- 1Second Clinical Medical College, Binzhou Medical University, Yantai, China
- 2Department of Urology, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, China
- 3Department of Anesthesiology, The Affiliated Yantai Yuhuangding Hospital of Qingdao University, Yantai, China
- 4Department of Urology, Beijing TianTan Hospital, Capital Medical University, Beijing, China
Objective: To determine the efficacy of peripheral nerve block (PNB) in preventing postoperative catheter-related bladder discomfort (CRBD).
Methods: Up to July 1, 2022, the PubMed, Embase and Cochrane Central Register of Controlled Trials databases were searched, and all articles that met the PICOS (Patient, Intervention, Comparator, Outcome, Study design) criteria were enrolled. The included trials were evaluated using the Cochrane Collaboration's tool. Patients in the block group received bilateral PNB, while those in the non-block group did not need any additional procedure or simply achieved “sham block”. CRBD was quantified using the visual analog scale (VAS) score, which was questioned and recorded at 0–1 h, 1–2 h, 4–8 h, 8–12 h and 12–24 h intervals. The incidences of CRBD, moderate to severe CRBD and postoperative nausea and vomiting (PONV) were meta-analysed.
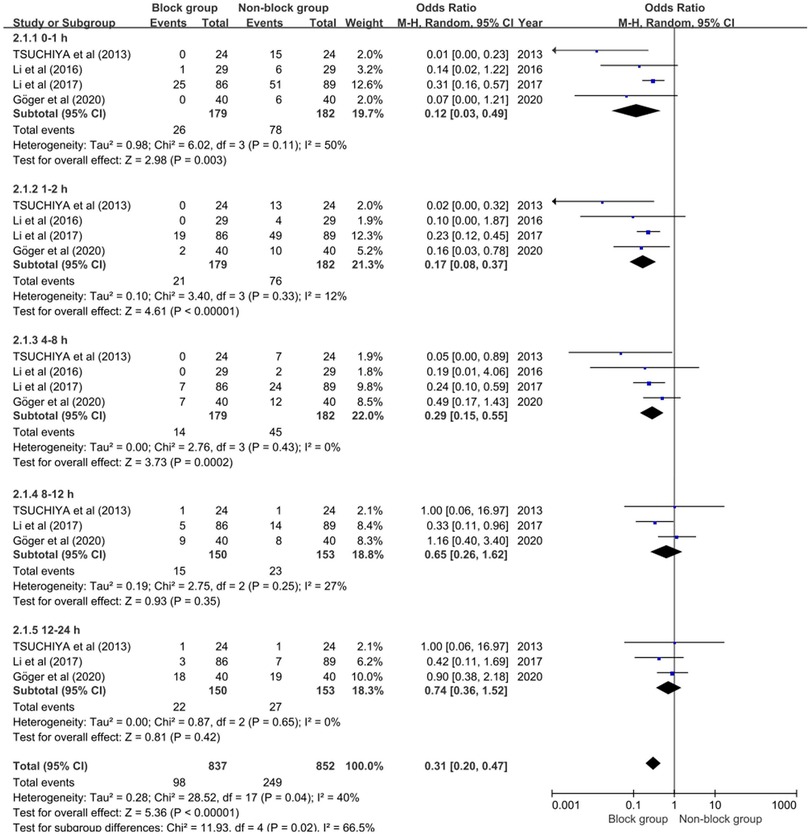
Results: Six trials with a total of 544 patients were considered. First, the block group had a lower incidence of CRBD than the non-block group at 0–1 h (OR 0.22; 95% CI, 0.18–0.08; P < 0.0001), 1–2 h (OR 0.14; 95% CI, 0.08–0.26; P < 0.00001), 4–8 h (OR 0.27; 95% CI, 0.13 to 0.58; P < 0.0008) and 8–12 h (OR 0.51; 95% CI, 0.30 to 0.87; P = 0.01). Second, the block group showed a lower incidence of moderate to severe CRBD than the non-block group at 0–1 h, 1–2 h and 4–8 h, and the ORs were 0.12 (95% CI, 0.03 to 0.49; P = 0.003), 0.17 (95% CI, 0.08 to 0.37; P < 0.00001) and 0.29 (95% CI, 0.15 to 0.55; P = 0.0002),respectively. Finally, the block group was significantly associated with a decreased incidence of PONV (OR, 0.14; 95% CI, 0.05 to 0.39; P = 0.0002).
Conclusion: This meta-analysis suggested that PNB markedly reduced the incidence and severity of early postoperative CRBD and decreased the occurrence of PONV.
1. Introduction
Various surgical procedures, particularly urology, mostly require an indwelling urethral catheter postoperatively. The importance of indwelling urethral catheters is self-evident, yet most patients frequently experience varied degrees of catheter-related bladder discomfort (CRBD), a phenomenon that appears to be more prevalent in male patients (1–3). CRBD can intensify postoperative pain and prolong the hospital stay of patients, impeding the progress of enhanced recovery after surgery (ERAS), and there are even reports in the literature that CRBD can increase the incidence of postoperative complications, including surgical incision dehiscence and hemorrhage (4, 5).
Not surprisingly, the incidence of CRBD can be as high as 90% in patients after transurethral resection of bladder tumors (6). The clinical manifestation of CRBD is a burning sensation that spreads from the suprapubic region to the penis, and some patients even develop an urge to pull out the urinary catheter. Moreover, some patients also present with symptoms similar to overactive bladder (OAB) (7, 8). Given that CRBD is primarily caused by involuntary contraction of bladder smooth muscle mediated by muscarinic receptors, a variety of antimuscarinic medications have developed. Furthermore, some antiepileptic agents, selective α2-adrenoceptor agonists and nonsteroidal anti-inflammatory drugs (NSAIDs) have been demonstrated to be effective (4, 5). In recent years, research on peripheral nerve block (PNB) for the prevention of CRBD has become a hotspot to decrease pharmacological side effects.
A prospective study showed that PNB can effectively relieve CRBD and minimize analgesic requirements, whereas Weinberg and his colleagues were skeptical (9, 10). Therefore, for the first time, we conducted a meta-analysis to assess the efficacy of PNB for the prevention of postoperative CRBD.
2. Methods
This systematic review and meta-analysis followed the latest Preferred Reporting Items for Systematic Reviews of Interventions (PRISMA 2020) statements and the completed PRISMA 2020 checklist is presented in the supplementary file.
2.1. Search strategy
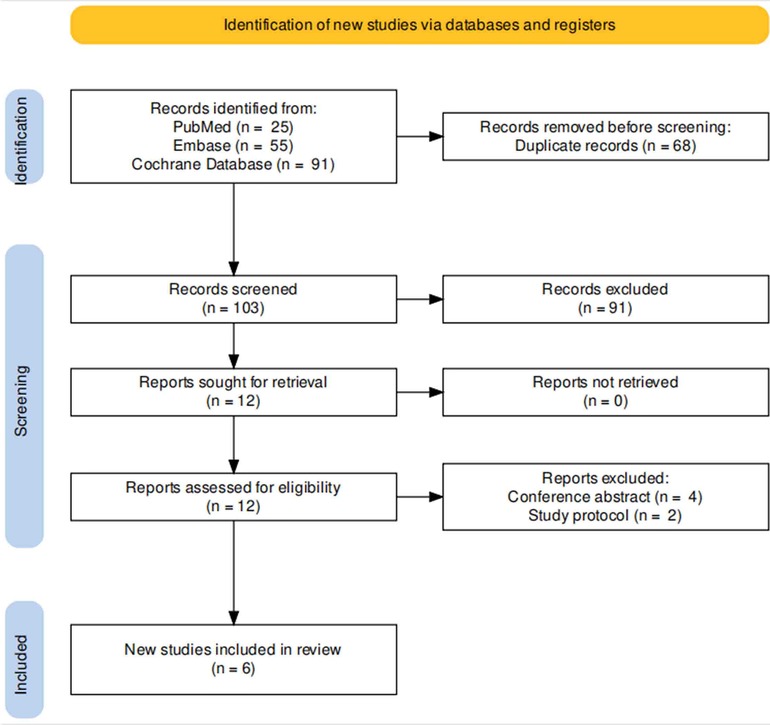
Up to July 1, 2022, search phrases (“catheter discomfort” and” block “) were retrieved from the PubMed, Embase and Cochrane Central Register of Controlled Trials databases, and all literature was systematically reviewed. Two authors utilized PICOS (Patient, Intervention, Comparator, Outcome, Study design) criteria to include relevant randomized controlled trials (RCTs). Case reports, editorials, conference abstracts, study protocols, and non-English records were not considered. In addition, we gathered articles of interest from the included articles’ reference lists. If the two reviewers disagreed, they consulted with a third author to reach a consensus. Figure 1 depicts the PRISMA flow diagram.
2.2. Inclusion criteria
The detailed PICOS criteria are presented in Table 1. Furthermore, all enrolled patients randomly performed the experimental or control interventions after surgery. After arrival at the post-anesthesia care unit (PACU), the visual analog scale (VAS) score was inquired and recorded at 0–1 h, 1–2 h, 4–8 h, 8–12 h and 12–24 h, respectively. The severity of CRBD was classified as none (VAS 0), mild (VAS 1–3), moderate (VAS 4–7) and severe (VAS 8–10). Patients were randomly allocated to one of two groups: block or non-block, with the former producing bilateral PNB via local anesthesia and the latter having no any additional procedure or simply replacing local anesthetics with saline to achieve “sham block”.

Table 1. Search strategy according to population, intervention, comparison, outcome, and study design.
2.3. Quality assessment
The Cochrane Collaboration's tool, which comprised seven aspects: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other potential bias, was used to evaluate the included RCTs (11). The above assessments were accomplished separately by two authors, and disagreements among reviewers were settled by consensus.
2.4. Data extraction
The following data were obtained from the included studies: (1) First author's name and year of publication; (2) nation of study and sample size in each RCT; (3) nerve block modalities and drugs; (4) anesthesiology and types of surgery; (5) operative duration; (6) catheter size and inflated volume; (7) the incidence of CRBD and moderate to severe CRBD; (8) the incidence of postoperative nausea and vomiting (PONV); and (9) the incidence of need for analgesic and opioid consumption 24 h after surgery.
2.5. Statistical analysis and meta-analysis
The interquartile range was converted into the mean and standard deviation (SD) using the quantile estimation (QE) methodology recently developed by McGrath and colleagues (12). Continuous variables were reported as the mean difference (MD) with 95% confidence interval (CI), whilst dichotomous variables were described using odds ratio (OR) and CI. Heterogeneity among the included studies was determined by the I-square (I2) and Q tests. A random-effect model was employed if the heterogeneity was significant (P < 0.05 and I2 ≥ 50%); otherwise, a fixed-effect model was used. A P value of less than 0.05 was judged statistically significant for the summary effect. Quality assessment and outcome analysis of the included RCTs were performed with RevMan v.5.4.0 (Cochrane Collaboration, Oxford, UK).
3. Results
3.1. Characteristics of the individual studies
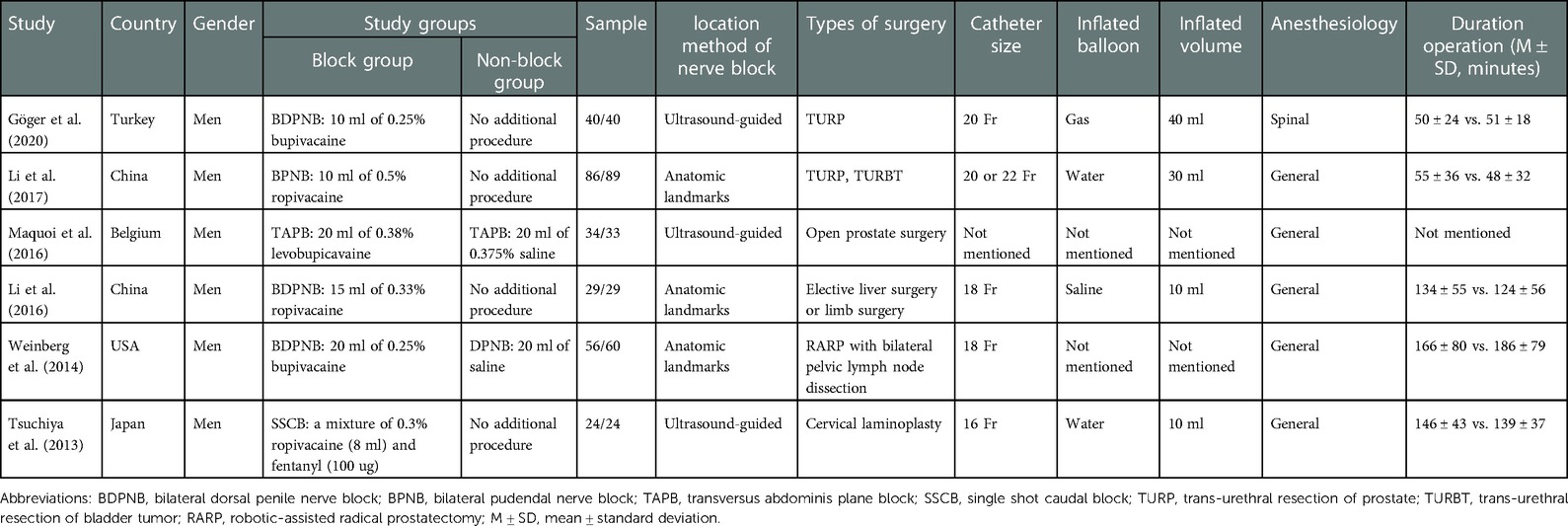
A total of 171 articles were retrieved. After screening titles and abstracts, 159 papers were rejected. After full-text access, four conference abstracts and two study protocols (13, 14) were removed, leaving six studies for inclusion in the meta-analysis. Three RCTs used dorsal penile nerve block (9, 10, 15), one caudal block (16), one pudendal nerve block (17), and one transvs. abdominis plane block (18) as nerve block methods. The patients with indwelling urinary catheters underwent various surgical interventions, the majority of which were prostatic operations, a few of which were bladder procedures, and a few of which were nonurologic surgeries. Table 2 summarizes the detailed features of the included studies.
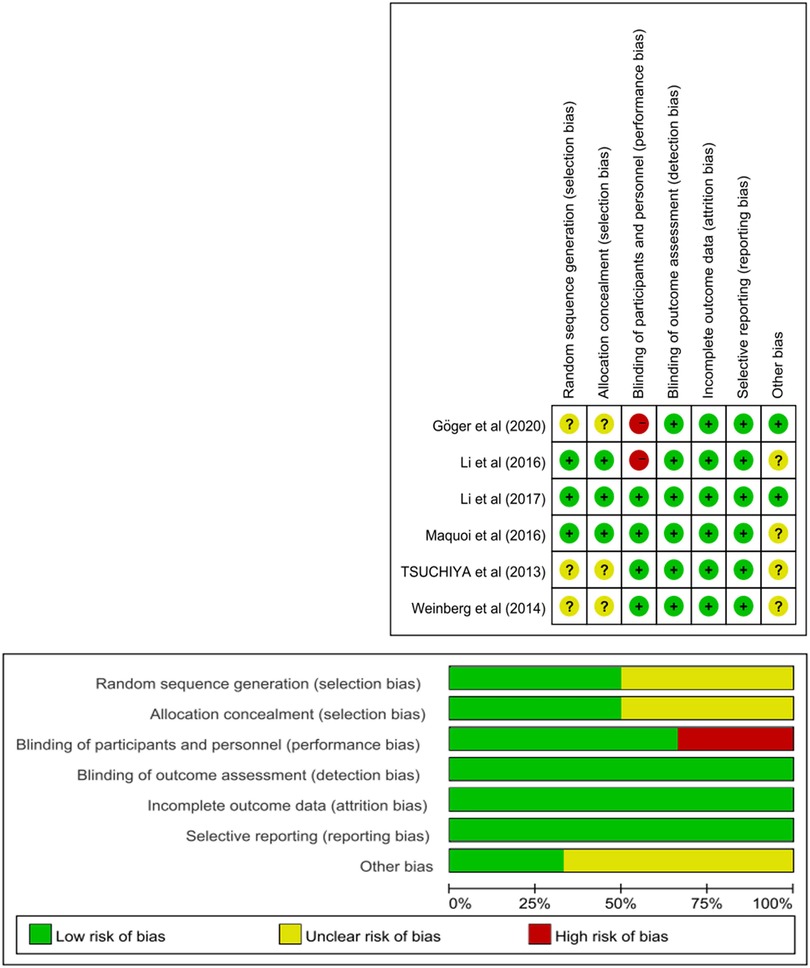
3.2. Quality assessment of the individual studies
Figure 2 shows the risk-of-bias summary and graph. Although all of the included studies were RCTs, only three of them (15, 17, 18) detailed their randomization protocols. Two RCTs (9, 15) did not use the double-blind method, and performance bias was rated as a high risk of bias. The others were classified as having a low or unclear risk of bias.
3.3. The efficacy of PNB
VAS scores of CRBD at 0–1 h (arrival in the PACU), 1–2 h, 4–8 h, 8–12 h and 12–24 h in the block and non-block groups were inquired and recorded, and a meta-analysis was performed to investigate the incidences of CRDB and moderate to severe CRBD between the two groups and to evaluate the effectiveness of PNB in preventing CRDB.
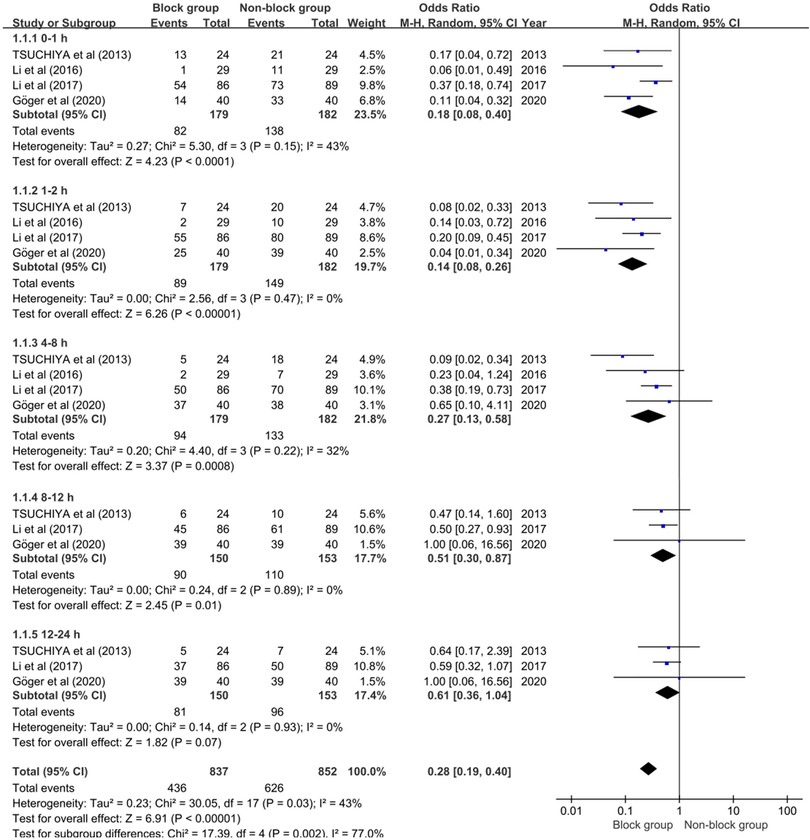
3.3.1. The incidence of CRBD
Four studies integrating 361 individuals (179 in the block group and 182 in the non-block group) were enrolled in the meta-analysis to assess the influence of PNB on the incidence of CRBD. Because of the considerable heterogeneity (P = 0.03, I2 = 43%) among studies, the random-effect model was used. Individuals who received a pudendal nerve block had a lower incidence of CRBD than those who did not receive a pudendal nerve block at 0–1 h (OR 0.22; 95% CI, 0.18–0.08; P < 0.0001), 1–2 h (OR 0.14; 95% CI, 0.08–0.26; P < 0.00001), 4–8 h (OR 0.27; 95% CI, 0.13 to 0.58; P < 0.0008) and 8–12 h (OR 0.51; 95% CI, 0.30 to 0.87; P = 0.01), while there was no significant difference between the two groups in the incidence of CRBD at 12–24 h (OR 0.61; 95% CI, 0.36 to 1.04; P = 0.07) (see Figure 3). According to the findings of this meta-analysis, PNB can dramatically lower the incidence of postoperative CRBD in male patients.
3.3.2. The incidence of moderate to severe CRBD
Four studies integrating 361 individuals (179 in the block group and 182 in the non-block group) were enrolled in the meta-analysis to further evaluate the impact of PNB on the incidence of moderate to severe CRBD. There was considerable heterogeneity (P = 0.04, I2 = 40%) among studies, hence the random-effect model was used. The block group showed a lower incidence of moderate to severe CRBD than non-block group at 0–1 h, 1–2 h and 4–8 h, and the ORs were 0.12 (95% CI, 0.03 to 0.49; P = 0.003), 0.17 (95% CI, 0.08 to 0.37; P < 0.00001) and 0.29 (95% CI, 0.15 to 0.55; P = 0.0002) respectively. Conversely, there was no significant difference at 8–12 h (OR 0.65; 95% CI, 0.26 to 1.62; P = 0.35) and 12–24 h postoperatively (OR 0.74; 95% CI, 0.36 to 1.52; P = 0.42), as shown in Figure 4. These findings showed that PNB significantly reduced the incidence of postoperative moderate to severe CRBD in male patients.
3.3.3. The incidence of PONV
Three studies incorporating 205 patients (103 in the block group and 102 in the non-block group) revealed adifference in the occurrence of PONV. There was no heterogeneity (P = 0.56, I2 = 0%) among studies, so the fixed-effect model was used for the meta-analysis. As shown in Figure 4, the non-block group was significantly associated with a higher incidence of PONV (OR, 0.14; 95% CI, 0.05 to 0.39; P = 0.0002). We concluded that PNB might greatly lower the incidence of PONV in male patients.
3.3.4. The opioid need in 24 h after surgery
First, two RCTs involving 138 patients reported the incidence of need for analgesics in 24 h after surgery. Our pooled analysis indicated that although there was a difference between the two groups in the incidence of need for analgesics, there was no statistical significance (OR 0.70; 95% CI, 0.33 to 1.47; P = 0.34).In addition, two RCTs involving 183 patients reported opioid consumption in 24 h after surgery. No significant difference was shown between the two sets (OR −6.33; 95% CI, −17.05 to 4.38; P = 0.25).
4. Discussion
CRBD, as an unavoidable clinical entity, not only afflicts patients but also frequently makes clinicians lose what to do. Studies on CRBD has never ended, and scholars have been striving for a better solution to handle this perplexing problem. Antimuscarinic agents are the first-line drugs for treating CRBD since it has long been recognized that CRBD is induced by involuntary contraction of bladder smooth muscle and that the neurotransmitter released in this physiological process isacetylcholine. Solifenacin, darifenacin, butylscopolamine, oxybutynin and tolterodine are antimuscarinic medicines with demonstrated effectiveness (4, 5). Nevertheless, some patients had adverse effects such as dry mouth, constipation, sleepiness and blurring of vision, resulting in poorer patient compliance (19). Emerging antiepileptic drugs such as gabapentin and pregabalin, as well as anesthetics like ketamine, have been demonstrated to significantly relieve CRBD, albeit with sedation (5, 20). Moreover, a recent meta-analysis revealed that subhypnotic doses of ketamine can decrease the incidence and severity of postoperative CRBD without causing significant adverse effects (21). Furthermore, paracetamol, as an inhibitor of prostaglandin synthesis, had some effect on CRBD, although there were fewer reports (22).
Nerve block technology has evolved with the advent of ultrasound devices. Physiologically, impulses in afferent nerves derived in the urethra and bladder triangle travel from the sacral nerves (S2–4) to the sacral segments of the spinal cord and eventually to the pudendal nerves and their branches, triggering urethral muscles and sphincters of the perineum and pelvic floor to contract (23). The mechanism of CRBD is strongly intertwined with this reflex arc, and the presence of a urinary catheter induces mechanical stimulation of the bladder or urethra, which in turn drives involuntary spasms of bladder smooth muscle (8). Based on this logic, blocking either region on this reflex arc would help avoid CRBD.
Pudendal nerve block and dorsal penile nerve block are now the most well-known methods of PNB, with the latter being the terminal branch of the pudendal nerve. In fact, pudendal nerve or branch block was initially employed to treat anal and urethral sphincter incompetence (24). Additionally, pudendal nerve block can also be used to relieve pain after vaginal birth, vaginal repair, circumcision and hypospadias (17). Weinberg and colleagues initially conducted a double-blind trial in 2014 to assess the effect of dorsal penile nerve block on CRBD following robot-assisted radical prostatectomy. Unfortunately, the evidence gathered did not support the efficacy of dorsal penile nerve block (10). In contrast, a prospective, randomized, controlled experiment indicated that dorsal penile nerve block was both safe and effective in preventing postoperative CRBD (15). Herein, we performed this meta-analysis with a total of six articles, and our study proved that PNB significantly decreased the incidence of CRBD, moderate to severe CRBD and PONV in patients with urinary catheters, especially within 8 h after surgery.
It is noteworthy that caudal block is the first to be utilized to treat CRBD. In 2013, Tsuchiya et al. discovered that ultrasound-guided caudal block might safely diminish CRBD in male patients following cervical laminoplasty (16). However, the caudal block procedure has been so dangerous, especially in obese or older patients, that clinicians have been overwhelmed. Caudal block can result in repeated punctures, hematomas, neurological damage, and infections due to anatomical variances of the sacral hiatus, even with ultrasound guidance (16, 25). In addition, a randomized controlled trial sought to validate the effectiveness of transvs. abdominis plane block in alleviating CRBD and pain in patients following open prostatectomy, however the findings were discouraging (18). Similarly, the current meta-analysis failed to demonstrate that nerve blocks reduced postoperative analgesic consumption in patients, but this cannot be ignored due to the small number of studies included in this meta-analysis. The difference in the incidence of CRBD and moderate to severe CRBD between the block group and non-block group vanished within 8 h postoperatively, possibly due to the anesthetic effect of the PNB wearing off. As a result, the timing of nerve blocks should be dictated by the length of the surgery (16). Currently, most studies have revealed no major complications with the use of PNB, which may benefit from ultrasound technology. Some self-limiting complications, including urine retention, mild bleeding, fever, tachycardia, or hypotension, usually heal on their own. Notably, hematoma, pudendal nerve injury, vascular injury, rectal perforation, muscular weakness or numbness in the region of nerve block, and urine or fecal incontinence are all unusual complications of PNB (26, 27). Once those issues occur, pharmacological or even surgical intervention may be warranted. A previous study reported that the risks of complicated fever, urinary retention, and hemorrhage in the PNB group were 3.4%, 1.7%, and 1.7%, respectively (28). Although the effectiveness of PNB in reducing CRBD is widely recognized, the risks of nerve block should not be neglected.
Despite the fact that all RCTs were included in this study, it had several flaws. First, the anesthetics used in the nerve block were not uniform, and whether this had an influence on our results had to be determined. Although the VAS score is frequently used to assess patients' symptoms, it is difficult to discern between CRBD and catheter-related pain or incision-related pain, so appropriate questionnaires to assess CRBD are desperately needed (5). It is also an important confounding element that we do not have access to whether antimuscarinic medications were used in included patients. Second, a prospective observational study (29) indicated that the type of surgery was a predictor of CRBD severity, and prostate surgery seemed to cause more severe CRBD than bladder or non urological surgery. However, the factor differed in our meta-analysis, which might be a significant confounding factor. Finally, the inconsistency of catheter diameter and balloon inflation are bound to impact our findings, but the subjects in this study were all male patients, which eliminated gender differences and made our findings more convincing, as a prospective observational study found that male sex and catheter diameter greater than or equal to 18 Fr were significant predictors of CRBD (1). To the best of our knowledge, this is the first systematic review and meta-analysis of the effectiveness of PNB in the treatment of CRBD.
5. Conclusion
In conclusion, our meta-analysis demonstrated that PNB is an effective measure for the prevention of postoperative CRBD in male patients, as it reduces the incidence of CRBD, moderate to severe CRBD and PONV, particularly within 8 h after surgery. Nevertheless, a pooled analysis with a larger sample to validate our conclusions is warranted.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
Guarantor of integrity of the entire study: XB, ML, JL, JW; Conceptualization: JW, YC; Literature search: XB, ML, HL; Data collection: XB, HY, GT; Statistical analysis: XB, ZZ, XW; Manuscript preparation: XB, ML; Manuscript editing: XB, ML, JL. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Joint fund of Shandong Natural Science Foundation, under Code ZR2021LSW019, grants from the National Nature Science Foundation of China (Nos. 81870525) and Taishan Scholars Program of Shandong Province (No. tsqn201909199).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
PNB, peripheral nerve block; CRBD, catheter-related bladder discomfort; ERAS, enhanced recovery after surgery; OAB, overactive bladder; NSAIDs, nonsteroidal anti-inflammatory drugs; RCTs, randomized controlled trials; PACU, post-anesthesia care unit; VAS, visual analog scale; CI, confidence interval; OR, odds ratio; SD, standard deviation; PONV, postoperative nausea and vomiting.
References
1. Binhas M, Motamed C, Hawajri N, Yiou R, Marty J. Predictors of catheter-related bladder discomfort in the post-anaesthesia care unit. Ann Fr Anesth Reanim. (2011) 30(2):122–5. doi: 10.1016/j.annfar.2010.12.009
2. Jeffery N, Mundy A. Innovations in indwelling urethral catheterisation. BJU Int. (2020) 125(5):664–8. doi: 10.1111/bju.14994
3. Lim N, Yoon H. Factors predicting catheter-related bladder discomfort in surgical patients. J Perianesth Nurs. (2017) 32(5):400–8. doi: 10.1016/j.jopan.2016.03.012
4. Bai Y, Wang X, Li X, Pu C, Yuan H, Tang Y, et al. Management of catheter-related bladder discomfort in patients who underwent elective surgery. J Endourol. (2015) 29(6):640–9. doi: 10.1089/end.2014.0670
5. Jang EB, Hong SH, Kim KS, Park SY, Kim YT, Yoon YE, et al. Catheter-related bladder discomfort: how can we manage it? Int Neurourol J. (2020) 24(4):324–31. doi: 10.5213/inj.2040108.054
6. Bala I, Bharti N, Chaubey VK, Mandal AK. Efficacy of gabapentin for prevention of postoperative catheter-related bladder discomfort in patients undergoing transurethral resection of bladder tumor. Urology. (2012) 79(4):853–7. doi: 10.1016/j.urology.2011.11.050
7. Tauzin-Fin P, Sesay M, Svartz L, Krol-Houdek MC, Maurette P. Sublingual oxybutynin reduces postoperative pain related to indwelling bladder catheter after radical retropubic prostatectomy. Br J Anaesth. (2007) 99(4):572–5. doi: 10.1093/bja/aem232
8. Anderson KE. Pharmacology of lower urinary tract smooth muscles and penile erectile tissues. Pharmacol Rev. (1993) 45(3):253–308.8248281
9. Göger YE, Özkent MS, Göger E, Kılınç MT, Ecer G, Pişkin MM, et al. A randomised-controlled, prospective study on the effect of dorsal penile nerve block after TURP on catheter-related bladder discomfort and pain. Int J Clin Pract. (2021) 75(5):e13963. doi: 10.1111/ijcp.13963
10. Weinberg AC, Woldu SL, Bergman A, Roychoudhury A, Patel T, Berg W, et al. Dorsal penile nerve block for robot-assisted radical prostatectomy catheter related pain: a randomized, double-blind, placebo-controlled trial. Springerplus. (2014) 3:181. doi: 10.1186/2193-1801-3-181
11. Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, et al. The cochrane Collaboration's tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
12. McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res. (2020) 29(9):2520–37. doi: 10.1177/0962280219889080
13. Li JY, Liao R. Prevention of catheter-related bladder discomfort—pudendal nerve block with ropivacaine versus intravenous tramadol: study protocol for a randomized controlled trial. Trials. (2016) 17(1):448. doi: 10.1186/s13063-016-1575-y
14. Li JY, Liao R. Dorsal penile nerve block with ropivacaine versus intravenous tramadol for the prevention of catheter-related bladder discomfort: study protocol for a randomized controlled trial. Trials. (2015) 16:596. doi: 10.1186/s13063-015-1130-2
15. Li JY, Yi ML, Liao R. Dorsal penile nerve block with ropivacaine-reduced postoperative catheter-related bladder discomfort in male patients after emergence of general anesthesia: a prospective, randomized, controlled study. Medicine. (2016) 95(15):e3409. doi: 10.1097/MD.0000000000003409
16. Tsuchiya M, Kyoh Y, Mizutani K, Yamashita J, Hamada T. Ultrasound-guided single shot caudal block anesthesia reduces postoperative urinary catheter-induced discomfort. Minerva Anestesiol. (2013) 79(12):1381–8.23811624
17. Xiaoqiang L, Xuerong Z, Juan L, Mathew BS, Xiaorong Y, Qin W, et al. Efficacy of pudendal nerve block for alleviation of catheter-related bladder discomfort in male patients undergoing lower urinary tract surgeries: a randomized, controlled, double-blind trial. Medicine. (2017) 96(49):e8932. doi: 10.1097/MD.0000000000008932
18. Maquoi I, Joris JL, Dresse C, Vandenbosch S, Venneman I, Brichant JF, et al. Transversus abdominis plane block or intravenous lignocaine in open prostate surgery: a randomized controlled trial. Acta Anaesthesiol Scand. (2016) 60(10):1453–60. doi: 10.1111/aas.12773
19. Andersson KE. Antimuscarinics for treatment of overactive bladder. Lancet Neurol. (2004) 3(1):46–53. doi: 10.1016/S1474-4422(03)00622-7
20. Moharari R S, Lajevardi M, Khajavi M, Najafi A, Shariat Moharari G, Etezadi F. Effects of intra-operative ketamine administration on postoperative catheter-related bladder discomfort: a double-blind clinical trial. Pain Pract. (2014) 14(2):146–50. doi: 10.1111/papr.12055
21. Lu Y, Li Q, Wang Y, Zhou Z, Zhang D, Bao Y, et al. Meta-analysis of the efficacy and safety of ketamine on postoperative catheter-related bladder discomfort. Front Pharmacol. (2022) 13:816995. doi: 10.3389/fphar.2022.816995
22. Ergenoglu P, Akin S, Yalcin Cok O, Eker E, Kuzgunbay B, Turunc T, et al. Effect of intraoperative paracetamol on catheter-related bladder discomfort: a prospective, randomized, double-blind study. Curr Ther Res Clin Exp. (2012) 73(6):186–94. doi: 10.1016/j.curtheres.2012.08.001
23. de Groat WC, Yoshimura N. Anatomy and physiology of the lower urinary tract. Handb Clin Neurol. (2015) 130:61–108. doi: 10.1016/B978-0-444-63247-0.00005-5
24. Shafik A, el-Sherif M, Youssef A, Olfat ES. Surgical anatomy of the pudendal nerve and its clinical implications. Clin Anat. (1995) 8(2):110–5. doi: 10.1002/ca.980080205
25. Sekiguchi M, Yabuki S, Satoh K, Kikuchi S. An anatomic study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain. (2004) 20(1):51–4. doi: 10.1097/00002508-200401000-00010
26. Di Giuseppe M, Saporito A, La Regina D, Tasciotti E, Ghielmini E, Vannelli A, et al. Ultrasound-guided pudendal nerve block in patients undergoing open hemorrhoidectomy: a double-blind randomized controlled trial. Int J Colorectal Dis. (2020) 35(9):1741–7. doi: 10.1007/s00384-020-03630-x
27. Fadel MG, Peltola L, Pellino G, Frunza G, Kontovounisios C. The role of pudendal nerve block in colorectal surgery: a systematic review. J Invest Surg. (2021) 34(11):1238–45. doi: 10.1080/08941939.2020.1786611
28. Tepetes K, Symeonidis D, Christodoulidis G, Spyridakis M, Hatzitheofilou K. Pudendal nerve block versus local anesthesia for harmonic scalpel hemorrhoidectomy: a prospective randomized study. Tech Coloproctol. (2010) 14(Suppl 1):S1–3. doi: 10.1007/s10151-010-0614-z
Keywords: peripheral nerve block, CRBD, VAS, PONV, incidence, meta-analysis
Citation: Bao X, Liu M, Li J, Yao H, Liu H, Tang G, Wang X, Zhou Z, Wu J and Cui Y (2023) The efficacy of peripheral nerve block on postoperative catheter-related bladder discomfort in males: A systematic review and meta-analysis. Front. Surg. 10:1099628. doi: 10.3389/fsurg.2023.1099628
Received: 18 November 2022; Accepted: 16 January 2023;
Published: 3 February 2023.
Edited by:
Murat Akand, University Hospitals Leuven, BelgiumReviewed by:
Francesco Mongelli, Lugano Regional Hospital, SwitzerlandAndrey O Morozov, I.M. Sechenov First Moscow State Medical University, Russia
© 2023 Bao, Liu, Li, Yao, Liu, Tang, Wang, Zhou, Wu and Cui. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yuanshan Cui OTc4OTQ2NzAwQHFxLmNvbQ== Jitao Wu d2p0dXJvbG9neUAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Xingjun Bao1,2,†
Xingjun Bao1,2,† Gonglin Tang
Gonglin Tang Zhongbao Zhou
Zhongbao Zhou Jitao Wu
Jitao Wu Yuanshan Cui
Yuanshan Cui