- 1Department of Anesthesiology, The First Affiliated Hospital of University of Science and Technology of China, Hefei, Anhui, China
- 2Department of Hand and Foot Surgery, The First Affiliated Hospital of University of Science and Technology of China, Hefei, Anhui, China
Background: Tourniquet pain is the most prominent problem in ankle surgery, and there is no proper method to predict it. It was reported that pain sensitivity questionnaires could evaluate the pain sensitivity of subjects. Its potential to predict tourniquet pain in ankle surgery is constructive and meaningful.
Methods: One hundred and twenty patients undergoing ankle surgery were included in this study. The pain sensitivity questionnaire (PSQ) and self-rating anxiety scale (SAS) were completed before the operation. The methods included an ultrasound-guided popliteal sciatic, a femoral nerve block, and a proximal thigh tourniquet. The pressure of the tourniquet was set according to the systolic blood pressure (SBP + 100 mmHg). A visual analogue scale (VAS) was used to assess the tourniquet pain. Also, the onset time of tourniquet pain ≥4 VAS units was recorded.
Results: The PSQ-total and PSQ-minor scores were significantly correlated with the onset time when the tourniquet pain ≥4 VAS units (r = −0.763, r = −0.731, P < 0.001). The PSQ-total score <6.5 group gave significantly lower ratings for items 3, 4, 14, and 16 in the PSQ survey compared to the PSQ-total score ≥6.5 group (P < 0.05). Patients with high pain sensitivity have a higher need for analgesic drugs (P < 0.001). PSQ-total score ≥6.5 (OR = 185.8, 95% CI = 39.8–1,437.6, P < 0.001), sex (male, OR = 0.11, 95% CI = 0.018–0.488, P < 0.05), and age (OR = 0.92, 95% CI = 0.842–0.995, P < 0.05) were risk factors for reporting a tourniquet pain ≥4 VAS units within 30 min.
Conclusion: The PSQ score is found to be correlated with intraoperative tourniquet pain. In addition, sex and age also affect the time of having intraoperative tourniquet pain.
Introduction
A proximal thigh tourniquet is often used in foot and ankle surgery to facilitate a bloodless field. With the extended use of a tourniquet, patients often complain of pain and discomfort at the tourniquet site or distal limb (1). However, it is difficult to relieve tourniquet pain, and the sensitivity of different patients to tourniquet pain is different. So, predicting the sensitivity to tourniquet pain might help in choosing a reasonable anesthesia scheme. Numerous studies have tried to predict acute postoperative pain by experimental pain tests or quantitative sensory tests (QSTs) before surgery (2, 3). None of these methods have been used as a routine approach for predicting pain due to the absence of an instrument and/or being time-consuming. The pain catastrophizing scale (PCS) describes different feelings and thoughts associated with pain and is used routinely in some preoperative settings for all patients (4). However, the PCS is a cognitive and emotional tendency and is not based on life events. The pain sensitivity questionnaire (PSQ) is a pain sensitivity self-assessment questionnaire based on events in daily life and designed by Ruscheweyh et al. (5). Furthermore, the PSQ is validated in Chinese populations and can typically be completed in less than 15 min, without the need for any special equipment or staff. Moreover, the questionnaire does not have any ethical concerns. Prior studies have shown that the PSQ can evaluate the pain sensitivity of subjects, predict postoperative acute pain, and screen individuals at high risk of postoperative chronic pain (6). However, whether the PSQ can predict the sensitivity of patients to tourniquet pain has not been reported as yet.
This study aims to evaluate the feasibility of the PSQ in predicting tourniquet pain in ankle surgery. Preoperative PSQ evaluation is helpful for guiding the formulation of an anesthesia plan, intervening in advance for predictable pain, and implementing individualized anesthesia management.
Materials and methods
Participants
The trial was registered at www.Chictr.org.cn on 9 July 2021 prior to patient recruitment (code: ChiCTR2100048525). The clinical trial was approved by the Medical Research Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China (ethics: 2020KY). The study was conducted between July 2021 and February 2022. Written informed consent was obtained from all participants. Patients aged ≥18 years with ASA (American Society of Anesthesiologists physical status classification) I and II and scheduled for ankle and calcaneal fracture surgery were recruited. Exclusion criteria were as follows: inability to consent to the study, multiple sclerosis, sensory loss, or other diseases affecting sensory function such as diabetes, receiving major opioids for chronic pain therapy or substance abuse, narcotic-intolerant, hepatic or renal failure, allergy to local anesthetics, pregnancy, and prior surgery in the popliteal fossa.
Preoperative assessment
The day before surgery, all patients were asked to complete the Chinese version of the PSQ (5, 7) and SAS (8) independently or with the assistance of researchers. The validity of the Chinese version of the two inventories has been confirmed (7). According to previous studies, the enrolled patients were assigned to either a low (PSQ score <6.5) or a high PSQ group (PSQ score ≥6.5) (9). The PSQ has 17 questions about life situations associated with pain, of which three are normally considered not painful by healthy subjects and are therefore excluded from the final score. The PSQ-total score was the average rating of items 1, 2, 3, 4, 6, 7, 8, 10, 11, 12, 14, 15, 16, and 17 (all but the three non-painful items), and the PSQ-minor score was the average rating of items 3, 6, 7, 10, 11, 12, and 14. The PSQ assesses individual pain sensitivity by imagining the pain degree of some scenes in life and performing VAS pain scores. The SAS is divided into 20 items (1–4/item), and a total score of 40–49 indicates mild anxiety, 50–59 moderate anxiety, ≥59 severe anxiety, and ≥40 anxiety patients.
Anesthesia and data collection
After entering the operating room, participants had intravenous cannulas (20-G) inserted into the peripheral vein of the upper limb, and 500 ml sodium acetate Ringer solution was intravenously injected within 30–40 min. The standardized monitoring methods of electrocardiogram (ECG), oxygen saturation (SPO2), and noninvasive blood pressure were established. All patients received intravenous dexmedetomidine sulphate 0.5 μg/kg within 15 min. All patients were placed in a lateral decubitus position, with the operated limb on the upper side and the hip and knee slightly bent. The block of the sciatic nerve in the popliteal fossa was performed under sterile conditions by ultrasound guidance (sonosite edge, USA). A total of 25 ml of a mixed solution of 0.25% ropivacaine and 1% lidocaine was injected around the sciatic nerve and adequate spread of the drugs around the nerves was monitored. Then, in the supine position, 10 ml of the same solution was injected for the femoral nerve block. In addition, adequate spread of the drug around the nerves was monitored. All blocks were performed by the same anesthesiologist. The level of sensory block was assessed using the ice test in 0–2 scale every 5 min. Sensory block rating: 0 = complete loss of sensation; 1 = hypoesthesia; 2 = feeling normal. Successful surgical block was defined as a grade 0 sensory block within 30 min (10). If the sensory block level was greater than 0 at 30 min, or the patient complained of pain at the time of skin incision, the patient was excluded from the study. When a complete sensory block was achieved, a 9 cm × 60 cm wide pneumatic thigh tourniquet (Changzhou Yanling Electronic Equipment Co., Ltd., model: ats-I) was applied to the proximal part of the thigh. The pressure was set at 100 mmHg more than SBP and the duration was 90 min. When the duration of tourniquet inflation was longer than 2 h, deflation of the tourniquet was performed for 10–15 min to allow tissue reperfusion (11). The tourniquet pain intensity was assessed by a blinded observer immediately after tourniquet inflation (time 0), every 5 min up to 20 min, and then every 15 min until the end of surgery with a 10-point visual analogue scale (VAS) (0 = no pain, and 10 = unbearable pain). Mostly, VAS ≤ 4 units was taken as mild pain and a widely acceptable pain threshold for patients (12, 13). If the patient complained of thigh pain and VAS ≥ 4 units, 5 µg of sufentanil was given intravenously. Additional 5 µg of sufentanil was given in the case of insufficient pain relief 5 min later. If thigh pain was still unbearable, general anesthesia was established. The main outcome is the onset time of tourniquet pain ≥4 VAS units. Persistent low limb numbness/paresthesia or motor deficit were also recorded within 48 h after the surgery.
Sample size and statistical analysis
The sample size was based on a pilot experiment of 20 cases in our observation. Also, the correlation coefficient between PSQ-total and the onset time of reporting a tourniquet pain score ≥4 VAS units was approximately −0.35. Using a power of 90% and a two-sided alpha error of 0.05, 83 participants were needed. Considering a 10% dropout rate, 90 participants were needed.
SPSS 26 was used for statistical analysis. Normally distributed continuous variables were expressed as the mean ± SD and compared between groups using a two-sample Student's t test. If the distribution was not normal, the median with interquartile range (IQR) was expressed, and a χ2 test was used. Pearson correlation analysis was used for data conforming. Logistic regression analysis was used to predict the risk factors for reporting tourniquet pain ≥4 VAS units within 30 min. All P-values < 0.05 were considered to be statistically significant.
Results
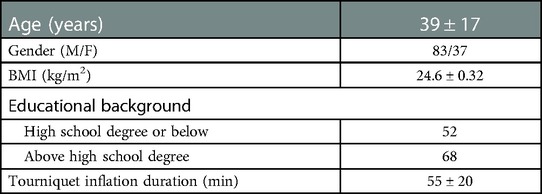
A total of 123 patients undergoing ankle and heel fracture surgery were enrolled in the study. Three patients who complained of pain at the moment of skin incision were excluded. Finally, the remaining 120 patients completed the protocol. The demographic characteristics of patients are listed in Table 1.
The PSQ-total score of all patients was 5.58 ± 1.44, ranging from 1.9 to 9.1. The number of patients with PSQ-total <6.5 was 80, and the number of other patients was 40. The PSQ-minor score of all patients was 2.42 ± 0.85, ranging from 0.8 to 4.6. The onset time of tourniquet pain ≥4 VAS units was 38 ± 17.3 min. Thirty-nine patients reported tourniquet pain ≥4 VAS units within 30 min, and others reported tourniquet pain 30 min later.
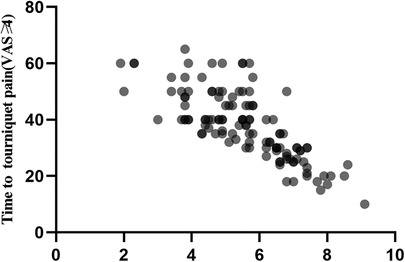
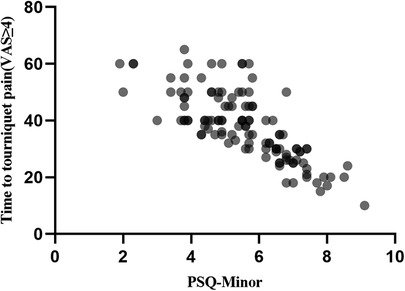
The PSQ-total and PSQ-minor scores were found to be significantly correlated with the onset time of tourniquet pain score ≥4 VAS (r = −0.763, r = −0.731, P < 0.001; Figures 1,2).
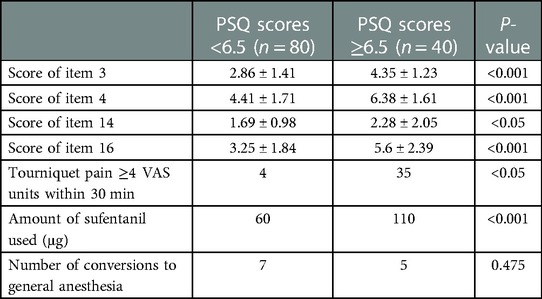
The PSQ-total score <6.5 group gave significantly lower ratings for items 3, 4, 14, and 16 in the PSQ survey compared to the group with a PSQ-total score ≥6.5 (P < 0.05). The ratio of tourniquet pain VAS ≥ 4 units at 30 min and the total amount of additional remedial sufentanil were significantly greater in the PSQ-total score ≥6.5 group compared with the PSQ-total score <6.5 group (P < 0.05). The number of patients who required general anesthesia was not significantly different between the two groups (Table 2).
The results of the logistic regression analysis are presented in Table 3. PSQ-total score ≥6.5, sex, and age were risk factors for reporting a tourniquet pain ≥4 VAS units within 30 min (P < 0.05). The SAS score of all patients was 23 ± 3. Also, no patient was anxious before the surgery.
None of the subjects enrolled in the study had complications or side effects associated with the nerve block or tourniquet-related pain within 48 h after surgery.
Discussion
This study investigated the correlation between the PSQ and tourniquet pain to evaluate whether it could identify patients susceptible to tourniquet pain and provide a basis for improved clinical management through treatment strategies in each patient.
We enrolled patients with ankle or heel fractures; thus, the femoral nerve and the sciatic nerve block could meet the analgesia requirement of the procedure. The effectiveness of different approaches to sciatic nerve block in preventing tourniquet pain is controversial. Spasiano et al. reported that the combination of proximal sciatic nerve block with femoral nerve and lateral femoral cutaneous nerve block might greatly suppress thigh pain after tourniquet inflation (14). In contrast, Fuzzier et al. found that the proximal approach of the sciatic nerve block provides no better thigh tourniquet pain relief than the popliteal approach during foot surgery (15). Furthermore, the popliteal fossa approach was easy to carry out, resulting in less discomfort postoperatively than the posterior approach because the nerve is more superficial and does not affect the movement of the thigh. Thus, the popliteal fossa approach of the femoral nerve and sciatic nerve block was established in this study.
We found that both PSQ-total and PSQ-minor scores are negatively correlated with the onset time of tourniquet pain ≥4 VAS units, which means that the PSQ score and its subgroup could predict the tourniquet pain to some extent. In healthy subjects, experimental pain intensity rating scores were more strongly correlated with the PSQ-minor subscore than with the PSQ-total score. Nevertheless, the authors mostly recommend that both the PSQ-total score and the PSQ-minor subscore should be collected (5, 6). Bearing this in mind, we used both PSQ-total and PSQ-minor in our study and observed similar trends in their correlation with the onset time of tourniquet pain ≥4 VAS units. Previous studies also demonstrated the similar strength of these two scores in patients with chronic pain (4, 16). Another finding is that patients with PSQ-total score ≥6.5 were more likely to report tourniquet pain earlier in the procedure and needed more rescue analgesics. These results indicated that patients with high PSQ are more sensitive to tourniquet pain. Tourniquet pain is described as a dull, tight, aching sensation at the site of tourniquet application. So, we analyzed several items (3, 4, 14, 16) of PSQ that were similar to the pain type of tourniquet and found that items 3, 4, 14, 16 scores were significantly lower in the PSQ-total score <6.5 group than those in the PSQ-total score ≥6.5 group. Furthermore, Duchow et al. also found that patients with high PSQ scores were more prone to central sensitization and more sensitive to acute and chronic pain (17). Accordingly, spinal or general anesthesia should be considered in patients with high PSQ scores instead of peripheral nerve blocks alone. The validity of PSQ in predicting pain sensitivity and intensity of postoperative pain has been confirmed in several studies. Bjornnes et al. reported a positive correlation between the PSQ score and acute postoperative pain intensity in patients undergoing abdominal, pulmonary, thyroid, and cardiac surgeries (17, 18). Moreover, the PSQ score affects improvements in pain and disability after spine surgery (9). Patients with higher PSQ have less improvement in postoperative back pain, leg pain, and disability. However, our findings showed that seven patients in the PSQ-total score <6.5 group required general anesthesia during the surgery, suggesting that tolerance of tourniquet pain is not only correlated with the PSQ score alone but also with other factors.
Another finding of our study is that female gender and age, besides PSQ, were all risk factors for the occurrence of tourniquet pain ≥4 VAS units within 30 min. Our results indicated that women might report tourniquet pain earlier than men after the tourniquet is inflated. Population-based pain research has shown that women are more likely than men to report a variable range of temporary and persistent pains and to report more severe pain, more frequent pain, and pain of longer duration than men (19–21), which is consistent with our study. In addition, older patients may report tourniquet pain later compared to younger patients. Also, previous studies had found lower subjective pain scores when older patients received painful stimuli, presumably related to reduced sensory nerve function in the elderly (22).
In this study, we tried to detect whether anxiety was a risk factor for pain sensitivity. Unexpectedly, we found that the SAS scores of all patients were less than 40, which means no patient was anxious before the surgery. Perhaps this was because all the subjects thought the procedure would be safe and were full of confidence about the curative effect.
There are some limitations in the present study. We did not measure the thigh circumference and local fat thickness of the tourniquet, which may affect the patient's susceptibility to tourniquet pain.
Conclusion
In conclusion, PSQ scores are found to be associated with intraoperative tourniquet pain. In addition, patients with high PSQ scores, women, and younger patients may have an earlier onset of tourniquet pain. Moreover, preoperative PSQ assessment can help guide the development of anesthetic protocols, earlier intervention for predictable pain, and the implementation of individualized anesthetic management.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Involve patient privacy. Requests to access these datasets should be directed to 709765934@qq.com.
Ethics statement
The studies involving human participants were reviewed and approved by the Medical Research Ethics Committee of the First Affiliated Hospital of the University of Science and Technology of China. The patients/participants provided their written informed consent to participate in this study.
Author contributions
QF, FK, MH, MY, LH, LL, XH and JL: participate in the planning, data transmission, report, concept, design and acquisition analysis and interpretation of data. QF and FK: participated planning, concept, design, data analysis and interpretation. All authors of the data contributed to the article and approved submitted version.
Funding
This study was funded by the Natural Science Foundation of Anhui Province (grant no. 2108085MH323) and Wujieping Medical Foundation (grant no. 320.6750.2021-03-2).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kamath K, Kamath SU, Tejaswi P. Incidence and factors influencing tourniquet pain. Chin J Traumatol. (2021) 24(5):291–4. doi: 10.1016/j.cjtee.2021.05.002
2. Gamez BH, Habib AS. Predicting severity of acute pain after cesarean delivery: a narrative review. Anesth Analg. (2018) 126(5):1606–14. doi: 10.1213/ANE.0000000000002658
3. Pan PH, Tonidandel AM, Aschenbrenner CA, Houle TT, Harris LC, Eisenach JC. Predicting acute pain after cesarean delivery using three simple questions. Anesthesiology. (2013) 118(5):1170–9. doi: 10.1097/ALN.0b013e31828e156f
4. Tuna T, Van Obbergh L, Van Cutsem N, Engelman E. Usefulness of the pain sensitivity questionnaire to discriminate the pain behaviour of chronic pain patients. Br J Anaesth. (2018) 121(3):616–22. doi: 10.1016/j.bja.2018.04.042
5. Ruscheweyh R, Marziniak M, Stumpenhorst F, Reinholz J, Knecht S. Pain sensitivity can be assessed by self-rating: development and validation of the pain sensitivity questionnaire. Pain. (2009) 146(1–2):65–74. doi: 10.1016/j.pain.2009.06.020
6. Ruscheweyh R, Verneuer B, Dany K, Marziniak M, Wolowski A, Colak-Ekici R, et al. Validation of the pain sensitivity questionnaire in chronic pain patients. Pain. (2012) 153(6):1210–8. doi: 10.1016/j.pain.2012.02.025
7. Quan X, Fong DYT, Leung AYM, Liao Q, Ruscheweyh R, Chau PH. Validation of the mandarin Chinese version of the pain sensitivity questionnaire. Pain Pract. (2018) 18(2):180–93. doi: 10.1111/papr.12587
8. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12(6):371–9. doi: 10.1016/S0033-3182(71)71479-0
9. Kim HJ, Lee JI, Kang KT, Chang BS, Lee CK, Ruscheweyh R, et al. Influence of pain sensitivity on surgical outcomes after lumbar spine surgery in patients with lumbar spinal stenosis. Spine (Phila Pa 1976). (2015) 40(3):193–200. doi: 10.1097/BRS.0000000000000699
10. Jeong , Shim . Minimum effective anaesthetic volume of 0.5% ropivacaine for ultrasound-guided popliteal sciatic nerve block in patients undergoing foot and ankle surgery: determination of ED50 and ED95. Anaesth Intensive Care. (2015) 43(1):92–7. doi: 10.1177/0310057X1504300114
11. Guideline Quick View: Pneumatic Tourniquet. AORN J. Pneumatic Tourniquet. (2019) 109(2):266–9. doi: 10.1002/aorn.12619
12. Bodian CA, Freedman G, Hossain S, Eisenkraft JB, Beilin Y. The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology. (2001) 95(6):1356–61. doi: 10.1097/00000542-200112000-00013
13. Charier D, Vogler MC, Zantour D, Pichot V, Martins-Baltar A, Courbon M, et al. Assessing pain in the postoperative period: analgesia nociception Index(TM) versus pupillometry. Br J Anaesth. (2019) 123(2):e322–7. doi: 10.1016/j.bja.2018.09.031
14. Spasiano A, Flore I, Pesamosca A, Della Rocca G. Comparison between spinal anaesthesia and sciatic-femoral block for arthroscopic knee surgery. Minerva Anestesiol. (2007) 73(1-2):13–21. accession number: 1715976417159764
15. Fuzier R, Hoffreumont P, Bringuier-Branchereau S, Capdevila X, Singelyn F. Does the sciatic nerve approach influence thigh tourniquet tolerance during below-knee surgery? Anesth Analg. (2005) 100(5):1511–4. doi: 10.1213/01.ANE.0000148119.99913.30
16. Kim HJ, Park JH, Kim JW, Kang KT, Chang BS, Lee CK, et al. Prediction of postoperative pain intensity after lumbar spinal surgery using pain sensitivity and preoperative back pain severity. Pain Med. (2014) 15(12):2037–45. doi: 10.1111/pme.12578
17. Duchow J, Schloricke E, Huppe M. Self-rated pain sensitivity and postoperative pain. Schmerz. (2013) 27(4):371–9. doi: 10.1007/s00482-013-1338-6
18. Bjornnes AK, Lie I, Parry M, Falk R, Leegaard M, Rustoen T, et al. Association between self-perceived pain sensitivity and pain intensity after cardiac surgery. J Pain Res. (2018) 11:1425–32. doi: 10.2147/JPR.S167524
19. Racine M, Tousignant-Laflamme Y, Kloda LA, Dion D, Dupuis G, Choiniere M. A systematic literature review of 10 years of research on sex/gender and pain perception – part 2: do biopsychosocial factors alter pain sensitivity differently in women and men? Pain. (2012) 153(3):619–35. doi: 10.1016/j.pain.2011.11.026
20. Maixner W, Humphrey C. Gender differences in pain and cardiovascular responses to forearm ischemia. Clin J Pain. (1993) 9(1):16–25. doi: 10.1097/00002508-199303000-00003
21. Riley JL 3rd, Robinson ME, Wise EA, Myers CD, Fillingim RB. Sex differences in the perception of noxious experimental stimuli: a meta-analysis. Pain. (1998) 74(2–3):181–7. doi: 10.1016/S0304-3959(97)00199-1
Keywords: pain sensitivity questionnaire, tourniquet, ankle surgery, nerve block, pain
Citation: Fu Q, Han M, Mu Y, Hao L, Lu L, Huang X, Li J and Kang F (2023) Does the pain sensitivity questionnaire correlate with tourniquet pain in patients undergoing ankle surgery? Front. Surg. 10:1102319. doi: 10.3389/fsurg.2023.1102319
Received: 18 November 2022; Accepted: 6 February 2023;
Published: 27 February 2023.
Edited by:
Huiyin Tu, University of Nebraska Medical Center, United StatesReviewed by:
Yossef Hassan AbdelQadir, Alexandria University, EgyptMengchen Yin, Shanghai University of Traditional Chinese Medicine, China
© 2023 Fu, Han, Mu, Hao, Lu, Huang, Li and Kang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Fang Kang a2FuZ2ZhbmcxOTk3NzFAMTYzLmNvbQ==
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Qiuyue Fu
Qiuyue Fu Mingming Han
Mingming Han Yuyang Mu
Yuyang Mu Lina Hao1
Lina Hao1