- 1Department of Vascular Surgery, First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, China
- 2Department of General Surgery, Children’s Hospital of Xi’an Jiaotong University, Xi’an, China
- 3Department of General Surgery, Yulin Traditional Chinese Medicine Hospital, Yulin, China
A 61-year-old man developed severe swelling in the left lower extremity after interventional embolization of liver tumor. Ultrasound examination showed a pseudoaneurysm and thrombosis in the upper thigh on the left. To recognize the causes and determine the effective therapy, lower extremity arteriography was performed. The results revealed a pseudoaneurysm arised from deep femoral artery. Considering of the size of cavity and symptoms of patient, a new method was tried instead of traditional treatment using PROGLIDE device. Postoperative angiography showed a powerful blocking effect. This case study provide us a specific treatment for pseudoaneurysm, and this method provide us a new therapeutic strategy in clinical practice.
1. Introduction
Pseudoaneurysm, an encapsulated hematoma that is connected to the arterial puncture site, is the most common complication during the interventional treatment of cardiovascular disease (1). In clinical, pseudoaneurysm frequently occurs due to a low puncture site and insufficient angiopressure support after catheter removal (2). However, until now, the current therapy for pseudoaneurysms mainly focuses on traditional treatments (3). Here we describe 1 cases of deep femoral artery pseudoaneurysm after interventional embolization of liver tumor.
2. Case presentation
A 61-year-old male suffered pain and swelling in her left lower extremity after a interventional operation. He had a medical history of interventional embolization of liver tumors 1 month ago. Vascular ultrasound clearly revealed a pseudoaneurysm connecting with left deep femoral artery with a symbol of mural thrombus within the lumen. Surgery was arranged on the 5nd day. Routine preoperative examination was evaluated prior to the surgery. Angiography result revealed a 2 cm × 5 cm-sized pseudoaneurysm arising from a branch of the left deep femoral artery (Figure 1A). After the placement of 6-F sheath (Terumo, Tokyo, Japan) over pseudoaneurysm sac, then another guide wire was transported into the pseudoaneurysm sac via another 6-F sheath over right femoral artery access. The catcher is used to catch the guide wire from the contralateral sheath (Figure 1B). A PROGLIDE device (Abbott Vascular, Redwood City, CA, United States) was used to suture the rupture of the pseudoaneurysm (Figure 1C), and the second angiography showed the rupture is completely closed (Figure 1D). The vital signs and symptoms of patient were stable after the procedure. Without any other complications, she was discharged 2 days after the operation. Informed consent was obtained from the patient for the publication of this study.
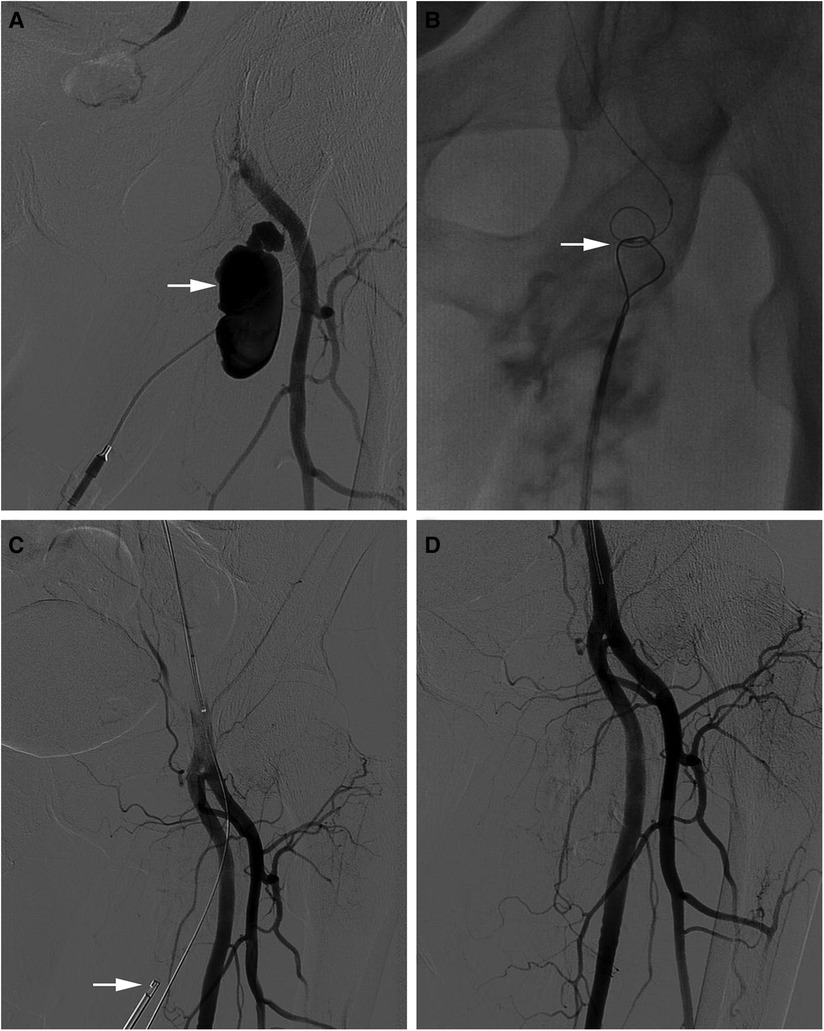
Figure 1. (A) Angiography result revealed a 2 cm × 5 cm-sized pseudoaneurysm arising from a branch of the left deep femoral artery. (B) The catcher is used to catch the guide wire from the contralateral sheath. (C) A PROGLIDE device was used to suture the rupture of the pseudoaneurysm. (D) Angiography showed the rupture is completely closed.
3. Discussion
Iatrogenic pseudoaneurysm is a vascular complication after interventional examination. In clinical practice, color doppler ultrasound was used to observe characteristic reciprocating signal of blood flow in the aneurysm cavity (4). Considering the serious consequences of the disease such as vascular rupture (5), thromboembolism (6), compression of peripheral nerve tissue (7) and skin tissue necrosis (8). so it is a crucial issue how to deal with pseudoaneurysm. In this case, we suspected that low-position puncture and insufficient compression caused a pseudoaneurysm of deep femoral artery.
We reviewed the relevant literature to find the solution of pseudoaneurysm, the method varies based on size of cavity and symptoms of patients. A cavity <2 cm in diameter that is not extending can be managed conservatively. During conservative procedure, external compression of the puncture can be the first option (9). If fails, multiple embolic materials, including polyvinyl alcohol (PVA) particles, sodium alginate microspheres amd coils, are injected into the aneurysm neck (10). Besides, surgery can be performed when some complication such as swelling, skin necrosis or compression of peripheral nerve tissue occurs (11). The puncture was sutured and the hematoma was removed in the pseudoaneurysm. In this cases, non-surgical treatments such as compression or a simple embolization could not be conducted due to severe pain and oversized pseudoaneurysm cavity. A closure device was used to suture puncture. Compared to other treatments, PROGLIDE device (12) shows an excellent blocking effect, effectively avoiding the trauma of surgical treatment, and also shortening the patient's hospital time.
Conclusion
Our study demonstrate another important function of PROGLIDE closure device, an excellent blocking effect depend on the combination of the closure device and guide wire was observed. This report describes a specific treatment of pseudoaneurysm, and this method would provide us a new therapeutic strategy in clinical practice.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LJ, LY and WJ wrote the manuscript. LS approved the manuscript. ZS and DZ made the figure. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jeon SH, Kang HG, Kim HJ, Seo MW, Shin BS. Femoral artery pseudoaneurysm after carotid artery stenting. Medicine. (2019) 98:e15309. doi: 10.1097/MD.0000000000015309
2. Gupta PN, Basheer AS, Sukumaran GG, Padmajan S, Praveen S, Velappan P, et al. Femoral artery pseudoaneurysm as a complication of angioplasty. How can it be prevented. Heart Asia. (2013) 5:144–7. doi: 10.1136/heartasia-2013-010297
3. Florescu M, Qiu F, Plumb TJ, Fillaus JA. Endovascular treatment of arteriovenous graft pseudoaneurysms, indications, complications, and outcomes: a systematic review. Hemodial int. (2014) 18:785–92. doi: 10.1111/hdi.12152
4. Cornacchiari M, Guastoni C, Borin F, Toma LD, Mereghetti M, Lullo LD, et al. Clinical, ultrasound and treatment of aneurysms and pseudoaneurysms in hemodialysis vascular access. G Ital Nefrol. (2016) 33:gin/33.2.10. PMID: 27067219
5. Regus S, Lang W. Rupture risk and etiology of visceral artery aneurysms and pseudoaneurysms: a single-center experience. Vasc Endovascular Surg. (2016) 50:10–5. doi: 10.1177/1538574415627868
6. Kruger K, Zahringer M, Sohngen FD, Gossmann A, Schulte O, Feldmann C, et al. Femoral pseudoaneurysms: management with percutaneous thrombin injections–success rates and effects on systemic coagulation. Radiology. (2003) 226:452–8. doi: 10.1148/radiol.2262012107
7. Liu JW, Zhong KJ, Lin DK. Median nerve compression caused by superficial brachial artery: an unusual clinical case. J Int Med Res. (2020) 48:300060520969043. doi: 10.1177/0300060520969043
8. Waldenberger P, Chemelli A, Hennerbichler A, Wick M, Freund MC, Jaschke W, et al. Transarterial embolization for the management of hemarthrosis of the knee. Eur J Radiol. (2012) 81:2737–40. doi: 10.1016/j.ejrad.2011.11.016
9. Kang SS, Labropoulos N, Mansour MA, Baker WH. Percutaneous ultrasound guided thrombin injection: a new method for treating postcatheterization femoral pseudoaneurysms. J Vasc Surg. (1998) 27:1032–8. doi: 10.1016/S0741-5214(98)70006-0
10. Webber GW, Jang J, Gustevson S, Olin JW. Contemporary management of postcatheterization pseudoaneurysms. Circulation. (2007) 115:2666–74. doi: 10.1161/CIRCULATIONAHA.106.681973
11. Tisi PV. Surgery versus non-surgical treatment for femoral pseudoaneurysms. Cochrane Database Syst Rev. (2009) 2:CD004981. doi: 10.1002/14651858.CD004981.pub2
Keywords: deep femoral artery, pseudoaneurysm, proGlide, angiography, guide wire
Citation: Jiaxin L, Yan L, Sheng Z, Zhiyi D, Jichang W and Shaoying L (2023) Case report: Successful and effective percutaneous closure of a deep femoral artery pseudoaneurysm using proglide device. Front. Surg. 10:1109243. doi: 10.3389/fsurg.2023.1109243
Received: 28 November 2022; Accepted: 2 March 2023;
Published: 31 March 2023.
Edited by:
Apostolos Tassiopoulos, Stony Brook University, United StatesReviewed by:
Zhenjiang Li, Zhejiang University, ChinaRosa María Moreno Carriles, Hospital Universitario Princess, Spain
© 2023 Jiaxin, Yan, Sheng, Zhiyi, Jichang and Shaoying. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wang Jichang aW50ZTEzODVAMTYzLmNvbQ== Lu Shaoying cm9iZXJ0bHVAbWFpbC54anR1LmVkdS5jbg==
Specialty Section: This article was submitted to Vascular Surgery, a section of the journal Frontiers in Surgery
 Liu Jiaxin
Liu Jiaxin Li Yan1
Li Yan1