- 1Department of Orthopedics, Shanghai Ninth People’s Hospital, School of Medicine, Shanghai Jiao Tong University, Shanghai, China
- 2Shanghai Key Laboratory of Orthopedic Implants, Department of Orthopedic Surgery, Shanghai Ninth People's Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
Intramedullary fixation is currently used to stabilize intertrochanteric fractures. Surgical reduction of the medial arch cortex is crucial to achieve stabilization of the internal fixation system, however, it is challenging to perform. To ensure anatomical reduction, we developed a novel surgical technique to assist in achieving accurate and convenient reduction. In this technique, right-angle forceps were used to pry and reset medial arch cortex fragments via a mini-helical blade incision. Noteworthily, all patients who underwent this technique achieved anatomical reduction with reduced operation times and bleeding. Our article illustrates intraoperative reduction techniques and summarizes tips and tricks that may be beneficial and educative for orthopedists.
1. Introduction
The incidence of intertrochanteric fractures is increasing with population aging, and the one-year mortality of this condition ranging from 14% to 36% (1). Fractures in elderly individuals with osteoporosis may be caused by accidental falls or minor trauma, and are usually treated surgically by closed reduction and internal fixation (2). Even if intramedullary nailing is reliable for the treatment of intertrochanteric fractures, especially involving medial or lateral wall destruction, the reduction of the medial arch cortex by closed manipulation is challenging. Research has suggested that adequate reduction of medial arch fracture fragments is important to achieve postoperative stability and rehabilitation of intertrochanteric fractures (3–5). Furthermore, understanding the deforming forces acting on various fracture patterns and using proper surgical techniques is important to ensure construct stability.
Several studies have previously indicated that point reduction clamps or even cerclage wire could contribute to reduction of the medial arch cortex fragments in subtrochanteric fractures, while causing great disturbance to surrounding soft tissues (6–9). However, to date, few studies have investigated irreducible medial arch fracture fragment displacement in patients with intertrochanteric fractures. In the current study, we made a mini-helical blade incision to palpate the medial arch fracture fragments, and then used right-angle forceps to reduce the displaced fracture fragments. This surgical technique has two novel aspects. First, the right-angle forceps interfere less with the soft tissues around the fracture fragments to minimize intraoperative bleeding. Second, this technique can be easily performed by an assistant surgeon, saves operation time, and is conducive to postoperative rehabilitation. Here, we describe the surgical techniques in detail.
2. Methods
2.1. Patients
Between June 2021 and March 2022, we operated on ten consecutive patients with displaced intertrochanteric fractures. Nine patients were female, and one was male, with an average age of 83.9 years. According to the latest AO/OTA classification (2018 edition), the fractures were categorized as 31-A1.3 in three cases, 31-A2.2 in five cases, 31-A3.1 in one case, and 31-A3.3 in one case. None of the patients had any other concomitant injury.
2.2. Position placement
Under general anesthesia, the patients were placed in the supine position on a radiolucent traction table. Antibiotic prophylaxis was administered approximately 30 min prior to the surgical incision. The involved lower limb was stabilized securely in the traction boot, and the limb was placed at approximately 10–15° in adduction, while the uninjured extremity was placed in abduction and flexion positions to facilitate intraoperative fluoroscopy. The foot must be handled with proper care to avoid skin abrasions. In addition, the upper trunk should be angled opposite to the fractured side to prevent obstruction of the entry point and guidewire insertion.
2.3. Surgical technique
The injury-to-surgery interval was 2 days on average (range, 1.5–4 days), and we were able to manage the reduction of the medial arch fracture fragments quickly and accurately during the operation.
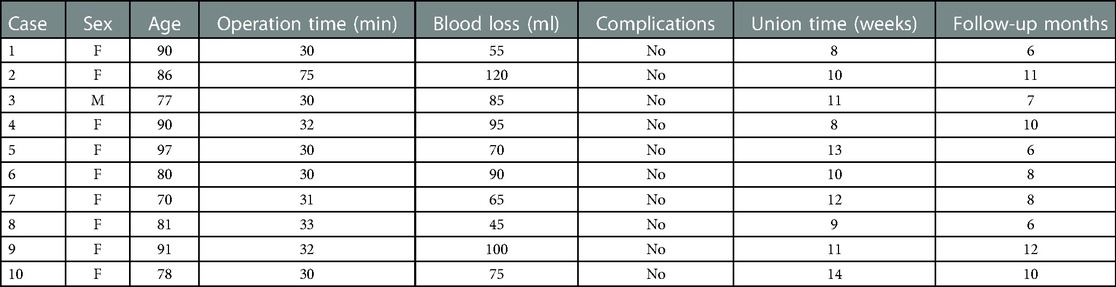
After restoring the neck shaft and anteversion angles on the traction table, a lateral incision was made starting approximately 2 cm proximal to the greater trochanter along the axis of the femur. The optimal entry point was confirmed by the cannulated awl according to intraoperative fluoroscopy and placed slightly more medial to the tip of the greater trochanter in the anteroposterior view and in the center of the femoral trochanter in the lateral view (Figure 1). The guidewire was advanced from the greater trochanter to the distal femur fragments, and the final position was confirmed by fluoroscopy, as eliciting a reduction of medial arch fragments may not be ideal. Minimally invasive reduction techniques were recommended when a femoral intramedullary nail was inserted. We used right-angle forceps that passed the lesser trochanter anteriorly and palpated the medial arch fracture fragments to assist in the reduction of the medial arch cortex through the mini-helical blade incision (Figure 2). The assistant surgeon pried the medial arch fracture fragments, and subsequently inserted the helical blade guide wire. Fluoroscopy confirmed that this procedure was successful at achieving anatomical reduction of the medial arch cortex (Figure 3). The reduction techniques not only inflicted limited intrusion to the soft tissues around the fractures, but were also easily manipulated by surgeons with minimal experience. Furthermore, it could resist the wedge effect when a femoral intramedullary nail was inserted. After the intramedullary nail became statically locked, the wound was irrigated with saline and closed in layers (Figure 4), and a suction drain was deemed not necessary.
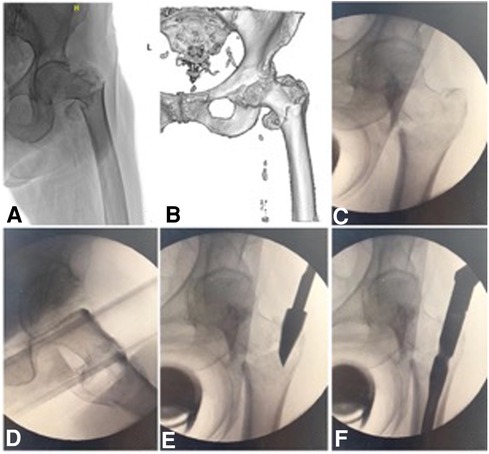
Figure 1. An 81-year-old woman with a comminuted intertrochanteric fracture, involving the medial arch and lateral wall was graded as AO/OTA 31-A2.2 (2018 edition). Preoperative x-ray (A) and CT scan (B) show the comminuted intertrochanteric fracture. (C,D), anteroposterior and lateral images show that the reduction was acceptable under axis traction. (E,F) The entry point was confirmed, and the displaced medial arch fragments developed after the femoral nail insertion.
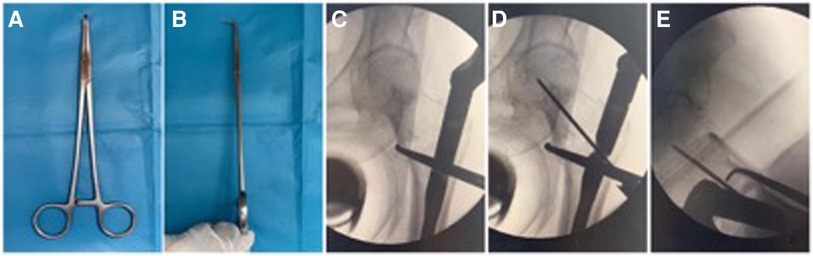
Figure 2. Right-angle forceps were used in the reduction of medial arch fragments. (A,B) shows the right-angle forceps. (C,D) The right-angle forceps were used to pry apart the medial arch fragments, and then the helical blade guide wire was inserted and confirmed under anteroposterior and lateral images.
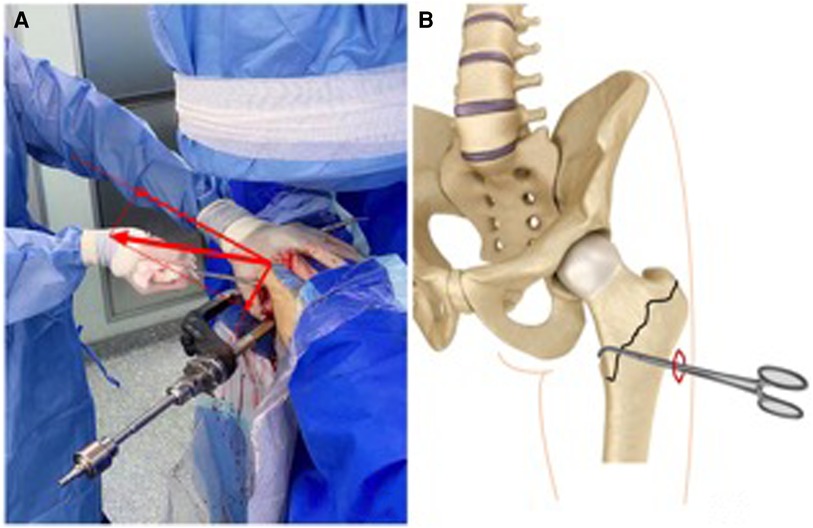
Figure 3. The minimally invasive reduction techniques were performed as follows: (A) the assistant surgeon palpated and pried the medial arch fragments. (B) Diagram of the minimally invasive reduction techniques: the right-angle forceps were passed anteriorly to assist the reduction of the medial arch fragments even the displaced lesser trochanter through the cephalomedullary incision.
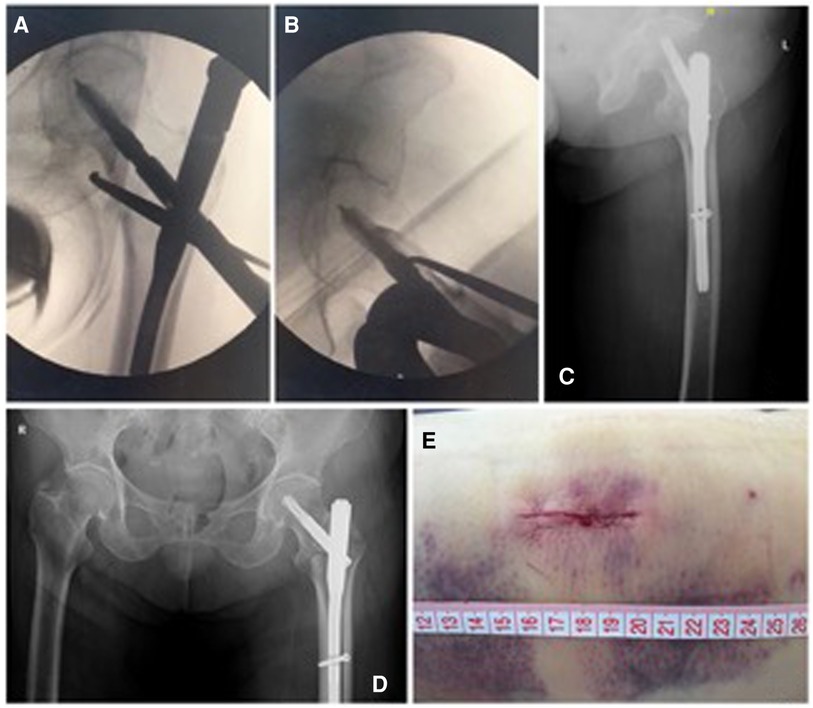
Figure 4. Routine maneuvers during nail fixation. (A,B) Anteroposterior and lateral views of the anatomical reduction and satisfactory fixation by PFNA. (C,D) Postoperative radiographs showing perfect fixation of the intertrochanteric fracture. (E) A minimal incision was used for reduction of the medial arch fragments and helical blade insertion.
In addition to the reduction of medial displaced fracture fragments, anteriorly displaced fragments could be reset effectively using our reduction techniques (Figure 5). By pressing the anteriorly displaced lesser trochanter fragment and resisting the wedge effect with right-angle forceps, the reduction of the medial arch fracture fragments could be successfully retained (Figure 6). Importantly, the entire operation time was dramatically reduced, which may guarantee the implementation of enhanced recovery after surgery (ERAS) and reduce the risk of postoperative complications. All patients had an average blood loss of 80 ml, and the mean operation time to manage these intertrochanteric fractures was 35 min (range, 30–75 min). Conventionally, low molecular weight heparin was applied postoperatively to prevent deep vein thrombosis.
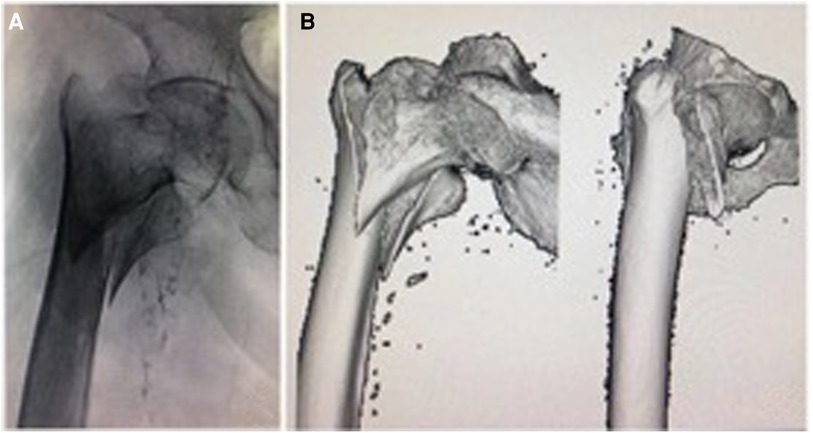
Figure 5. Intertrochanteric fracture in another patient, a 97-year-old woman, in which the medial arch was involved and displaced anteriorly. Preoperative x-ray (A) and CT scan (B) show that the intertrochanteric fracture and the medial arch fragment were displaced anteriorly.
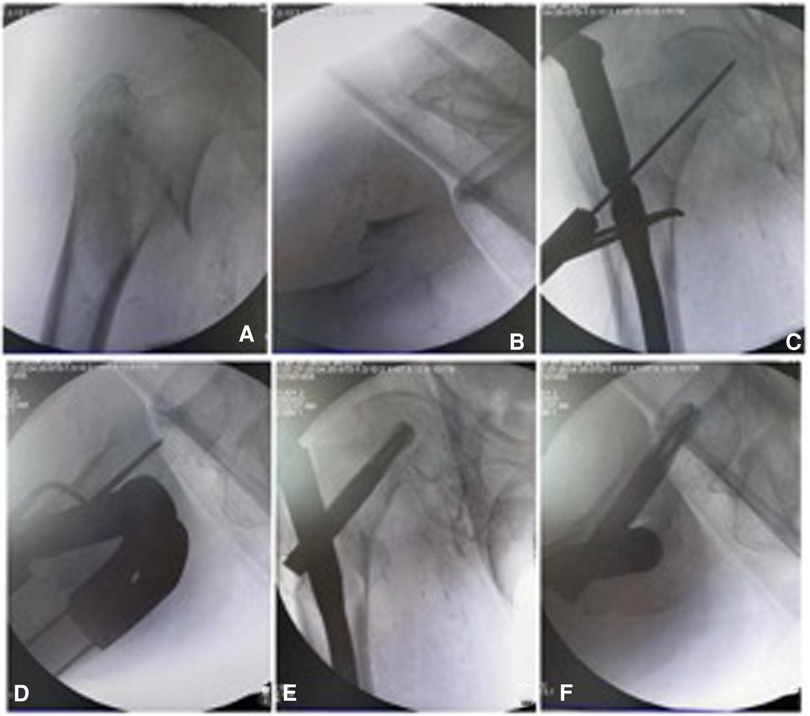
Figure 6. The right-angle forceps was used for reduction of the medial arch fragments. (A,B) Under axis traction, anteroposterior and lateral images show the medial arch fragment displaced anteromedially. (C,D) the right-angle forceps were used to pry the medial arch fragment, which was confirmed under anteroposterior and lateral images. (E,F) The helical blade was inserted and anatomical reduction of the medial arch was achieved.
3. Results
After applying the reduction techniques of right-angle forceps, all patients achieved anatomical reduction, especially of the displaced medial arch cortex, with reduced operation time and blood loss. No complications, such as infection, delayed union or nonunion, implant breakage, or helical blade cutoff, were observed in any of the patients, and routine follow-up was performed until fracture healing. (Table 1) The average follow-up time was 8.4 months. Finally, all patients returned to full weight-bearing when an obvious callus was found.
4. Discussion
Consensus on reduction and intramedullary nail fixation has become the optimum treatment for unstable intertrochanteric fractures among orthopedic surgeons, and anatomical reduction of fractures is significant following fixation and rehabilitation (10). The integrity of the medial arch is an important factor for the stability and healing of intertrochanteric fractures (5, 11, 12). Anatomical reduction of medial arch fracture fragments is of critical importance in intertrochanteric fractures. Many surgical reduction techniques have been applied to achieve satisfactory reduction of irreducible reverse intertrochanteric or subtrochanteric fractures, such as point reduction clamps, bone hooks, and Hohmann retractors (7, 13, 14). However, the limitations of these studies should be noted. These surgical reduction techniques might require open reduction or extended skin incision and can cause significant damage to the surrounding soft tissues, resulting in increased bleeding and operation time (15). In addition, cerclage was used, followed by disruption of the regional blood circulation and delayed fracture healing (16). Therefore, we developed a novel surgical technique to achieve reduction of the medial arch fracture fragments, even the lesser trochanter, using right-angle forceps through the mini helical blade incision without additional damage.
The morphological character of most medial arch fragments is the femoral neck connecting with the lesser trochanter along the sagittal plane, such as AO/OTA 31-A1.3 and 31-A2.3(2007 edition), resulting in a loss of anteromedial support, which is consistent with other research results (17). The lesser trochanter fracture fragment is displaced anteromedially under the traction of the iliacus, and it is difficult to achieve anatomical reduction by relying solely on traction and internal rotation of the lower limbs. Therefore, our novel reduction technique is suitable for these types of fractures. Crucially, the reduction techniques not only requires little intrusion into soft tissues around the fracture, but can also be easily performed by beginners. Moreover, it could resist the wedge effect when a femoral intramedullary nail was inserted. Research shows that prolonged operative duration is associated with postoperative complications, such as surgical site infection, urinary tract infection, pneumonia, and cardiac complications (18, 19). Importantly, our novel reduction techniques could reduce operation time, and be conducive to rapid postoperative recovery.
In addition to restoring fracture fragments satisfactorily, minimizing detrimental effects and complications has always been the goal of orthopedic surgeons. Although the number of patients treated with our novel surgical techniques in this study was small, we nevertheless found that this novel procedure guaranteed reduction of medial arch fragments, even in the lesser trochanter, with rapid recovery observed during follow-up. This novel surgical technique is simple and can be directly applied in the care of difficult intertrochanteric fractures, especially the reduction of medial arch fracture fragments. However, the limitations of our study should be noted as well. First, the number of relevant cases is small due to the outbreak of COVID-19. Second, it may be more convincing if more surgical teams use the novel surgical technique. Even so, we believe the novel surgical technique is simple and good in reduction of the medial arch fracture fragments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by The Institutional Review Board Research of Shanghai Ninth People's Hospital, Shanghai Jiaotong University School of Medicine. The patients/participants provided their written informed consent to participate in this study.
Author contributions
XL and XW contributed to design, and drafted the manuscript. CZ, GS, PL and JT contributed to implementation and interpretation of operations. FY contributed critically revised the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by National Natural Science Foundation of China (grant No. 81871791) and Shanghai Ninth People's Hospital Cross Research Fund of Medical Engineering (grant No. JYJC201915).
Acknowledgments
We are particularly grateful to all the people who have given us help on our article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lee WC, Chou SW, Tan CW, Chng LS, Yam GJM, Chua THI. Intertrochanteric fracture with distal extension: when is the short proximal femoral nail antirotation too short? Injury. (2021) 52(4):926–32. doi: 10.1016/j.injury.2020.10.059
2. Bhandari M, Swiontkowski M. Management of acute hip fracture. N Engl J Med. (2017) 377(21):2053–62. doi: 10.1056/NEJMcp1611090
3. Ren H, Ao R, Wu L, Jian Z, Jiang X, Yu B. Effect of lesser trochanter posteromedial wall defect on the stability of femoral intertrochanteric fracture using 3D simulation. J Orthop Surg Res. (2020) 15(1):242. doi: 10.1186/s13018-020-01763-x
4. Nie B, Chen X, Li J, Wu D, Liu Q. The medial femoral wall can play a more important role in unstable intertrochanteric fractures compared with lateral femoral wall: a biomechanical study. J Orthop Surg Res. (2017) 12(1):197. doi: 10.1186/s13018-017-0673-1
5. Zhang Y, Sun Y, Liao S, Chang S. Three-dimensional mapping of medial wall in unstable pertrochanteric fractures. Biomed Res Int. (2020) 2020:8428407.32596385
6. Mingo-Robinet J, Torres-Torres M, Moreno-Barrero M, Antonio Alonso J, García-González S. Minimally invasive clamp-assisted reduction and cephalomedullary nailing without cerclage cables for subtrochanteric femur fractures in the elderly: surgical technique and results. Injury. (2015) 46(6):1036–41. doi: 10.1016/j.injury.2015.01.019
7. Kokkalis ZT, Mavrogenis AF, Ntourantonis DI, Igoumenou VG, Antoniadou T, Karamanis R, et al. Reduction techniques for difficult subtrochanteric fractures. Eur J Orthop Surg Traumatol. (2019) 29(1):197–204. doi: 10.1007/s00590-018-2239-2
8. Yoon YC, Jha A, Oh CW, Durai SK, Kim YW, Kim JH, et al. The pointed clamp reduction technique for spiral subtrochanteric fractures: a technical note. Injury. (2014) 45(6):1000–5. doi: 10.1016/j.injury.2014.01.007
9. Gao YS, Guo YJ, Yu XG, Chen Y, Chen C, Lu NJ. A novel cerclage wiring technique in intertrochanteric femoral fractures treated by intramedullary nails in young adults. BMC Musculoskelet Disord. (2018) 19(1):359. doi: 10.1186/s12891-018-2284-3
10. Evaniew N, Bhandari M. Cochrane in CORR ®: intramedullary nails for extracapsular hip fractures in adults (review). Clin Orthop Relat Res. (2015) 473(3):767–74. doi: 10.1007/s11999-014-4123-7
11. Wang X, Zhang YQ, Zhang SM, Du SC, Chen K, Wang ZY. [Image study of anteromedial cortical morphology of intertrochanteric fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. (2019) 33(10):1260–4.31544436
12. Xiong WF, Zhang YQ, Chang SM, Hu SJ, Du SC. Lesser trochanteric fragments in unstable pertrochanteric hip fractures: a morphological study using three-dimensional computed tomography (3-D CT) reconstruction. Med Sci Monit. (2019) 25:2049–57. doi: 10.12659/MSM.913593
13. Hao YL, Zhang ZS, Zhou F, Ji HQ, Tian Y, Guo Y, et al. Predictors and reduction techniques for irreducible reverse intertrochanteric fractures. Chin Med J (Engl). (2019) 132(21):2534–42. doi: 10.1097/CM9.0000000000000493
14. Ruecker AH, Rueger JM. Pertrochanteric fractures: tips and tricks in nail osteosynthesis. Eur J Trauma Emerg Surg. (2014) 40(3):249–64. doi: 10.1007/s00068-013-0366-3
15. Chen W, Wang BJ, Bai XD, Gao H, Liu ZY, Li YD, et al. [Analysis of perioperative blood loss by fast track protocol in cephalomedullary nailing for geriatric intertrochanteric fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. (2019) 33(10):1265–9.31544437
16. Cebesoy O, Subasi M, Isik M. Cerclage cable in fracture: frustration or necessity? Int Orthop. (2011) 35(5):783–4; author reply 785. doi: 10.1007/s00264-011-1238-2
17. Zhang S, Zhang JY, Yang DM, Yang M, Zhang PX. [Morphology character and reduction methods of sagittally unstable intertrochanteric fractures]. Beijing Da Xue Xue Bao Yi Xue Ban. (2017) 49(2):236–41.28416831
18. Cheng H, Clymer JW, Chen BP, Sadeghirad B, Ferko NC, Cameron CG, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. (2018) 229:134–44. doi: 10.1016/j.jss.2018.03.022
Keywords: Intertrochanteric fractures, medial arch, right angle forceps, reduction techniques, enhanced recovery after surgery (ERAS)
Citation: Li X, Zhao C, Sun G, Liu P, Tang J, Yang F and Wang X (2023) Accurate reduction of medial arch fracture fragments in intertrochanteric fractures: A novel technical note. Front. Surg. 10:1140250. doi: 10.3389/fsurg.2023.1140250
Received: 8 January 2023; Accepted: 10 February 2023;
Published: 27 February 2023.
Edited by:
Carl Haasper, Orthopaedic Surgery Bremerhaven-Wesermünde, GermanyReviewed by:
Yao Lu, Xi’an Jiaotong University, ChinaWu Zhou, Huazhong University of Science and Technology, China
© 2023 Li, Zhao, Sun, Liu, Tang, Yang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoqing Wang b3N0ZW9ibGFzdEAxNjMuY29t Fei Yang ZmVpeWFuZ3luQDE2My5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Xiaodong Li
Xiaodong Li Chen Zhao
Chen Zhao Guantong Sun1,2
Guantong Sun1,2 Pengcheng Liu
Pengcheng Liu Xiaoqing Wang
Xiaoqing Wang