- 1Department of Orthopedic Surgery and Orthopedic Research Institute, West China Hospital, Sichuan University, Chengdu, China
- 2Department of Obstetrics and Gynecology, Ruijin Hospital, Shanghai Jiaotong University School of Medicine, Shanghai, China
Introduction: Most women of reproductive age suffered from the primary dysmenorrhea (PD). Up to date, most studies on the etiology of dysmenorrhea focused on endocrine factors while ignored the effect of spino-pelvic bony anatomy on uterus. In this study, we innovatively shed light on the relationship between primary dysmenorrhea and sagittal spino-pelvic alignment.
Materials and Methods: 120 patients diagnosed with primary dysmenorrhea and a control group of 118 healthy volunteers were enrolled into this study. All subjects received the standing full-length posteroanterior plain radiography to evaluate the sagittal spino-pelvic parameters. The visual analog scale (VAS) was used to assess pain rating of primary dysmenorrhea patients. Analysis of variance (ANOVA) or Student's t test was performed to measure statistical significance between differences.
Results: There was a significant difference in pelvic incidence (PI), sacral slope (SS), lumbar lordosis (LL) and thoracic kyphosis (TK) between PD group and Normal group (P<0.05). Furthermore, in PD group, the PI and SS was significant different between mild pain group and moderate pain group (P<0.05) and there was a significant negative correlation between pain rating and SS. From the perspective of sagittal spinal alignment, the majority of PD patients were classified with Roussouly type 2, meanwhile most normal people were classified with Roussouly type 3.
Conclusion: Sagittal spino-pelvic alignment was related to primary dysmenorrhea symptoms. Lower SS and PI angles may contribute to a worsen pain in PD patients.
Introduction
Primary dysmenorrhea (PD) is one of the most complained diseases among adolescence and childbearing age female. Women of reproductive age are reported to suffer from dysmenorrhea to the extent of 16%-91%, with a higher incidence in adolescents observed in 56.1% to 93.0% (1–4). In addition to the high prevalence rate, a series of related symptoms often lead to impairment in quality of life (5–7). The symptoms associated with dysmenorrhea include gastrointestinal symptoms such as nausea, bloating, diarrhea, constipation, or both, along with vomiting and indigestion. Also, irritability, headache, and low back pain are prevalent among women presenting with primary dysmenorrhea.
The etiology of PD is not fully elucidated. Since no organic lesion was detected in primary dysmenorrhea, there were various possible pathogenic factors reported in the previous literature such as overproduction of uterine PGs, psychological factors, vasoconstriction caused by the increase of vasopressin level and adverse uterine position (8).
However, patho-physiologic rather than anatomical factors are more stressed in the present literature discussing the etiology of PD. Since Roussouly etal. reported the classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis (9), the spino-pelvic sagittal alignment has attracted more and more attention in recent years. Spinopelvic imbalance may lead to low back pain(LBP) and LBP-related disabilities (10, 11). There are no studies now have been reported on the relationship between primary dysmenorrhea and the sagittal lumbar-pelvic alignment. The mismatch lumbar-pelvic parameters may affect the muscleskeleton system of the pelvis cavity, which could further lead to the adverse uterine position, and may be one of the causes of dysmenorrhea in some women. This study was aimed to illustrate the relationship between lumbar-pelvic alignment and primary dysmenorrhea.
Patients and methods
A retrospective study design was conducted to investigate the relationship between spino-pelvic alignment and primary dysmenorrhea.We enrolled 120 patients (24.7 ± 3.8 years old) diagnosed with primary dysmenorrhea and a control group of 118 healthy volunteers (23.5 ± 3.6 years old) without any uterine diseases or musculoskeletal disorders such as low back pain in the outpatient clinic of our department of West China hospital from July 2018 until May 2021. The exclusion criteria were: 1. Scoliosis or any congenital deformity of lumbosacral segment; 2. history of spinal or abdominal surgery; 3. smoking; 4. history of anxiety, depression, or severe mental disease; 5. obesity, defined as body mass index (BMI) > 25.0; and 6. history of taking oral contraceptive pills; 7. history of delivery.; 8. history of gynecological disease. All experimental procedures and methods were approved by the research ethics committee of the West China hospital and provided informed consent. All protocols were conducted in accordance with the research principles set forth in the Declaration of Helsinki.
Clinical symptoms assessment
The visual analog scale (VAS) was used to assess lower abdominal pain of primary dysmenorrhea. And the patients were divided into three groups: (1) mild pain (1–3 scores), which can be tolerated and have little affect on daily life and sleep quality; (2) moderate pain (4–6 scores), evident pain affecting sleep but tolerable after simple treatment; (3) severe pain (7–10 scores), progressively intensive pain that is intolerable and requires specialized treatment for its relief.
Radiographic assessment
All subjects underwent standing full-length posteroanterior plain radiography. All radiological parameters were measured by two attending spinal surgeons, and the average values were adopted. The radiographic measurements included the following: lumbar lordosis (LL) was measured as the angle between the upper end plates of L1 and S1; Thoracic kyphosis (TK) was measured as the angle between the upper endplate of T5 and the lower endplate of T12; C7-sagittal vertical axis (SVA) was measured as the distance between the C7 plumb line and the posterosuperior border of S1; pelvic incidence (PI) was measured as the angle between a vertical line perpendicular to the sacral endplate at its midpoint and a line connecting the midpoint of the sacral endplate and the midpoint of a line connecting the centers of the two femoral heads; sacral slope (SS) was measured as the angle between the horizontal plane and the sacral plate (Figure 1A). And the PD patients were grouped by radiographic results according to the Roussouly classification (9) (Figure 1B).
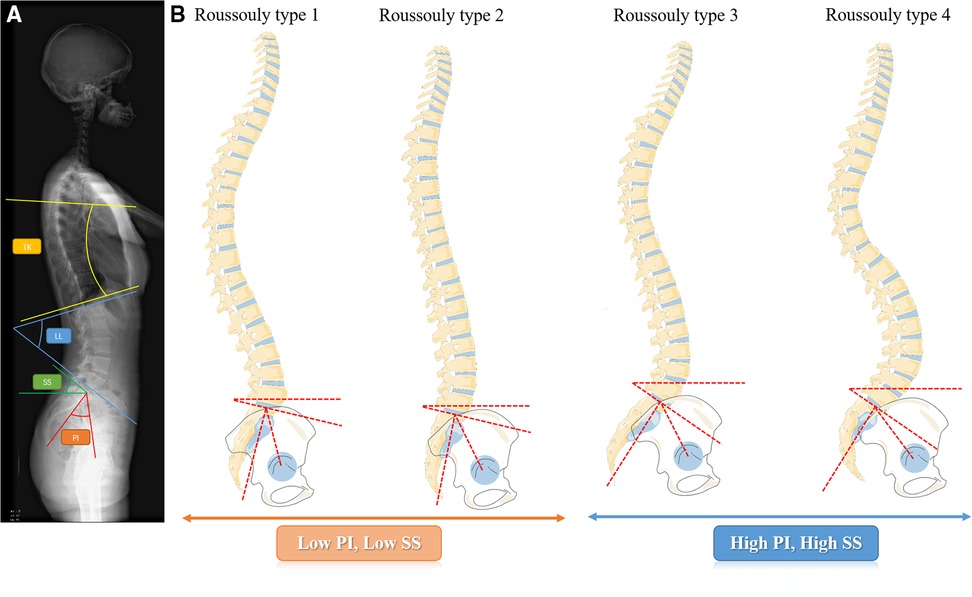
Figure 1. (A) The spino-pelvic parameters measured in the full-length plain radiography; (B) the roussouly classification: type 1: the sacral slope is less than 35°. The apex of the lumbar lordosis is located in the center of L5 vertebral body, The lower arc of lordosis is minimal, showing an incongruous long thoracolumbar kyphosis and short lumbar lordosis curve. Type 2: The sacral slope is less than 35°. The apex of the lumbar lordosis is located at base of the L4 vertebral body. The lower arc of lordosis is relatively flat. Type 3: The sacral slope is between 35° and 45°. The apex of lumbar lordosis is located at the center of the L4 vertebral body, showing a coordinated curve of almost equal length of thoracic kyphosis and lumbar lordosis. Type 4: the sacral slope is greater than 45°, which is associated with a high pelvic incidence. The apex of the lumbar lordosis is located at the base of the L3 vertebral body or higher, showing a coordinated longer lumbar lordosis and a shorter, larger thoracic kyphosis curve.
Statistical analysis
Statistical analyses were performed using GraphPad Prism (GraphPad Prism 8; GraphPad). The measurement data are expressed as mean ± standard deviation. Analysis of variance (ANOVA) or Student's t test was performed to measure statistical significance between differences, correlations were assessed using Pearsons correlative analysis, and P < 0.05 was considered statistically significant.
Results
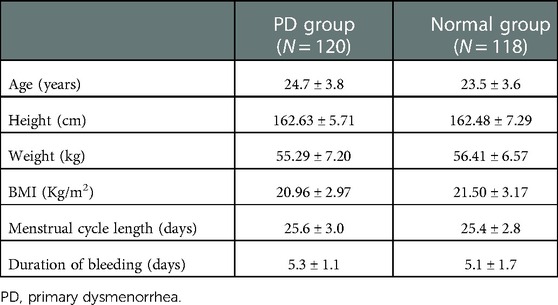
Table 1 shows the general characteristics of the primary dysmenorrhea group and the normal group. There were no statistically significant differences.
Comparison of spino-pelvic alignment between PD and normal groups
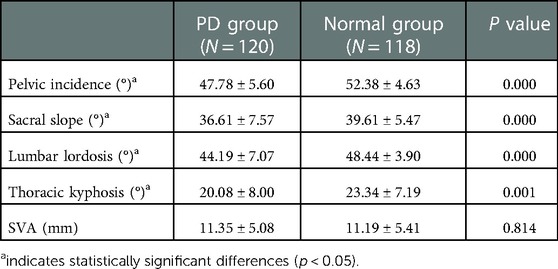
The parameters of lumbar-pelvic alignment between PD and normal groups were shown in Table 2. There was a significant difference in PI, SS, LL and TK between PD group and Normal group (P<0.05). The PI of PD group was 47.78 ± 5.60° vs. 52.38 ± 4.63° of Normal group (P = 0.000), the SS of PD group was 36.61 ± 7.57° vs. 39.61 ± 5.47° of Normal group (P = 0.0006), and the LL of PD group was 44.19 ± 7.07° vs. 48.44 ± 3.90° (P = 0.000), the TK of PD group was 20.08 ± 8.00° vs. 23.34 ± 7.19° of Normal group (P = 0.001). Whereas, there was no significant difference in SVA between PD group and Normal group the SVA of PD group was 11.35 ± 5.08 mm vs. 11.19 ± 5.41 mm of Normal group (P = 0.814).
Analysis of the spino-pelvic alignment parameters in the PD subgroups divided according to the severity of pain
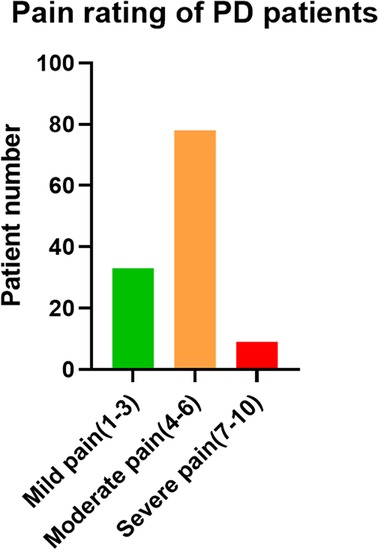
The PD patients were divided into three groups according to VAS scores. As shown in Figure 2, there were 33 patients with mild pain, 78 with moderate pain, and 9 with severe pain. Spino-pelvic parameters were analyzed among each group. The PI was significant different between mild pain group and moderate pain group (49.98 ± 6.66° vs. 47.28 ± 4.98°, P = 0.046), however, there was no significant difference between moderate pain group and severe pain group(47.28 ± 4.98° vs. 44.03 ± 3.57°, P = 0.208). The SS was also significant different between mild pain group and moderate pain group (42.64 ± 6.53°vs. 34.66 ± 6.58°, P = 0.000), whereas, no significant difference was found between moderate pain group and severe pain group (34.66 ± 6.58°vs. 33.06 ± 9.19°, P = 0.342). For LL,TK, and SVA, none of these differences were found statistically significant. The LL in each group were 45.51 ± 6.68°, 43.73 ± 6.93° and 43.30 ± 9.64° (45.51 ± 6.68° vs. 43.73 ± 6.93°, P = 0.281; 43.73 ± 6.93° vs. 43.30 ± 9.64°, P = 0.981). The TK in each group were 21.41 ± 4.38°, 19.34 ± 8.83° and 21.63 ± 10.55° respectively (21.41 ± 4.38° vs. 19.34 ± 8.83°, P = 0.431; 19.34 ± 8.83° vs. 21.63 ± 10.55°, P = 0.696). The SVA in each group were 10.90 ± 5.30 mm, 11.74 ± 4.92 mm and 9.68 ± 5.83 mm (10.90 ± 5.30 mm vs. 11.74 ± 4.92 mm, P = 0.710; 11.74 ± 4.92 mm vs. 9.68 ± 5.83 mm, P = 0.487). The results above were illustrated in Table 3.
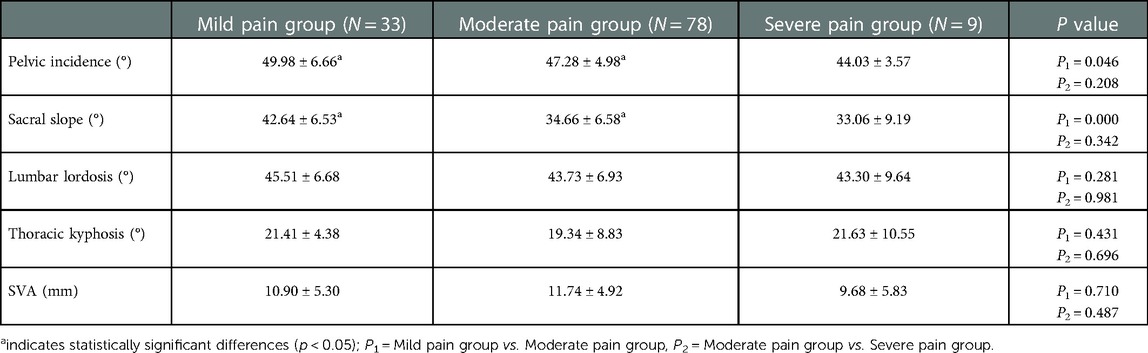
Table 3. Results of sagittal spino-pelvic alignment parameters between mild to severe pain subgroups in PD patient.
The correlation analyses were carried out to assess the correlation between pain rating and each spino-pelvic alignment parameters above. In summary, there were no significant correlation between pain rating and PI (r2 = 0.031, P = 0.054), LL (r2 = 0.011, P = 0.256),TK (r2 = 0.000, P = 0.830) and SVA (r2 = 0.004, P = 0.505), while a significant negative correlation between pain rating and SS (r2 = 0.184, P = 0.000). The linear regression of correlation analyses above were shown in Figure 3.
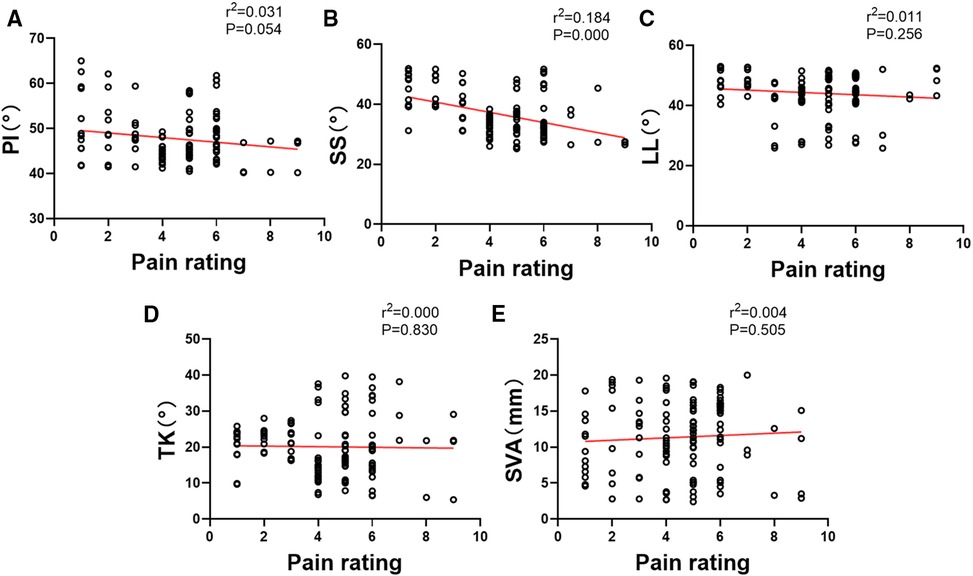
Figure 3. The correlation analysis of the pain rating and sagittal spino-pelvic alignment parameters.
The correlation between Roussouly spine classification and PD
The PD patients and normal volunteers’ radiographic data were then classified according to their Roussouly spine classification. The Roussouly type 1 patient number of PD group and normal group were 19 and 11 respectively. As for Roussouly type 2, the patient number of PD group and normal group were 41 and 19. And the Roussouly type 3 patient number of PD group and normal group were 33 and 58, the Roussouly type 4 patient number of PD group and normal group were 27 and 30. The distribution of the patients number of each Roussouly type was shown in Figure 4.
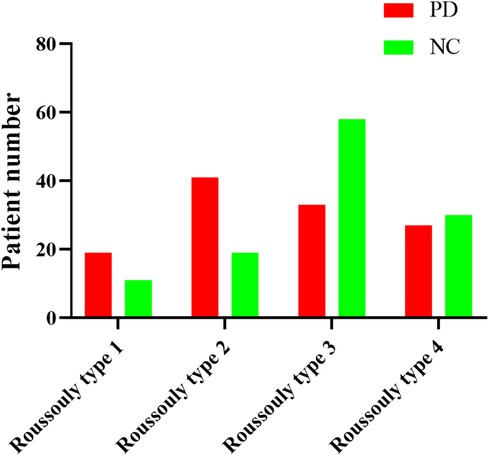
Figure 4. The patients number of PD group and normal group in each Roussouly spine classification type.
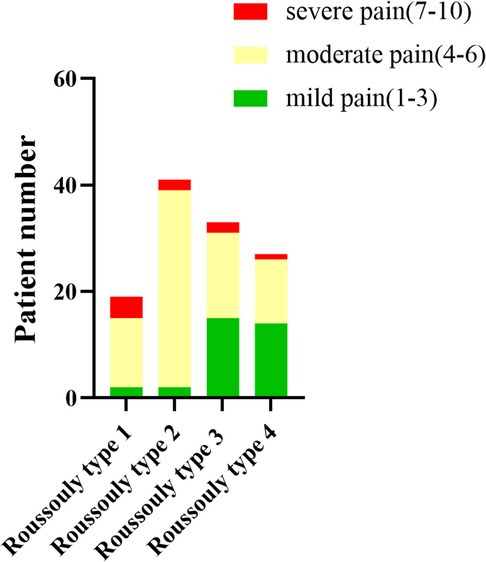
To further investigate the correlation between Roussouly classification of PD patients and pain rating, the different pain rating PD patients were sorted by Roussouly spine classification type. There were 2 mild pain patients, 13 moderate pain patients and 4 severe pain patients classified with Roussouly type 1. And 2 mild pain patients, 37 moderate pain patients and 2 severe pain patients were classified with Roussouly type 2. While 15 mild pain patients, 16 moderate pain patients and 2 severe pain patients were classified with Roussouly type 3. Besides, 14 mild pain patients, 12 moderate pain patients and 1 severe pain patients were classified with Roussouly type 4. The distribution of the PD patients with different pain rating classified with Roussouly type was shown in Figure 5.
Discussion
In recent years, the sagittal spino-pelvic alignment or balance had received more and more attention from various scholars and spine surgeons. Several studies have investigated the importance of sagittal spino-pelvic alignment in spinal disorders such as lumbar spondylolisthesis (12–14), adolescent idiopathic scoliosis (15–18), and adult spinal deformity (19, 20). At the same time, the research on the etiology of primary dysmenorrhea mainly focuses on uterine over contraction (21), vasoconstriction (22, 23), inflammation and release of inflammatory mediators (24, 25), brain Imaging and stimulation of pain fibers (26–29).
The human species is characterized by bipedal walking, which has the advantage of freeing up upper limbs for other tasks, but at the expense of a more unstable overall balance. Indeed, other primates, unlike humans, move on all the four limbs. Their spine presents a single thoraco-lumbar curvature in kyphosis which provides more space for pelvic and abdominal organs and a better global sagittal balance (30). However, at present, there is no study that reported other primates or mammals have primary dysmenorrhea. Primary dysmenorrhea can be defined as a unique symptom to human females. So far, research on the etiology of primary dysmenorrhea has focused more on the pathophysiological factors. In this study, we innovatively discussed the relationship between primary dysmenorrhea and sagittal spino-pelvic alignment, which provided a new and original insights on the etiology of primary dysmenorrhea.
Our results firstly indicated that the PI, SS and LL in PD patients were significant lower than those in normal people (Table 2). In addition, we found that the PI and SS in patients with PD who experienced mild pain were significantly higher than those in patients with moderate pain (Table 3). Surprisingly, a significant negative correlation was found between PD patients' pain rating and SS (Figure 3), which indicated that the lower SS was, the higher pain rating would be. Besides, the distribution of Roussouly spine classification in normal and PD groups showed significant differences. There were more PD patients classified with Roussouly type 2, meanwhile the majority of normal people were classified with Roussouly type 3 (Figure 4). Moreover, a large part of PD patients with moderate pain were classified with Roussouly type 2 (Figure 5). The Roussouly type 2 was defined as that SS was less than 35°, the apex of the lumbar lordosis is located at base of the L4 vertebral body, and the both thoracic and lumbar curve were small, presenting a harmonious flat back appearance. Based on all the results above, it could conceivably be hypothesized that a lower SS and PI angle may be related to a worsen pain in PD patients.
According to the results we found and the hypothesis raised above, an implication of this is the possibility that a lower sacral slope and pelvic incidence may lead to a related smaller pelvic space and a retroversion of uterus. The excessive retroversion could lead to outflow obstruction of menstrual blood and uterine secretions, resulting in local inflammatory reaction, so as to stimulate uterine contraction and cause dysmenorrhea. On the other hand, a higher SS and PI could make uterus a relatively anteversion position, leading to a smooth outflow of menstrual discharge through vagina and therefore relieving the pain. The possible pathophysiological mechanisms were shown in Figure 6.
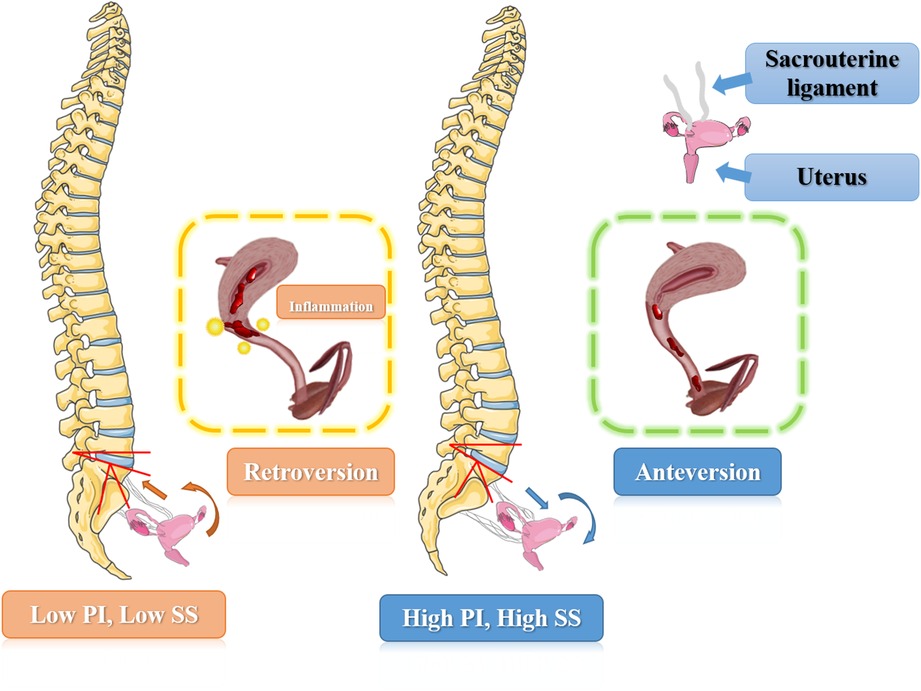
Figure 6. The schematic illustration of possible pathological mechanisms how spino-pelvic alignment parameters affect the primary dysmenorrhea symptoms.
However, this study still has some limitations. The number of patient samples was limited in this retrospective study, a larger sample size was required to fully validate the hypothesis above. Furthermore, limited by the current gynecological ultrasound and abdominal CT examination require supine position, we were not able to assess the patients’ exact uterine position in a standing position, thus could not precisely verify the correlation between the spino-pelvic alignment parameters and pelvic organ position.
Conclusion
In summary, we first reported the relationship between sagittal spino-pelvic alignment and primary dysmenorrhea. In PD patients, worsening pain may be correlated with lower SS and PI angles, which provided a fresh and unique perspective on the cause of primary dysmenorrhea.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the West China Hospital. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
All contributing authors have read and approved the manuscript in its present form. JHW – data collection, study design, data analysis and manuscript writing. XH – data collection, study design, data analysis and manuscript writing. XY – consulting, study supervisor, study design. CZ – data collection, data analysis. HD – data analysis. GJF – supervision, writing. YMS – manuscript review. LML – study supervisor, study design and manuscript review. All authors contributed to the article and approved the submitted version.
Funding
This study was supported in part by the Projects of the Science & Technology Department of Sichuan Province (2022ZDZX0029 and 2021YFS0218), the National Natural Science Foundation of China (81871772; 82172495; 82072434 and 82272546), and the 1·3·5 project for disciplines of excellence–Clinical Research Incubation Project, West China Hospital, Sichuan University (2021HXFH003).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ju H, Jones M, Mishra G. The prevalence and risk factors of dysmenorrhea. Epidemiol Rev. (2014) 36:104–13. doi: 10.1093/epirev/mxt009
2. Yasir S, Kant B, Dar MF. Frequency of dysmenorrhoea, its impact and management strategies adopted by medical students. J Ayub Med Coll Abbottabad. (2014) 26(3):349–52. PMID: 25671945
3. Potur DC, Bilgin NC, Komurcu N. Prevalence of dysmenorrhea in university students in Turkey: effect on daily activities and evaluation of different pain management methods. Pain Manag Nurs. (2014) 15(4):768–77. doi: 10.1016/j.pmn.2013.07.012
4. Tanmahasamut P, Chawengsettakul S. Dysmenorrhea in Siriraj medical students; prevalence, quality of life, and knowledge of management. J Med Assoc Thai. (2012) 95(9):1115–21. PMID: 23140026
5. Chia CF, Joyce HY Lai, Cheung PK, Kwong LT, Fiona PM Lau, Leung KH, et al. Dysmenorrhoea among Hong Kong university students: prevalence, impact, and management. Hong Kong Med J. (2013) 19(3):222–8. doi: 10.12809/hkmj133807
6. Cheng HF, Lin YH. Selection and efficacy of self-management strategies for dysmenorrhea in young Taiwanese women. J Clin Nurs. (2011) 20(7-8):1018–25. doi: 10.1111/j.1365-2702.2010.03363.x
7. Iacovides S, Avidon I, Bentley A, Baker FC. Reduced quality of life when experiencing menstrual pain in women with primary dysmenorrhea. Acta Obstet Gynecol Scand. (2014) 93(2):213–7. doi: 10.1111/aogs.12287
8. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. (2015) 21(6):762–78. doi: 10.1093/humupd/dmv039
9. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). (2005) 30(3):346–53. doi: 10.1097/01.brs.0000152379.54463.65
10. Teraguchi M, Kawakami M, Ishimoto Y, Nagata K, Nakagawa M, Minetama M, et al. Sagittal imbalance of the spine-pelvis-lower extremity axis associated with back-related disability [published online ahead of print, 2020 Dec 5]. J Orthop Sci. (2021) 26(6):986–91. doi: 10.1016/j.jos.2020.10.014
11. de Baranda PS, Andújar P, Collazo-Diéguez M, Pastor A, Santonja-Renedo F, Martínez-Romero MT, et al. Sagittal standing spinal alignment and back pain in 8 to 12-year-old children from the Region of Murcia, Spain: the ISQUIOS program. J Back Musculoskelet Rehabil. (2020) 33(6):1003–14. doi: 10.3233/BMR-191727
12. Maciejczak A, Jabłońska-Sudoł K. Correlation between correction of pelvic balance and clinical outcomes in mid- and low-grade adult isthmic spondylolisthesis. Eur Spine J. (2017) 26(12):3112–21. doi: 10.1007/s00586-016-4808-6
13. Labelle H, Mac-Thiong JM, Roussouly P. Spino-pelvic sagittal balance of spondylolisthesis: a review and classification. Eur Spine J. (2011) 20(Suppl 5):641–6. doi: 10.1007/s00586-011-1932-1
14. Roussouly P, Gollogly S, Berthonnaud E, Labelle H, Weidenbaum M. Sagittal alignment of the spine and pelvis in the presence of L5-s1 isthmic lysis and low-grade spondylolisthesis. Spine (Phila Pa 1976). (2006) 31(21):2484–90. doi: 10.1097/01.brs.0000239155.37261.69
15. Pasha S, Sankar WN, Castelein RM. The link between the 3D spino-pelvic alignment and vertebral body morphology in adolescent idiopathic scoliosis. Spine Deform. (2019) 7(1):53–9. doi: 10.1016/j.jspd.2018.05.016
16. Abelin-Genevois K, Sassi D, Verdun S, Roussouly P. Sagittal classification in adolescent idiopathic scoliosis: original description and therapeutic implications. Eur Spine J. (2018) 27(9):2192–202. doi: 10.1007/s00586-018-5613-1
17. Hu P, Yu M, Liu X, Zhu B, Liu X, Liu Z. Analysis of the relationship between coronal and sagittal deformities in adolescent idiopathic scoliosis. Eur Spine J. (2016) 25(2):409–16. doi: 10.1007/s00586-015-3986-y
18. Upasani VV, Tis J, Bastrom T, Pawelek J, Marks M, Lonner B, et al. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ? Spine (Phila Pa 1976). (2007) 32(12):1355–9. doi: 10.1097/BRS.0b013e318059321d
19. Durand WM, Daniels AH, Hamilton DK, Passias P, Kim HJ, Protopsaltis T, et al. The spino-pelvic ratio: a novel global sagittal parameter associated with clinical outcomes in adult spinal deformity patients. Eur Spine J. (2020) 29(9):2354–61. doi: 10.1007/s00586-020-06472-x
20. Shimizu T, Lehman RA Jr, Sielatycki JA, Pongmanee S, Cerpa M, Takemoto M, et al. Reciprocal change of sagittal profile in unfused spinal segments and lower extremities after complex adult spinal deformity surgery including spinopelvic fixation: a full-body x-ray analysis. Spine J. (2020) 20(3):380–90. doi: 10.1016/j.spinee.2019.09.012
21. Wei Y, Ma T, Wang H, et al. Extracts of compound Muniziqi granule suppressed uterus contraction and ameliorated oxytocin-induced primary dysmenorrhea. J Ethnopharmacol. (2018) 223:33–40. doi: 10.1016/j.jep.2018.05.024
22. Bossmar T, Akerlund M, Szamatowicz J, Laudanski T, Fantoni G, Maggi M. Receptor-mediated uterine effects of vasopressin and oxytocin in nonpregnant women. Br J Obstet Gynaecol. (1995) 102(11):907–12. doi: 10.1111/j.1471-0528.1995.tb10880.x
23. Akerlund M. Vasopressin and oxytocin in normal reproduction and in the pathophysiology of preterm labour and primary dysmenorrhoea. Development of receptor antagonists for therapeutic use in these conditions. Rocz Akad Med Bialymst. (2004) 49:18–21. PMID: 15631309
24. Tang B, Liu D, Chen L, Liu Y. NLRP3 Inflammasome inhibitor MCC950 attenuates primary dysmenorrhea in mice via the NF-κB/COX-2/PG pathway. J Inflamm (Lond). (2020) 17:22. Published 2020 Jun 24. doi: 10.1186/s12950-020-00251-7
25. Barcikowska Z, Rajkowska-Labon E, Grzybowska ME, Hansdorfer-Korzon R, Zorena K. Inflammatory markers in dysmenorrhea and therapeutic options. Int J Environ Res Public Health. (2020) 17(4):1191. Published 2020 Feb 13. doi: 10.3390/ijerph17041191
26. Chan HL, Low I, Chen LF, Chen YS, Chu IT, Hsieh JC. A novel beamformer-based imaging of phase-amplitude coupling (BIPAC) unveiling the inter-regional connectivity of emotional prosody processing in women with primary dysmenorrhea [published online ahead of print, 2021 Mar 10]. J Neural Eng. (2021) 18(4):10.1088/1741-2552/abed83. doi: 10.1088/1741-2552/abed83
27. Dun W, Fan T, Wang Q, Wang K, Yang J, Liet H, et al. Association between trait empathy and resting brain activity in women with primary dysmenorrhea during the pain and pain-free phases. Front Psychiatry. (2020) 11:608928. Published 2020 Nov 26. doi: 10.3389/fpsyt.2020.608928
28. Quan S, Yang J, Dun W, Wang K, Liu H, Liu J. Prediction of pain intensity with uterine morphological features and brain microstructural and functional properties in women with primary dysmenorrhea. Brain Imaging Behav. (2021) 15(3):1580–8. doi: 10.1007/s11682-020-00356-w
29. Zhang YN, Huo JW, Huang YR, Hao Y, Chen ZY. Altered amplitude of low-frequency fluctuation and regional cerebral blood flow in females with primary dysmenorrhea: a resting-state fMRI and arterial spin labeling study. J Pain Res. (2019) 12:1243–50. Published 2019 Apr 16. doi: 10.2147/JPR.S177502
Keywords: primary dysmenorrhea, sagittal spino-pelvic alignment, global sagittal balance, pathological mechanisms, sacral slope
Citation: Wang J, He X, Zhu C, Ding H, Feng G, Yang X, Liu L and Song Y (2023) The relationship between spino-pelvic alignment and primary dysmenorrhea. Front. Surg. 10:1125520. doi: 10.3389/fsurg.2023.1125520
Received: 16 December 2022; Accepted: 17 January 2023;
Published: 8 February 2023.
Edited by:
Carl Haasper, Orthopaedic Surgery Bremerhaven-Wesermünde, GermanyReviewed by:
Huri Güvey, Private Parkhayat Hospital, TürkiyeYang Liu, Shanghai Changzheng Hospital, China
© 2023 Wang, He, Zhu, Hong, Feng, Yang, Liu and Song. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xi Yang Zm9ybW9zYTg4QDE2My5jb20= Limin Liu bGl1bGltaW5fc3BpbmVAMTYzLmNvbQ==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Juehan Wang1,†
Juehan Wang1,† Ganjun Feng
Ganjun Feng Xi Yang
Xi Yang Limin Liu
Limin Liu Yueming Song
Yueming Song