
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 05 May 2023
Sec. Surgical Oncology
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1156337
Background: Spontaneous hemorrhage of gastro-omental hemangioma is a rare disease. The treatment strategy for this disease changes as it develops. In the acute stage, surgery is the first priority, among which laparoscopic treatment should be the most frequently considered option in large general hospitals. Due to the rarity of this disease, such cases have rarely been reported.
Case description: We present the first report of two eldely cases with gastro-omental hemangioma with hemorrhage by laparoscopic treatment. Both cases were initially admitted with upper abdominal pain, and abdominal computed tomography (CT) scan revealed masses alongside the greater curvature of the stomach. Laparoscopic surgery was conducted immediately in both patients. The two cases recovered well after surgery, and no obvious abnormalities were observed in the follow-up period.
Conclusion: Gastro-omental hemangioma rupture remains an uncommon cause of intraperitoneal hemorrhage. Timely diagnosis and surgery are paramount for treatment. Medical institutions with the correct technology and equipment should perform laparoscopic treatment to minimize surgical trauma and promote rapid recovery of patients with abdominal apoplexy.
Spontaneous hemorrhage of gastro-omental hemangioma is not common, and it may occur without any recent history of abdominal trauma, surgery, anticoagulant therapy, or systemic vascular disease. Clinical diagnosis should be made with abdominal B-ultrasound, abdominal CT, abdominal puncture, and other auxiliary examinations. The treatment methods generally depend on the disease development and the patient's conditions. In the onset or chronic phase, clinical observation and medical treatment are routine options, while in the advanced or acute phase, surgical treatment is preferred (1, 2). Recently, several case reports of gastro-omental hemangioma combined with hemorrhage have been reported; however, few studies have reported on laparoscopic surgery for this condition (3, 4). In this article, we present two elderly cases with spontaneous gastro-omental hemangioma with hemorrhage and huge intra-abdominal hematoma treated with laparoscopic surgery, achieving a good treatment effect. Both cases recovered well after operation, and experienced no discomfort in the follow-up period.
A 61-year-old female was admitted to our hospital on September 16, 2018 due to persistent dull pain in the middle and upper abdomen for > 2 months, with aggravation for 1 day. The pain was relieved after taking an oral anodyne (specific name and dosage unknown) prescribed by a local physician, and no further examination or treatment was given. She denied any history of hypertension, diabetes, hepatitis, tuberculosis, heart disease, abdominal trauma, or operation. Physical examination showed the patient had acute facial features and pallid eyelid conjunctiva, and her skin was clammy and less elastic, with a body temperature (T) of 36.5°C, pulse frequency (P) of 80 beats/min, respiration frequency (R) of 20 beats/min and blood pressure (BP) of 126/80 mmHg. Abdominal moving dullness was positive, and non-coagulated blood was extracted by diagnostic abdomen puncture.
Routine blood examination revealed the following: white blood cell count (WBC) of 9,800/mm3 (normal range 4,000–10,000/mm3), red blood cell count (RBC) of 3,100/mm3 (normal range 3,800–5,100/mm3), platelet (PLT) of 130/mm3 (normal range 100–300/mm3), Hematocrit (HCT) of 0.283 (normal range 0.350–0.450), and a hemoglobin (HGB) concentration of 91 g/dl (normal range 115–150 g/dl). No abnormality was found on coagulation function examination. The above results indicated that the patient had an intraperitoneal hemorrhage combined with moderate anemia.
Abdominal enhanced computed tomography (CT) revealed an effusion in the abdomen and pelvis, suspicious blood accumulation around the liver and spleen, and a slightly patchy high-density shadow on the side of the great curvature of the gastric body, about 9.8 × 6.9 × 6.5 cm in size (Figure 1A). Emergency laparoscopic exploration was subsequently performed. During the procedure, about 1,400 ml of bloody fluid was found in the abdominal pelvic cavity, and an elliptical mass about 10.1 × 8.2 × 8.0 cm in size, with a surrounding blood clot was detected in the omentum of the greater curvature of the gastric body (Figure 1B). The boundary of the mass was unclear, and accompanied by active hemorrhage, which was difficult to separate from the greater curvature of the gastric body. Therefore, the mass and the attached wedge-shaped stomach wall were simultaneously removed by an endoscopic linear cutting stapler (EC60A, Ethicon) (Figure 1C). Hemostasis, anti-infection, and symptomatic treatment were provided postoperatively. Postoperative pathological examination revealed an omental capillary hemangioma with hemorrhage (Figure 1D), and the patient was discharged on postoperative Day 7. No complaints of special discomfort were mentioned, and no abnormal findings were found on routine blood and abdominal CT examination in the 1 year followed-up period (data not shown).
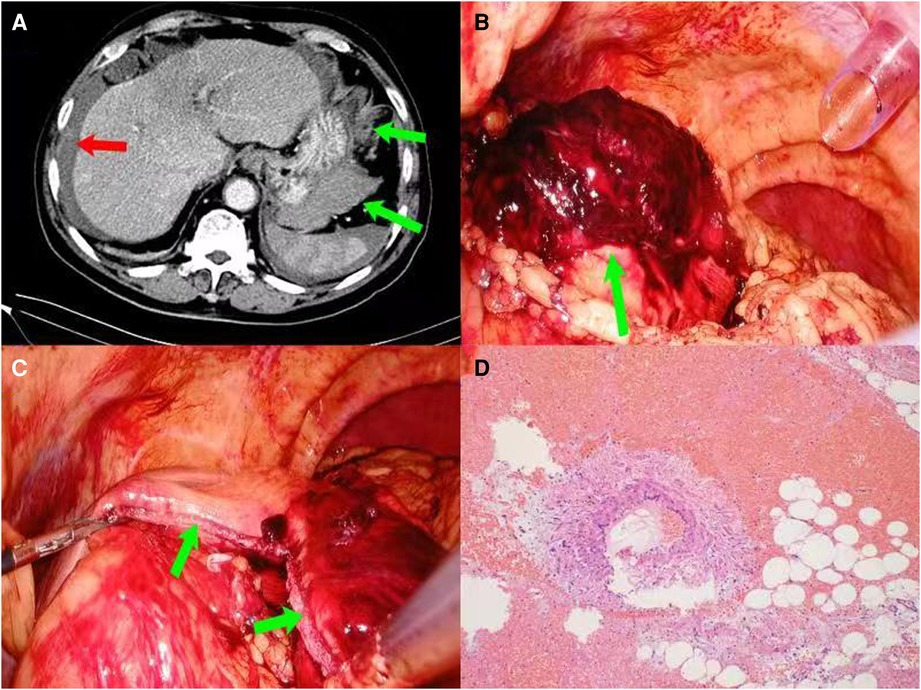
Figure 1. (Case 1) (A): enhanced CT of the upper abdomen showing a mass in the greater curvature of the stomach (green arrows), with fluid/blood accumulation around the liver and spleen (red arrow); (B): the boundary between the hematoma and the greater curvature of the gastric wall was not clear (green arrow); (C): intraoperative resection of the hematoma and part of the wedge-shaped gastric wall (green arrows); (D): postoperative pathological examination identified identified an omental capillary hemangioma with hemorrhage (HE × 100).
An 81-year-old male was admitted on December 13, 2020 due to upper abdominal pain for 20 h. His medical history revealed hypertension for approximately 10 years, with a maximum blood pressure of 180/110 mmHg. He was receiving Nifedipine to control blood pressure. The patient had no history of hepatitis, tuberculosis, heart disease, diabetes, trauma, surgery, or blood transfusion.
Physical examination indicated acute facial features, clammy and weakened elastic skin, with T 36.7°C, P 90 beats/min, R 25 beats/min and BP 138/90 mmHg. His abdomen was flat, and the middle and upper abdomen had a moderate tenderness and rebound pain, without muscle tension; however, abdominal moving dullness was strongly positive, and non-coagulated blood was obtained by diagnostic abdominal puncture. Routine blood examination showed the following: WBC 9,800/mm3, RBC 3,200/mm3 (normal range 4,300–5,800/mm3), PLT 91/mm3, HCT 0.311 (normal range 0.400–0.500), HGB: 107 g/L (normal range 130–175 g/dl), and a normal coagulation index. The above results confirmed that the patient had an intraperitoneal hemorrhage combined with moderate anemia.
Abdominal enhanced CT scan revealed the following: 1. Obvious local lumen stenosis was observed at the beginning of the Celiac axis, with a few calcifications on the wall. This was considered as atherosclerosis. Calcified plaques had formed in the abdominal aorta, bilateral common iliac artery, bilateral internal iliac artery, and right external iliac artery, partially accompanied by mural thrombosis (Figure 2A). 2. Hematoma had formed in the upper left abdominal cavity. The boundary between the hematoma and the greater curvature of the gastric wall was unclear, and abdominal pelvic fluid/blood was detected (Figure 2B). The hematoma was 10.2 × 9.5 × 3.3 cm in size, and located in the greater curvature of the stomach. Their boundary was not clear. Surgery involved removal of the mass and partial attachment of the gastric wall with an endoscopic linear cutting stapler (EC60A, Ethicon) (Figure 2C). The postoperative pathological results confirmed the diagnosis of ruptured omental cavernous hemangioma accompanied by thrombosis (Figure 2D). The patient was discharged on postoperative Day 8. No obvious abnormalities were reported and no abnormal findings were detected by blood routine and abdominal CT examination in the 6-month outpatient follow-up period (data not shown).
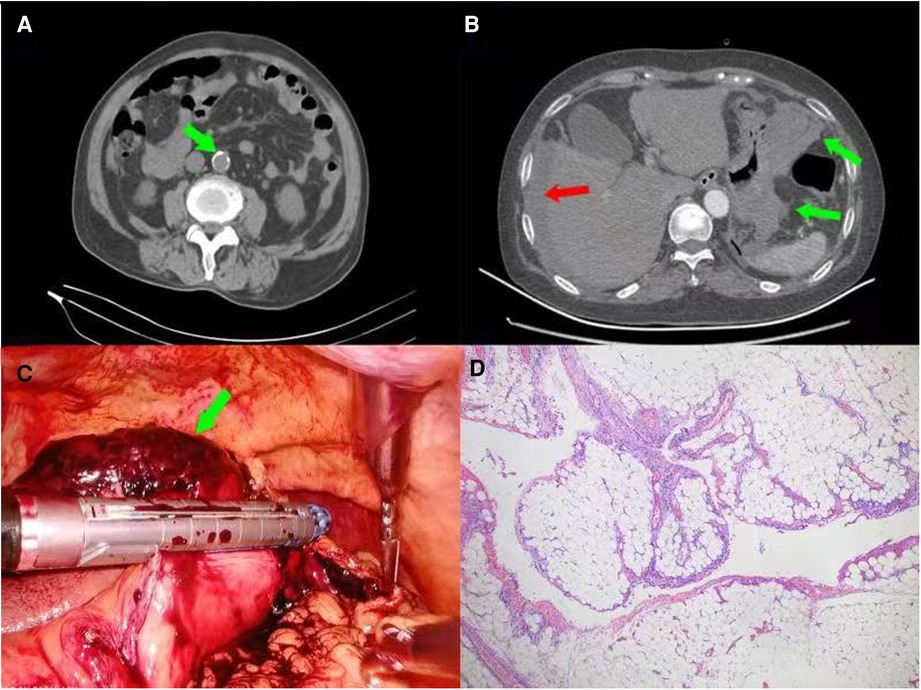
Figure 2. (Case 2) (A): CT-scan showing the formation of calcified plaques in the abdominal aorta (green arrow), bilateral common iliac artery, bilateral internal iliac artery, and right external iliac artery, partially accompanied by mural thrombosis; (B): enhanced CT of the upper abdomen showing hematoma formation in the upper left abdominal cavity, an unclear boundary between the hematoma and stomach (green arrows), and abdominal pelvic fluid/blood (red arrow). (C): The procedure was conducted by removing the mass and partly attached gastric wall with an endoscopic linear cutting stapler (EC60A, Ethicon). (D): Postoperative pathological examination showing a ruptured cavernous hemangioma with hemorrhage and thrombosis (HE × 100).
Intraperitoneal bleeding can have many causes, including trauma, iatrogenic or ruptured aneurysm, gynecological disease, malignant tumors, and inflammatory or autoimmune processes, but spontaneous or idiopathic bleeding is rare. Abdominal apoplexy is a type of acute abdomen usually caused by unknown factors, and is accompanied by intra-abdominal vascular spontaneous rupture and retroperitoneal hemorrhage. The pathogenesis of abdominal apoplexy is still unclear; however, a few reports have reported possible causes as follows: 1. Abdominal organ vascular malformations, visceral tumors, abnormal coagulation function, liver cirrhosis, hypertension, arteriosclerosis, rheumatism, immune system diseases, and so on. It has also been documented that visceral vascular rupture can lead to abdominal bleeding. Kumari J et al. (5) reported the occurrence of a case of spontaneous intraperitoneal bleeding without obvious inducement during pregnancy. Pancreatic tumor fibroma has also been reported as a rare cause of abdominal bleeding (6). In addition, rupture of large liver tumors and female uterine fibroids may also lead to accidental bleeding in the abdominal cavity (7, 8). Another study reported that some abdominal varicose veins can lead to spontaneous abdominal bleeding (9); 2. A small number of young people with no definite cause may also be at risk of abdominal apoplexy (1); 3. The rupture of Gastro-omental hemangioma is another infrequent cause of intraperitoneal hemorrhage (10), also as reported in this paper.
Previous reports have indicated that patients with abdominal apoplexy should undergo auxiliary examination, including blood routine examination, abdominal B-ultrasound, abdominal x-ray, abdominal CT, computed tomography angiography (CTA), angiography, intervention, etc (3–7). Surgeons may choose different treatment measures for abdominal apoplexy, as follows: A) Conservative treatment: thrombin, blood transfusion and rehydration are selectively administered to patients with an unclear diagnosis, small amount of bleeding, or stable vital signs (11); B) Surgical treatment: Exploratory laparotomy is strongly recommended for those with clear surgical indications who suffered from a large amount of blood loss, and a poor or ineffective response to conservative treatment. Surgical treatment can be roughly divided into two types: laparoscopic exploration and open laparotomy (12); C) Interventional therapy: Patients with definite bleeding sites with stable hemodynamics could underwent if the bleeding site is special or with high risk of surgical methods (6).
In this article, we reported two cases of gastro-omental angioma with spontaneous rupture and bleeding. As shown in Table 1, due to the rarity of this factor as a causes of abdominal apoplexy, there are currently 8 cases reported in the literature (3, 4, 10, 13–17). The specific pathogenesis of this disease is still unclear, but the following high-risk factors need to be considered when coming to the diagnosis: 1. Elderly patients with cardiovascular disease, such as hypertension, arteriosclerosis, hyperlipidemia, coronary heart disease, etc, who take long-term oral anticoagulant medicine should be considered for the possibility of gastro-omental angioma rupture (18). For example, the second case in this paper suffered from primary hypertension, with a blood pressure occasionally reaching up to 180/110 mmHg, and a past history of cerebral infarction and subsequent long-term oral aspirin anticoagulation therapy; 2. This disease can also occur in some patients without high-risk factors and no obvious triggers (19); 3. Patients with congenital vascular malformations can also have abdominal apoplexy, especially in the case of overeating, alcoholism, etc. Several studies have reported a mortality of up to 100% in patients with abdominal apoplexy treated with conservative methods (18, 19). If the bleeding site can be found by exploratory laparotomy, and the bleeding can be controlled effectively, the mortality rate can be reduced to around 8.6%; however, it can reach up to 54.8% if the bleeding site cannot be detected. The main causes of death are hemorrhagic shock and its corresponding complications (20).
In this article, although the vital signs and hemodynamics were relatively stable in both cases, we chose to perform operation as both patients were advanced in age, and their tolerance to bleeding was poor. Moreover, abdominal B-ultrasound and CT examination both confirmed heavy intra-abdominal bleeding, and the bleeding sites were undefined. In fact, if the patient's conditions are permitted, further preoperative examinations, including CTA, MRI or upper GI Endoscopy, ect, should be conducted to identify the source of bleeding for these types of cases. In the follow-up (at 6 and 12 months in cases 1 and 2, respectively) no obvious abnormalities were reported, indicating a good prognostic outcome.
Taken together, this is the first report of two eldely cases with gastro-omental hemangioma hemorrhage treated with laparoscopy. Clinicians should consider the possibility of spontaneous rupture of gastro-omental hemangioma when diagnosing patients with high-risk factors for abdominal apoplexy. Furthermore, laparoscopic exploration should be conducted in medical institutions with the relevant experience, as this can greatly reduce the surgical trauma to the patients, while aiding in a quick recovery. Although laparoscopic treatment of abdominal apoplexy achieved good therapeutic effect in the two cases reported herein, in patients where laparoscopic surgery is difficult, the procedure could be converted to open laparotomy or exploratory laparotomy.
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients provided informed consent for for the publication of this case report.
All authors contributed to the article and approved the submitted version.
This work was supported by the program of strategic cooperation in science and technology of Nanchong City of China (18SXHZ0110).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Hwang Y, Gartrell R, Winter N, Sethi H, Won CK. Laparoscopic management of abdominal apoplexy. Cureus. (2019) 11(3):e4324. doi: 10.7759/cureus.4324
2. Wang H, Xiu D. Abdominal apoplexy because of the rupture of gastroduodenal artery and inferior pancreaticoduodenal artery: a case report. Medicine (Baltimore). (2017) 96(43):e8264. doi: 10.1097/MD.0000000000008264
3. Chateil JF, Saragne-Feuga C, Pérel Y, Brun M, Neuenschwander S, Vergnes P, et al. Capillary haemangioma of the greater omentum in a 5-month-old female infant: a case report. Pediatr Radiol. (2000) 30(12):837–9. doi: 10.1007/s002470000352
4. Nagano H, Goi T, Taguchi S, Tsubaki T, Tsuchiyama T, Uematsu H, et al. Capillary hemangioma arising from the lesser omentum in an adult: a case report. Medicine (Baltimore). (2020) 99(4):e18693. doi: 10.1097/MD.0000000000018693
5. Kumari J, Harkin R. Abdominal apoplexy during pregnancy. BMJ Case Rep. (2020) 13(10):e235946. doi: 10.1136/bcr-2020-235946
6. Qian L, Qiao Z, Chen H. Pancreatic fibroma: a rare cause of intraperitoneal hemorrhage. Am J Med Sci. (2020) 360(6):e13–4. doi: 10.1016/j.amjms.2020.04.039
7. Sahu SK, Chawla YK, Dhiman RK, Singh V, Duseja A, Taneja S, et al. Rupture of hepatocellular carcinoma: a review of literature. J Clin Exp Hepatol. (2019) 9(2):245–56. doi: 10.1016/j.jceh.2018.04.002
8. Jespersen C, Hare KJ. Myoma with an intra-abdominal bleeding. Ugeskr Laeger. (2018) 180(41):V04180268.30327080
9. Lin HH, Garber AM. Intra-Abdominal varix rupture: a life-threatening cause of hemoperitoneum. Am J Med. (2018) 131(10):e419–20. doi: 10.1016/j.amjmed.2018.05.028
10. Ritossa C, Ferri M, Destefano I, De Giuli P. Hemoperitoneum caused by cavernous angioma of the omentum. Minerva Chir. (1989) 44(5):907–8. PMID: 2725917
11. Capitán Del Río I, Ramos Sanfiel J, Zurita Saavedra MS, Hernández García D. Conservative treatment in spontaneous yeyunal hematoma with moderate hemoperitoneum. Cir Esp (Engl Ed). (2022) 100(1):48. doi: 10.1016/j.cireng.2021
12. Law EK, Lee RK, Hung EH, Ng AW. Radiological diagnosis and management of idiopathic spontaneous intra-abdominal haemorrhage (abdominal apoplexy): a case series. Abdom Imaging. (2015) 40(2):343–51. doi: 10.1007/s00261-014-0220-z
13. Shih SL, Sheu JC, Chen BF, Ma YC. Malignant hemangioendothelioma presenting as omental masses in a child. J Pediatr Surg. (1995) 30(1):118–9. doi: 10.1016/0022-3468(95)90626-6
14. Ratan S, Bhatnagar V, Gupta SD, Mitra DK. Epithelioid hemangioendothelioma of the greater omentum: report of a case. Surg Today. (1999) 29(9):919–21. doi: 10.1007/BF02482787
15. Chung J, Kim M, Lee JT, Yoo HS. Hemangiopericytoma/solitary fibrous tumor of the greater omentum: a case report and review of the literature. Int J Surg Case Rep. (2016) 23:160–2. doi: 10.1016/j.ijscr.2016.04.028
16. McHugh K, Spitz L. Capillary haemangioma of the greater omentum. Pediatr Radiol. (2002) 32(2):148–9. doi: 10.1007/s00247-001-0618-y
17. Vyčítal O, Liška V, Hadravská Š, Třeška V. Hemangiomatosis of the greater omentum—a case report. Rozhl Chir. (2019) 98(4):178–80. doi: 10.33699/pis.2019.98.4.178-180
18. Kimura J, Okumura K, Katagiri H, Lefor AK, Mizokami K, Kubota T. Idiopathic omental hemorrhage: a case report and review of the literature. Int J Surg Case Rep. (2016) 28:214–8. doi: 10.1016/j.ijscr.2016.10.003
19. Cawyer JC, Stone CK. Abdominal apoplexy: a case report and review. J Emerg Med. (2011) 40(3):e49–52. doi: 10.1016/j.jemermed.2007.11.080
Keywords: laparoscope, omentum, hemangioma, hemorrhage, abdominal apoplexy
Citation: Yin L-K, Liu J-J, Feng Y-G, Yuan H-Y, Wang W, Bai X-Y and Wang P (2023) Case report: Laparoscopic treatment of gastro-omental hemangioma with hemorrhage: two cases reports and review of literature. Front. Surg. 10:1156337. doi: 10.3389/fsurg.2023.1156337
Received: 1 February 2023; Accepted: 20 April 2023;
Published: 5 May 2023.
Edited by:
Saurabh Kataria, University of Missouri, United StatesReviewed by:
Tingliang Fu, Binzhou Medical University Hospital, China© 2023 Yin, Liu, Feng, Yuan, Wang, Bai and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pan Wang bmN3YW5ncGFuQDEyNi5jb20=
†These authors have contributed equally to this work
‡ORCID Long-Kuan Yin orcid.org/0000-0001-5974-5443 Jian-Jun Liu orcid.org/0000-0003-1206-6480 Yi-Guo Feng orcid.org/0000-0003-1334-4833 Hua-Yan Yuan orcid.org/0000-0001-5983-3849 Wei Wang orcid.org/0000-0002-6035-5925 Xiang-Yu Bai orcid.org/0000-0003-0259-1994 Pan Wang orcid.org/0000-0003-2805-8346
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.