
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 27 March 2023
Sec. Surgical Oncology
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1095329
Background: Delirium detection is challenging due to the fluctuating nature and frequent hypoactive presentation. This study aimed to determine an optimal strategy that detects delirium with higher sensitivity but lower effort in older patients admitted to the intensive care unit (ICU) after surgery.
Methods: This was a secondary analysis of the database from a randomized trial. Seven hundred older patients (aged ≥65 years) who were admitted to the ICU after elective noncardiac surgery were enrolled. Delirium was assessed with the Confusion Assessment Method for the ICU (CAM-ICU) twice daily during the first 7 days postoperatively. The sensitivity of different strategies in detecting delirium were analyzed and compared.
Results: Of all enrolled patients, 111 (15.9%; 95% CI: 13.3% to 18.8%) developed at least one episode of delirium during the first 7 postoperative days. Among patients who developed delirium, 60.4% (67/111) had their first delirium onset on postoperative day 1, 84.7% (94/111) by the end of day 2, 91.9% (102/111) by the end of day 3, and 99.1% (110/111) by the end of day 4. Compared with delirium assessment twice daily for 7 days, twice-daily measurements for 5 days detected 100% of delirium patients with 71% efforts; twice-daily measurements for 4 days detected 99% (95% CI: 94% to 100%) of delirium patients with 57% efforts; twice-daily assessment for 3 days detected 92% (95% CI: 85% to 96%) of delirium patients with only 43% efforts.
Conclusions: For older patients admitted to the ICU after elective noncardiac surgery, it is reasonable to detect delirium with the CAM-ICU twice daily for no more than 5 days, and if the personnel and funds are insufficient, 4 days could be sufficient.
Delirium is an acutely occurred and short-lived syndrome, characterized by fluctuating changes in attention, level of consciousness, and cognitive function (1). It is a common complication after major surgery, especially in older patients (2). According to a recent systematic review, the reported incidence ranged from 4% to 46% in patients aged ≥60 years following noncardiac surgery (3). The occurrence of postoperative delirium is associated with increased morbidity and mortality (4), prolonged stays in the intensive care unit (ICU) and hospital, and worsened functional recovery (5, 6). Studies showed that postoperative delirium mostly occurs in the first few days (7–9). Various diagnostic tools, such as the Confusion Assessment Method (CAM) and the CAM for the intensive care unit (CAM-ICU), have been introduced and validated to facilitate delirium screening (10–12).
The detection of delirium can be challenging due to the fluctuating nature and frequent hypoactive presentation. Interview-based methods, i.e., delirium assessed by trained interviewers during brief encounters, is frequently used in clinical studies and daily practice (13). However, it is still unknown how often should the assessments be done and how long should the evaluation period be. A previous study reported that daily assessment is not enough because cases occurring during night-shift might be missed (14). In a recent study of 788 patients following cardiac surgery, delirium was detected more often in the mornings than evenings, and CAM-ICU assessment twice daily for 4 days detected an estimated 97% of postoperative delirium (15).
In this analysis, we aimed to evaluate the effect of different strategies in detecting delirium during the first 7 days after non-cardiac surgery, and to determine the most favorable strategy that detected delirium with high sensitivity and low effort.
This was a post hoc analysis of data collected during a randomized trial. The underlying trial was conducted in two affiliated hospitals of Peking University from August 17, 2011 to November 20, 2013 (www.chictr.org.cn, number ChiCTR-TRC-10000802) (5). The protocol for this analysis was approved by the Biomedical Research Ethics Committee of Peking University First Hospital [2022(407) on September 21, 2022; No. 8 Xishiku Street, Beijing 100034, China; Chairperson Prof. Yan-Yan Yu]; informed consent was waived since all analysis was performed on de-identified data without any further patient/family member contact.
We enrolled patients aged ≥65 years who were admitted to the ICU after elective noncardiac surgery. We excluded those who met the following criteria: refused to participate; preoperative history of schizophrenia, epilepsy, Parkinson's disease, or myasthenia gravis; inability to communicate because of coma, severe dementia or language barriers before surgery; brain injury or neurosurgery; preoperative left ventricular ejection fraction (LVEF) <30%, sick sinus syndrome, severe sinus bradycardia (<50 beats per minute), or second-degree or higher atrioventricular block without pacemaker; severe liver dysfunction (Child-Pugh C grade); severe renal dysfunction (preoperative renal replacement therapy); or expected survival <24 h (5).
In the underlying trial, the enrolled patients were randomly assigned to receive intravenous infusion of either placebo (normal saline) or dexmedetomidine (at a rate of 0.1 μg/kg/h) from ICU admission on the day of surgery until 8:00 am on the first day after surgery (5).
Postoperative delirium was assessed with the CAM-ICU (11, 16) by investigators who had been trained by a psychiatrist. The CAM-ICU detects four features of delirium including (1) acute onset of mental status changes or a fluctuating course, (2) inattention, (3) disorganized thinking, and (4) altered level of consciousness. Patients showing features of (1) and (2), with either (3) or (4), were diagnosed as having delirium. The Chinese verison CAM-ICU had been validated in the ICU setting (11, 16). We have considerable experience in assessing delirium with the CAM-ICU (17, 18).
Delirium assessment was performed twice daily, i.e., from 8:00 to 10:00 am and from 18:00 to 20:00 pm, during the first 7 postoperative days or until hospital discharge. Before each delirium assessment, sedation and agitation was evaluated with the Richmond Agitation Sedation Scale (RASS); the score ranges from −5 [unarousable] to +4 [combative] and 0 indicates alert and calm (19). Deeply sedated or unarousable patients (RASS score −4 or −5) were marked as comatose and not assessed for delirium. Delirium was assessed for those with a RASS score from −3 to +4. Investigators performing delirium assessment had been trained by a psychiatrist before initiating the trial.
Continuous variables with normal distribution were analyzed using the independent samples t-test. Continuous variables with non-normal distribution and ranked data were analyzed using the Mann–Whitney U test. Categorical variables were analyzed using the chi-square test or Fisher's exact test. We used frequency tables to describe the number (%) of delirium assessments completed each morning and afternoon on postoperative days 1–7, and the proportion of patients with detected delirium at different times and frequencies of assessment. Kaplan–Meier estimators were used to analyze time to first-onset delirium over postoperative days 1–7 with 3 different evaluation strategies: morning and afternoon assessments, morning only assessments, and afternoon only assessments. McNemar's test for paired proportions was used to compare morning and evening delirium detection. We used the Wilson score method to estimate the 95% CIs for the proportion of postoperative delirium cases detected for each evaluation strategy. SPSS statistical software version 25.0 was used for all analyses.
A total of 700 patients were enrolled in the underlying trial. The average age of enrolled patients was 74 years, with 60.4% were male. Patients who experienced delirium were older, had lower body mass index, suffered more previous stroke, had lower preoperative serum albumin, were more frequently admitted to ICU with intubation, and received less low-dose dexmedetomidine when compared with those who did not (Table 1).
Of all enrolled patients, 111 (15.9%; 95% CI: 13.3% to 18.8%) developed at least one episode of delirium during the first 7 postoperative days. Among these, 60.4% (67/111) had their first delirium onset on postoperative day 1, 84.7% (94/111) by the end of day 2, 91.9% (102/111) by the end of day 3, 99.1% (110/111) by the end of day 4, and 100% (111/111) by the end of day 5 (Table 2).
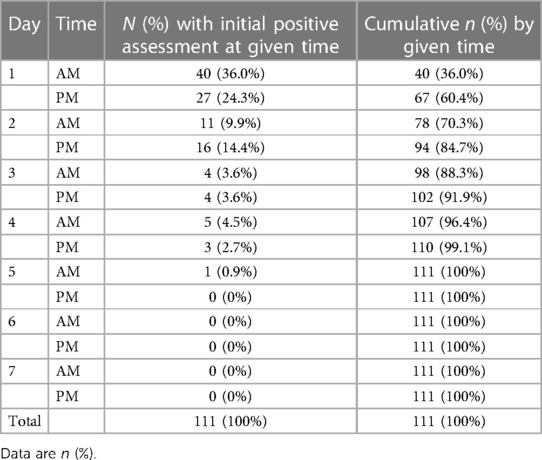
Table 2. First delirium event for patients (n = 111) with any positive delirium during the first 7 postoperative days.
We compared the sensitivity of different strategies in detecting first postoperative delirium compared with twice-daily assessments for 7 days (Table 3). There was no significant difference in the sensitivity of delirium detection with morning only or afternoon only assessments (Figure 1). Both of the above strategies detected 83 (11.9% of 700) delirium patients during the first 7 postoperative days. Twice-daily measurements for 4 days detected 99% (95% CI: 94% to 100%) of delirium patients with 57% efforts. Similarly, twice-daily assessment for 3 days detected 92% (95% CI: 85% to 96%) of delirium patients with only 43% efforts.
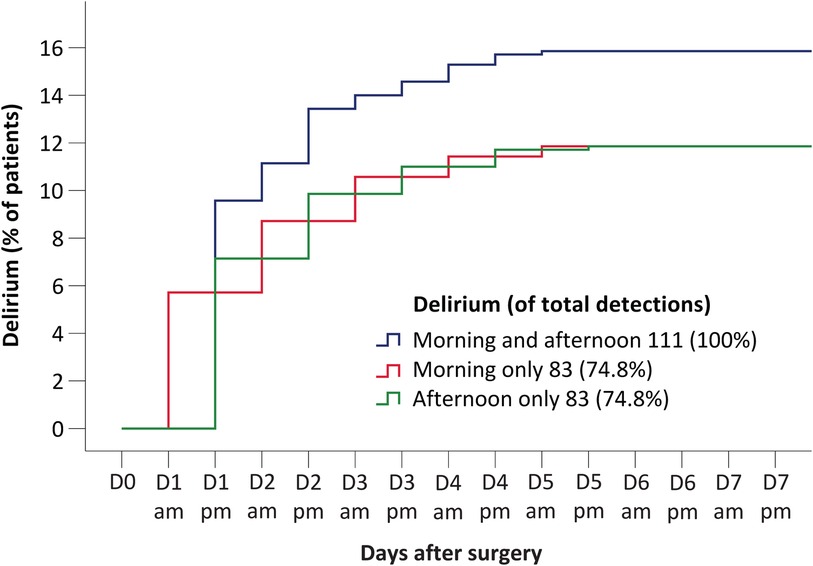
Figure 1. Time to onset of delirium using morning and afternoon assessments (blue curve), morning assessments only (red curve), and afternoon assessments only (green curve). Results to the right of figure legends indicate the number and fraction of the 111 detected delirium cases identified with each strategy.
In the present study, delirium occurred in 15.9% of our patients during the first seven days after non-cardiac surgery. The rate was relatively lower than previously reported incidence (24.4% to 44.5%) in similar patient populations (20, 21). This could be explained by the fact that half of our patients received low-dose dexmedetomidine infusion during the night after surgery, a regimen that has been proved effective in decreasing delirium in high-risk patients (5, 22, 23). Another possible reason was that multiple non-pharmacological measures have been widely applied in clinical practice to prevent delirium (24, 25). When patients given dexmedetomidine were excluded, the incidence of delirium (22.6%) was close to the reported range.
Our results showed that delirium mainly occurred early after surgery, i.e., 91.9% of new-onset delirium developed within the first three postoperative days in our patients. This is in line with other studies (8, 26). Similar results were also reported in recent trials. For example, 89% of all delirious cases occurred within 3 days after cardiac surgery (7), and that after noncardiac surgery was 88% (27). The phenomenon could be attributed to the fact that surgery-related responses including the degree of inflammation and the secretion of neuroendocrine hormone, which play important roles in the pathogenesis of delirium, peak in the early postoperative period (17, 28–30).
Delirium has a fluctuating nature and is frequently presented in a hypoactive form (31, 32). It is not surprising that many delirious cases, up to 76%, were miss diagnosed in the settings of emergency department, palliative care unit, and ICU (33–35). Delirium detection can be improved with frequent monitoring, and early treatment of the underlying condition can improve outcome (36). However, redundant evaluations require more manpower and can be costly. The commonly used delirium evaluation strategy is twice daily after surgery for several days. Limiting the number of delirium assessments while maintaining high sensitivity would help to make the research work cheaper and more practical.
During the analysis, we designed various evaluation strategies to simplify the original one that assessed delirium twice daily for 7 days after surgery. We found that CAM-ICU assessments twice daily for 5 postoperative days detected 100% delirium but required 29% less evaluation, while CAM-ICU assessment twice daily for 4 days detected 99% delirium but required 43% less evaluation. It is thus reasonable to design studies with no more than 5 days of delirium assessments, and if the personnel and funds of the study are insufficient, 4 days could be sufficient. A previous study reported that delirium was detected more often in the morning than in the evening (15). However, we did not find difference in detecting delirium between morning only and afternoon only assessments, possibly due to different patient population and improved nighttime environment and care in the ICU. Both methods detected only 75% delirium within 7 days and are therefore not recommended.
The advantages of our study included that the investigators who performed delirium assessment had been trained by a psychiatrist and that delirium assessment was performed twice daily for 7 consecutive days. These helped us to detect most delirium cases. There are also some limitations. Firstly, while investigators had been trained for delirium assessment, the inter-investigator differences were hardly avoidable. Secondly, we enrolled patients following various kinds of non-cardiac surgeries. This increases the generalizability of our study but increases the complexity in explaining the results. Thirdly, all patients included in the underlying trial were admitted to the ICU after noncardiac surgery. Whether our results can be extrapolated to non-ICU patients requires further investigation.
In older patients admitted to the ICU after elective noncardiac surgery, 60.4% of all delirium detected over 7 days occurred during the first postoperative day and 91.2% occurred within the first 3 postoperative days. Compared with CAM-ICU assessment twice daily for 7 days, a twice-daily assessment for 5 days detected 100% delirium with 29% less effort, while a twice-daily assessment for 4 days detected 99% delirium with 43% less effort. Delirium assessments should therefore be performed twice daily for at least 4 initial postoperative days.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Ethics Committee of Peking University First Hospital. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
KW and XS designed the study, collected, analyzed and interpreted the data, and drafted the manuscript. JM contributed to data analysis. DW conceived and designed the study, reviewed the original data and the results of analyses, and critically revised the manuscript. All authors contributed to the article and approved the submitted version.
This work was supported by the National Key R&D Program of China (2018YFC2001800). The sponsors had no role in the design or conduct of the trial; data collection, trial management, data analysis, interpretation of the results, or preparation and approval of the manuscript.
The authors gratefully acknowledge Zhao-Ting Meng and Fan Cui (Department of Anesthesiology, Peking University First Hospital, Beijing, China) for their help in data collection.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
2. Evered L, Silbert B, Knopman DS, Scott DA, DeKosky ST, Rasmussen LS, et al. Recommendations for the nomenclature of cognitive change associated with anaesthesia and surgery-2018. Anesthesiology. (2018) 129(5):872–9. doi: 10.1097/ALN.0000000000002334
3. Silva AR, Regueira P, Albuquerque E, Baldeiras I, Cardoso AL, Santana I, et al. Estimates of geriatric delirium frequency in noncardiac surgeries and its evaluation across the years: a systematic review and meta-analysis. J Am Med Dir Assoc. (2021) 22(3):613–20.e9. doi: 10.1016/j.jamda.2020.08.017
4. Klein Klouwenberg PMC, Zaal IJ, Spitoni C, Ong DSY, van der Kooi AW, Bonten MJM, et al. The attributable mortality of delirium in critically ill patients: prospective cohort study. Br Med J. (2014) 349:g6652. doi: 10.1136/bmj.g6652
5. Su X, Meng Z-T, Wu X-H, Cui F, Li H-L, Wang D-X, et al. Dexmedetomidine for prevention of delirium in elderly patients after non-cardiac surgery: a randomised, double-blind, placebo-controlled trial. Lancet. (2016) 388(10054):1893–902. doi: 10.1016/S0140-6736(16)30580-3
6. Abelha FJ, Luís C, Veiga D, Parente D, Fernandes V, Santos P, et al. Outcome and quality of life in patients with postoperative delirium during an ICU stay following major surgery. Crit Care. (2013) 17(5):R257. doi: 10.1186/cc13084
7. Turan A, Duncan A, Leung S, Karimi N, Fang J, Mao G, et al. Dexmedetomidine for reduction of atrial fibrillation and delirium after cardiac surgery (DECADE): a randomised placebo-controlled trial. Lancet. (2020) 396(10245):177–85. doi: 10.1016/S0140-6736(20)30631-0
8. Li CJ, Wang BJ, Mu DL, Hu J, Guo C, Li XY, et al. Randomized clinical trial of intraoperative dexmedetomidine to prevent delirium in the elderly undergoing major non-cardiac surgery. Br J Surg. (2020) 107(2):e123–e32. doi: 10.1002/bjs.11354
9. Wildes TS, Mickle AM, Ben Abdallah A, Maybrier HR, Oberhaus J, Budelier TP, et al. Effect of electroencephalography-guided anesthetic administration on postoperative delirium among older adults undergoing major surgery: the ENGAGES randomized clinical trial. JAMA. (2019) 321(5):473–83. doi: 10.1001/jama.2018.22005
10. Gusmao-Flores D, Salluh JI, Chalhub R, Quarantini LC. The confusion assessment method for the intensive care unit (CAM-ICU) and intensive care delirium screening checklist (ICDSC) for the diagnosis of delirium: a systematic review and meta-analysis of clinical studies. Crit Care. (2012) 16(4):R115. doi: 10.1186/cc11407
11. Ely EW, Inouye SK, Bernard GR, Gordon S, Francis J, May L, et al. Delirium in mechanically ventilated patients: validity and reliability of the confusion assessment method for the intensive care unit (CAM-ICU). JAMA. (2001) 286(21):2703–10. doi: 10.1001/jama.286.21.2703
12. Wei LA, Fearing MA, Sternberg EJ, Inouye SK. The confusion assessment method: a systematic review of current usage. J Am Geriatr Soc. (2008) 56(5):823–30. doi: 10.1111/j.1532-5415.2008.01674.x
13. Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA. (2017) 318(12):1161–74. doi: 10.1001/jama.2017.12067
14. Saczynski JS, Kosar CM, Xu G, Puelle MR, Schmitt E, Jones RN, et al. A tale of two methods: chart and interview methods for identifying delirium. J Am Geriatr Soc. (2014) 62(3):518–24. doi: 10.1111/jgs.12684
15. Hamadnalla H, Sessler DI, Troianos CA, Fang J, Rivas E, Ma C, et al. Optimal interval and duration of CAM-ICU assessments for delirium detection after cardiac surgery. J Clin Anesth. (2021) 71:110233. doi: 10.1016/j.jclinane.2021.110233
16. Wang C, Wu Y, Yue P, Ely EW, Huang J, Yang X, et al. Delirium assessment using confusion assessment method for the Intensive Care Unit in Chinese critically ill patients. J Crit Care. (2013) 28(3):223–9. doi: 10.1016/j.jcrc.2012.10.004
17. Mu DL, Wang DX, Li LH, Shan GJ, Li J, Yu QJ, et al. High serum cortisol level is associated with increased risk of delirium after coronary artery bypass graft surgery: a prospective cohort study. Crit Care. (2010) 14(6):R238. doi: 10.1186/cc9256
18. Wang W, Li HL, Wang DX, Zhu X, Li SL, Yao GQ, et al. Haloperidol prophylaxis decreases delirium incidence in elderly patients after noncardiac surgery: a randomized controlled trial. Crit Care Med. (2012) 40(3):731–9. doi: 10.1097/CCM.0b013e3182376e4f
19. Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, et al. The richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. (2002) 166(10):1338–44. doi: 10.1164/rccm.2107138
20. Chaiwat O, Chanidnuan M, Pancharoen W, Vijitmala K, Danpornprasert P, Toadithep P, et al. Postoperative delirium in critically ill surgical patients: incidence, risk factors, and predictive scores. BMC Anesthesiol. (2019) 19(1):39. doi: 10.1186/s12871-019-0694-x
21. Shi CM, Wang DX, Chen KS, Gu XE. Incidence and risk factors of delirium in critically ill patients after non-cardiac surgery. Chin Med J. (2010) 123(8):993–9. doi: 10.3760/cma.j.issn.0366-6999.2010.08.004
22. Skrobik Y, Duprey MS, Hill NS, Devlin JW. Low-dose nocturnal dexmedetomidine prevents ICU delirium. A randomized, placebo-controlled trial. Am J Respir Crit Care Med. (2018) 197(9):1147–56. doi: 10.1164/rccm.201710-1995OC
23. Ng KT, Shubash CJ, Chong JS. The effect of dexmedetomidine on delirium and agitation in patients in intensive care: systematic review and meta-analysis with trial sequential analysis. Anaesthesia. (2019) 74(3):380–92. doi: 10.1111/anae.14472
24. Collinsworth AW, Priest EL, Campbell CR, Vasilevskis EE, Masica AL. A review of multifaceted care approaches for the prevention and mitigation of delirium in intensive care units. J Intensive Care Med. (2016) 31(2):127–41. doi: 10.1177/0885066614553925
25. Bounds M, Kram S, Speroni KG, Brice K, Luschinski MA, Harte S, et al. Effect of ABCDE bundle implementation on prevalence of delirium in intensive care unit patients. Am J Crit Care. (2016) 25(6):535–44. doi: 10.4037/ajcc2016209
26. Mu DL, Zhang DZ, Wang DX, Wang G, Li CJ, Meng ZT, et al. Parecoxib supplementation to morphine analgesia decreases incidence of delirium in elderly patients after hip or knee replacement surgery: a randomized controlled trial. Anesth Analg. (2017) 124(6):1992–2000. doi: 10.1213/ANE.0000000000002095
27. Li YW, Li HJ, Li HJ, Zhao BJ, Guo XY, Feng Y, et al. Delirium in older patients after combined epidural-general anesthesia or general anesthesia for major surgery: a randomized trial. Anesthesiology. (2021) 135(2):218–32. doi: 10.1097/ALN.0000000000003834
28. Cerejeira J, Batista P, Nogueira V, Vaz-Serra A, Mukaetova-Ladinska EB. The stress response to surgery and postoperative delirium: evidence of hypothalamic-pituitary-adrenal axis hyperresponsiveness and decreased suppression of the GH/IGF-1 axis. J Geriatr Psychiatry Neurol. (2013) 26(3):185–94. doi: 10.1177/0891988713495449
29. Alam A, Hana Z, Jin Z, Suen KC, Ma D. Surgery, neuroinflammation and cognitive impairment. EBioMedicine. (2018) 37:547–56. doi: 10.1016/j.ebiom.2018.10.021
30. Mulkey MA, Hardin SR, Olson DM, Munro CL. Pathophysiology review: seven neurotransmitters associated with delirium. Clin Nurse Spec. (2018) 32(4):195–211. doi: 10.1097/NUR.0000000000000384
31. Pandharipande P, Cotton BA, Shintani A, Thompson J, Costabile S, Truman Pun B, et al. Motoric subtypes of delirium in mechanically ventilated surgical and trauma intensive care unit patients. Intensive Care Med. (2007) 33(10):1726–31. doi: 10.1007/s00134-007-0687-y
32. Robinson TN, Raeburn CD, Tran ZV, Brenner LA, Moss M. Motor subtypes of postoperative delirium in older adults. Arch Surg. (2011) 146(3):295–300. doi: 10.1001/archsurg.2011.14
33. Lee JS, Tong T, Chignell M, Tierney MC, Goldstein J, Eagles D, et al. Prevalence, management and outcomes of unrecognized delirium in a national sample of 1,493 older emergency department patients: how many were sent home and what happened to them? Age Ageing. (2022) 51(2):afab214. doi: 10.1093/ageing/afab214
34. Klankluang W, Tongsai S, Sriphirom C, Siriussawakul A, Chanthong P, Tayjasanant S. The prevalence, associated factors, clinical impact, and state of diagnosis of delirium in palliative care patients. Support Cancer Ther. (2021) 29(12):7949–56. doi: 10.1007/s00520-021-06367-7
35. Reznik ME, Daiello LA, Thompson BB, Wendell LC, Mahta A, Potter NS, et al. Fluctuations of consciousness after stroke: associations with the confusion assessment method for the intensive care unit (CAM-ICU) and potential undetected delirium. J Crit Care. (2020) 56:58–62. doi: 10.1016/j.jcrc.2019.12.008
Keywords: delirium, cognitive fuction, elderly, noncardiac surgery, CAM-ICU (confusion assessment method for the intensive care unit)
Citation: Wang K, Su X, Ma J-H and Wang D-X (2023) Optimal strategy for delirium detection in older patients admitted to intensive care unit after non-cardiac surgery. Front. Surg. 10:1095329. doi: 10.3389/fsurg.2023.1095329
Received: 11 November 2022; Accepted: 7 March 2023;
Published: 27 March 2023.
Edited by:
Alparslan Turan, Cleveland Clinic, United StatesReviewed by:
He Liu, Zhejiang University School of Medicine & Huzhou Central Hospital, China© 2023 Wang, Su, Ma and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dong-Xin Wang d2FuZ2Rvbmd4aW5AaG90bWFpbC5jb20=; ZHh3YW5nNjVAYmptdS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Surgical Oncology, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.