
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Surg., 17 May 2023
Sec. Surgical Oncology
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1116473
Trans oral video-assisted thyroidectomy (TOVAT) is increasingly performed for cosmetic reasons. The quality of life after thyroidectomy is important for decision-making. This is the first meta-analysis to compare the quality of life among conventional transcervical thyroidectomies. This meta-analysis aimed to assess the same in the current literature. The authors systematically searched PubMed, Google Scholar, and EBSCO for relevant articles from the first published to December 4, 2022. The keywords endoscopic transoral via vestibular thyroidectomy, transcervical thyroidectomy, conventional thyroidectomy, scarless thyroidectomy, and quality of life were used. Out of the 482 studies retrieved, 27 full texts were reviewed, and only six fulfilled the inclusion and exclusion criteria. Patients with transoral thyroidectomy showed better quality of life that their counterparts who underwent transcervical thyroidectomy at 4–6 weeks following surgery, odd ratio, 2.26, 95% CI, 2.02–2.5, P-value <0.001. Substantial heterogeneity was observed, I2 for heterogeneity, 100%. The quality of life was better among patients who underwent the trans oral video-assisted thyroidectomy (TOVAT) compared to their counterparts with the conventional cervical approach (surgical questionnaire). All the components of the SF-36 quality of life questionnaire were better among TOVAT compared to the conventional approach except for social and general health components, which were equal between the two arms. Further multi-center studies with larger samples and controlling for pain and the surgical curve are needed.
Thyroid surgery is increasingly performed mirroring the increasing detection of low-risk differentiated thyroid carcinoma. Transoral thyroidectomy through different approaches is more popular due to the lack of unwanted neck scars (1). In addition, to the minimal dissection needed and surgical anatomical space respect. The patients are selected depending on thyroid diameter, thyroid volume, and underlying thyroid disease (2). Endoscopic thyroidectomy through the sublingual and the trans-tracheal approaches was first performed in Germany for a better cosmesis and discontinued due to safety issues (3, 4). Transoral thyroidectomy had the same outcomes as the traditional transcervical approaches with better cosmetic outcomes. However, unusual complications including mental nerve injury, carbon dioxide embolism, infections, burns, and perforation (5) are of great concern. Due to the excessive emphasis on physical appearance especially among young females and those prone to excessive scarring and keloids. Remote approaches including transoral thyroidectomy (either robotic or endoscopic approaches) are gaining popularity among both patients and Surgeons (6). Trans oral video-assisted thyroidectomy is increasingly used as truly scarless thyroid surgery for low-risk differentiated thyroid carcinoma. Patients who underwent thyroidectomy were found to live longer and have a lower quality of life compared to the general population (7, 1). Literature comparing different forms of remote thyroidectomy is scarce, and this is the first meta-analysis to compare transoral endoscopic thyroidectomy and conventional thyroidectomy. Therefore, this meta-analysis aimed to compare the quality of life of transoral and conventional thyroidectomy.
The studies were included if they were retrospective or prospective cohorts, case-control studies, or randomized controlled studies (RCTs) comparing the quality of life among patients who underwent thyroidectomy via the conventional cervical approach or the endoscopic transoral via vestibular route. Thyroidectomy via other routes including areolar, breast axillary, and postauricular was not included. Case reports and case series were not included.
Comparing the quality of life between conventional thyroidectomy and trans oral video-assisted thyroidectomy.
The two researchers searched three databases, PubMed, Medline, EBSCO, and Google Scholar. The search engine was limited to the period from the first published article up to December 2022. The keywords trans oral video-assisted thyroidectomy, transcervical thyroidectomy, conventional thyroidectomy, scarless thyroidectomy, and quality of life were used.
The information retrieved included the author's name, year of publication, patient's number, the study duration, the criteria of patient selection, the quality of life using the SF-36, SF-12 quality of life questionnaire, and surgical questionnaire. The two authors cross-checked the data and discrepancies were solved by consensus. Newcastle Ottawa Scale assessed the quality of the included study (8) (Figure 1 and Tables 1, 2).
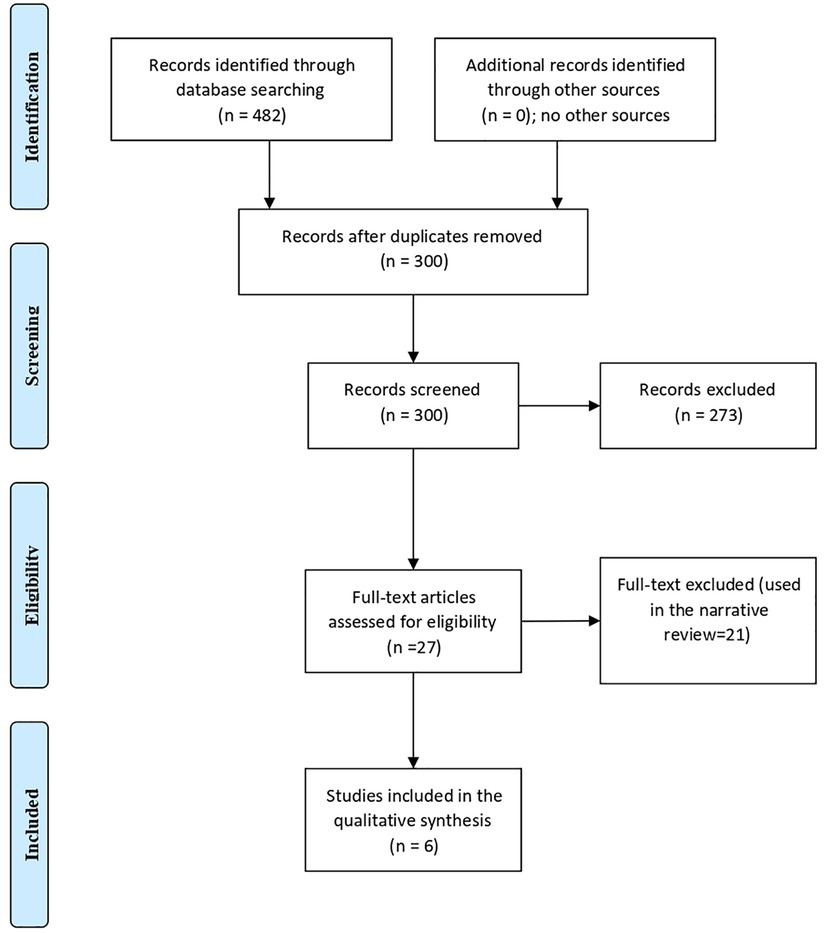
Figure 1. A comparison between the endoscopic trans oral video-assisted thyroidectomy and conventional thyroidectomy quality of life (the PRISMA chart).
The RevMan system for meta-analysis was used, and the data were all continuous. The fixed effect or random effect was used depending on the level of heterogeneity. Funnel plots were used to assess lateralization. A P-value of <0.05 was considered significant.
There were six studies (9–14), five from Asia and one from France. Patients with TOETVA were younger and mostly females, all patients were diagnosed with benign thyroid nodules in three studies, with more benign nodules among patients with TOETVA in the other three studies.
In the present meta-analysis patients with transoral thyroidectomy showed better quality of life that their counterparts who underwent transcervical thyroidectomy at 4–6 weeks following surgery, odd ratio, 2.26, 95% CI, 2.02–2.5, P-value <0.001. Substantial heterogeneity was observed, I2 for heterogeneity, 100%. Figure 2 showed the quality of life of 530 patients.
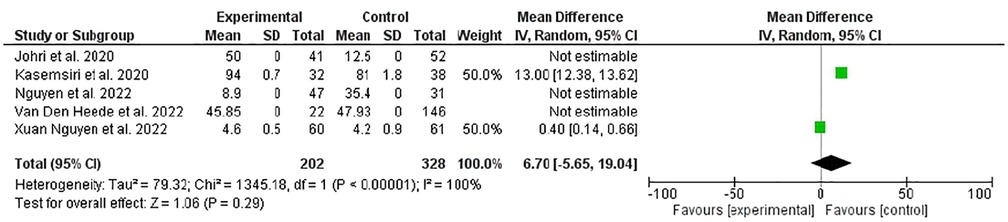
Figure 2. A comparison of quality of life between trans oral video-assisted thyroidectomy and conventional open thyroidectomy at 4–6 weeks (specific thyroid surgery-related QOL questionnaire).
In the present meta-analysis, three studies including 322 patients were pooled. The quality of life was assessed using the thyroid surgery-specific questionnaire. Transoral thyroidectomy showed a better physical function compared to conventional thyroidectomy, odd ratio, 9.11, 95% CI, 2.98–15.24, no heterogeneity was observed, I2, 0.0, P-value for overall effect, 0.004. Regarding role physics, TOVAT showed better results, odd ratio, 30.49, 95% CI, 20.61–40.36, no heterogeneity was observed, I2, 0.0%%, P-value for overall effect <0.001. Emotion, bodily pain, and vitality were better among the TOETVA arm, with odd ratio, 22.58, 95% CI, 2.88–42.27, odd ratio, 7.91, 95% CI, 2.25–13.56, odd ratio, 11.46, 95% CI, 5.52–17.41. However, no difference was evident regarding social function, odd ratio, 10.16, 95% CI, 4.77–25.8. Transoral thyroidectomy was better than conventional thyroidectomy regarding mental health, but not general health, odd ratio, 9.11, 95% CI, 3.73–14.49, and odd ratio, 10.11, 95% CI, 5.32–25.53, respectively, P-values, 0.009, and 0.2 respectively (Figure 3).
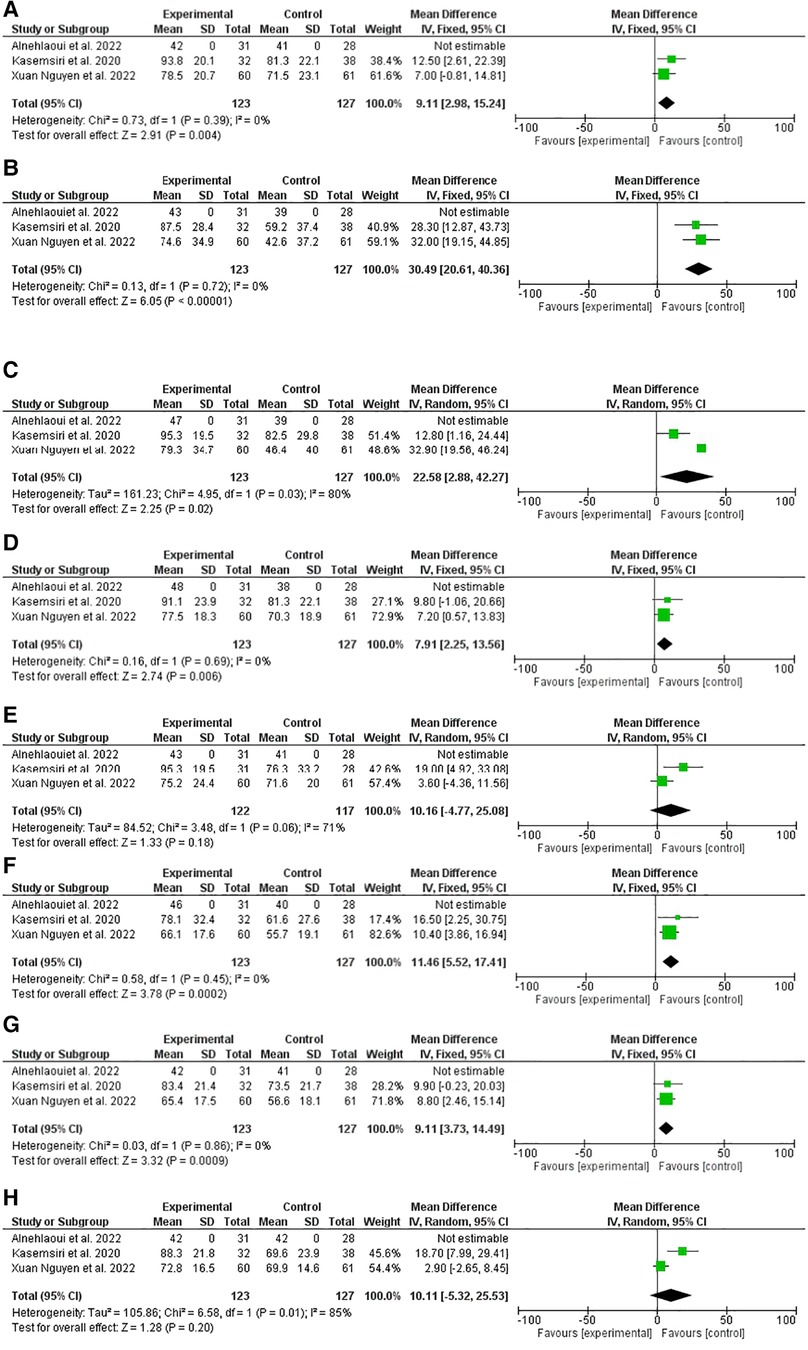
Figure 3. A comparison of quality of life between trans oral video-assisted thyroidectomy and conventional open thyroidectomy at four-six weeks after surgery (36- item short-form health survey). (A) Physical function, (B) role physics, (C) emotion, (D) bodily pain, (E) vitality, (F) social function, (G) mental health, (H) general health.
Patients with papillary thyroid carcinoma (especially young women) are willing to travel and pay extra expenses to avoid the visible open thyroidectomy scar. Trans oral video-assisted thyroidectomy (TOVAT) is a scar-free approach that satisfies the cosmetic requirements of the patients. Due to the long survival of PTC, many patients including the elderly are more concerned about cosmetic outcomes and quality of life (15, 16). In the present meta-analysis, TOVAT was associated with a better quality of life at 4–6 weeks compared to conventional thyroidectomy using specific thyroid surgery-related QOL questionnaire overall satisfaction (odd ratio, 2.26, 95% CI, 2.02–2.5). However, discrepancies were observed among the different items of 36- the item Short-Form Health Survey. TOVAT was better in all quality of life domains except for the social and general health domains in them there was no difference between the two approaches. A plausible explanation might be the SF-36 is not specific in evaluating cancer symptoms (17). In addition, the quality of life among patients with papillary thyroid carcinoma differs significantly according to the temporal profile (worse at one month and improves in six months but never reaches that of the general population) (18). Furthermore, patients with thyroid cancer tend to have poor role emotion for years after surgery; this is because they fear the rare rate of metastasis (19). Absence of scaring improved the cosmetic outcomes, overall satisfaction, and quality of life among patients with TOVAT compared to their counterparts who underwent open surgery. Importantly, TOVAT might improve communication, career development, self-esteem, quality of life, and fashion (20–22). Postoperative exercise can improve pulling sensation and limitation of neck movement from corridor application in TOVAT. Therefore, early neck exercises are recommended to improve the quality of life among patients undergoing TOVAT (23).
In the present meta-analysis, most of the patients who choose TOVAT were young females with benign thyroid nodules. The explanations are that young females are more concerned about cosmetic appearance, also, the extent of surgery and the Surgeon's experience might affect the operation choice (24).
Importantly, low/intermediate grade differentiated thyroid carcinoma are heterogeneous. Tumor-specific genetic alterations and vascularization are linked to recurrence and prognostication (many germline vascular endothelial growth factor-A single nucleotide polymorphisms) (25). It is vital to consider the above possibility when choosing the approach for thyroidectomy as TOVAT might increase the seeding of such tumors. Another important issue is the calcitonin negative tumors, which pose a clinical diagnostic challenge (26). Recurrent laryngeal nerve palsy is the most feared post-thyroidectomy complications with medicolegal litigation; transcutaneous laryngeal ultrasonography is a noninvasive sensitive measure for evaluating laryngeal nerves before operation with a high concordance to laryngoscopy (27).
The study had several limitations: the small number of the included studies, the short duration of the studies included, not reporting the analgesia that might affect the quality of life, and not evaluating the quality of life before surgery.
The quality of life was better among patients who underwent the trans oral video-assisted thyroidectomy compared to their counterparts with the conventional cervical approach (surgical questionnaire). All the components of the SF-36 quality of life questionnaire were better among TOVAT compared to the conventional approach except for social and general health components, which were equal between the two arms. Further multi-center studies with larger samples and controlling for pain and the surgical curve are needed.
All authors listed have made a substantial, direct, and intellectual contribution to the work and approved it for publication.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Jongekkasit I, Jitpratoom P, Sasanakietkul T, Anuwong A. Transoral endoscopic thyroidectomy for thyroid cancer. Endocrinol Metab Clin North Am. (2019) 48(1):165–80. doi: 10.1016/j.ecl.2018.11.009
2. Dionigi G, Lavazza M, Wu CW, Sun H, Liu X, Tufano RP, et al. Transoral thyroidectomy: why is it needed? Gland Surg. (2017) 6(3):272–6. doi: 10.21037/gs.2017.03.21
3. Benhidjeb T, Wilhelm T, Harlaar J, Kleinrensink GJ, Schneider TA, Stark M. Natural orifice surgery on thyroid gland: totally transoral video-assisted thyroidectomy (TOVAT): report of first experimental results of a new surgical method. Surg Endosc. (2009) 23(5):1119–20. doi: 10.1007/s00464-009-0347-0
4. Anuwong A. Transoral endoscopic thyroidectomy vestibular approach: a series of the first 60 human cases. World J Surg. (2016) 40(3):491–7. doi: 10.1007/s00268-015-3320-1
5. Tae K. Complications of transoral thyroidectomy: overview and update. Clin Exp Otorhinolaryngol. (2021) 14(2):169–78. doi: 10.21053/ceo.2020.02110
6. Richmon JD, Kim HY. Transoral robotic thyroidectomy (TORT): procedures and outcomes. Gland Surg. (2017) 6(3):285–289. doi: 10.21037/gs.2017.05.05
7. Yu HW, An AR, Kang HI, Suh YJ, Kwon H, Kim SJ, et al. Does thyroidectomy impact quality of life: retrospective case-control study of post-thyroidectomy patients and matched individuals from the general population. Medicina (Kaunas). (2020) 56(11):603. doi: 10.3390/medicina56110603
8. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25(9):603–5. doi: 10.1007/s10654-010-9491-z
9. Johri G, Chand G, Mishra A, Mayilvaganan S, Agarwal G, Agarwal A, et al. Endoscopic versus conventional thyroid surgery: a comparison of quality of life, cosmetic outcomes and overall patient satisfaction with treatment. World J Surg. (2020) 44(12):4118–26. doi: 10.1007/s00268-020-05732-7
10. Kasemsiri P, Trakulkajornsak S, Bamroong P, Mahawerawat K, Piromchai P, Ratanaanekchai T. Comparison of quality of life between patients undergoing trans-oral endoscopic thyroid surgery and conventional open surgery. BMC Surg. (2020) 20(1):18. doi: 10.1186/s12893-020-0685-3
11. Nguyen HX, Nguyen HX, Le AD, Van Le Q. Comparison of transoral endoscopic thyroidectomy vestibular approach and conventional open thyroidectomy in benign thyroid tumors. Indian J Surg Oncol. (2022) 13(1):178–83. doi: 10.1007/s13193-022-01494-x
12. Van Den Heede K, Brusselaers N, Gaujoux S, Menegaux F, Chereau N. Feasibility and safety of ambulatory transoral endoscopic thyroidectomy via vestibular approach (TOETVA). World J Surg. (2022) 46(11):2678–86. doi: 10.1007/s00268-022-06666-y
13. Xuan Nguyen H, Nguyen HX, Thi Hoang H, Van Le Q. Quality of life and surgical outcome of transoral endoscopic thyroidectomy vestibular approach (TOETVA) versus open thyroid surgery: experience from a single center in Vietnam. J Thyroid Res. (2022) 2022:2381063. doi: 10.1155/2022/2381063
14. Alnehlaoui F, Alsarraj MN, Malaki Z, Guraya SY. The effectiveness and quality of life outcomes by transoral endoscopic vestibular thyroidectomy using intraoperative indocyanin green fluorescence imaging and neuromonitoring—a cohort study. Healthcare (Basel). (2022) 10(5):953. doi: 10.3390/healthcare10050953
15. Sukpanich R, Sanglestsawai S, Seib CD, Gosnell JE, Shen WT, Roman SA, et al. The influence of cosmetic concerns on patient preferences for approaches to thyroid lobectomy: a discrete choice experiment. Thyroid. (2020) 30(9):1306–13. doi: 10.1089/thy.2019.0821
16. Arora A, Swords C, Garas G, Chaidas K, Prichard A, Budge J, et al. The perception of scar cosmesis following thyroid and parathyroid surgery: a prospective cohort study. Int J Surg. (2016) 25:38–43. doi: 10.1016/j.ijsu.2015.11.021
17. Borget I, Bonastre J, Catargi B, Déandréis D, Zerdoud S, Rusu D, et al. Quality of life and costeffectiveness assessment of radioiodine ablation strategies in patients with thyroid cancer: results from the randomized journal of (yroid research 7 phase III ESTIMABL trial. J Clin Oncol. (2015) 33(26):2885–92. doi: 10.1200/JCO.2015.61.6722
18. Gou J, Cheng W, Lei J, Pan Q, You W, Cai M, et al. Health-related quality-of-life assessment in surgical patients with papillary thyroid carcinoma. Medicine (Baltimore). (2017) 96(38):e8070. doi: 10.1097/MD.0000000000008070
19. Hedman C, Djarv T, Strang P, Lundgren CI. Determinants of long-term quality of life in patients with differentiated thyroid carcinoma—a population-based cohort study in Sweden. Acta Oncol (Madr). (2016) 55(3):365–9. doi: 10.3109/0284186X.2015.1102965
20. Choi Y, Lee JH, Kim YH, Lee YS, Chang HS, Park CS, et al. Impact of postthyroidectomy scar on the quality of life of thyroid cancer patients. Ann Dermatol. (2014) 26(6):693–9. doi: 10.5021/ad.2014.26.6.693
21. Annunziata MA, Giovannini L, Muzzatti B. Assessing the body image: relevance, application and instruments for oncological settings. Support Care Cancer. (2012) 20(5):901–7. doi: 10.1007/s00520-011-1339-x
22. Lee S, Kim HY, Lee CR, Park S, Son H, Kang SW, et al. A prospective comparison of patient body image after robotic thyroidectomy and conventional open thyroidectomy in patients with papillary thyroid carcinoma. Surgery. (2014) 156(1):117–25. doi: 10.1016/j.surg.2014.02.007
23. Miyauchi A, Ito Y, Miya A. Stretching exercise for the prevention of postoperative neck symptoms following thyroid surgery. Video Endocrinol. (2021) 8(1):ve.2021.0003. doi: 10.1089/ve.2021.0003
24. Luo JH, Xiang C, Wang P, Wang Y. The learning curve for transoral endoscopic thyroid surgery: a single surgeon's 204 case experience. J Laparoendosc Adv Surg Tech A. (2020) 30(2):163–9. doi: 10.1089/lap.2019.0560
25. Marotta V, Sciammarella C, Capasso M, Testori A, Pivonello C, Chiofalo MG, et al. Germline polymorphisms of the VEGF pathway predict recurrence in nonadvanced differentiated thyroid cancer. J Clin Endocrinol Metab. (2017) 102(2):661–71. doi: 10.1210/jc.2016-2555
26. Gambardella C, Offi C, Patrone R, Clarizia G, Mauriello C, Tartaglia E, et al. Calcitonin negative medullary thyroid carcinoma: a challenging diagnosis or a medical dilemma? BMC Endocr Disord. (2019) 19(Suppl 1):45. doi: 10.1186/s12902-019-0367-2
27. Gambardella C, Offi C, Romano RM, De Palma M, Ruggiero R, Candela G, et al. Transcutaneous laryngeal ultrasonography: a reliable, non-invasive and inexpensive preoperative method in the evaluation of vocal cords motility-a prospective multicentric analysis on a large series and a literature review. Updates Surg. (2020) 72(3):885–92. doi: 10.1007/s13304-020-00728-3
Keywords: oral thyroidectomy, transcervical thyroidectomy, vestibular approach, quality of life, cosmetic thyroidectomy
Citation: Altedlawi Albalawi IA and Mirghani HO (2023) The quality of life after trans oral video-assisted thyroidectomy and cervical thyroidectomy: a systematic review and meta-analysis. Front. Surg. 10:1116473. doi: 10.3389/fsurg.2023.1116473
Received: 5 December 2022; Accepted: 3 May 2023;
Published: 17 May 2023.
Edited by:
Calogero Virgone, University Hospital of Padua, ItalyReviewed by:
Michael Stark, New European Surgical Academy (NESA), Germany© 2023 Altedlawi Albalawi and Mirghani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ibrahim A. Altedlawi Albalawi ZHJiYWxhd2lAeWFob28uY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.