- 1Department of Orthopaedic Surgery, Third Hospital of Hebei Medical University, Shijiazhuang, China
- 2Key Laboratory of Biomechanics of Hebei Province, Third Hospital of Hebei Medical University, Shijiazhuang, China
- 3NHC Key Laboratory of Intelligent Orthopaedic Equipment, Third Hospital of Hebei Medical University, Shijiazhuang, China
- 4Chinese Academy of Engineering, Beijing, China
Objective: The aim of this study was to compare the clinical efficacy of close suction drainage (CSD) and no-CSD after a modified Stoppa approach for the surgical fixation of acetabular fractures.
Methods: This retrospective study included 49 consecutive acetabular fracture patients, who presented to a single level I trauma center for surgical fixation, using a modified Stoppa approach from January 2018 to January 2021. All surgeries were performed by a senior surgeon using the same approach, and the patients were divided into two groups based on whether CSD was used after the operation. Details of the patient demographics, fracture characteristics, intraoperative indicators, reduction quality, intra and postoperative blood transfusion, clinical outcomes, and incision-related complications were collected.
Results: No significant differences were found in the demographics, fracture characteristics, intraoperative indicators, reduction quality, clinical outcomes, and incision-related complications between the two groups (P > 0.05). The use of CSD was associated with a significantly higher postoperative blood transfusion volume (P = 0.034) and postoperative blood transfusion rate (P = 0.027). In addition, there was a significant difference in postoperative temperatures, especially on postoperative Day 2 (no-CSD 36.97 ± 0.51°C vs. CSD 37.34 ± 0.69°C, P = 0.035), and higher visual analogue scale (VAS) scores, especially on postoperative Day 1 (no-CSD 3.00 ± 0.93 vs. CSD 4.14 ± 1.43, P = 0.002) and 3 (no-CSD 1.73 ± 0.94 vs. CSD 2.48 ± 1.08, P = 0.013).
Conclusion: The results of this study suggest that routine use of CSD should not be recommended for patients with acetabular fractures after surgical fixation using a modified Stoppa approach.
1. Introduction
Acetabular fractures are usually caused by high-energy trauma, have an incidence of ∼3 out of every 100,000 patients per year, and are one of the most difficult fractures to manage in orthopedic surgery (1, 2). Because it is an intraarticular fracture, displaced acetabular fracture patients usually need surgical treatment (3). Many surgical approaches have been used to treat acetabular fractures, such as the iliofemoral, ilioinguinal, Kocher–Langenbeck, combined anterior/posterior, modified Stoppa, and extended iliofemoral approaches (4–6). The modified Stoppa approach was proposed by Cole and Bolhofner in 1994 and has been widely used in recent years (7). It is an ideal surgical fixation method for the majority of acetabular fractures, because it not only results in good exposure of the fracture area but also achieves a good reduction of fracture fragments, especially those involving the anterior column, anterior wall, and posterior hemitransverse, transverse, T-type, and both columns with predominately anterior displacement (2, 4, 8, 9).
In clinical applications, closed suction drainage (CSD) is often used as a preventive strategy to eliminate dead space and reduce the occurrence of postoperative wound complications, including hematoma formation, redness, infection, pain, and incisional hernia (10, 11). The application of CSD in open wound or infectious surgeries can play a role in draining pus and necrotic tissue debris, and its use in these cases was previously beyond doubt (11). However, there is little published evidence to support its routine use after surgery. Some literature suggests that the use of CSD may be associated with increased postoperative blood transfusion rates, days in hospital, and incision pain (10, 12). In addition, some have argued that CSD, as a foreign body, may become a potential source of infection, allowing external pathogens to enter deep wounds and increasing the chances of infection (13–15). Similar debates have been reported in the orthopedic spine and trauma literature (16, 17).
To prevent the formation of wound hematomas and enhance postoperative recovery, many orthopedic surgeons still routinely use CSD after using a modified Stoppa approach to treat acetabular fractures. However, we have found that the use of CSD will not provide any benefit to patients with acetabular fractures repaired using a modified Stoppa approach. Therefore, the aim of this study was to compare the clinical efficacy of CSD with no-CSD after a modified Stoppa approach in the surgical fixation of acetabular fractures.
2. Patients and methods
2.1. Patients
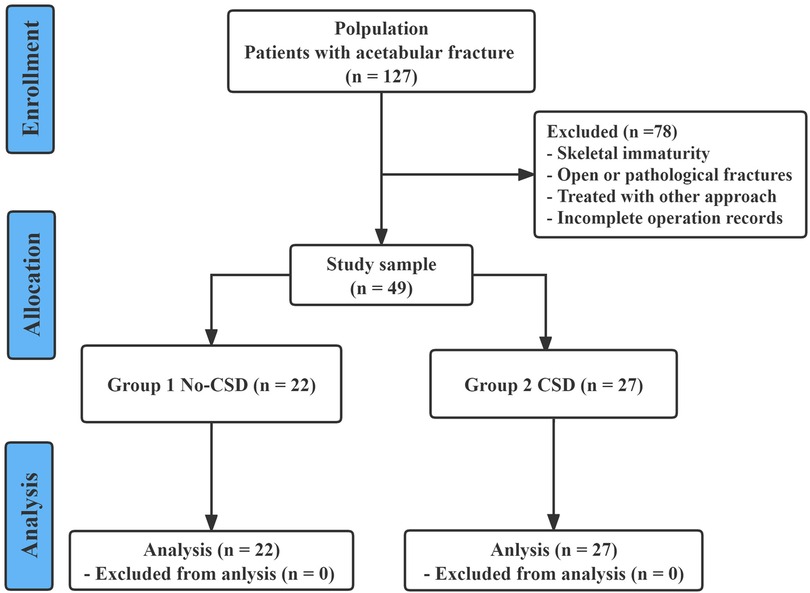
Between January 2018 and January 2021, a total of 127 skeletally mature patients with acetabular fractures were surgically treated in our level I trauma center. The inclusion criteria included the following: (1) adult patients aged 18 years or older; (2) diagnosis of an acute and closed acetabular fracture; (3) patients who underwent open reduction and internal fixation via a modified Stoppa approach; and (4) complete and available imaging and hospitalization data. The exclusion criteria were as follows: (1) open acetabular fractures; (2) previous history of acetabular fracture or bone tumor; (3) patients who underwent surgical treatment via another approach; and (4) patients with incomplete hospitalization and operation records. A total of 49 patients with acetabular fractures who underwent surgical treatment through a modified Stoppa approach were enrolled in our study for analysis. All 49 patients were divided into two groups according to whether CSD was used after surgery (in Group 1, 22 patients underwent no-CSD after surgery; in Group 2, 27 patients underwent CSD after surgery). Figure 1 shows a chart of the study design.
This study was approved by the Ethics Committee of Third Hospital of Hebei Medical University (Theoretical No. K2015-001-12) and conformed to the ethical standards of the Declaration of Helsinki, adopted in 1964, and its subsequent amendments. Signed informed consent was obtained from all patients.
2.2. Preoperative management
All patients were hemodynamically stable before the operation. When available, radiography and CT scans of the injured hip were performed in all patients to assess the extent of displacement. According to the imaging data results, these fractures were graded by the Judet–Letournel classification system (18). If no contraindication was present, low-molecular-weight heparin was given to the patients before the operation. For unstable fractures, bone traction or skin traction was used to facilitate intraoperative reduction.
2.3. Surgical techniques
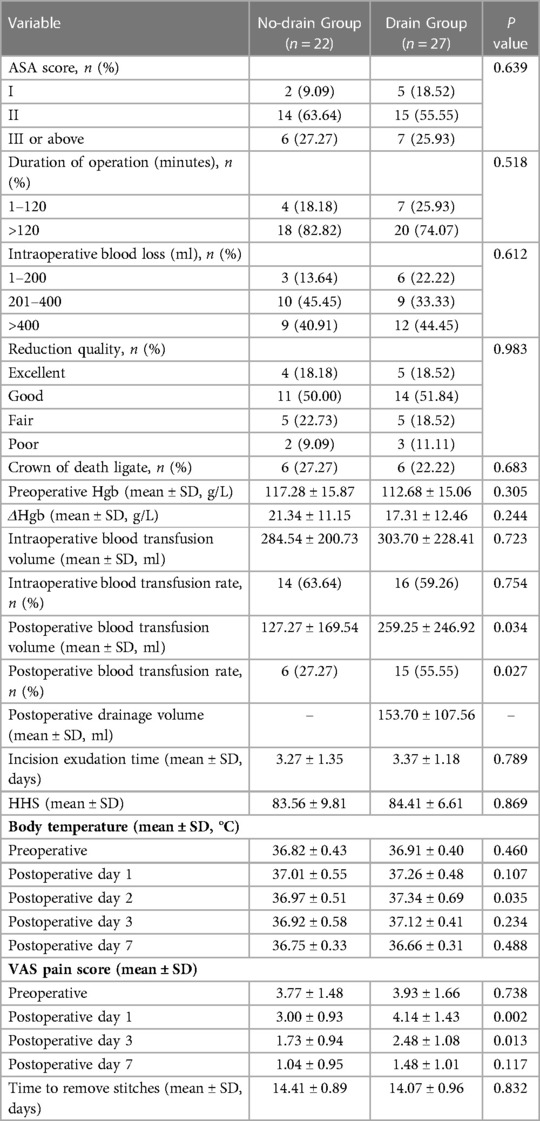
All patients underwent general anesthesia in the supine position during the operation. A vertical midline incision was made from approximately 2 cm below the umbilicus to 1 cm above the pubic symphysis joint. After making an incision along the alba line of the rectus abdominis muscle, blunt finger dissection was performed to detach the superior ramus of the pubis, releasing the periosteum and iliopectineal fascia, extending to the pelvic brim and the internal iliac fossa, and continuing to emerge laterally. During exposure, the anastomotic branches (corona mortis) between the internal and external iliac vessels were identified for protection. Tying or cauterization was performed to avoid bleeding if the corona mortis was damaged. Subperiosteal dissection was performed along the pelvic brim, exposing the fracture fragments. Attention was paid to identify and protect the obturator nerves and blood vessels during the further operation. Once the fracture site was exposed, reduction tools were used to attempt reduction and internal fixation. After confirmation by fluoroscopy, the wounds were closed in layers for the patients in Group 1. For the patients in Group 2, all surgical procedures were same as those in Group 1, except that a drain for CSD was placed before closing the wound (Figure 2).
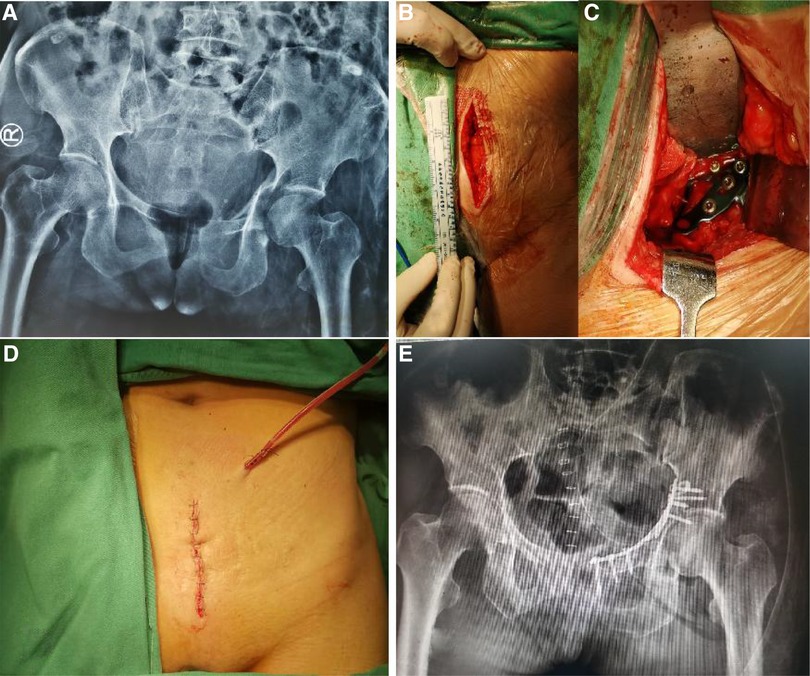
Figure 2. A female patient, 57 years old, with a T-type acetabular fracture who underwent surgical treatment via a modified stoppa approach. (A) preoperative anteroposterior pelvic radiograph; (B), picture of the incision of the modified Stoppa approach; (C), internal fixation was placed after fracture reduction; (D), a CSD was used after surgery; (E), postoperative anteroposterior pelvic radiograph.
2.4. Postoperative care
Patients in both groups received the same postoperative rehabilitation program. Low-molecular-weight sodium heparin was given to prevent deep vein thrombosis from 6 h to 4 weeks after surgery. The drain CSD was removed 48 h after surgery if the drainage did not exceed 50 ml/day. After surgery, the patients were encouraged to perform passive hip mobility as soon as possible. According to the general condition of the patient, the severity of the injury, and the quality of the reduction and fixation, the patients were guided to perform gradual rehabilitation exercises.
2.5. Observation index
In the present study, demographic characteristics, fracture characteristics, and medical records, including operative reports and inpatient progress notes, were collected retrospectively and compared between the two groups. The primary outcome measures were perioperative hemoglobin changes, postoperative blood transfusion volume and rate, and postoperative clinical outcomes. The secondary outcome measures included changes in body temperature from before surgery and on postoperative Day 1, 2, 3, and 7, as well as incision-related complications. Data on the duration of operation, intraoperative blood loss, and corona mortis ligation were obtained from the operation records. Data on the preoperative hemoglobin (Hgb) and intra and postoperative blood transfusion volume and rate were obtained from the inpatient progress notes. ΔHgb was expressed as the Hgb change from immediately before to after surgery. The Harris hip score (HHS) was used to evaluate the function of the hip after surgery. Visual analogue scale (VAS) scores were used to evaluate the degree of pain before surgery and on postoperative Day 1, 3, and 7. Incision-related complications mainly included wound infections, wound dehiscence, hematomas, and non-union. Wound-related complications and other perioperative issues were followed up for at least one year.
2.6. Statistical analysis
The analyses were performed using SPSS 23.0 software (IBM, Armonk, New York). Measurement data were expressed as the mean ± SD or numbers and percentages (%). The Kolmogorov–Smirnov test was used to confirm a normal distribution. Potential explanatory variables were evaluated using a chi-square test or Fisher's test for categorical variables and independent-samples t tests or Mann–Whitney U tests for continuous variables. The level of significance was set at P < 0.05.
3. Results
3.1. Patient and fracture characteristics
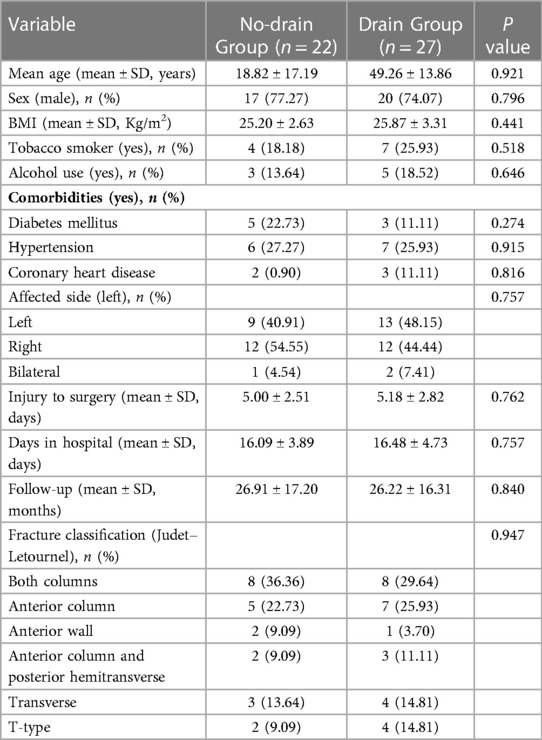
In the present study, 49 patients with acetabular fractures who met our screening criteria were enrolled in the analysis, of whom 37 were male and 12 were female (mean age: 49.06 ± 15.28; range: 21–80 years). Among them, 22 patients (44.9%) did not use CSD after surgery via a modified Stoppa approach and were enrolled in Group 1. According to the Judet–Letournel classification, there were six fracture types managed by a single modified Stoppa approach, including column fractures (16/49, 32.7%), anterior column fractures (12/49, 24.5%), anterior wall fractures (3/49, 6.1%), anterior column and posterior hemitransverse fractures (5/49, 10.2%), transverse fractures (7/49, 14.3%), and T-type fractures (6/49, 12.2%). All fracture types were identified by the same senior orthopedic surgeon according to the preoperative radiographs and CT scans. There were no significant differences in demographics or fracture classifications between the two groups (Table 1).
3.2. Perioperative-related indicators
Perioperative variables are shown in Table 2. There were no significant differences observed in intraoperative indicators between the two groups, including the duration of operation, intraoperative blood loss, reduction quality, corona mortis ligation, preoperative Hgb, changes in Hgb from immediately before to after surgery (ΔHgb), and intraoperative blood transfusion volume and rate. While the postoperative blood transfusion volume and rate tended to be higher in the CSD group than in the no-CSD group, the differences were statistically significant (P = 0.034 and P = 0.027, respectively). There were no significant intergroup differences in incision exudation time (P = 0.789) or HHS (P = 0.869). Preoperatively, no significant differences were found in body temperature or VAS pain score between the two groups. Postoperatively, there were significant intergroup differences in body temperature on postoperative Day 2 (no-CSD group, 36.97 ± 0.51°C vs. CSD group, 37.34 ± 0.69°C; P = 0.035) and VAS pain score on postoperative Day 1 (no-CSD group, 3.00 ± 0.93 vs. CSD group,4.14 ± 1.43; P = 0.002) and 3 (no-CSD group,1.73 ± 0.94 vs. CSD group, 2.48 ± 1.08; P = 0.013).
3.3. Postoperative incision-related complications
There were no significant differences in postoperative incision-related complications between the two groups (P > 0.05). Three patients (3/22) in the no-CSD group and five patients (5/27) in the CSD group suffered superficial wound infections that were completely improved by effective antibiotics. Two patients (2/22) in the no-CSD group and three patients (3/27) in the CSD group developed a hematoma, which was absorbed after one week of local physiotherapy. All specific data on incision-related complications are summarized in Table 3.
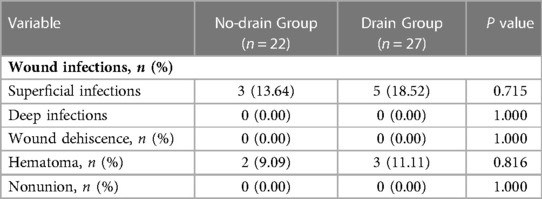
Table 3. Detailed presentation of postoperative incision-related complications between the two groups.
4. Discussion
To our knowledge, our study is the first to evaluate whether using CSD has an impact on the clinical outcome of acetabular fractures treated by a modified Stoppa approach. Previous studies have suggested that CSD could be used as a preventive treatment to decrease the likelihood of surgical site infection and incision-related complications in high-risk patients after orthopedic surgery (10, 19). However, according to our study results, compared to the patients in the no-CSD group, the patients with CSD for acetabular fractures repaired by a modified Stoppa approach were associated with a higher risk of postoperative blood transfusion and pain, with no impact on clinical outcomes and incision-related complications.
Acetabular fracture is one of the most difficult fractures to manage in orthopedic surgery. An ideal surgical approach for acetabular fractures is invaluable. It not only facilitates good exposure of the surgical field and effective reduction of the fracture but also causes as few complications as possible (2). The modified Stoppa approach is only appropriate in specific surgical indications and does not often allow for posterior column access if needed. This approach has many advantages, including large areas of visualization, less chance of damaging major nerves and vessels, short operation time, and less trauma (4, 20).
Traditionally, CSD has been successfully used in the management of acute and chronic open wounds to decrease the incidence of hematomas and infection by reducing the accumulation of blood and exudate in the incision cavity (10, 21, 22). In recent years, researchers have tried to apply CSD to closed incisions for acetabular fractures to prevent surgical site infection and wound complications after surgery (19). A retrospective study by Reddix et al. (23) showed that the use of CSD in patients with acetabular fracture may significantly reduce the incidence of deep infections. Although certain high-risk patients with acetabular fractures, such as obese patients, may benefit from treatment with CSD, the use of CSD remains controversial. For example, the results published by Boissonneault et al. (24) show that, in their study, the use of CSD after the surgical fixation of acetabular fractures via the Kocher–Langenbeck approach significantly increased postoperative blood transfusion rates and days in hospital, but wound complications and incision infection rates did not differ.
Similarly, in the current study, the patients in the CSD group showed higher postoperative transfusion volumes (259.25 ml vs. 127.27 ml, P = 0.034) and transfusion rates (55.55% vs. 27.27%, P = 0.027) than those in the no-CSD group. Some scholars believe that 24–48 h after surgery is the stage of maximum bleeding and seepage of surgical sites (25). Negative pressure suction caused the exudate to continue to drain outside the body and disrupted the self-coagulation mechanism, which were the main reasons for the increase in postoperative blood transfusion (25). In fact, prophylactic CSD after acetabular fractures remains controversial. The use of CSD is almost always determined by the surgeon after surgery based on the quality of intraoperative hemostasis, magnitude of the surgical procedure, and experience (17, 26).
Several authors have reported that the advantages of using CSD after acetabular fracture surgery were controlling postoperative wound drainage and preventing local accumulation of hematomas (27). However, Kim et al. (28) found that routine use of CSD not only failed to prevent or reduce postoperative morbidities but also may have led to prolonged postoperative pain. Some published studies confirmed that the application of CSD may produce undesired results, such as an increased risk of infection and pain and an increased length of hospital stay after surgery. In addition, some studies suggested that compared with the CSD group, the VAS scores of the patients in the no-CSD group decreased by 50%, especially on postoperative Day 2 (26).
In our study, we found that there was no increase in the frequency of incision-related complications in the no-CSD group. A total of three patients (11.11%) developed hematomas and five (18.52%) developed superficial infections in the CSD group, which were no significant difference from those in the no-CSD group. Theoretically, the use of CSD is beneficial to reduce the incidence of pain and fever. However, our findings were the opposite, with the patients in the CSD group having higher VAS scores on postoperative Day 1 (CSD group, 4.14 ± 1.43 vs. no-CSD group, 3.00 ± 0.93; P = 0.002) and 3 (CSD group, 2.48 ± 1.08 vs. no-CSD group, 1.73 ± 0.94; P = 0.013) and higher temperatures on postoperative Day 2 (CSD group, 37.34 ± 0.69°C vs. no-CSD group, 36.97 ± 0.51°C; P = 0.035) than the patients in the no-CSD group. We believed that the drain itself, similar to a foreign body, increased discomfort and anxiety. In addition, active pulling and removal can also increase patient pain, and the absorption of residual exudate in the cavity after removal of the drain can cause fever.
This study has several potential limitations, including the retrospective design with the associated bias. The small sample size from a single institution was also a main limitation. In addition, the retrospective evaluation of intra and postoperative blood loss from medical records may lead to concerns about the reliability of this study. We only compared and analyzed a few perioperative laboratory indicators, while other indicators, such as white blood cell count and platelet count, were not addressed. Furthermore, we only compared the placement of drains after treating acetabular fractures via a modified Stoppa approach and did not include other approaches or the number of drains. Finally, although it is an important evaluation indicator in the perioperative period of hip fracture, the incidence of deep vein thrombosis was not included due to incomplete data. We will conduct further research in the future.
5. Conclusions
It is unnecessary to use CSD routinely after treating acetabular fractures via a modified Stoppa approach, because the application of CSD will not effectively reduce the incidence of postoperative incision-related complications and will increase the risk of increased postoperative blood transfusion rate and pain.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
LJ and ZW: interpreted the data and wrote the manuscript; KZ and XL: collected and analyzed the data; WC and YZ: revised the manuscript; ZH: designed and revised the final manuscript. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Natural Science Foundation of Hebei (grant number: H2020206193).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Laird A, Keating JF. Acetabular fractures: a 16-year prospective epidemiological study. J Bone Joint Surg Br. (2005) 87(7):969–73. doi: 10.1302/0301-620X.87B7.16017
2. Meena S, Sharma PK, Mittal S, Sharma J, Chowdhury B. Modified stoppa approach versus ilioinguinal approach for anterior acetabular fractures; A systematic review and meta-analysis. Bull Emerg Trauma. (2017) 5(1):6–12.28246617
3. Matta JM, Merritt PO. Displaced acetabular fractures. Clin Orthop Relat Res. (1988) (230):83–97.3365902
4. Kilinc CY, Acan AE, Gultac E, Kilinc RM, Hapa O, Aydogan NH. Treatment results for acetabulum fractures using the modified stoppa approach. Acta Orthop Traumatol Turc. (2019) 53(1):6–14. doi: 10.1016/j.aott.2018.11.003
5. Bray TJ, Esser M, Fulkerson L. Osteotomy of the trochanter in open reduction and internal fixation of acetabular fractures. J Bone Joint Surg Am. (1987) 69(5):711–7. doi: 10.2106/00004623-198769050-00012
6. Kloen P, Siebenrock KA, Ganz R. Modification of the ilioinguinal approach. J Orthop Trauma. (2002) 16(8):586–93. doi: 10.1097/00005131-200209000-00008
7. Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. (1994) 305:112–23. doi: 10.1097/00003086-199408000-00015
8. Zou R, Wu M, Guan J, Xiao Y, Chen X. Clinical results of acetabular fracture via the pararectus versus ilioinguinal approach. Orthop Surg. (2021) 13(4):1191–5. doi: 10.1111/os.12970
9. Al Adawy AS, Aziz AHA, El Sherief FA, Mahmoud WS, Mabrook M, Hassan YE. Modified stoppa as an alternative surgical approach for fixation of anterior fracture acetabulum: a randomized control clinical trial. J Orthop Surg Res. (2020) 15(1):154. doi: 10.1186/s13018-020-01660-3
10. Crist BD, Oladeji LO, Khazzam M, Della Rocca GJ, Murtha YM, Stannard JP. Role of acute negative pressure wound therapy over primarily closed surgical incisions in acetabular fracture ORIF: a prospective randomized trial. Injury. (2017) 48(7):1518–21. doi: 10.1016/j.injury.2017.04.055
11. Zhang JZ, Zhao K, Li JY, Meng HY, Zhu YB, Zhang YZ. Prophylactic closed suction drainage is irrelevant to accelerated rehabilitation after open reduction and internal fixation for closed distal femur fractures. Orthop Surg. (2020) 12(6):1768–75. doi: 10.1111/os.12812
12. Parker MJ, Livingstone V, Clifton R, McKee A. Closed suction surgical wound drainage after orthopaedic surgery. Cochrane Database Syst Rev. (2007) 2007(3):Cd001825.17636687
13. Sankar B, Ray P, Rai J. Suction drain tip culture in orthopaedic surgery: a prospective study of 214 clean operations. Int Orthop. (2004) 28(5):311–4. doi: 10.1007/s00264-004-0561-2
14. Gurusamy KS, Allen VB. Wound drains after incisional hernia repair. Cochrane Database Syst Rev. (2013) (12):Cd005570. doi: 10.1002/14651858.CD005570.pub4
15. Arbadoro P, Marmorale C, Recanatini C, Mazzarini G, Pellegrini I, D'Errico MM, et al. May the drain be a way in for microbes in surgical infections? Am J Infect Control. (2016) 44(3):283–8. doi: 10.1016/j.ajic.2015.10.012
16. Magnussen RA, Tressler MA, Obremskey WT, Kregor PJ. Predicting blood loss in isolated pelvic and acetabular high-energy trauma. J Orthop Trauma. (2007) 21(9):603–7. doi: 10.1097/BOT.0b013e3181599c27
17. Andrew Glennie R, Dea N, Street JT. Dressings and drains in posterior spine surgery and their effect on wound complications. J Clin Neurosci. (2015) 22(7):1081–7. doi: 10.1016/j.jocn.2015.01.009
18. Zhang R, Yin Y, Li A, Wang Z, Hou Z, Zhuang Y, et al. Three-column classification for acetabular fractures: introduction and reproducibility assessment. J Bone Joint SurgAm. (2019) 101(22):2015–25. doi: 10.2106/JBJS.19.00284
19. Stannard JP, Volgas DA, McGwin G, Rena LS, William O, Thomas M, et al. Incisional negative pressure wound therapy after high-risk lower extremity fractures. J Orthop Trauma. (2012) 26(1):37–42. doi: 10.1097/BOT.0b013e318216b1e5
20. Kim HY, Yang DS, Park CK, Choy WS. Modified stoppa approach for surgical treatment of acetabular fracture. Clin Orthop Surg. (2015) 7(1):29–38. doi: 10.4055/cios.2015.7.1.29
21. Suzuki T, Minehara A, Matsuura T, Kawamura T, Soma K. Negative-pressure wound therapy over surgically closed wounds in open fractures. J Orthop Surg. (2014) 22(1):30–4. doi: 10.1177/230949901402200109
22. Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. (1997) 38(6):553–62. doi: 10.1097/00000637-199706000-00001
23. Reddix RN, Leng XI Jr, Woodall J, Jackson B, Dedmond B, Webb LX. The effect of incisional negative pressure therapy on wound complications after acetabular fracture surgery. J Surg Orthop Adv. (2010) 19(2):91–7.20727304
24. Boissonneault AR, Schenker M, Staley C, Roorbach M, Erwood AA, Grabel ZJ, et al. Impact of closed suction drainage after surgical fixation of acetabular fractures. Arch Orthop Trauma Surg. (2019) 139(7):907–12. doi: 10.1007/s00402-019-03110-0
25. Reddix RN, Tyler HK Jr, Kulp B, Webb LX. Incisional vacuum-assisted wound closure in morbidly obese patients undergoing acetabular fracture surgery. Am J Orthop. (2009) 38(9):446–9.19911098
26. Schietroma M, Pessia B, Bianchi Z, De Vita F, Carlei F, Guadagni S, et al. Thyroid surgery: to drain or not to drain, that is the problem—a randomized clinical trial. ORL J Otorhinolaryngol Relat Spec. (2017) 79(4):202–11. doi: 10.1159/000464137
27. Sen O, Kizilkilic O, Aydin MV, Yalcin O, Erdogan B, Cekinmez M, et al. The role of closed-suction drainage in preventing epidural fibrosis and its correlation with a new grading system of epidural fibrosis on the basis of MRI. Eur Spine J. (2005) 14(4):409–14. doi: 10.1007/s00586-004-0801-6
Keywords: acetabular fracture, close suction drainage, modified stoppa approach, surgical method, treatment
Citation: Jin L, Wang Z, Zhao K, Lian X, Chen W, Zhang Y and Hou Z (2023) Drain vs. no-drain for acetabular fractures after treatment via a modified stoppa approach: A retrospective study. Front. Surg. 10:1133744. doi: 10.3389/fsurg.2023.1133744
Received: 29 December 2022; Accepted: 23 February 2023;
Published: 17 March 2023.
Edited by:
Paphon Sa-ngasoongsong, Mahidol University, ThailandReviewed by:
Mitchell K. Ng, Maimonides Medical Center, United StatesShuisheng Yu, Second Hospital of Anhui Medical University, China
© 2023 Jin, Wang, Zhao, Lian, Chen, Zhang and Hou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiyong Hou ZHJ6eWhvdUBnbWFpbC5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Lin Jin
Lin Jin Zhongzheng Wang
Zhongzheng Wang Kuo Zhao1,2
Kuo Zhao1,2 Wei Chen
Wei Chen Zhiyong Hou
Zhiyong Hou