- 1Department of Burns and Plastic Surgery, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
- 2Department of Urology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, China
Female urethral stricture is currently a challenging situation. In general, urethra dilatation can be selected for treatment, but the complications and high recurrence rate urge doctors to consider other treatments. Recently, dorsal oral mucosa graft urethroplasty is concerned by more and more surgeons, but there are not enough reports so far. A comprehensive search of dorsal oral mucosa graft urethroplasty was performed. According to the existing literature, there are applications of buccal mucosa and lingual mucosa, and compared with other kinds of grafts, the success rate is higher. However, there is a lack of multicenter, large sample and long follow-up studies. And there is still no enough comparative study between different types of oral mucosa. In summary, dorsal oral mucosa graft urethroplasty is an effective option for the management of female urethral stricture. More multicenter and large sample studies with long-term follow-up data are needed.
Introduction
Female urethral stricture (FUS) is a rare and challenging problem in reconstructive surgery or urology. FUS accounts for 4% and 13% of the causes of bladder outlet obstruction (BOO) (1–6). The real prevalence of FUS is unknown, but it is normally considered a rare disease, and the absence of large series makes FUS underestimated (1, 7). Osman et al. proposed a descriptive definition of urethral stricture as “a symptomatic anatomical narrowing of the urethra based on failure in catheterization, urethral calibration, endoscopic or radiographic vision” (1).
The traditional treatment is urethra dilatation, but it may cause damage, and the cure rate is less than 50% (1, 3). Therefore, urethroplasty has gradually become a popular treatment in recent years (3, 8), There are a variety of surgical methods, including ventral, dorsal, mini-dorsal and dorsolateral approaches, etc. The types of grafts are also varied, such as vaginal mucosa reported by Tsivian et al., and oral mucosa reported by many studies (9–12). In the existing literature on dorsal oral mucosa graft (DOMG) urethroplasty, there are few serious postoperative complications, including restenosis and urinary incontinence. Despite the small sample size and the short follow-up, it seems that the use of oral mucosa is effective in this kind of operation (1, 3). This article intends to review the application of DOMG urethroplasty and summarize the existing literatures.
Etiology
The potential etiologies of female urethral stricture disease are idiopathic, iatrogenic, traumatic, inflammatory, or malignant. In a systematic review of FUS, etiology was defined in a total of 271 patients out of 554 as idiopathic in 139 (51.3%), iatrogenic in 89 (32.8%), inflammatory/infective in 25 (9.2%), and traumatic in 18 (6.6%) (13). Iatrogenic injuries include anterior vaginal or urinary tract surgery, urinary catheterization and radiotherapy of pelvic malignant tumors (14). Traumatic urethral injuries often result from obstetric complications. Infection or inflammation can cause peri-urethral fibrosis and lead to stricture (15). For the women with vaginal mass or suspicious urothelial changes, the malignancy should be considered as a cause of urethral stricture (15).
Methods
For this review article, a literature search was conducted in January 2023, using the Pubmed and EMBASE databases. the searching terms were “urethral stricture” AND “Female” AND [“oral mucosa” OR “buccal mucosa” OR “lingual mucosa” OR “labial mucosa”] AND “dorsal urethroplasty”. Studies were limited to humans, women, and the language must be English. Studies were reviewed independently by the authors.
Surgical technique
Dorsal oral mucosa graft urethroplasty
Gomez et al. and Kore et al. reported their detailed description of the technique (3, 16). The patient was under general anesthesia and in lithotomy position. Then methylene blue was injected for a better visualization of the mucosa. After placing a hydrophilic guidewire, an inverted U-shaped incision was made between the urethra and the clitoris, from 9 o'clock to 3 o'clock. Dissection was performed between the inferior margin of the pubis and the dorsal tissue around the urethra, until the exposure of the bladder neck. Then, at 12 o'clock of the urethra, the dorsal side of the urethra was longitudinally cut from the midline until the site of stricture with the help of catheter. In this process, the surgeon should be careful to protect the urethral tube, the clitoris and the sphincter muscle. Gomez et al. emphasized that if there was no stricture around the meatus, the incision could begin 1 cm proximal to preserve the original structure (3). Then the oral mucosal side was placed towards the urethral lumen. The edges of the graft were sutured to the urethra, including the mucosa and lateral periurethral tissues. Additionally, the graft could be quilted to the undersurface of the clitoris.
The harvest of oral mucosa
Different types of oral mucosa are harvested in different ways. Generally, the buccal mucosa is harvest from the inner cheek and the size of the graft is determined by the stricture length (3, 17). Before the use, the graft needs to be defatted. As for the harvest of lingual mucosa, Sharma et al. reported their experience (11). After the oro-tracheal intubation, the tongue was pulled out of the mouth. The required lingual mucosa graft was harvested using a right-angled scissor. Like buccal mucosa, all the submucosal adventitial tissues need to be removed before the use.
Current literatures
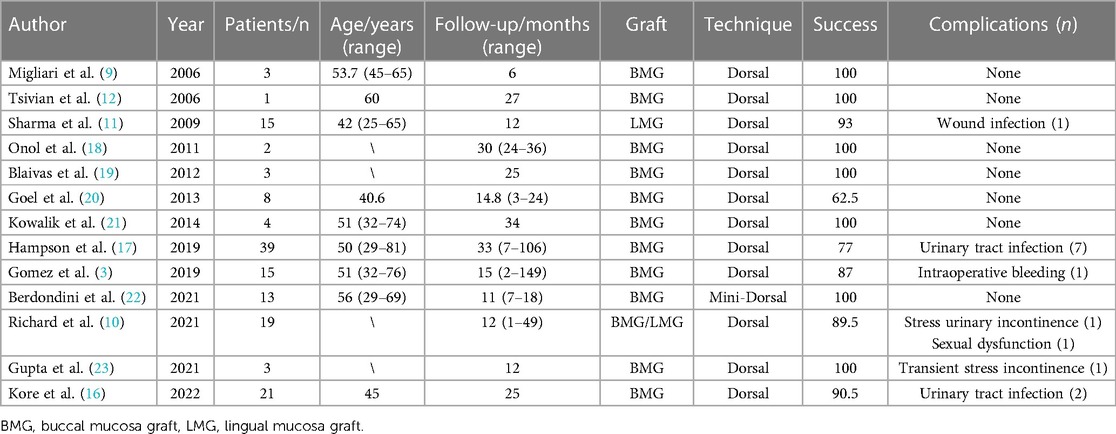
Most authors do not have clear criteria to define successful outcomes, so they resort to no further intervention and symptom relief. Patients with normal urinary flow pattern, maximum urinary flow rate > 12∼15 ml/s, urinary tract diameter > 17F, or normal anatomical imaging data are considered successful (13). As shown in Table 1, in 2006, Tsivian et al. first reported their experience in dorsal buccal mucosa graft (DBMG) urethroplasty (12). The patient was a 60-year-old woman with a history of recurrent urinary tract infection and obstructive voiding symptoms. The surgical team harvested the buccal mucosa which was 1.5 cm in width and 3.5 cm in length. Then the DBMG urethroplasty was performed. After 3 weeks, the suprapubic catheter was removed after voiding cystourethrogrphy (VCUG) showing a patent urethra. No additional treatment was required after 27-month follow-up. Migliari et al. also reported three cases of DBMG urethroplasty (9). The success rate was 100% after 6-month follow-up.
In 2009, Sharma et al. first reported their experience in dorsal lingual mucosa graft (DLMG) urethroplasty (11). 15 female patients who had undergone multiple urethral dilatations were selected for DLMG urethroplasty. The mean length of harvested mucosa was 2.95 cm. After about 15 days, all the patients underwent a trail of VCUG to establish a urethra. The success rate was 93% after 3-month follow-up with one patient having submeatal stenosis who required urethral dilatation. At the 1-year follow-up, none of the patients had any complications.
In recent ten years, the DOMG urethroplasty had become an effective and low-morbidity option for FUS. A few of literatures reported their cases of dorsal urethroplasty with buccal or lingual mucosa. All of them showed high success rates and low complication rates (3, 10, 16, 22–18). In 2019, Hampson et al. reported 39 cases of DBMG urethroplasty from multiple centers, which is the largest series for this technique (17). The mean stricture length was 2.1 cm. After mean duration of 17 days, the catheter was removed. The mean postoperative follow-up was 33 months. Stricture recurrence was seen in 9 patients with mean time to recurrence 14 months. The whole success rate was 77% without serious postoperative complications.
Discussion
Advantages
FUS is a rare disease. Traditionally, the treatment is symptomatic treatment, such as urethra dilatation. However, this method cannot achieve the effect of radical cure. The recurrence rate is more than 50%, and it may cause some trauma to the urethra and surrounding tissue, aggravating the formation of fibers (1, 8, 24, 25). On the contrary, urethroplasty have a high success rate in the existing reports(1, 3). Therefore, surgery should be the first choice for recurrent FUS (8).
For female urethroplasty, the option grafts include vaginal grafts, vaginal flaps or oral mucosa. Vaginal or labial flap was the most common urethroplasty technique. The advantages of local flaps are that they are mobile, usually well vascularized, and can be raised with minimal morbidity. Studies have demonstrated this technique could reach near complete resolution of symptoms (15, 18, 26–28). When vaginal fibrosis or atrophy precludes the use of a local flap, oral mucosa could be great replacement and is getting more and more popular in recent years. Oral mucosa is a natural mucosal tissue, which is elastic, hairless, easy to obtain and large enough. What's more, the process of harvesting has little damage to the donor area. That's why it is an ideal graft for urinary reconstruction (3). In recent years, oral mucosa has also been widely used in the reconstruction of male urethral stricture and the results are optimistic (29, 30). Oral mucosa is also used in the reconstruction of ureteral stricture (31). Recently, Liang et al. reported their results of 41 cases of ureteroplasty with lingual mucosa, which proved the universality and effectiveness of oral mucosa (32). As all of these materials gives good results in the urethral stricture treatment, the selection of specific materials is determined according to the specific clinical conditions and the wishes of patients.
The choice of approach is also very important. In fact, technically speaking, ventrally or dorsally is feasible (33). But recent studies have shown that dorsal approach may have more advantages: 1. The dorsal approach can avoid the occurrence of urethrovaginal fistula; 2. the graft has a firm support from the flat ventral surface of the clitoris; 3. The blood supply of the dorsal approach is more abundant, which is beneficial to the survival of the graft; 4. If patients with stress urinary incontinence need to undergo sling surgery, the ventral approach may make it difficult to perform sling surgery while the dorsal approach can avoid this problem (9, 11, 12, 20, 25, 34). Therefore, DOMG urethroplasty is accepted by more and more surgeons and widely used in clinic.
Limitations
The current limitations are obvious. The number of cases in the existing literature is small, and most of them are single-center studies, and the follow-up time is not long enough. There is a lack of high-quality studies with multi-center, large sample size and long follow-up time.
In addition, there are many types of oral mucosa, including labial mucosa, lingual mucosa and buccal mucosa. The survival rate of different mucosa and its effect on operation are also different. In male urethral reconstruction, it has been reported that the overall result of lingual mucosa is similar to buccal mucosa (35, 36). In ureteral reconstruction, several studies have demonstrated that ureteroplasty using lingual mucosa grafts yields better recipient site outcomes and fewer donor site complications than that using BMG (37, 38). In the study of FUS, only Coskun et al. compared the effects of labial and buccal mucosa (39). There is a lack of more high-quality random controlled trails to further confirm the effects of different mucosa.
Further directions
We need large sample, multi-center and long follow-up studies to demonstrate the effect of DOMG urethroplasty. Also, the comparison of different oral mucosa types is also needed, which is of great guiding significance to the clinic. As for the improvement of surgical methods, Berdondini et al. put forward their ideas (22). Considering that traditional dorsal approach may damage the sphincter or the clitoral bodies, they use a transurethral approach without dissection of the dorsal urethra from the surrounding tissues to preserve as much urethra/periurethral tissues as possible. They presented this novel surgical technique as “mini-dorsal BMG urethroplasty”. All the patients got good results in their follow-up. In the future, we need more improvements in surgical methods to make the surgery less traumatic, recover faster and benefit more patients.
Conclusions
DOMG urethroplasty is an effective option for the management of female urethral stricture. More multicenter and large sample studies with long-term follow-up data are needed.
Author contributions
CT and HZ contributed to conception and design of the study. HZ provided study materials. CT and XJ collected and assembled data. CT wrote the first draft of the manuscript. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that this study received funding from China University Innovation Fund (number 2021JH049). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Osman NI, Mangera A, Chapple CR. A systematic review of surgical techniques used in the treatment of female urethral stricture. Eur Urol. (2013) 64(6):965–73. doi: 10.1016/j.eururo.2013.07.038
2. Carr LK, Webster GD. Bladder outlet obstruction in women. Urol Clin North Am. (1996) 23(3):385–91. doi: 10.1016/S0094-0143(05)70319-0
3. Gomez RG, Segura FJ, Saavedra A, Campos RA. Female urethral reconstruction: dorsal buccal mucosa graft onlay. World J Urol. (2020) 38(12):3047–54. doi: 10.1007/s00345-019-02958-6
4. Groutz A, Blaivas JG, Chaikin DC. Bladder outlet obstruction in women: definition and characteristics. Neurourol Urodyn. (2000) 19(3):213–20. doi: 10.1002/(SICI)1520-6777(2000)19:3%3C213::AID-NAU2%3E3.0.CO;2-U
5. Kuo HC. Videourodynamic characteristics and lower urinary tract symptoms of female bladder outlet obstruction. Urology. (2005) 66(5):1005–9. doi: 10.1016/j.urology.2005.05.047
6. Spilotros M, Malde S, Solomon E, Grewal M, Mukhtar BM, Pakzad M, et al. Female urethral stricture: a contemporary series. World J Urol. (2017) 35(6):991–5. doi: 10.1007/s00345-016-1947-7
7. Smith AL, Ferlise VJ, Rovner ES. Female urethral strictures: successful management with long-term clean intermittent catheterization after urethral dilatation. BJU Int. (2006) 98(1):96–9. doi: 10.1111/j.1464-410X.2006.06206.x
8. West C, Lawrence A. Female urethroplasty: contemporary thinking. World J Urol. (2019) 37(4):619–29. doi: 10.1007/s00345-018-2564-4
9. Migliari R, Leone P, Berdondini E, De Angelis M, Barbagli G, Palminteri E. Dorsal buccal mucosa graft urethroplasty for female urethral strictures. J Urol. (2006) 176(4 Pt 1):1473–6. doi: 10.1016/j.juro.2006.06.043
10. Richard C, Peyronnet B, Drain A, Rosenblum N, Hascoet J, Sussman RD, et al. Dorsal onlay oral Mucosa graft urethroplasty for female urethral stricture. Urology. (2021) 158:215–21. doi: 10.1016/j.urology.2021.09.001
11. Sharma GK, Pandey A, Bansal H, Swain S, Das SK, Trivedi S, et al. Dorsal onlay lingual mucosal graft urethroplasty for urethral strictures in women. BJU Int. (2010) 105(9):1309–12. doi: 10.1111/j.1464-410X.2009.08951.x
12. Tsivian A, Sidi AA. Dorsal graft urethroplasty for female urethral stricture. J Urol. (2006) 176(2):611–3.; discussion 3. doi: 10.1016/j.juro.2006.03.055
13. Sarin I, Narain TA, Panwar VK, Bhadoria AS, Goldman HB, Mittal A. Deciphering the enigma of female urethral strictures: a systematic review and meta-analysis of management modalities. Neurourol Urodyn. (2021) 40(1):65–79. doi: 10.1002/nau.24584
14. Chua KJ, Mikhail M, Patel HV, Tabakin AL, Doppalapudi SK, Sterling J, et al. Treatment of urethral stricture disease in women: nonsystematic review of surgical techniques and intraoperative considerations. Res Rep Urol. (2021) 13:381–406. doi: 10.2147/RRU.S282651
15. Campbell J, Vanni AJ, Kowalik CG. An update on female urethral stricture disease. Curr Urol Rep. (2022) 23(11):303–8. doi: 10.1007/s11934-022-01113-w
16. Kore RN, Martins FE. Dorsal onlay urethroplasty using buccal mucosal graft and vaginal wall graft for female urethral stricture—outcome of two-institution study. Indian J Urol: IJU. (2022) 38(2):140–5. doi: 10.4103/iju.iju_329_21
17. Hampson LA, Myers JB, Vanni AJ, Virasoro R, Smith TG 3rd, Capiel L, et al. Dorsal buccal graft urethroplasty in female urethral stricture disease: a multi-center experience. Transl Androl Urol. (2019) 8(Suppl 1):S6–s12. doi: 10.21037/tau.2019.03.02
18. Önol FF, Antar B, Köse O, Erdem MR, Önol Ş Y. Techniques and results of urethroplasty for female urethral strictures: our experience with 17 patients. Urology. (2011) 77(6):1318–24. doi: 10.1016/j.urology.2011.01.017
19. Blaivas JG, Santos JA, Tsui JF, Deibert CM, Rutman MP, Purohit RS, et al. Management of urethral stricture in women. J Urol. (2012) 188(5):1778–82. doi: 10.1016/j.juro.2012.07.042
20. Goel A, Paul S, Dalela D, Sankhwar P, Sankhwar SN, Singh V. Dorsal onlay buccal mucosal graft urethroplasty in female urethral stricture disease: a single-center experience. Int Urogynecol J. (2014) 25(4):525–30. doi: 10.1007/s00192-013-2249-x
21. Kowalik C, Stoffel JT, Zinman L, Vanni AJ, Buckley JC. Intermediate outcomes after female urethral reconstruction: graft vs flap. Urology. (2014) 83(5):1181–5. doi: 10.1016/j.urology.2013.12.052
22. Berdondini E, Tosco L, Margara A, Giacobbe A, Collura D, Germinale F, et al. Minimally invasive buccal Mucosa dorsal graft for female distal urethroplasty. Eur Urolo Open Sci. (2021) 24:34–8. doi: 10.1016/j.euros.2020.12.001
23. Gupta P, Kalra S, Dorairajan LN, Manikandan R, Sreerag KS, Jagannath A. Dorsal onlay buccal mucosal graft urethroplasty in post radiation female urethral stricture—a technical appraisal with outcomes. Urology. (2021) 156:321. doi: 10.1016/j.urology.2021.06.006
24. Faiena I, Koprowski C, Tunuguntla H. Female urethral reconstruction. J Urol. (2016) 195(3):557–67. doi: 10.1016/j.juro.2015.07.124
25. Osman NI, Chapple CR. Contemporary surgical management of female urethral stricture disease. Curr Opin Urol. (2015) 25(4):341–5. doi: 10.1097/MOU.0000000000000186
26. Gormley EA, Lightner DJ, Burgio KL, Chai TC, Clemens JQ, Culkin DJ, et al. Diagnosis and treatment of overactive bladder (non-neurogenic) in adults: aUA/SUFU guideline. J Urol. (2012) 188(6 Suppl):2455–63. doi: 10.1016/j.juro.2012.09.079
27. Schwender CE, Ng L, McGuire E, Gormley EA. Technique and results of urethroplasty for female stricture disease. J Urol. (2006) 175(3 Pt 1):976–80.; discussion 80. doi: 10.1016/S0022-5347(05)00336-8
28. Simonato A, Varca V, Esposito M, Carmignani G. Vaginal flap urethroplasty for wide female stricture disease. J Urol. (2010) 184(4):1381–5. doi: 10.1016/j.juro.2010.06.042
29. Ma Y, Jian ZY, Hu Q, Luo Z, Jin T. Oral Mucosa vs. Penile skin flap in substitution urethroplasty for anterior urethral strictures: a systematic review and meta-analysis. Front Surg. (2021) 8:803750. doi: 10.3389/fsurg.2021.803750
30. Zhang K, Wang T, Cao S, Song L, Hu X, Zhang J, et al. Multi-Factorial analysis of recurrence and complications of lingual Mucosa graft urethroplasty for anterior urethral stricture: experience from a Chinese referral center. Urology. (2021) 152:96–101. doi: 10.1016/j.urology.2021.03.017
31. Yang K, Fan S, Wang J, Yin L, Li Z, Xiong S, et al. Robotic-assisted lingual mucosal graft ureteroplasty for the repair of Complex ureteral strictures: technique description and the Medium-term outcome. Eur Urol. (2022) 81(5):533–40. doi: 10.1016/j.eururo.2022.01.007
32. Liang C, Wang J, Hai B, Xu Y, Zeng J, Chai S, et al. Lingual mucosal graft ureteroplasty for long proximal ureteral stricture: 6 years of experience with 41 cases. Eur Urol. (2022) 82(2):193–200. doi: 10.1016/j.eururo.2022.05.006
33. Berglund RK, Vasavada S, Angermeier K, Rackley R. Buccal mucosa graft urethroplasty for recurrent stricture of female urethra. Urology. (2006) 67(5):1069–71. doi: 10.1016/j.urology.2005.12.010
34. Rehder P, Glodny B, Pichler R, Exeli L, Kerschbaumer A, Mitterberger MJ. Dorsal urethroplasty with labia minora skin graft for female urethral strictures. BJU Int. (2010) 106(8):1211–4. doi: 10.1111/j.1464-410X.2010.09240.x
35. Chauhan S, Yadav SS, Tomar V. Outcome of buccal mucosa and lingual mucosa graft urethroplasty in the management of urethral strictures: a comparative study. Urol Ann. (2016) 8(1):36–41. doi: 10.4103/0974-7796.165715
36. Sharma AK, Chandrashekar R, Keshavamurthy R, Nelvigi GG, Kamath AJ, Sharma S, et al. Lingual versus buccal mucosa graft urethroplasty for anterior urethral stricture: a prospective comparative analysis. Int J Urol. (2013) 20(12):1199–203. doi: 10.1111/iju.12158
37. Barbagli G, Vallasciani S, Romano G, Fabbri F, Guazzoni G, Lazzeri M. Morbidity of oral mucosa graft harvesting from a single cheek. Eur Urol. (2010) 58(1):33–41. doi: 10.1016/j.eururo.2010.01.012
38. Xiong S, Wang J, Zhu W, Yang K, Ding G, Li X, et al. Onlay repair technique for the management of ureteral strictures: a comprehensive review. BioMed Res Int. (2020) 2020:6178286. doi: 10.1155/2020/6178286
Keywords: female urethra stricture, oral mucosa graft, dorsal urethroplasty, urethral reconstruction, narrative review
Citation: Tao C, Jin X and Zhang H (2023) Dorsal oral mucosa graft urethroplasty for female urethral stricture reconstruction: A narrative review. Front. Surg. 10:1146429. doi: 10.3389/fsurg.2023.1146429
Received: 17 January 2023; Accepted: 6 March 2023;
Published: 21 March 2023.
Edited by:
Borko Stojanovic, University of Belgrade, SerbiaReviewed by:
Akhmad Mustafa, Dr. Hasan Sadikin General Hospital, IndonesiaMarta Bizic, University Children's Hospital, Serbia
© 2023 Tao, Jin and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hengshu Zhang MTM5MDUyNzAzMEBxcS5jb20=
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Chunqin Tao1
Chunqin Tao1 Hengshu Zhang
Hengshu Zhang