- 1Department of Orthopaedics, Lishui People's Hospital, The Sixth Affiliated Hospital of Wenzhou Medical University, The First Affiliated Hospital of Lishui University, Lishui, China
- 2Department of Orthopaedics, Longquan People’s Hospital, Longquan, China
Purpose: The aim of this study was to explore the treatment outcomes of a novel single lateral approach via fibular fracture line for patients with posterior pilon fractures.
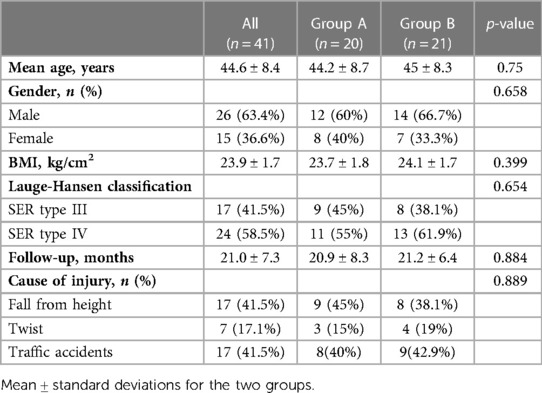
Patients and methods: From January 2020 to December 2021, a total of 41 patients with posterior pilon fractures who received surgical treatment in our hospital were retrospectively reviewed. Twenty patients (Group A) were treated with open reduction and internal fixation (ORIF) via posterolateral approach. Twenty-one patients (Group B) were treated with ORIF using a simple single lateral approach via stretching fibular fracture line. Clinical assessments, including operation time, intraoperative blood loss, the American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, visual analogue scale (VAS), and the active range of motion (ROM) of the ankle at the final follow-up visit after surgery, were performed in all patients. Radiographic outcome was evaluated by using the criteria proposed by Burwell and Charnley.
Results: The mean follow-up time was 21 months (range 12–35). The average operation time and intraoperative blood loss in the Group B were significantly less than those in the Group A. Moreover, the AOFAS score and ankle ROM in the Group B were significantly higher than those in the Group A at the final follow-up visit. Eighteen cases (90%) in Group A and 19 cases (90.5%) in Group B achieved anatomical reduction of the fracture.
Conclusion: The single lateral approach via stretching fibular fracture line is a simple and effective technique for reduction and fixation of posterior pilon fractures.
Introduction
Posterior articular fractures of the distal tibia include posterior malleolus fractures and posterior pilon fractures (1). Previous studies showed that posterior pilon fractures have a low incidence and variation in fracture morphology. Recently, posterior pilon fractures has gained increasing interest in clinical practice due to its poor outcome (2, 3). Anatomically, posterior pilon fractures extends to the medial malleolus (4, 5). Posterior pilon fractures are caused by rotation and axial load and characterized with large fracture fragments (6). Meanwhile, the treatment for this fracture type has been increasingly reported and remains a challenge. However, the best surgical approach for posterior pilon fractures has not been determined (7).
Currently, a single incisional posterolateral approach is often chosen for treating posterior pilon fractures (1). But this approach cannot fully expose the broken end of the bone and the articular surface of the distal tibia. In order to achieve clear visualization of the surgical field and minimal operative trauma, we innovatively used a simple single lateral approach via stretching fibular fracture line to treat posterior pilon fractures combined with a fibula fracture at the same level. The aim of the study was to evaluate the clinical efficacy of this surgical approach and promote its clinical application.
Material and methods
Study population
A retrospective analysis in 41 patients with posterior pilon fractures treated between January 2020 and December 2021 was conducted. Twenty patients (Group A) were treated with open reduction and internal fixation (ORIF) via posterolateral approach. Twenty-one patients (Group B) were treated with ORIF using a simple single lateral approach via stretching fibular fracture line. All surgeries were performed by the same team. This research was approved by the Ethics Committee of Lishui City People's Hospital and was in accordance with the Helsinki Declaration. All patients gave informed consent and signed informed consent.
Our inclusion criteria were (1) posterior pilon fractures combined with fibula fracture at the same level (2). Those who were treated with ORIF via posterolateral approach or lateral approach via stretching fibular fracture line. Our exclusion criteria were (1) Pathological fractures and open fractures (2) Those who cannot tolerate surgery (3) Follow-up data were incomplete and the follow-up time was less than 12 months.
Surgical approach
In the Group A, posterolateral approach was used for osteosynthesis of the posterior and lateral malleolus (8). In the Group B, we used a simple single lateral approach via stretching fibular fracture line to treat both posterior pilon fractures and fibular fractures (Figure 1). Two 2.0 mm Kirschner wires were placed at both ends of the fibula fracture line and inserted into both fibula and tibia. Then the Hintermann retractor was used to open the gap between the fibula fractures. Thus, the broken end of the tibia can be fully exposed. Surgeons can observe the articular surface of the distal tibia under direct vision and reduce and fix the posterior malleolus fracture block under direct vision. Ultimately, reduction and internal fixation of the fibula fracture was performed. Notably, this approach has less interference with the surrounding soft tissue. Conclusively, our novel approach allows for minimally invasive reduction and firm fixation.

Figure 1. Surgical procedure of a single lateral approach via stretching fibular fracture line. (A) A single lateral incision was used to expose the broken end of the fibula fracture. (B) The ankle joint was distracted with a Hintermann retractor to obtain sufficient working space. (C) A hollow guide needle was inserted from the anterior tibia to the posterolateral tibia to fix the posterior malleolus fracture. (D,E) Preoperative 3D reconstruction images. (F) Preoperative sagittal CT image. (G) Preoperative transverse CT image. (H) Intraoperative anterior–posterior x-ray image showed the fixation of the fracture with Kirschner wires. (I) Intraoperative lateral x-ray image showed the fixation of the posterior malleolus fracture with the Kirschner wire and the fracture reduction was mildly poor. (J) After adjustment, anatomic reduction with the Kirschner wire. (K) Postoperative anterior–posterior x-ray image. (L) Postoperative lateral x-ray image.
Assessments
All patients were followed up for over 12 months. Basic clinical information, operating time, and intraoperative blood loss were recorded. The time to fracture healing and the time to full bear weight were documented during the follow-up. The American Orthopaedic Foot and Ankle Society (AOFAS) ankle-hindfoot score, visual analogue scale (VAS), the active range of motion (ROM) of the ankle, and complications were recorded at regular follow-up after surgery. The radiological outcome was evaluated through standard XR using the criteria proposed by Burwell and Charnley (9).
Statistical methods
All statistical analyses were performed by using IBM SPSS Statistics 22.
Quantitative variables were shown in the form of mean ± standard deviation and a t-test was used for the comparison. Categorical variables were presented in the form of frequency (%) and a χ2 test and Fisher exact test were used for analyses. Variables with two-tailed p < 0.05 were considered statistically significant.
Results
Patient characteristics
There were 26 male and 15 female included in the study, aged 28–60 years (average age 44.6 years). Five patients were excluded, including two open fractures, two lost to follow-up, and one with less than 1 year of follow-up. The average BMI of all patients was 23.9 kg/cm2 (20.7–28.3). According to Lauge–Hansen classification, there were 17 cases of supination-external rotation (SER) type III ankle fracture, 24 of SER type IV ankle fracture. The causes of injury were falling from height (n = 17), twist (n = 7), and traffic accident (n = 17). The postoperative follow-up duration was 12–35 months (mean 21months). There was no significant difference between the two groups in age, gender, BMI, Lauge–Hansen classification, follow-up, and cause of injury (p > 0.05) (Table 1).
Clinical outcomes
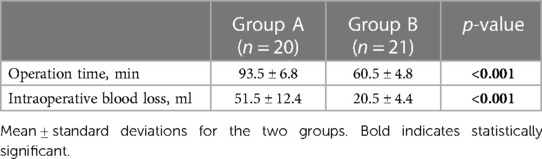
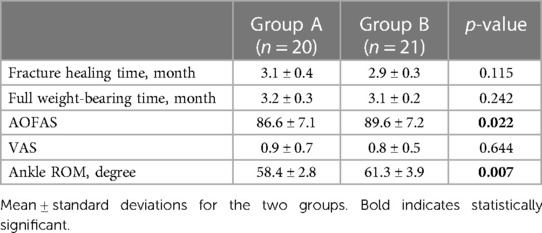
Group A had significantly more operation time and intraoperative blood loss than group B (p < 0.001) (Table 2). In terms of fracture healing time and full weight-bearing time, no significance was observed between the two groups (Table 3). Additionally, there was no significance in VAS between the two groups (Table 3). The mean AOFAS and ankle ROM in Group B was significantly higher than that in Group A at the final follow-up visit (p < 0.05) (Table 3).
According to the postoperative radiological examination, 18 cases (90%) in Group A and 19 cases (90.5%) in Group B achieved anatomical reduction of the fracture. Wound healing was satisfactory in all patients. No incision infection, deep vein thrombosis, and sural nerve injury occurred. No internal fixation failure and bone ununion were observed during the follow-up.
Discussion
In clinical practice, several approaches for posterior pilon fracture fixation have been reported (10–13). However, optimal approaches for minimizing the operative trauma and achieve effective internal fixation has not yet been established. In order to achieve satisfactory articular function outcomes, we innovatively used a simple single lateral approach via stretching fibular fracture line to treat posterior pilon fractures combined with a fibula fracture at the same level. This approach has the advantages of clear visualization of the surgical field and less soft tissue interference. Notably, when posterior pilon fractures are not accompanied by fibula fracture, this approach is not appropriate for treatment. To our knowledge, this is the first research that compared the clinical effect of posterior pilon fractures between the single lateral approach via stretching fibular fracture line and the posterolateral approach.
According to our results, the operation time in those who were treated with a single lateral approach via stretching fibular fracture line was shorter and the intraoperative blood loss in those patients was also less. This is mainly because application of a single lateral approach via stretching fibular fracture line can fully expose the articular surface of the distal tibia and collapsed articular surface with less soft tissue interference. Furthermore, posterior pilon fractures can be reduced and fixed under direct vision with less soft tissue interference.
The average AOFAS score was 86.6 points in Group A, which was similar with some previous studies (1, 4, 10). Moreover, Group B had more satisfactory clinical outcomes than Group A in terms of AOFAS and ankle ROM, suggesting the advantages of the lateral approach via stretching fibular fracture line in postoperative functional recovery. Additionally, high anatomical reduction rate (90.5%) was achieved by using this approach. This is mainly because the surgical approach gives full play to the function of the Hintermann retractor's distraction and reduction. Some studies applied a similar method-the transfibular approach for posterior malleolus fracture fixation (14–16). However, these studies did not use retractors for distraction and reduction, which may make anatomic reduction difficult. The results of our study suggest that a single lateral approach via stretching fibular fracture line for the treatment of posterior pilon fractures can achieve good clinical efficacy, which is worthy of clinical promotion and application.
Notably, there are some limitations presented in this study. First, the retrospective nature of this study can lead to bias. Second, the sample size included in this study was relatively small. Relevant clinical studies with larger sample sizes can be carried out in the future. Additionally, future multi-center, prospective, randomized controlled studies should be conducted to further confirm the clinical value of our innovative surgical approach. Nevertheless, this study lays a foundation for subsequent clinical research on posterior pilon fractures.
Conclusion
For posterior pilon fractures combined with fibula fractures at the same level, a simple single lateral approach via stretching fibular fracture line has good clinical effect and prognosis, which provides an alternative for the treatment of this kind of fracture.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Lishui City People's Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
XZ and WL: conceived and designed the study. WL, MZ, and ZJ: collected the data. WL, MZ, ZJ, and XM: performed the statistical analysis. WL: wrote the manuscript. XZ: revised it. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Gao M, Liu N, Cheng Y, Shi W, Yang H. Treatment outcomes of the posterolateral approach of plate fixation for posterior pilon fractures. Exp Ther Med. (2019) 17(5):4267–72. doi: 10.3892/etm.2019.7458
2. Quan Y, Lu H, Xu H, Liu Y, Xie W, Zhang B, et al. The distribution of posterior malleolus fracture lines. Foot Ankle Int. (2021) 42(7):959–66. doi: 10.1177/1071100721996700
3. Chaparro F, Ahumada X, Urbina C, Lagos L, Vargas F, Pellegrini M, et al. Posterior pilon fracture: epidemiology and surgical technique. Injury. (2019) 50(12):2312–7. doi: 10.1016/j.injury.2019.10.007
4. Zhang J, Wang H, Pen C, Qu WC, Duan L, Ren J, et al. Characteristics and proposed classification system of posterior pilon fractures. Medicine. (2019) 98(3):e14133. doi: 10.1097/MD.0000000000014133
5. Klammer G, Kadakia AR, Joos DA, Seybold JD, Espinosa N. Posterior pilon fractures: a retrospective case series and proposed classification system. Foot Ankle Int. (2013) 34(2):189–99. doi: 10.1177/1071100712469334
6. Switaj PJ, Weatherford B, Fuchs D, Rosenthal B, Pang E, Kadakia AR. Evaluation of posterior malleolar fractures and the posterior pilon variant in operatively treated ankle fractures. Foot Ankle Int. (2014) 35(9):886–95. doi: 10.1177/1071100714537630
7. Black AT, Stowers JM, Tran S, Mata K, Sherman AE, RahnamaVaghef A. Clinical outcomes for pilon variant posterior malleolar fractures: a multicenter retrospective analysis. J Foot Ankle Surg. (2022). doi: 10.1053/j.jfas.2022.04.007
8. Choi JY, Kim JH, Ko HT, Suh JS. Single oblique posterolateral approach for open reduction and internal fixation of posterior malleolar fractures with an associated lateral malleolar fracture. J Foot Ankle Surg. (2015) 54(4):559–64. doi: 10.1053/j.jfas.2014.09.043
9. Burwell HN, Charnley AD. The treatment of displaced fractures at the ankle by rigid internal fixation and early joint movement. J Bone Jt Surg Br Vol. (1965) 47(4):634–60. doi: 10.1302/0301-620X.47B4.634
10. Sukur E, Akman YE, Gokcen HB, Ozyurek EC, Senel A, Ozturkmen Y. Open reduction in pilon variant posterior malleolar fractures: radiological and clinical evaluation. Orthop Traumatol Surg Res. (2017) 103(5):703–7. doi: 10.1016/j.otsr.2017.05.012
11. Wang Y, Wang J, Luo CF. Modified posteromedial approach for treatment of posterior pilon variant fracture. BMC Musculoskelet Disord. (2016) 17:328. doi: 10.1186/s12891-016-1182-9
12. Amorosa LF, Brown GD, Greisberg J. A surgical approach to posterior pilon fractures. J Orthop Trauma. (2010) 24(3):188–93. doi: 10.1097/BOT.0b013e3181b91927
13. Hoekstra H, Rosseels W, Rammelt S, Nijs S. Direct fixation of fractures of the posterior pilon via a posteromedial approach. Injury. (2017) 48(6):1269–74. doi: 10.1016/j.injury.2017.03.016
14. Taki M, Hio N. The lateral trans-malleolar approach for posterior malleolar fracture of the ankle: a clinical and computed tomography evaluation. Foot Ankle Orthop. (2020) 5(4):2473011420S0046. doi: 10.1177/2473011420S00463
15. Gonzalez TA, Watkins C, Drummond R, Wolf JC, Toomey EP, DiGiovanni CW. Transfibular approach to posterior malleolus fracture fixation: technique tip. Foot Ankle Int. (2016) 37(4):440–5. doi: 10.1177/1071100715617760
Keywords: posterior pilon fracture, single lateral approach, posterolateral approach, fibular fracture line, treatment outcome
Citation: Liang W, Zhou M, Jiang Z, Mao X and Zhou X (2023) Treatment outcomes of posterior pilon fractures using a simple single lateral approach via stretching fibular fracture line. Front. Surg. 10:1141606. doi: 10.3389/fsurg.2023.1141606
Received: 10 January 2023; Accepted: 6 March 2023;
Published: 30 March 2023.
Edited by:
Xun Sun, Tianjin Hospital, China© 2023 Liang, Zhou, Jiang, Mao and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiang Zhou emhvdXhpYW5nd21jQDEyNi5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Wei Liang
Wei Liang Mingping Zhou1
Mingping Zhou1 Xiang Zhou
Xiang Zhou