- 1Key Laboratory of Biomechanics and Mechanobiology, Ministry of Education, Beijing Advanced Innovation Center for Biomedical Engineering, School of Biological Science and Medical Engineering, Beihang University, Beijing, China
- 2Engineering Research Center of Digital Medicine, Ministry of Education; School of Biomedical Engineering, Shanghai Jiao Tong University, Shanghai, China
- 3Department of Joint Surgery, Ningbo No.6 Hospital, Ningbo, China
Background: Component alignment is a crucial factor affecting the clinical outcome of total knee arthroplasty (TKA). Accelerometer-based navigation (ABN) systems were developed to improve the accuracy of alignment during surgery. This study aimed to compare differences in component alignment, clinical outcomes, and surgical duration when using conventional instrumentation (CONI), ABN, and computer navigation (CN) systems.
Methods: A comprehensive literature search was carried out using the Web of Science, Embase, PubMed, and Cochrane databases. Articles that met the eligibility criteria were included in the study. Meta-analyses were performed using the Cochrane Collaboration Review Manager based on Cochrane Review Method. The variables used for the analyses were postoperative clinical outcome (PCO), surgical duration, and component alignment, including the hip-knee-ankle (HKA) angle, coronal femoral angle (CFA), coronal tibial angle (CTA), sagittal femoral angle (SFA), sagittal tibial angle (STA), and the outliers for the mentioned angles. The mean difference (MD) was calculated to determine the difference between the surgical techniques for continuous variables and the odds ratio (OR) was used for the dichotomous outcomes.
Results: The meta-analysis of the CONI and ABN system included 18 studies involving 2,070 TKA procedures, while the comparison of the ABN and CN systems included 5 studies involving 478 TKA procedures. The results showed that the ABN system provided more accurate component alignment for HKA, CFA, CTA, and SFA and produced fewer outliers for HKA, CFA, CTA, and STA. However, while the ABN system also required a significantly longer surgical time than the CONI approach, there was no statistical difference in PCO for the two systems. For the ABN and CN systems, there was no statistical difference in all variables except for the ABN system having a significantly shorter surgical duration.
Conclusion: There was no significant difference in the accuracy of component alignment between the ABN and CN systems, but the ABN approach had a shorter surgical duration and at lower cost. The ABN system also significantly improved the accuracy of component alignment when compared to the CONI approach, although the surgery was longer. However, there was no significant difference in PCO between the CONI, ABN, and CN systems.
Introduction
Knee osteoarthritis (OA) is one of the most common musculoskeletal disorders, reportedly affecting over 300 million people globally (1). Total knee arthroplasty (TKA) is an effective treatment for severe knee OA and, due to successive developments over the past several decades, this treatment boasts an excellent survival rate (2). However, about 20% of patients report dissatisfaction with postoperative outcomes because of pain and restricted knee function (3). Previous studies demonstrated that the alignment of the knee prosthesis was a key factor influencing postoperative clinical outcomes (4, 5). Malalignment of the prosthesis can affect the mechanics and kinematics of the joint, such as femoral roll-back, tibial rotation, and stress on the ligaments and insert, as well as increasing the wear rate of polyethylene components (6–10). Some prosthetic designs can also take longer to insert, with longer surgical durations being linked to an increased risk of clinical complications and revision (11, 12).
Conventional instrumentation (CONI) is the most widely used apparatus for implanting knee prostheses and uses an intramedullary guide for femoral bone resection and extramedullary tibial bone resection. However, it is difficult to maintain accurate component alignment using this method, with studies showing that about 40% of the coronal and sagittal alignments errors were more than 3 degree which was regarded as the outliers of TKA procedures, and there are more outliers for the femoral component than the tibial component (13). Computer navigation (CN) systems using optical positioning have been developed to improve the accuracy of component alignment during TKA, with results showing fewer outliers and better long-term clinical scores than the CONI system (14, 15). However, computerized systems are relatively novel and complex and so have a higher cost and longer surgical duration (16, 17). Accelerometer-based navigation (ABN) systems are portable surgical navigation systems based on the inertial measurement unit (IMU). ABN has been reported with more accurate alignment than CONI and lower cost than CN systems. Studies have attempted to compare component alignment, surgical duration, and clinical outcomes between the ABN system and CONI, but the results were inconsistent. Li et al. reported that the ABN system could improve the precision of the alignment, but required a longer surgical time (18). Sun et al. suggested that the ABN system could reduce the number of outliers, but there was no significant difference with CONI in terms of the mean values of the alignments, and there was a negligible difference in surgical duration (19). The possible reasons for these discrepancies might be the not latest literature which the studies included in the two analyses were published before 2019. Such previous studies also did not include the CN system in the evaluation, so it is not known how effective this system is by comparison.
Therefore, the purpose of this study is to compare component alignment, surgical duration, and clinical outcomes of TKA procedures performed with conventional instrumentation (CONI), an accelerometer-based navigation (ABN) system, and a computer navigation (CN) system. It was hypothesized that the ABN system would produce a more accurate joint alignment, better clinical outcomes, and require a shorter surgical duration.
Materials and methods
This systematic review and meta-analysis were based on the Cochrane Review Method and reported using the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA). The review protocol was registered in the International Prospective register of systematic reviews [CRD42022363153].
Search strategy and study selection
A comprehensive literature search was carried out using Web of Science, Embase, PubMed, and Cochrane databases. The following terms were used: “arthroplasty, replacement, Knee” and “accelerometer”. For example, the search strategy in PubMed was “[arthroplasty, replacement, knee (MeSH Terms)] AND (accelerometer)”. All publications in English and Chinese up to June 2022 were collected. Relevant studies were identified by the title and abstract of each article. The full text was then reviewed using the eligibility criteria below to confirm whether to include the article in this study.
Eligibility criteria
Publications were included in this study if they that met the following inclusion criteria: (1) The experimental group used an accelerometer-based navigation (ABN) system in primary TKA. (2) The control group used conventional instrumentation or computer navigation systems in primary TKA. (3) All the TKA procedures were operated by performed using mechanical alignment. (4) At least one of the following outcomes was included: surgical duration, postoperative clinical outcomes (PCO), hip-knee-ankle angle (HKA), coronal femoral angle (CFA), coronal tibial angle (CTA), sagittal femoral angle (SFA), sagittal tibial angle (STA), and the outliers for the mentioned angles, (5) The studies were randomized controlled trials (RCT) or prospective and retrospective nonrandomized controlled trials (nRCT).
Quality assessment
The risk of bias in the included studies was evaluated by two reviewers according to the Cochrane risk of bias tool. The assessed parameters included randomization procedure, allocation concealment, blinding of patients and surgeons, blinding of outcome assessors, selective outcome reporting, incomplete outcome data, and other biases. Each parameter was judged as a having high, low, or unclear risk of bias by the two reviewers independently. A discussion proceeded in case of any disagreements in the bias judgment.
Data extraction and analysis
The data was extracted from the included studies by the two reviewers. The information on the publications included the first author, year of publication, sample size, ABN device, and implant system. Patient information included age, gender, and body mass index (BMI). The primary outcomes were postoperative alignment parameters, including HKA, CFA, CTA, SFA, STA, and their outliers. The rotational alignment was not extracted from the studies since the rotational alignment was not considered in any of the currently approved ABN systems. The secondary outcome was the postoperative clinical outcome. The surgical duration was regarded as the tertiary outcome. Any discrepancies in the extracted data were resolved by discussion among the reviewers.
Statistical analysis
A meta-analysis of the comparison between the ABN and CONI systems and between the ABN and CN systems was performed using the Cochrane Collaboration Review Manager 5.4 software. For continuous variables, such as the alignment angles, clinical outcomes, and surgical duration, the mean difference (MD) was calculated with the Inverse-Variance method to show the difference between the surgical techniques. The odds ratio (OR) was used with the Mantel-Haenszel method to determine discrepancies between the surgical techniques for the dichotomous outcomes, such as the number of outliers of the measured alignment angles. The 95% confidence interval (CI) of the MD and OR was calculated for each study. The I2 statistic was used to assess the heterogeneity. A fixed model was utilized for the variables where I2 < 50% and a random model was used where I2 > 50%. Values of P < 0.05 were considered statistically significant.
Results
Study selection
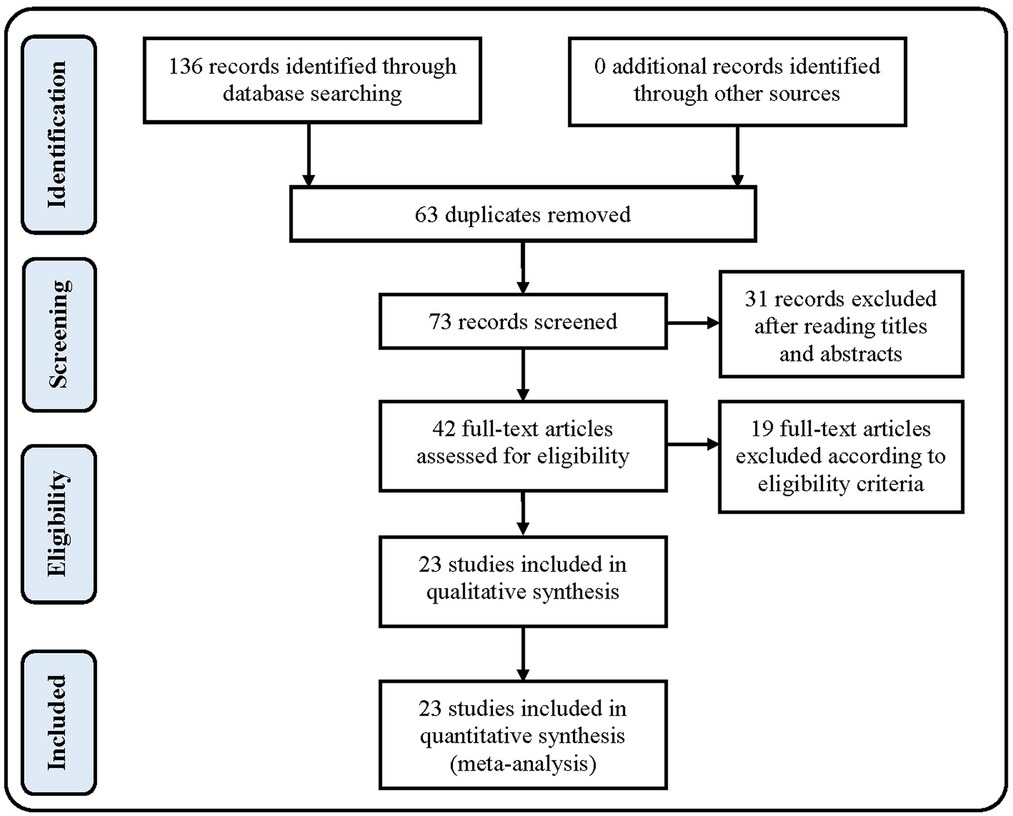
The screening process of the included studies is shown in Figure 1. One hundred and thirty-six publications were identified through the database search, sixty-three of which were excluded because of duplicates and another thirty-one were excluded after reading the title and abstract. Of the remaining forty-two full-text articles, twenty-three articles (20–42) met the eligibility criteria and were included in this study. eighteen articles compared the ABN and CONI systems, and five articles compared the ABN and CN systems.
Characteristics
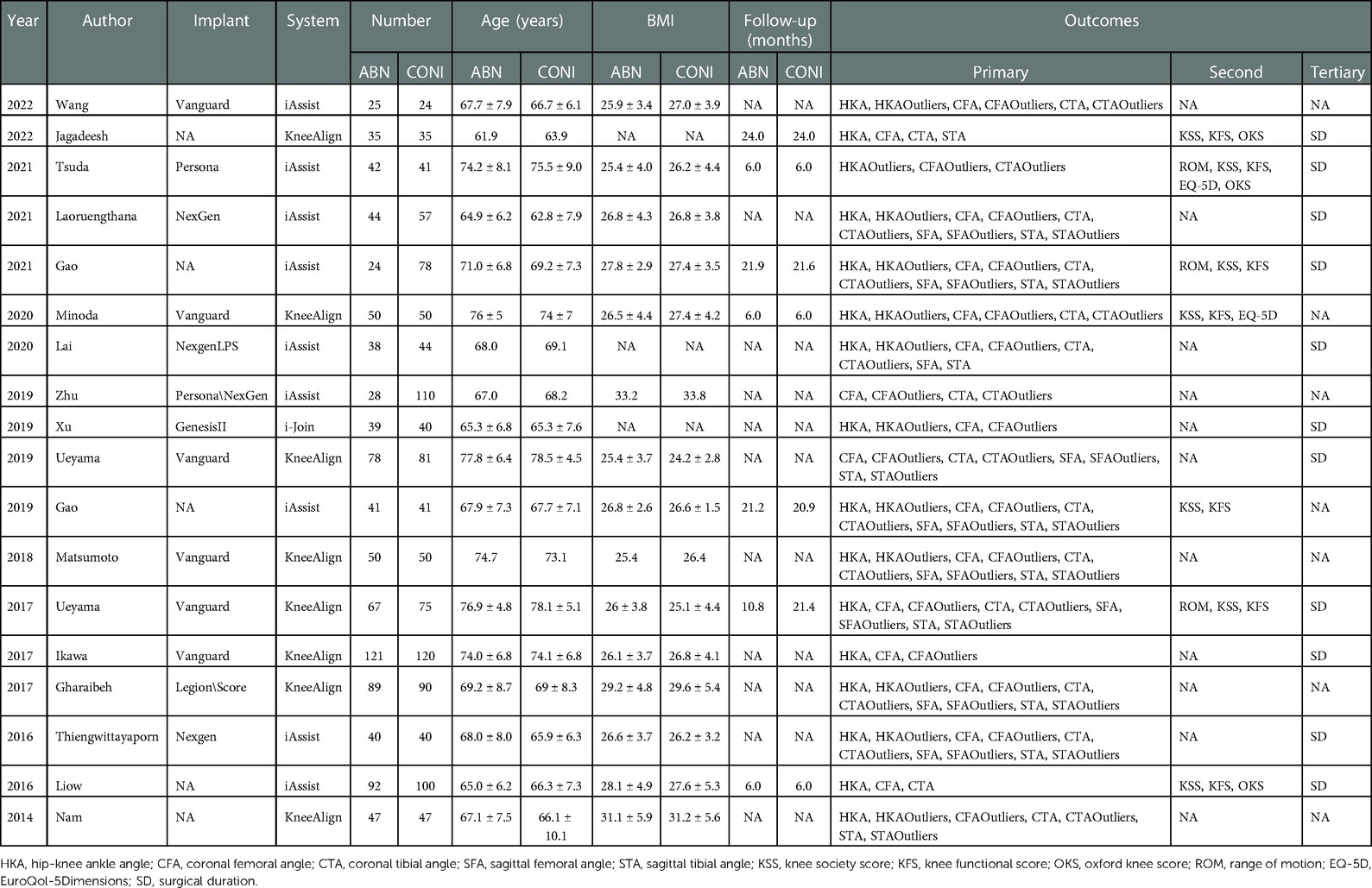
Table 1 details the characteristics of the studies for the meta-analysis of the ABN and CONI systems. The eighteen studies included in this report assessed a total of 2,070 TKA procedures, of which 947 used the ABN system and the remaining 1,123 patients underwent conventional surgery. The ABN system used in most cases was either iAssist® (Zimmer Biomet Inc., Warsaw, IN, USA) or KneeAlign® (OrthAlign Inc., Columbia, CA, USA), while one study used i-Join® (i-Join Medical Technology Inc., Shanghai, China). The mean age of the patients in the ABN group and CONI group was 70.58 and 70.24 years old, respectively, and the average BMI of the patients was 27.15 and 27.77, respectively. All of the included studies reported at least one primary outcome, and 7 studies also reported the PCO scores (secondary outcome). 11 studies reported the surgical duration (tertiary outcome).
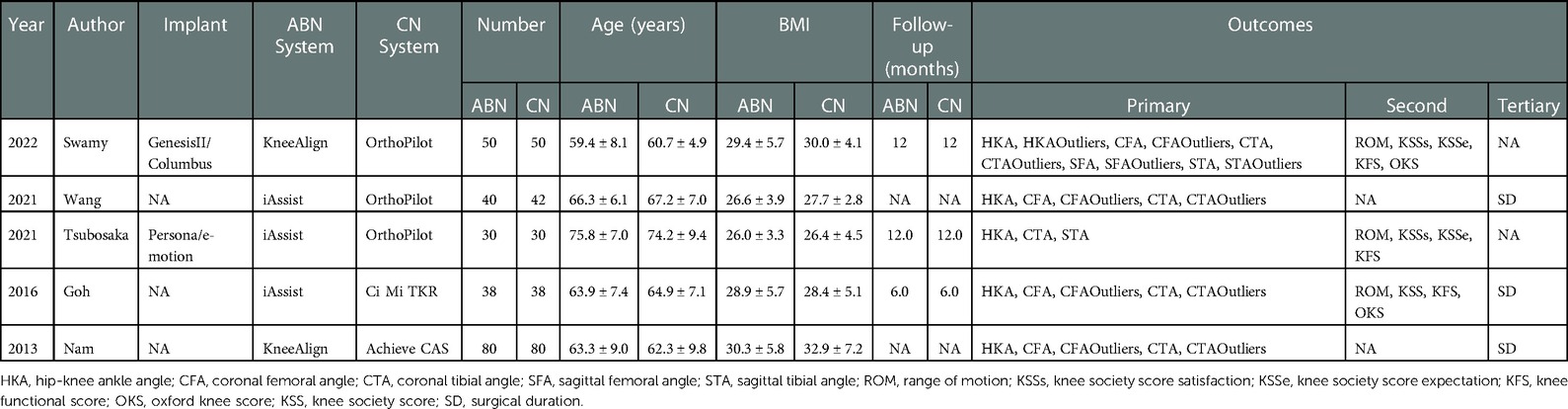
Table 2 shows the characteristics of the studies for the meta-analysis of the ABN and CN systems. The five studies included in this report assessed a total of 478 TKA procedures, of which 238 used the ABN system and the remaining 240 patients underwent computer navigation surgery. The iAssist® and KneeAlign® systems were used in the ABN group. The computer navigation system included AchieveCAS® (Smith & Nephew Inc., Memphis, Tennessee, USA), Ci Mi TKR® (BrainLab/DePuy Orthopaedics Inc. Munich, Germany), and OrthoPilot® (B. Braun Aesculap Inc., Tuttlingen, Germany). The mean age of the patients in the ABN Group and CN Group was 64.66 and 64.72 years old, respectively, and the patients had an average BMI of 28.72 and 29.86, respectively. All of the included studies reported at least one primary outcome, 3 studies described the PCO scores (secondary outcome), and 3 studies reported the surgical duration (tertiary outcome).
Risk of bias
The risk of bias for the included studies is shown in Figure 2A. The risk of selection bias and performance bias was not unclear because information on the randomization process and blinding of participants and personnel in some of the included studies were not described in sufficient detail. All studies reported the complete outcome data. The overall risk of bias for all studies is shown in Figure 2B, with each measure being presented as a percentage. The funnel plots of the coronal femoral angle were shown in Figure 2C which indicated a low publication bias.
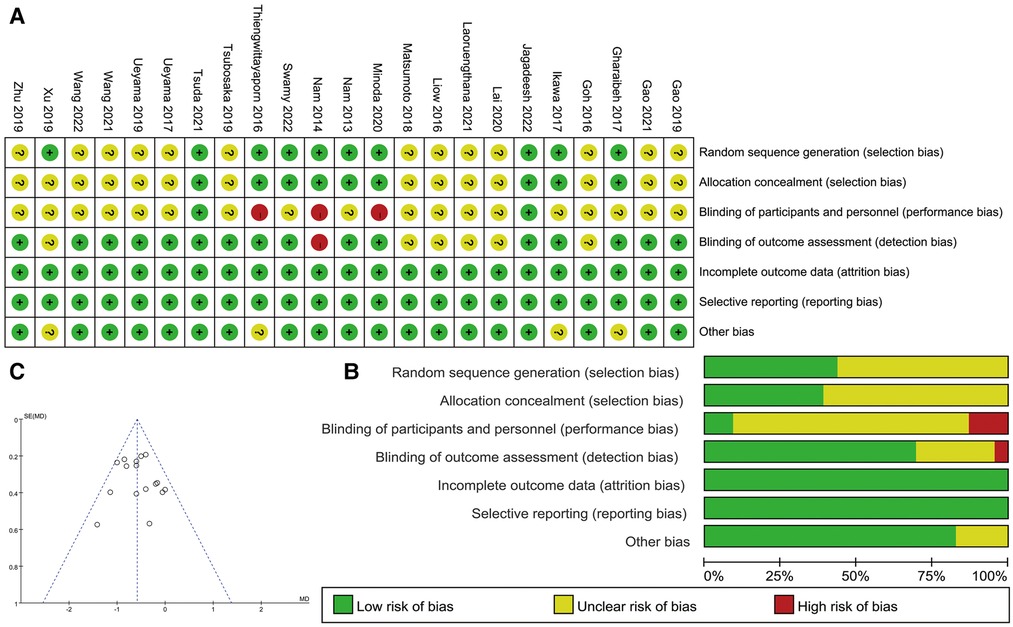
Figure 2. (A) Risk of bias for the included studies (+: low risk, ?: unclear risk, −: high risk); (B) overall risk of bias for all studies; (C) the funnel plots of the coronal femoral angle.
Primary outcome
Fourteen studies reported the postoperative hip-knee-ankle (HKA) angle when using the ABN system or CONI approach. The results suggest that the ABN system allows for more accurate lower limb alignment (Figure 3A, MD: −0.64, 95% CI: −0.92 to −0.35, P < 0.0001, I2 = 59%). The results of five studies comparing the HKA when using the ABN and CN systems did not show any significant difference between the two alignment techniques (Figure 3B, MD: −0.26, 95% CI: −0.55 to −0.04, P = 0.08, I2 = 0%).
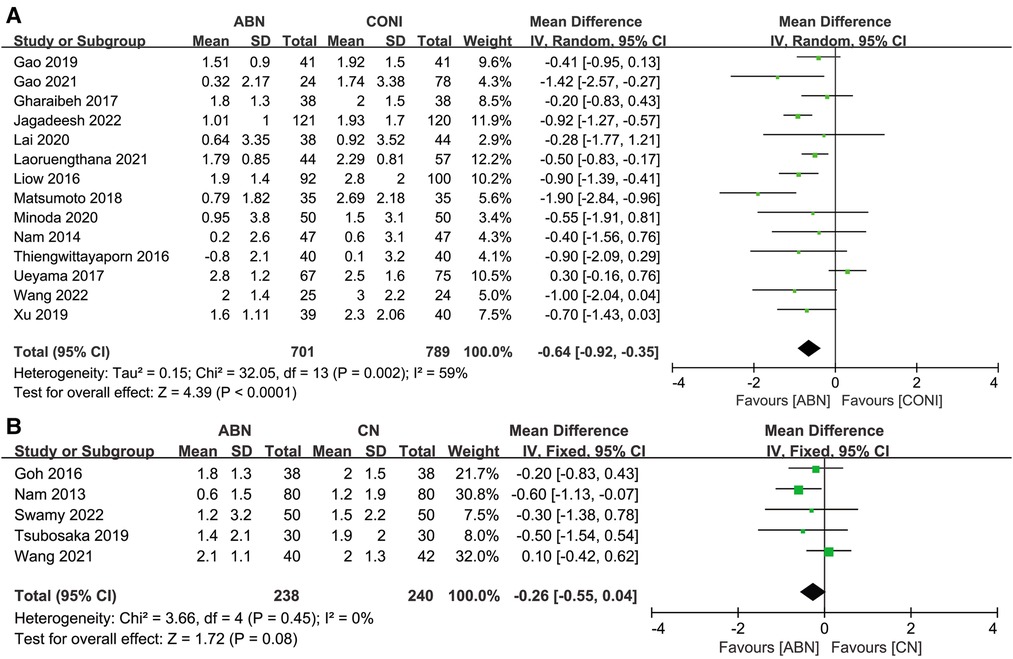
Figure 3. Forest plot of hip-knee-ankle (HKA) angle. (A) Accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
Details of outliers for HKA measurements for the ABN and CONI groups were documented in 11 articles, and the results suggested fewer outliers when using the ABN system (Figure 4A, OR:0.44, 95% CI: 0.31 to 0.61, P < 0.00001, I2 = 37%). Only four studies compared HKA outliers between the ABN and CN systems, and no significant differences were re-ported (Figure 4B, OR:0.75, 95% CI: 0.41 to 1.40, P = 0.37, I2 = 0%).

Figure 4. Forest plot of HKA outliers. (A) Accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
Sixteen studies compared the coronal femoral angle (CFA) when using the ABN and CONI approaches, with the results showing that the ABN system provides more accurate alignment (Figure 5A, MD: −0.58, 95% CI: −0.72 to −0.44, P < 0.00001, I2 = 14%). A further four studies compared the CFA for the ABN and CN systems, and no significant difference was found (Figure 5B, MD: −0.28, 95% CI: −0.86 to 0.31, P = 0.36, I2 = 74%).
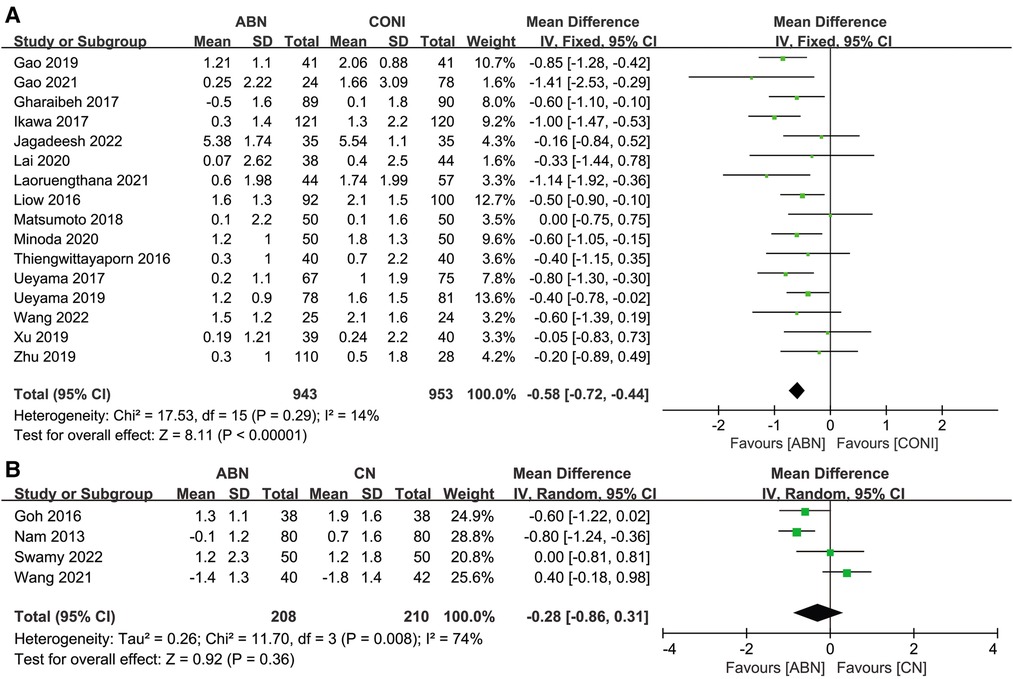
Figure 5. Forest plot of coronal femoral angle (CFA). (A) Accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
Fourteen studies assessed CFA outliers recorded following surgery using the ABN and CONI approach. The results showed fewer outliers in the ABN group (Figure 6A, OR: 0.39, 95% CI: 0.28 to 0.54, P < 0.00001, I2 = 53%). Only four articles assessed differences in CFA outliers between the ABN and CN groups, with the results showing no significant difference between the two groups (Figure 6B, OR: 0.58, 95% CI: 0.30 to 1.13, P = 0.11, I2 = 0%).
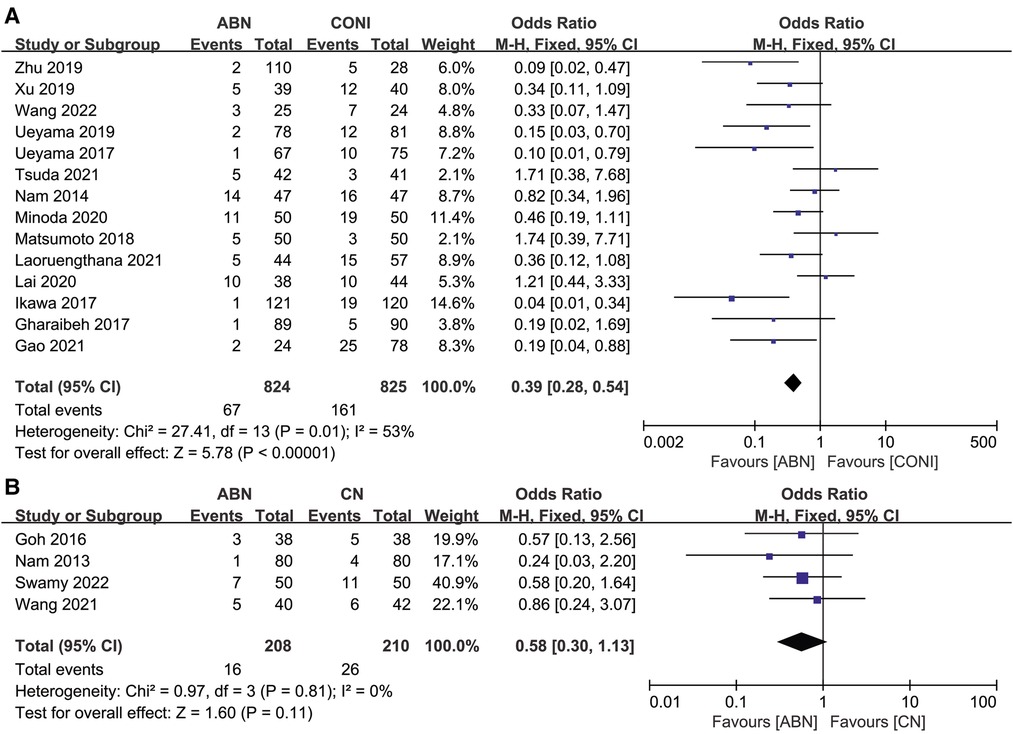
Figure 6. Forest plot of CFA outliers. (A) Accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
Fifteen studies reported on the measurements for the coronal tibial angle (CTA) following ABN and CONI. As with previous measurements, the ABN system was capable of more accurate alignment (Figure 7A, MD: −0.40, 95% CI: −0.66 to −0.14, P = 0.003, I2 = 74%). Five studies recorded the CTA following ABN and CN, with no significant difference reported be-tween the results for the two systems (Figure 7B, MD: 0.01, 95% CI: −0.19 to 0.20, P = 0.94, I2 = 28%).
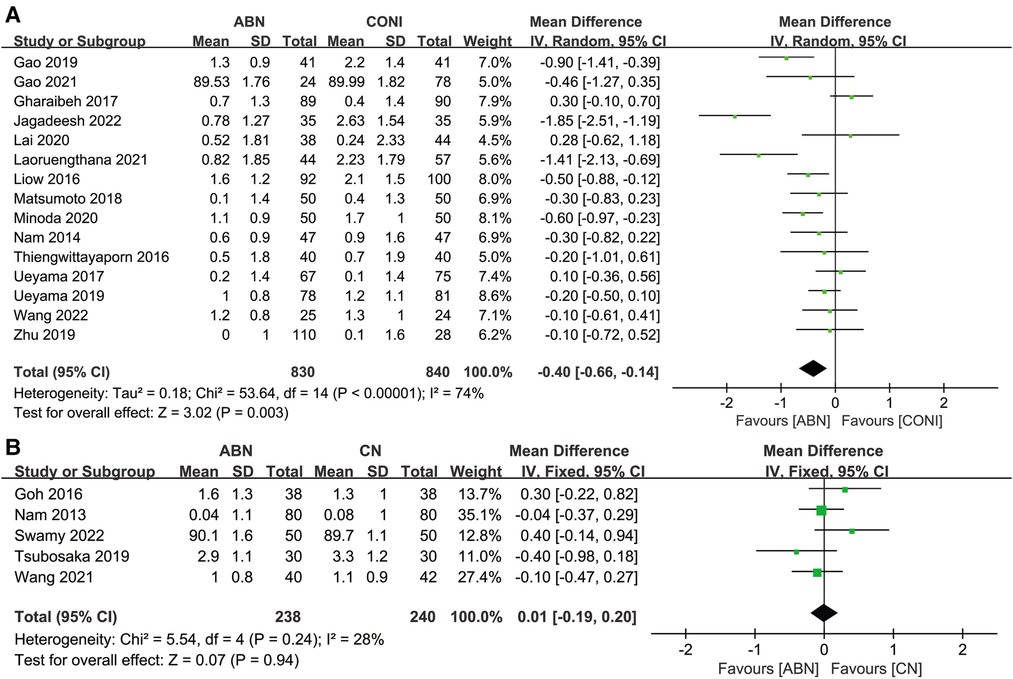
Figure 7. Forest plot of coronal tibial angle (CTA). (A) Accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
Fourteen articles presented the CTA outliers after performing surgery using ABN and CONI, with the fewer outliers reported for the ABN group (Figure 8A, OR: 0.28, 95% CI: 0.19 to 0.43, P < 0.00001, I2 = 0%). Four studies compared CTA outliers for the ABN and CN groups, with no significant difference reported between the two groups (Figure 8B, OR:2.23, 95% CI: 0.89 to 5.56, P = 0.09, I2 = 0%).
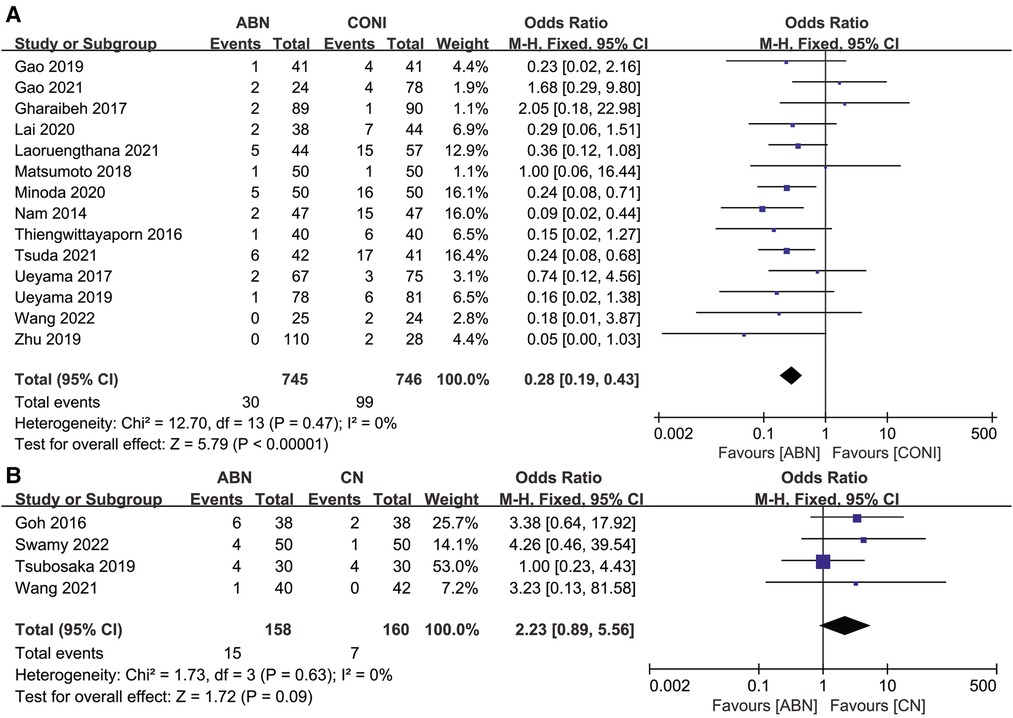
Figure 8. Forest plot of CTA outliers. (A) Accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
Nine articles reported on the sagittal femoral angle (SFA) after using the ABN and CONI approach. As expected, the ABN system provided more accurate alignment (Figure 9A, MD: −0.53, 95% CI: −0.92 to −0. 14, P = 0.007, I2 = 62%). However, there was no significant difference in SFA outliers for the two approaches (Figure 9B, OR:0.57, 95% CI: 0.32 to 1.02, P = 0.06, I2 = 54%). Only one study compared the SFA and outliers for the ABN and CN systems, with the results showing no significant difference between the two groups (P = 0.51) (33).
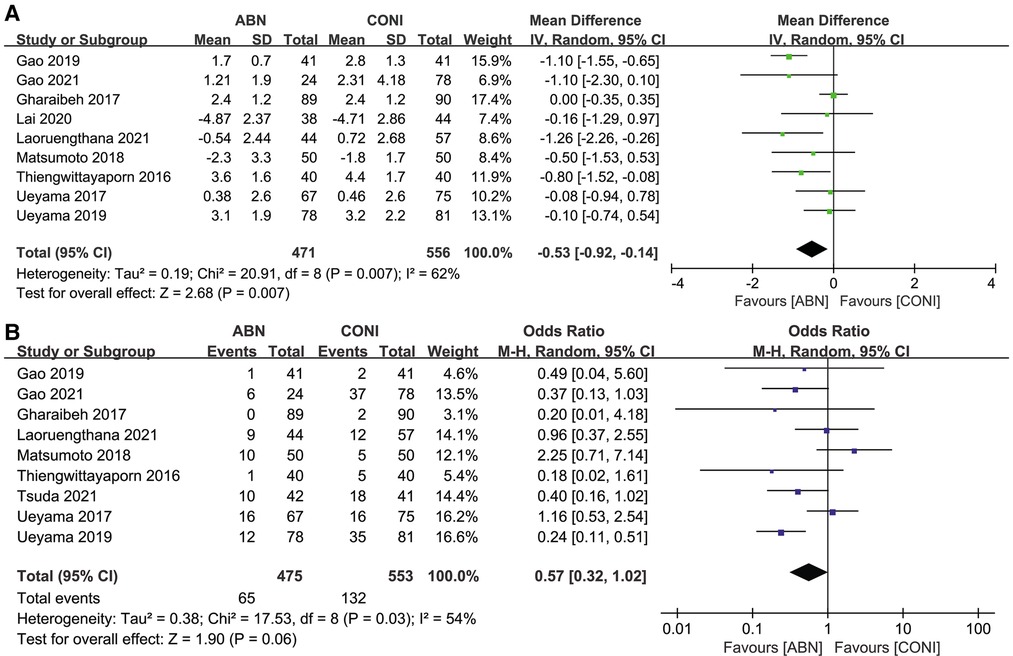
Figure 9. Forest plot of sagittal femoral angle (SFA). (A) And SFA outliers (B) between accelerometer-based navigation (ABN) system and conventional instrumentation (CONI).
Eleven articles assessed the sagittal tibial angle (STA) recorded wen using the ABN and CONI approach. The differences between the two groups were not significant (Figure 10A, MD: 0.09, 95% CI: −0.59 to 0.77, P = 0.80, I2 = 89%). Nine studies reported on STA outliers and the results suggested fewer outliers with the ABN approach (Figure 10B, OR:0.46, 95% CI: 0.31 to 0.68, P = 0.0001, I2 = 35%). Only 1 study reported on the STA and its outliers following the ABN and CN approaches. No significant difference was identified for the STA (P = 0.36) or its outliers (P = 0.15) (33).

Figure 10. Forest plot of sagittal tibial angle (STA). (A) And STA outliers (B) between accelerometer-based navigation (ABN) system and conventional instrumentation (CONI).
Secondary outcome
For the secondary outcome in this current study, seven articles report on short-term postoperative clinical outcomes (PCO) following surgery using the ABN and CONI approaches. Analysis of the results did not identify any significant difference between the two groups (Figure 11A, MD:0.11, 95% CI: −0.11 to 0.33, P = 0.34, I2 = 55%). Three articles compared the short-term PCO for the ABN and CN groups. The difference between the groups was not significant (Figure 11B, MD: 0.74, 95% CI: −1.15 to 2.63, P = 0.44, I2 = 0%).

Figure 11. Forest plot of postoperative clinical outcomes (PCO). (A) Accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
Tertiary outcome
For the tertiary outcome on surgical duration, eleven articles assessed the duration required when using the ABN and CONI approach. The results showed that using the ABN system significantly prolonged the surgical time (Figure 12A, MD: 4.81, 95% CI: 1.36 to 8.26, P = 0.006, I2 = 70%). Three studies assessed the required surgical duration when using the ABN and CN systems, and was found that the surgical time with the CN system was significantly longer (Figure 12B, MD: −8.65, 95% CI: −16.08 to −1.21, P = 0.02, I2 = 73%).
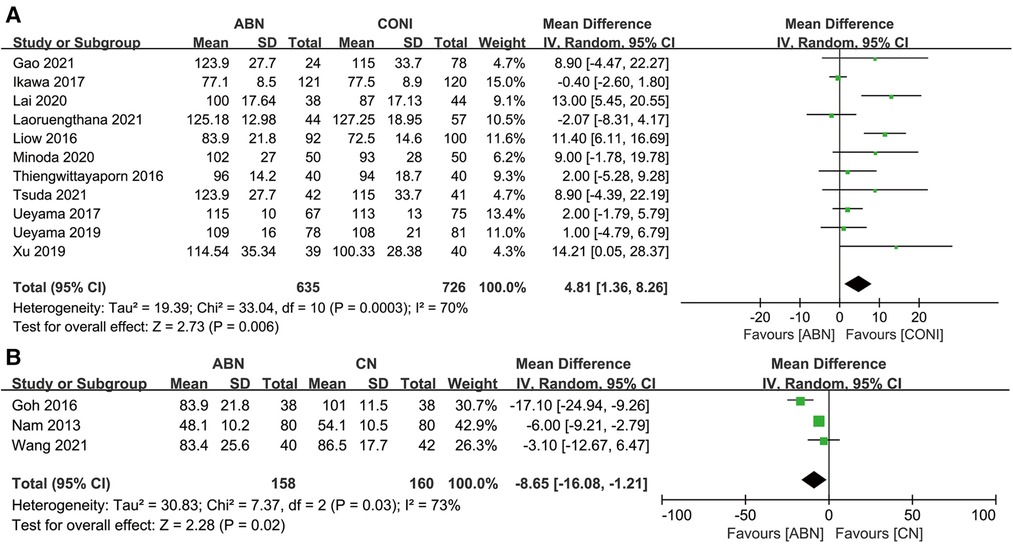
Figure 12. (A) Forest plot of surgical duration A: accelerometer-based navigation (ABN) system vs. conventional instrumentation (CONI); (B) ABN system vs. computer navigation (CN) system.
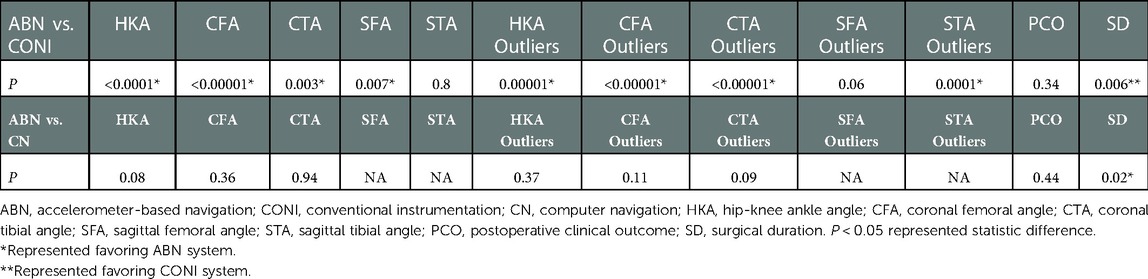
The P values of all the outcomes from the meta-analysis are shown in Table 3. Statis-tical differences were found between the ABN and CONI groups for HKA, CFA, CTA, SFA, HKA outliers, CFA outliers, CTA outliers, STA outliers, and surgical duration. However, no statistical differences were found between the ABN and CN groups, except for with surgical duration.
Discussion
The main finding of this study is that using an accelerometer-based navigation (ABN) system during total knee arthroplasty improves the accuracy of coronal and sagittal alignments and generates fewer outliers compared with conventional instrumentation. However, the ABN system also prolongs the surgical time and there was no statistical difference in postoperative clinical outcomes. The results also did not show any significant differences in coronal alignments, outliers, and postoperative clinical outcomes between the ABN and CN systems, but using the ABN system resulted in a shorter surgery.
Component alignment is regarded as one of the most crucial factors affecting postoperative functionality and clinical outcomes (4, 5). This study found that using the ABN system resulted in more accurate alignment and fewer outliers than with CONI, which could allow the centers of the femoral head and ankle joint to be more precisely located during surgery. The accelerometer and gyroscope with the ABN system permit the mechanical axis of the lower extremity to be identified, which is then used to guide the resection of the distal femur and proximal tibia on the coronal and sagittal planes. The CONI approach uses an intramedullary guidance system for femoral bone resection, with a rod being used to represent the anatomical axis of the femur. However, the accuracy of the anatomical axis can be affected by the location of the entry point and direction of insertion, as well as femoral deformities such as the sagittal bowing, which can lead to malalignment (43, 44). Also, the alignment accuracy of the femoral and tibial components could be confirmed during the ABN surgery. These characteristics of the ABN system led to more accurate alignment than the CONI approach. However, a longer surgical duration is required when using the ABN system, with 9 of 11 studies showing that the ABN system prolonged the surgical time more than CONI. This may be due to the calculation of the centers of the femoral head and ankle joint which requires the surgeon to swing the leg more than 13 times during the surgery. Moreover, the 3 studies included in the meta-analysis of ABN and CN systems indicated that the CN system required a significantly longer surgical time. A possible reason is the more complicated procedure which required the placements of pin trackers and bone registration. In contrast, the surgical techniques and tools used with the ABN system are more similar to the conventional instrumentation, which most surgeons are familiar with. Compared with conventional instrumentation (CONI), computer navigation (CN) based on image-guidance improves the accuracy of component alignment, but the longer surgical duration than both CONI and ABN might increase the risk of wound complications (45). The additional cost and complications with pin trackers, such as femoral shaft fracture, also limit the widespread application of CN systems (46–48).
The use of ABN and CN systems results in less blood loss for the patient because they do not require intramedullary nailing for navigation (24, 49). This is beneficial for rehabilitation and improving clinical outcomes (49). However, the meta-analysis in this study did not show any statistically significant difference in postoperative outcomes between the ABN system and CONI approach, which is supported by previous studies (18, 19). There is no evidence to indicate that the ABN and CN systems improve long-term clinical outcomes, although they have been shown to improve the accuracy of the alignments. Studies have demonstrated that component rotational alignment plays a key role in knee mechanics and kinematics and can have a demonstratable effect on postoperative clinical outcome (6, 8, 9). Complications like anterior knee pain, patellar subluxation, excessive polyethylene wear, and early failure have been associated with component malrotation. Similarly, errors with internal rotational alignment of the tibial component have been reported as a major cause of knee pain after TKA (7, 50, 51). Unfortunately, none of the studies assessed used an ABN system for rotational alignment on the transverse plane. Future work may consider using an approved ABN system for the rotational alignment of components during TKA surgery, which may further improve clinical outcomes. Kinematical alignment (KA) is a method that differed from the mechanical alignment (MA) for TKA. Previous studies demonstrated that the clinical outcomes of TKA procedures with KA were better than MA (52, 53). However, the requirement for accuracy of bone resection and alignment in KA was much higher. Besides, functional alignment (FA) is a new method based on navigation and robots which aimed to reduce the damage to the soft tissues and enhance rehabilitation, as well as improve clinical outcomes. The ABN may promote the application of KA and FA by achieving a more accurate alignment. An inertial measurement unit (IMU) based on the accelerometer and gyroscope could also be incorporated into a wearable device to record joint activity during postoperative rehabilitation (54).
There are several limitations to this study. First, a small number of studies were included in the meta-analysis, especially when comparing the ABN and CN systems, the differences in sagittal alignments, and outliers between the ABN and CN systems were not analyzed, which might weaken the analysis. While the entire pool of relevant literature that was identified was included in the analysis, the relative novelty of ABN and CN systems meant there were few publications to assess. Besides, the follow-up period of the included studies varied widely, with the longest period being less than 2 years, which could not reliably predict long-term outcomes. Inconsistencies in the observation period may negatively influence the reliability of the pooled results.
Conclusion
The meta-analysis performed in this study suggested that the ABN system was simi-lar to the CN system in terms of the accuracy of component alignment, but had a longer surgical period. The ABN system also significantly improved the precision of alignments over the CONI approach, although it prolonged the surgical time, whereas the ABN system save the surgical time than the CN system. However, there was no significant difference in the postoperative clinical outcome when using the CONI, ABN, and CN systems.
Author contributions
YL and C-KC contributed to conception and design of the study. YL, HW, CF and MZ searched the literature and extracted the data. YL, JL, NZ, BL and JS checked the date and performed the statistical analysis. YL wrote the first draft of the manuscript. YL and C-KC interpreted the data. All authors contributed to manuscript revision, read, and approved the submitted version.
Funding
This research was funded by Ningbo Public Welfare Science and Technology project (grant number 2022S064), Yinzhou District Agriculture and Social Development Science and Technology Project (2022AS066), National Key Research and Development Program (grant number 2016YFC1101904) and Project of NINGBO Leading Medical & Health Discipline (grant number 2022-X13).
Acknowledgments
We would like to thank Colin McClean for his assistance with editing this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TKA, total knee arthroplasty; CONI, conventional instrumentation; CN, computer navigation; ABN, accelerometer-based navigation; IMU, inertial measurement unit; PCO, postoperative clinical outcomes; HKA, hip-knee-ankle angle; CFA, coronal femoral angle; CTA, coronal tibial angle; SFA, sagittal femoral angle; STA, sagittal tibial angle; RCT, randomized controlled trials; nRCT, nonrandomized controlled trials; BMI, body mass index; MD, mean difference; OR, odds ratio; CI, confidence interval; MA, mechanical alignment; KA, kinematical alignment; FA, functional alignment
References
1. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. (2018) 392(10159):1789–858. doi: 10.1016/S0140-6736(18)32279-7
2. Hamel MB, Toth M, Legedza A, Rosen MP. Joint replacement surgery in elderly patients with severe osteoarthritis of the hip or knee: decision making, postoperative recovery, and clinical outcomes. Arch Intern Med. (2008) 168(13):1430–40. doi: 10.1001/archinte.168.13.1430
3. Bourne RB, Chesworth BM, Davis AM, Mahomed NN, Charron KD. Patient satisfaction after total knee arthroplasty: who is satisfied and who is not? Clin Orthop Relat Res. (2010) 468(1):57–63. doi: 10.1007/s11999-009-1119-9
4. Valkering KP, Breugem SJ, van den Bekerom MP, Tuinebreijer WE, van Geenen RC. Effect of rotational alignment on outcome of total knee arthroplasty. Acta Orthop. (2015) 86(4):432–9. doi: 10.3109/17453674.2015.1022438
5. Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty. (2009) 24(4):570–8. doi: 10.1016/j.arth.2008.03.002
6. Liau JJ, Cheng CK, Huang CH, Lo WH. The effect of malalignment on stresses in polyethylene component of total knee prostheses–a finite element analysis. Clin Biomech. (2002) 17(2):140–6. doi: 10.1016/s0268-0033(01)00109-7
7. Johnston H, Abdelgaied A, Pandit H, Fisher J, Jennings LM. The effect of surgical alignment and soft tissue conditions on the kinematics and wear of a fixed bearing total knee replacement. J Mech Behav Biomed Mater. (2019) 100:103386. doi: 10.1016/j.jmbbm.2019.103386
8. Wang ZW, Wen L, Luan YC, Ma DS, Dong X, Cheng CK, et al. Restoration of joint inclination in total knee arthroplasty offers little improvement in joint kinematics in neutrally aligned extremities. Front Bioeng Biotechnol. (2021) 9:673275. doi: 10.3389/fbioe.2021.673275
9. Fang C, Luan Y, Wang Z, Shao L, Qu T, Cheng CK. Moderate external rotation of tibial component generates more natural kinematics than internal rotation after total knee arthroplasty. Front Bioeng Biotechnol. (2022) 10:910311. doi: 10.3389/fbioe.2022.910311
10. Ro J, Ro DH, Kang Y, Han HS, Shin CS. Biomechanical effect of coronal alignment and ligament laxity in total knee arthroplasty: a simulation study. Front Bioeng Biotechnol. (2022) 10:851495. doi: 10.3389/fbioe.2022.851495
11. Young SW, Mutu-Grigg J, Frampton CM, Cullen J. Does speed matter? Revision rates and functional outcomes in tka in relation to duration of surgery. J Arthroplasty. (2014) 29(7):1473–7.e1. doi: 10.1016/j.arth.2014.03.004
12. Morcos MW, Nowak L, Schemitsch E. Prolonged surgical time increases the odds of complications following total knee arthroplasty. Can J Surg. (2021) 64(3):E273–e9. doi: 10.1503/cjs.002720
13. Luan Y, Zhang M, Ran T, Wang H, Fang C, Nie M, et al. Correlation between component alignment and short-term clinical outcomes after total knee arthroplasty. Front Surg. (2022) 9:991476. doi: 10.3389/fsurg.2022.991476
14. Mullaji A, Kanna R, Marawar S, Kohli A, Sharma A. Comparison of limb and component alignment using computer-assisted navigation versus image intensifier-guided conventional total knee arthroplasty: a prospective, randomized, single-surgeon study of 467 knees. J Arthroplasty. (2007) 22(7):953–9. doi: 10.1016/j.arth.2007.04.030
15. Petursson G, Fenstad AM, Gøthesen Ø, Dyrhovden GS, Hallan G, Röhrl SM, et al. Computer-assisted compared with conventional total knee replacement: a multicenter parallel-group randomized controlled trial. J Bone Joint Surg Am. (2018) 100(15):1265–74. doi: 10.2106/jbjs.17.01338
16. Yasunaga H, Tsuchiya K, Matsuyama Y, Ohe K. Analysis of factors affecting operating time, postoperative complications, and length of stay for total knee arthroplasty: nationwide web-based survey. J Orthop Sci. (2009) 14(1):10–6. doi: 10.1007/s00776-008-1294-7
17. Novak EJ, Silverstein MD, Bozic KJ. The cost-effectiveness of computer-assisted navigation in total knee arthroplasty. J Bone Joint Surg Am. (2007) 89(11):2389–97. doi: 10.2106/jbjs.F.01109
18. Li JT, Gao X, Li X. Comparison of iassist navigation system with conventional techniques in total knee arthroplasty: a systematic review and meta-analysis of radiographic and clinical outcomes. Orthop Surg. (2019) 11(6):985–93. doi: 10.1111/os.12550
19. Sun H, Li S, Wang K, Wu G, Zhou J, Sun X. Efficacy of portable accelerometer-based navigation devices versus conventional guides in total knee arthroplasty: a meta-analysis. J Knee Surg. (2020) 33(7):691–703. doi: 10.1055/s-0039-1685145
20. Gao J, Hou Y, Li R, Ke Y, Li Z, Lin J. The accelerometer-based navigation system demonstrated superior radiological outcomes in restoring mechanical alignment and component sagittal positioning in total knee arthroplasty. BMC Musculoskelet Disord. (2021) 22(1):351. doi: 10.1186/s12891-021-04213-9
21. Gao X, Sun Y, Chen Z-H, Dou T-X, Liang Q-W, Li X. Comparison of the accelerometer-based navigation system with conventional instruments for total knee arthroplasty: a propensity score-matched analysis. J Orthop Surg Res. (2019) 14:223. doi: 10.1186/s13018-019-1258-y
22. Gharaibeh MA, Solayar GN, Harris IA, Chen DB, MacDessi SJ. Accelerometer-based, portable navigation (kneealign) vs conventional instrumentation for total knee arthroplasty: a prospective randomized comparative trial. J Arthroplasty. (2017) 32(3):777–82. doi: 10.1016/j.arth.2016.08.025
23. Goh GS-H, Liow MHL, Lim WS-R, Tay DK-J, Yeo SJ, Tan MH. Accelerometer-based navigation is as accurate as optical computer navigation in restoring the joint line and mechanical axis after total knee arthroplasty a prospective matched study. J Arthroplasty. (2016) 31(1):92–7. doi: 10.1016/j.arth.2015.06.048
24. Ikawa T, Takemura S, Kim M, Takaoka K, Minoda Y, Kadoya Y. Usefulness of an accelerometer-based portable navigation system in total knee arthroplasty. Bone Joint J. (2017) 99B(8):1047–52. doi: 10.1302/0301620X.99B8.BJJ20160596.R3
25. Jagadeesh N, Kumar H, Sarparaju V, Shivalingappa V. Comparative analysis of radiological evaluation and early functional outcomes of total knee arthroplasty using an accelerometer-based handheld navigation system and conventional instrumentation: a prospective study. Cureus. (2022) 14(1):e21039-e. doi: 10.7759/cureus.21039
26. Lai HYC, Tang YHB, Wong HL. Comparison of early results of total knee replacement performed with zimmer iassist versus conventional technique. J Orthop Trauma Rehabil. (2020) 27(2):208–13. doi: 10.1177/2210491720941208
27. Laoruengthana A, Rattanaprichavej P, Tantimethanon T, Eiamjumras W, Teekaweerakit P, Pongpirul K. Usefulness of an accelerometer-based navigation system in bilateral one-stage total knee arthroplasty. BMC Musculoskelet Disord. (2021) 22(1):164. doi: 10.1186/s12891-021-04027-9
28. Liow MHL, Goh GS-H, Pang H-N, Tay DKJ, Lo NN, Yeo SJ. Computer-assisted stereotaxic navigation improves the accuracy of mechanical alignment and component positioning in total knee arthroplasty. Arch Orthop Trauma Surg. (2016) 136(8):1173–80. doi: 10.1007/s00402-016-2483-z
29. Matsumoto K, Ogawa H, Fukuta M, Mori N, Akiyama H. Comparative study for alignment of extramedullary guides versus portable, accelerometer-based navigation in total knee arthroplasty. J Knee Surg. (2018) 31(1):92–8. doi: 10.1055/s-0037-1602133
30. Minoda Y, Hayakawa K, Hagio K, Konishi N, Tamaki T, Iwakiri K. Usefulness of an accelerometer-based portable navigation system for total knee arthroplasty: a multicenter prospective randomized controlled trial. J Bone Joint Surg Am. (2020) 102(22):1993–2000. doi: 10.2106/jbjs.20.00387
31. Nam D, Cody EA, Nguyen JT, Figgie MP, Mayman DJ. Extramedullary guides versus portable, accelerometer-based navigation for tibial alignment in total knee arthroplasty: a randomized, controlled trial: winner of the 2013 hap paul award. J Arthroplasty. (2014) 29(2):288–94. doi: 10.1016/j.arth.2013.06.006
32. Nam D, Weeks KD, Reinhardt KR, Nawabi DH, Cross MB, Mayman DJ. Accelerometer-based, portable navigation vs image less, large-console computer-assisted navigation in total knee arthroplasty a comparison of radiographic results. J Arthroplasty. (2013) 28(2):255–61. doi: 10.1016/j.arth.2012.04.023
33. Swamy AM, Malhotra R, Digge V, Manhas V, Gautam D, Srivastava DN. Accelerometer-based portable navigation, a faster guide compared to computer-assisted navigation in bilateral total knee arthroplasty-a randomized controlled study. Knee Surg Sports Traumatol Arthrosc. (2022). doi: 10.1007/s00167-021-06842-y
34. Thiengwittayaporn S, Fusakul Y, Kangkano N, Jarupongprapa C, Charoenphandhu N. Hand-held navigation may improve accuracy in minimally invasive total knee arthroplasty: a prospective randomized controlled trial. Int Orthop. (2016) 40(1):51–7. doi: 10.1007/s00264-015-2848-x
35. Tsubosaka M, Kamenaga T, Kuroda Y, Takayama K, Hashimoto S, Ishida K, et al. Accelerometer-based portable navigation system is useful for tibial bone cutting in modified kinematically aligned total knee arthroplasty. J Knee Surg. (2021) 34(8):870–6. doi: 10.1055/s-0039-3402481
36. Tsuda K, Shibuya T, Okamoto N, Shiigi E, Shirakawa N, Hosaka K, et al. Can accuracy with the iassist navigation be confirmed by assessment? A multi-center prospective randomized controlled trial with independent three-dimensional image assessment. Knee. (2021) 30:344–52. doi: 10.1016/j.knee.2021.04.019
37. Ueyama H, Matsui Y, Minoda Y, Matsuura M, Nakamura H. Using accelerometer-based portable navigation to perform accurate total knee arthroplasty bone resection in Asian patients. Orthopedics. (2017) 40(3):e465–e72. doi: 10.3928/01477447-20170223-01
38. Ueyama H, Minoda Y, Sugama R, Ohta Y, Yamamura K, Nakamura S, et al. An accelerometer-based portable navigation system improved prosthetic alignment after total knee arthroplasty in 3d measurements. Knee Surg Sports Traumatol Arthrosc. (2019) 27(5):1580–6. doi: 10.1007/s00167-018-5082-4
39. Wang XG, Geng X, Li Y, Wu TC, Li ZJ, Tian H. Comparison of alignment and operative time between portable accelerometer-based navigation device and computer assisted surgery in total knee arthroplasty. Beijing Da Xue Xue Bao Yi Xue Ban. (2021) 53(4):728–33. doi: 10.19723/j.issn.1671-167X.2021.04.018
40. Wang XG, He YZ, Wu TC, Li Y, Li ZJ, Tian H. Comparison of alignment and position of prosthesis between portable accelerometer-based navigation device and conventional instrumentation in total knee arthroplasty with Valgus deformity. Zhonghua Yi Xue Za Zhi. (2022) 102(1):56–61. doi: 10.3760/cma.j.cn112137-20210909-02058
41. Xu X, Liu P, Yuan Z, Wang D, Lu Q, Zhang Z, et al. Comparison of a novel handheld accelerometer-based navigation system and conventional instrument for performing distal femoral resection in total knee arthroplasty: a randomized controlled trial. Ann Transl Med. (2019) 7(22):659. doi: 10.21037/atm.2019.10.55
42. Zhu M, Lindsay E, Keenan A, Monk P, Munro J. The use of accelerometer-based navigation for coronal tka alignment: a prospective, single surgeon comparative study. Arch Orthop Trauma Surg. (2020) 140(9):1169–74. doi: 10.1007/s00402-019-03295-4
43. Thippanna RK, Kumar MN. Lateralization of femoral entry point to improve the coronal alignment during total knee arthroplasty in patients with bowed femur. J Arthroplasty. (2016) 31(9):1943–8. doi: 10.1016/j.arth.2016.02.057
44. Ke S, Ran T, He Y, Lv M, Song X, Zhou Y, et al. Does patient-specific instrumentation increase the risk of notching in the anterior femoral Cortex in total knee arthroplasty? A comparative prospective trial. Int Orthop. (2020) 44(12):2603–11. doi: 10.1007/s00264-020-04779-4
45. Orland MD, Lee RY, Naami EE, Patetta MJ, Hussain AK, Gonzalez MH. Surgical duration implicated in Major postoperative complications in total hip and total knee arthroplasty: a retrospective cohort study. J Am Acad Orthop Surg Glob Res Rev. (2020) 4(11):e20.00043. doi: 10.5435/JAAOSGlobal-D-20-00043
46. Christen B, Tanner L, Ettinger M, Bonnin MP, Koch PP, Calliess T. Comparative cost analysis of four different computer-assisted technologies to implant a total knee arthroplasty over conventional instrumentation. J Pers Med. (2022) 12(2). doi: 10.3390/jpm12020184
47. Bonutti P, Dethmers D, Stiehl JB. Case report: femoral shaft fracture resulting from femoral tracker placement in navigated tka. Clin Orthop Relat Res. (2008) 466(6):1499–502. doi: 10.1007/s11999-008-0150-6
48. Jung KA, Lee SC, Ahn NK, Song MB, Nam CH, Shon OJ. Delayed femoral fracture through a tracker pin site after navigated total knee arthroplasty. J Arthroplasty. (2011) 26(3):505.e9–505.e11. doi: 10.1016/j.arth.2010.01.006
49. Millar NL, Deakin AH, Millar LL, Kinnimonth AW, Picard F. Blood loss following total knee replacement in the morbidly obese: effects of computer navigation. Knee. (2011) 18(2):108–12. doi: 10.1016/j.knee.2010.03.002
50. Nicoll D, Rowley DI. Internal rotational error of the tibial component is a major cause of pain after total knee replacement. J Bone Joint Surg Br. (2010) 92(9):1238–44. doi: 10.1302/0301-620x.92b9.23516
51. Panni AS, Ascione F, Rossini M, Braile A, Corona K, Vasso M, et al. Tibial internal rotation negatively affects clinical outcomes in total knee arthroplasty: a systematic review. Knee Surg Sports Traumatol Arthrosc. (2018) 26(6):1636–44. doi: 10.1007/s00167-017-4823-0
52. Tian G, Wang L, Liu L, Zhang Y, Zuo L, Li J. Kinematic alignment versus mechanical alignment in total knee arthroplasty: an up-to-date meta-analysis. J Orthop Surg. (2022) 30(3):10225536221125952. doi: 10.1177/10225536221125952
53. Liu B, Feng C, Tu C. Kinematic alignment versus mechanical alignment in primary total knee arthroplasty: an updated meta-analysis of randomized controlled trials. J Orthop Surg Res. (2022) 17(1):201. doi: 10.1186/s13018-022-03097-2
Keywords: accelerometer-based navigation, component alignment, clinical outcome, surgical duration, meta-analysis, total knee arthroplasty
Citation: Luan Y, Wang H, Zhang M, Li J, Zhang N, Liu B, Su J, Fang C and Cheng C (2023) Comparison of navigation systems for total knee arthroplasty: A systematic review and meta-analysis. Front. Surg. 10:1112147. doi: 10.3389/fsurg.2023.1112147
Received: 2 December 2022; Accepted: 3 January 2023;
Published: 17 January 2023.
Edited by:
Hongyi Zhu, Shanghai Jiao Tong University, ChinaReviewed by:
Bernardo Innocenti, Université libre de Bruxelles, BelgiumLiang Wen, Capital Medical University, China
© 2023 Luan, Wang, Zhang, Li, Zhang, Liu, Su, Fang and Cheng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chaohua Fang ZmFuZ2NoYW9odWFAMTI2LmNvbQ== Cheng-Kung Cheng Y2tjaGVuZzIwMjBAc2p0dS5lZG4uY24=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Yichao Luan
Yichao Luan Huizhi Wang
Huizhi Wang Min Zhang
Min Zhang Junwei Li1
Junwei Li1 Ningze Zhang
Ningze Zhang Chaohua Fang
Chaohua Fang Cheng-Kung Cheng
Cheng-Kung Cheng