- 1Hospital of Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2School of Nursing, Chengdu University of Traditional Chinese Medicine, Chengdu, China
Objective: Spinal endoscopic surgery has been promoted rapidly in the past decade, attracting an increasing number of young, dedicated surgeons. However, it has long been denounced for its long learning curve as a factor impeding the development of this state-of-the-art technique. The aim of the present study was to discover what really matters in the educational process of becoming a spinal endoscopic surgeon.
Methods: An online survey consisting of 14 compulsory questions was distributed in April and May 2022 through the First Chinese Spinal Endoscopic Surgeons Skills Competition. Reminders were sent to increase response rates.
Results: Of the 893 emails that were sent, we received 637 responses. A total of 375 (76.7%) surgeons most frequently used endoscopic techniques in their practices. Regardless of their different backgrounds, 284 (75.7%) surgeons thought it would be necessary for a young spinal endoscopic surgeon to perform 300 cases independently in order to become proficient, followed by 500 (n=43, 11.5%), 100 (n=40, 10.7%), and 1,000 (n=8, 2.1%) cases. According to the surgeons, the most difficult aspect of mastering the endoscopic technique is a disparate surgical view (n=255, 68%), followed by adaption to new instruments (n=86, 22.9%) and hand-eye coordination (n=34, 9.1%). The most helpful training method for helping the spinal endoscopic surgeons of younger generations improve is operating on simulation models or cadaver courses (n=216, 57.6%), followed by online or offline theoretical courses (n=67, 17.9%), acquiring opportunities during surgeries (n=51, 13.6%), and frequently participating in surgeries as an assistant (n=41, 10.9%).
Conclusion: From the perspective of surgeons, to be skilled in spinal endoscopic surgery means overcoming a steep learning curve. However, training systems should be given more attention to make them more accessible to younger surgeons so they can work on simulation models or take cadaver courses.
Background
Spinal endoscopic surgery, with its unique advantages of a clearer surgical view and continuous irrigation, has been promoted worldwide to treat various forms of spinal disease, from initial degenerative pathology to spinal trauma, infection, and even deformity (1–3). Technically, in terms of the novel instruments being invented steadily with great efforts coming from peers in this field, its surgical approaches and methods have flourished in the past decade to meet the challenges of these diseases (4–6). It is for this reason that spinal endoscopic surgery has attracted an increasing number of young, dedicated surgeons (7).
However, when it comes to this state-of-the-art technique, it is worth mentioning that its learning curve has been long considered a barrier keeping many young surgeons from mastering it (8, 9). Several studies have clarified the steep learning curve and pointed out that it was likely much steeper than any other minimally invasive spinal surgery (10–12). Yet, very few articles have disclosed the reason for this curve and what training techniques young surgeons most urgently need. The aim of the present study was to conduct an online survey in order to analyze the most difficult aspect of learning spinal endoscopic surgery and identify the most beneficial training method for the younger generation of spinal surgeons.
Methods
A questionnaire was developed using the Tencent Questionnaire Platform for spinal surgeons about the relevant educational issues of spinal endoscopic surgery (Supplementary Material 1). The study samples were targeted at the members of the First Chinese Spinal Endoscopic Surgeons Skills Competition, which is a national academic competition for spinal endoscopic surgery. Spinal endoscopic surgery has a predominant status in the field of minimally invasive spinal surgery in China, and this nationwide competition was held to represent surgeons and allied health professionals dedicated to advancement in this field (13, 14). As the corresponding author’s institution was also the participating and reviewing institution, 2,893 members were contacted via email. Questionnaires were sent out in April and May 2022, with reminders after 2 weeks to increase the response rate.
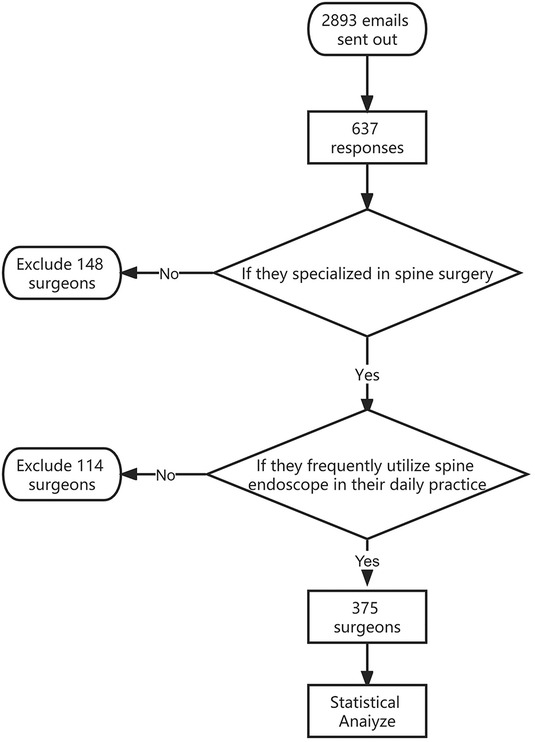
Screening for surgeons
To make the study more representative, the participants involved in this survey were the surgeons who frequently utilized spinal endoscopy in their daily practice. Hence, surgeons who did not specialize in spinal surgery or who did not regularly use spinal endoscopy in their daily practice were excluded from the study.
Survey content
The survey consisted of 14 compulsory questions for surgeons. The first six questions were about basic personal information such as background, age, gender, training specialty, and title. Questions 7–11 were to acknowledge the status of their application on spinal endoscopic surgery. The last three questions collected the surgeons’ attitudes toward endoscopic education.
Statistical analyses
For statistical analyses, IBM SPSS version 25.0 (IBM Corp., Armonk, NY, USA) was used. The age of the participants was represented as the mean and standard deviation () while other indexes were expressed as a percentage [n (%)].
Results
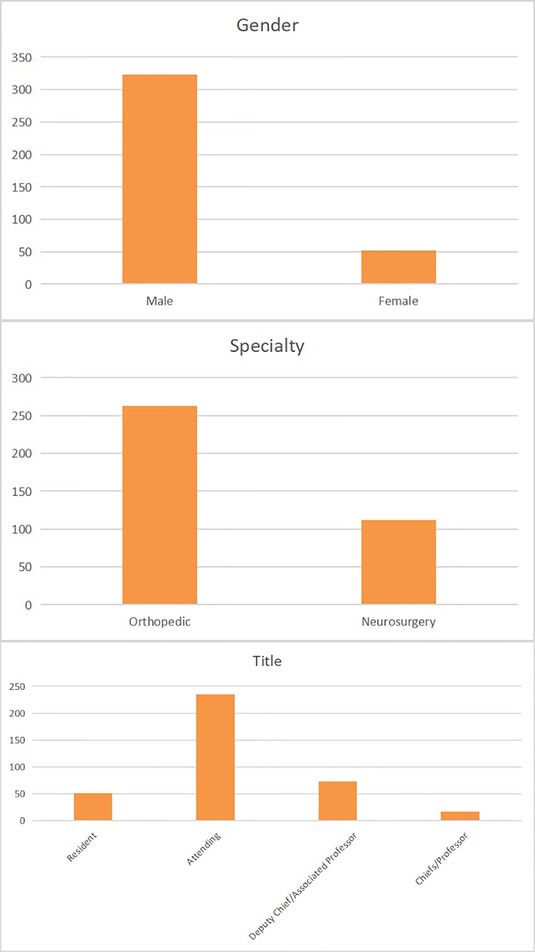
Of the 893 emails that were sent, we received 637 responses. All respondents specialized in spinal surgery; with 489 (76.8%) considering minimally invasive spinal surgery to be their subspecialty. Among them, 375 (76.7%) surgeons used the endoscopic technique most frequently in their practice. The screening process for surgeons is shown in Figure 1. Of these 375 surgeons (mean age 42.5 ± 4.3 years) 323 (86.1%) were men and 52 (13.9%) were women. Of them, 263 (70.1%) were from an orthopedic background while 112 (29.9%) were from a neurosurgery background. In terms of titles, 51 (13.6%) were residents, followed by 235 (62.7%) attendings, 73 (19.5%) deputy chiefs/associated professors, and 16 (4.3%) chiefs/professors (Figure 2).
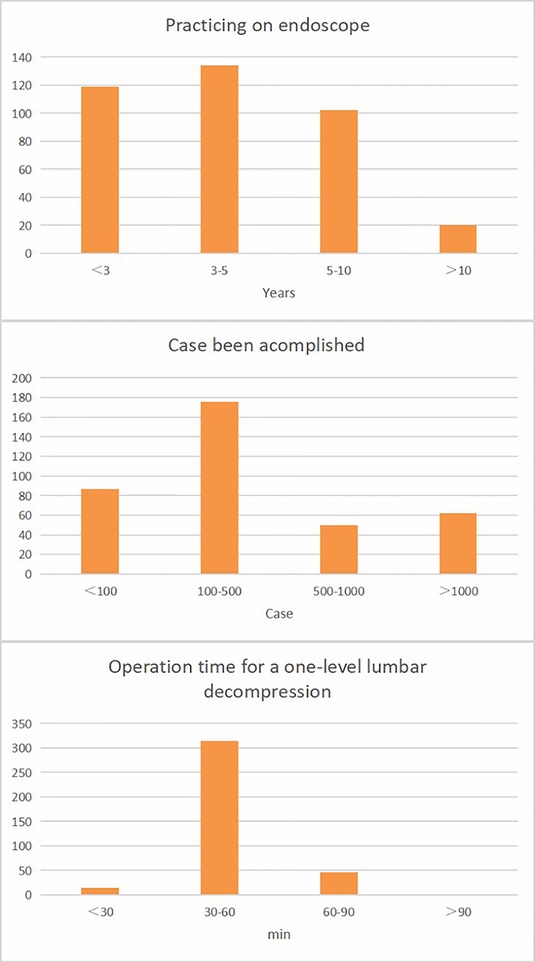
With regard to their years of experience with the endoscopic application, 119 (31.7%) surgeons had been practicing endoscopic surgery for less than 3 years, 134 (35.7%) had been practicing for 3–5 years, 102 (27.2%) had been practicing for 5–10 years, and only 20 (5.3%) surgeons had been practicing for more than 10 years. Concerning the number of cases they had already completed, 87 (23.2%) of the surgeons had worked on less than 100 cases, 176 (46.9%) had already done 100–500 cases, 50 (13.3%) had already done 500–1,000 cases, and 62 (16.5%) of them had already done more than 1,000 cases. In terms of the operating time for a one-level lumbar decompression, 15 (4%) of the surgeons could complete the procedure in less than 30 minutes, 314 (83.7%) in 30–60 minutes, 46 (12.3%) in 60–90 minutes, and none of them took more than 90 minutes (Figure 3).
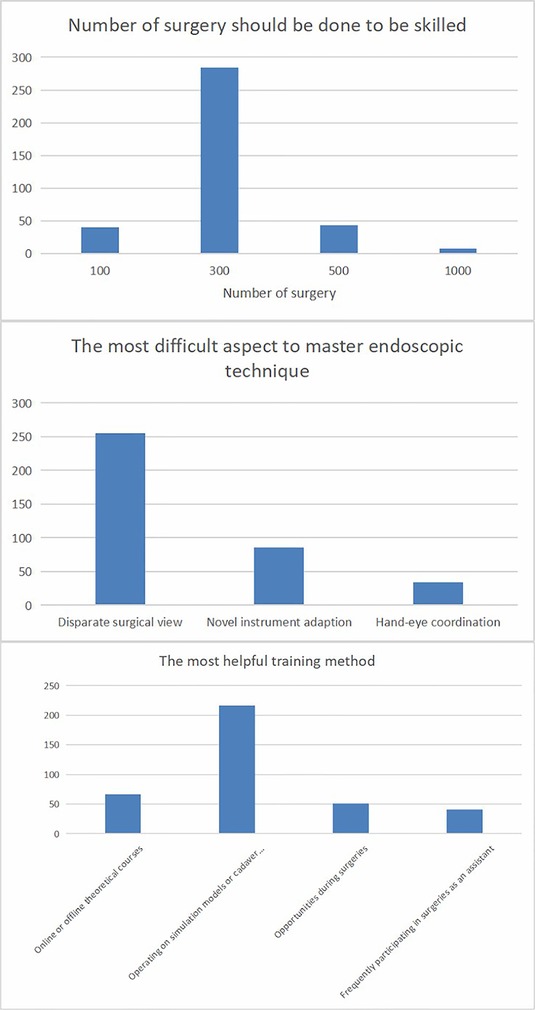
Regarding the surgeons’ attitudes toward the education process for spinal endoscopic surgeons, 284 (75.7%) of them thought it would be necessary for a young spinal endoscopic surgeon to perform 300 cases independently to become proficient, followed by 500 (n=43, 11.5%) cases, 100 (n=40, 10.7%) cases, and 1,000 (n=8, 2.1%) cases. According to the surgeons, the most difficult aspect of this technique to master was the disparate surgical view (n=255, 68%), followed by adapting to the novel instruments (n=86, 22.9%) and hand-eye coordination (n=34, 9.1%). The most helpful training method to help the spinal endoscopic surgeon of the younger generation improve was operating on simulation models or cadaver courses (n=216, 57.6%), followed by online or offline theoretical courses (n=67, 17.9%), acquiring opportunities during surgeries (n=51, 13.6%), and frequently participating in surgeries as an assistant (n=41, 10.9%) (Figure 4).
Discussion
The steep learning curve of this state-of-the-art technique has long been mentioned in many previous studies (10–12). Kotheeranurak et al. conducted an online survey about the learning curve, motivation, and obstacles of full-endoscopic spinal surgery in Thailand. They drew the conclusion that the trend of endoscopic spinal surgery has continued to grow and that the appropriate number of cases until one felt confident was approximately 28. The primary motivator and obstacles were personal interest and lack of support (15). Hsu et al. retrospectively evaluated the clinical presentation of 57 patients who underwent full-endoscopic lumbar discectomy and 66 patients who underwent open microdiscectomy using Spearman's coefficient of rank correlation (rho) to assess the learning curves for the transforaminal and interlaminar procedures of full-endoscopic lumbar discectomy. They believed that the transforaminal approach had a steep and easy learning curve, whereas the learning curve of the interlaminar approach was deemed flat and difficult (16). Gadjradj et al. conducted a study by observing the clinical outcomes during and after the learning curve (20 cases) presented by three surgeons new to spinal endoscopy. They later determined that spinal endoscopic surgery had a relevant steep learning curve and that young spinal surgeons should use the endoscope under the supervision of a senior surgeon (17).
In order to uncover the deeper factor for this challenging issue, the present study conducted a survey of 375 spinal endoscopic surgeons to reveal what matters to the growth of a young, medical professionals. Through the screening based on questions 3–7, it was determined that they were all peers who were dedicated specifically to this method. It was critical that the survey be representative. Despite their varied backgrounds, most of the respondents performed well in endoscopic surgery according to questions 8–10 of the survey. The study pointed out that the majority of surgeons thought the threshold for a surgeon to be skilled in spinal endoscopy was at least 300 cases. In fact, surgeons may face many challenges in the initial phase of practicing this technique, such as a lengthy operating time, a high complication rate, and even failure to finish the procedure (18–20). However, they should be patient and persevere rather than be dejected in order to add to their experiences regularly. There is also evidence that the situation will improve over time (17). According to the surgeons, the most difficult aspect of mastering this technique is the disparate surgical view (21). Unlike conventional open surgery or the cadaver specimens that medical students see regularly in medical school, the surgical view from a spinal endoscopy is entirely different because its limited view with the amplified image by the lens will make the normal-sized anatomic sites appear fairly magnified, which might confuse the beginners when recognizing the anatomic landmarks (22). Hence, great importance should be given to training. Based on the survey, the most beneficial training method for surgeons was operating on simulation models or cadaver courses. This conveyed a vital message to organizations and manufacturers who are dedicated to promoting the technique and helping less-experienced surgeons. Even though cadavers are not always available, especially in some regions, it is satisfying to see peers develop innovative alternative training programs (23, 24). This trend is in line with the survey, and it should be maintained for our efforts to be worthwhile.
Conclusion
From the perspective of surgeons, to be skilled in spinal endoscopic surgery means overcoming a steep learning curve. However, more importance should be attached to training systems so that younger generations of surgeons can operate on simulation models or take cadaver courses.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
YX and QZ contributed equally to this work and should be considered the first authors. YY and XF are jointly responsible for the project and should be considered the corresponding authors. YY and XF organized and supervised the case report. YX and QZ collected the literature and wrote the article. CF and YW performed, recorded, and audited the article. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Chengdu Science and Technology Bureau (No. 2022-YF05-02035-SN), and China Geriatric Health Care Association (CAWA202105281637000503382-09).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2023.1116376/full#supplementary-material.
References
1. Simpson AK, Lightsey HM 4th, Xiong GX, Crawford AM, Minamide A, Schoenfeld AJ Spinal endoscopy: evidence, techniques, global trends, and future projections. Spine J. (2022) 22(1):64–74. doi: 10.1016/j.spinee.2021.07.004
2. Khandge AV, Sharma SB, Kim JS. The evolution of transforaminal endoscopic spine surgery. World Neurosurg. (2021) 145:643–56. doi: 10.1016/j.wneu.2020.08.096
3. Ahn Y. A historical review of endoscopic spinal discectomy. World Neurosurg. (2021) 145:591–6. doi: 10.1016/j.wneu.2020.08.008
4. Chen B, Li S, Wang Z. Clinical efficacy of percutaneous transforaminal endoscopic TESSYS technique in the treatment of senile lumbar spinal stenosis. Am J Transl Res. (2021) 13(8):9356–63.34540053
5. Pan M, Li Q, Li S, Mao H, Meng B, Zhou F, et al. Percutaneous endoscopic lumbar discectomy: indications and complications. Pain Physician. (2020) 23(1):49–56.32013278
6. Meng SW, Peng C, Zhou CL, Tao H, Wang C, Zhu K, et al. Massively prolapsed intervertebral disc herniation with interlaminar endoscopic spine system delta endoscope: a case series. World J Clin Cases. (2021) 9(1):61–70. doi: 10.12998/wjcc.v9.i1.61
7. Lohre R, Wang JC, Lewandrowski KU, Goel DP Virtual reality in spinal endoscopy: a paradigm shift in education to support spine surgeons. J Spine Surg. (2020) 6(Suppl 1):S208–23. doi: 10.21037/jss.2019.11.16
8. Sclafani JA, Kim CW. Complications associated with the initial learning curve of minimally invasive spine surgery: a systematic review. Clin Orthop Relat Res. (2014) 472(6):1711–7. doi: 10.1007/s11999-014-3495-z
9. Lewandrowski KU, Telfeian AE, Hellinger S, Jorge Felipe RamÍrez León , Paulo Sérgio Teixeira de Carvalho Ramos MRF, et al. Difficulties, challenges, and the learning curve of avoiding complications in lumbar endoscopic spine surgery. Int J Spine Surg. (2021) 15(suppl 3):S21–37. doi: 10.14444/8161
10. Son S, Ahn Y, Lee SG, Kim WK, Yoo BR, Jung JM, et al. Learning curve of percutaneous endoscopic transforaminal lumbar discectomy by a single surgeon. Medicine. (2021) 100(4):e24346. doi: 10.1097/MD.0000000000024346
11. Kim JE, Yoo HS, Choi DJ, Hwang JH, Park EJ, Chung S. Learning curve and clinical outcome of biportal endoscopic-assisted lumbar interbody fusion. Biomed Res Int. (2020) 2020:8815432. doi: 10.1155/2020/8815432
12. Yang J, Guo C, Kong Q, Zhang B, Wang Y, Zhang L, et al. Learning curve and clinical outcomes of percutaneous endoscopic transforaminal decompression for lumbar spinal stenosis. Int Orthop. (2020) 44(2):309–17. doi: 10.1007/s00264-019-04448-1
13. Lin GX, Kotheeranurak V, Mahatthanatrakul A, Ruetten S, Yeung A, Lee SH, et al. Worldwide research productivity in the field of full-endoscopic spine surgery: a bibliometric study. Eur Spine J. (2020) 29(1):153–60. doi: 10.1007/s00586-019-06171-2
14. Lewandrowski KU, Soriano-Sánchez JA, Zhang X, RamÍrez León JF, Soriano Solis S, Rugeles OrtÍz JG, et al. Regional variations in acceptance, and utilization of minimally invasive spinal surgery techniques among spine surgeons: results of a global survey. J Spine Surg. (2020) 6(Suppl 1):S260–74. doi: 10.21037/jss.2019.09.31
15. Kotheeranurak V, Liawrungrueang W, Kuansongtham V, Sriphirom P, Bamrungthin N, Keorochana G, et al. Surgeons’ perspective, learning curve, motivation, and obstacles of full-endoscopic spine surgery in Thailand: results from a nationwide survey. Biomed Res Int. (2022) 2022:4971844. doi: 10.1155/2022/4971844
16. Hsu HT, Chang SJ, Yang SS, Chai CL. Learning curve of full-endoscopic lumbar discectomy. Eur Spine J. (2013) 22(4):727–33. doi: 10.1007/s00586-012-2540-4
17. Gadjradj PS, Vreeling A, Depauw PR, Schutte PJ, Harhangi BS, PTED-Study Group. Surgeons learning curve of transforaminal endoscopic discectomy for sciatica. Neurospine. (2022) 19(3):594–602. doi: 10.14245/ns.2244342.171
18. Zhou C, Zhang G, Panchal RR, Ren X, Xiang H, Xuexiao M, et al. Unique complications of percutaneous endoscopic lumbar discectomy and percutaneous endoscopic interlaminar discectomy. Pain Physician. (2018) 21(2):E105–12.29565953
19. Lee DY, Lee SH. Learning curve for percutaneous endoscopic lumbar discectomy. Neurol Med Chir. (2008) 48(9):383–8; discussion 388–9. doi: 10.2176/nmc.48.383
20. Park SM, Kim HJ, Kim GU, Choi MH, Chang BS, Lee CK, et al. Learning curve for lumbar decompressive laminectomy in biportal endoscopic spinal surgery using the cumulative summation test for learning curve. World Neurosurg. (2019) 122:e1007–13. doi: 10.1016/j.wneu.2018.10.197
21. Hussain I, Yeung AT, Wang MY. Challenges in spinal endoscopy. World Neurosurg. (2022) 160:132–7. doi: 10.1016/j.wneu.2021.11.082
22. Hahn BS, Park JY. Incorporating new technologies to overcome the limitations of endoscopic spine surgery: navigation, robotics, and visualization. World Neurosurg. (2021) 145:712–21. doi: 10.1016/j.wneu.2020.06.188
23. Amato MCM, Aprile BC, de Oliveira CA, Carneiro VM, de Oliveira RS. Experimental model for interlaminar endoscopic spine procedures. World Neurosurg. (2019) 129:55–61. doi: 10.1016/j.wneu.2019.05.199
Keywords: spine endoscopic surgery, minimally invasive spine surgery, education, spinal endoscopic surgeon of younger generations, online survey
Citation: Xie Y, Zhou Q, Wang Y, Feng C, Fan X and Yu Y (2023) Training to be a spinal endoscopic surgeon: What matters?. Front. Surg. 10:1116376. doi: 10.3389/fsurg.2023.1116376
Received: 5 December 2022; Accepted: 14 February 2023;
Published: 6 March 2023.
Edited by:
Ji Tu, University of New South Wales, AustraliaReviewed by:
Vadim Byvaltsev, Irkutsk State Medical University, RussiaOsvaldo Mazza, Bambino Gesù Children's Hospital (IRCCS), Italy
© 2023 Xie, Zhou, Wang, Feng, Fan and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yang Yu c3BpbmVfeXlAMTYzLmNvbQ== Xiaohong Fan ZnhoMjAyMDEwQDE2My5jb20=
†These authors share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Yizhou Xie
Yizhou Xie Qun Zhou1,†
Qun Zhou1,† Chengzhi Feng
Chengzhi Feng Yang Yu
Yang Yu