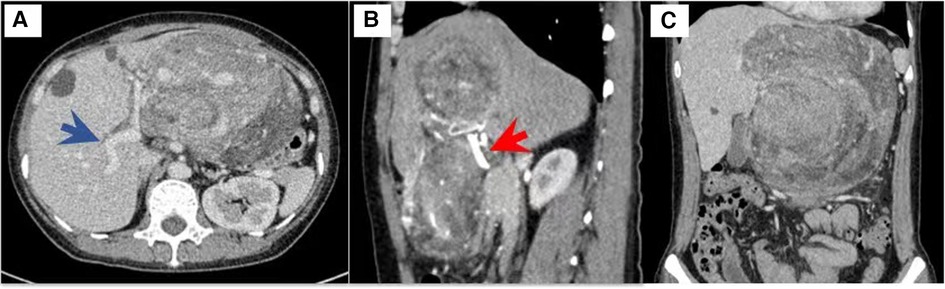
Figure 1. Contrast-enhanced computed tomography of the mass. Blue arrow, portal vein. Red arrow, hepatic artery.
Retroperitoneal tumor, gastrointestinal stromal tumor, and left hepatic tumor were suspected before surgery. Hepatic hemangioma is the most common benign hepatic tumor, characterized by a hypervascular appearance on imaging studies such as contrast-enhanced CT or magnetic resonance imaging (MRI). However, in contrast to HAML, hemangiomas typically demonstrate a homogeneous enhancement pattern during the arterial phase, followed by a progressive centripetal filling and delayed washout during the venous phase. Furthermore, the absence of a central scar and the presence of fat components in HAML can aid in differentiating it from hepatic hemangioma.
As the preoperative diagnosis was uncertain, there was a risk associated with puncture due to potential hemorrhage. Therefore, we decided to proceed directly with surgical intervention. During laparoscopic exploration, a protruding, well-encapsulated tumor from the left liver was identified. A laparoscopic approach was employed for the resection of the tumor and left liver. Subcapsular hemorrhage indicated a spontaneous rupture (Figure 2, white asterisk, the left liver; black asterisk, the tumor with subcapsular hemorrhage). Thus, the entire tumor and left liver were resected. This patient recovered well and was discharged on postoperative day 6.
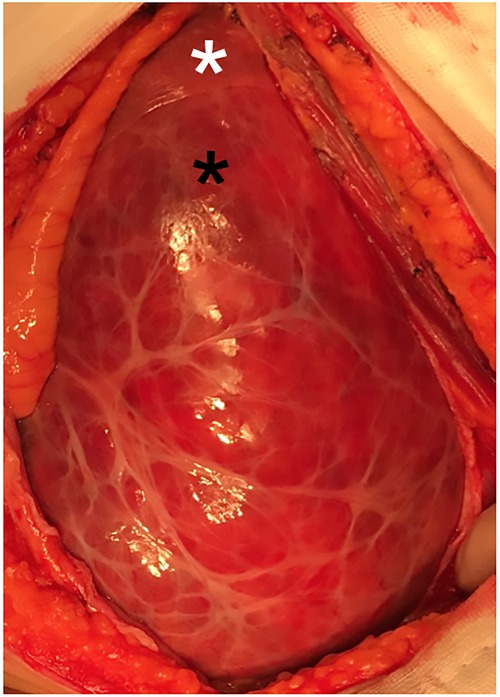
Figure 2. Intraoperative image of the mass. white asterisk: left liver; black asterisk: the tumor with subcapsular hemorrhage.
Her histological examination (Figure 3) showed that the tumor was composed of mixed proportions of blood vessels, smooth muscle cells (SMCs), and adipose tissue. Immunohistochemistry staining indicated that the tumor had positive homatropine methylbromide-45 (HMB-45), smooth muscle actin (SMA), and Melan-A (not shown) but was negative for S100. The Ki-67 index was 5%.
HAML typically occurs in a non-cirrhotic liver. Generally, patients with HAML have no obvious symptoms and find the tumor occasionally during medical examination (42%–72%) (4). In renal AML, tumor size (≥4 cm) and pregnancy are known risk factors for rupture (5). However, the risk factors for the rupture of HAML remain unclear, given the paucity of available data. In previous studies, the size of ruptured HAML was often reported as small (with a median of 4 cm) (3). Only one case of HAML with a size greater than 10 cm (12 cm) had been reported (6). In this report, the size of HAML is 18 cm. Despite the subcapsular rupture, the capsular is still intact. Current evidence suggests that tumor size may not be a risk factor for rupture. However, more evidence is needed to draw a convincing conclusion.
HAML is typically difficult to diagnose before biopsy due to its significantly varying composition. It was summarized that only 28.2% of patients had the correct diagnosis before resection (1). In this case, there was an increase in the degree of malignancy suspicion due to the adjacent tissues being heavily compressed, which strongly resembled an “invasion” as seen on CT.
Although HAML is typically regarded as benign, its aggressive potential is drawing more and more attention as evidence increases. Thus, radical resection should be considered for suspected patients, especially taking into consideration that the tumor has a risk of rupture. Some risk factors, e.g., tumor size greater than 5 cm, infiltrative growth pattern, high nuclear grade, necrosis, and mitotic activity >1/50 high power field, were proposed (3). This patient needs further surveillance for a better prognosis. The limitation of this case report is that this is a single-patient design and further studies with larger patient cohorts are needed to validate our observations.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Conception and design: QQ. Administrative support: FT. Provision of study materials or patients: YY. Collection and assembly of data: YX. Manuscript writing: CW. All authors contributed to the article and approved the submitted version.
This article was supported by the China Medical Board Project (ZYJ201912).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Klompenhouwer AJ, Verver D, Janki S, Bramer WM, Doukas M, Dwarkasing RS, et al. Management of hepatic angiomyolipoma: a systematic review. Liver Int. (2017) 37(9):1272–80. doi: 10.1111/liv.13381
2. Kamimura K, Nomoto M, Aoyagi Y. Hepatic angiomyolipoma: diagnostic findings and management. Int J Hepatol. (2012) 2012:410781. doi: 10.1155/2012/410781
3. Calame P, Tyrode G, Verhoeven DM, Felix S, Klompenhouwer AJ, Martino VD, et al. Clinical characteristics and outcomes of patients with hepatic angiomyolipoma: a literature review. World J Gastroenterol. (2021) 27(19):2299–311. doi: 10.3748/wjg.v27.i19.2299
4. Klompenhouwer AJ, Dwarkasing RS, Doukas M, Pellegrino S, Vilgrain V, Paradis V, et al. Hepatic angiomyolipoma: an international multicenter analysis on diagnosis, management and outcome. HPB. (2020) 22(4):622–9. doi: 10.1016/j.hpb.2019.09.004
5. Pontis A, Piras B, Meloni A, Lisa AD, Melis GB, Angioni S. Rupture of renal angiomyolipoma in pregnancy. J Obstet Gynaecol. (2013) 33(6):628–9. doi: 10.3109/01443615.2013.810201
Keywords: hepatic angiomyolipoma (HAML), subcapsular rupture, laparoscopic—laparotomy, left liver, case report
Citation: Wu C, Yang Y, Tian F, Xu Y and Qu Q (2023) A rare case of giant hepatic angiomyolipoma with subcapsular rupture. Front. Surg. 10:1164613. doi: 10.3389/fsurg.2023.1164613
Received: 13 February 2023; Accepted: 23 June 2023;
Published: 10 July 2023.
Edited by:
Krzysztof Zieniewicz, Medical University of Warsaw, PolandReviewed by:
Nguyen Cong Long, Bạch Mai Hospital, Vietnam© 2023 Wu, Yang, Tian, Xu and Qu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiang Qu cWlhbmdxdUBob3RtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.