
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 30 January 2023
Sec. Genitourinary Surgery and Interventions
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1081951
Cervical lymphadenopathy as the initial presentation of metastatic prostate cancer is particularly uncommon, and easily misdiagnosed. In the current study, we describe five cases of metastatic prostate cancer in our hospital that presented with cervical lymphadenopathy as an initial symptom. The diagnosis was confirmed by needle biopsy of the suspicious lymph nodes and the serum prostate specific antigen (PSA) levels of all patients exceeded 100 ng/ml. The five patients were treated with hormonal therapy; four received traditional hormonal therapy, including bicalutamide and goserelin; one patient received hormonal therapy that included abiraterone and goserelin. Case 1 developed into castration-resistant prostate cancer (CRPC) after 7 months and died after 12 months. Case 2 rejected regular hormonal therapy for personal reasons and died 6 months after the initial diagnosis. Case 3 was still alive at the time of writing. Case 4 was administered with abiraterone, prednisolone and goserelin; the treatment was effective and the patient has remained symptom-free for the last 24 months. Case 5 was treated with hormonal and chemotherapy but died 8 months after diagnosis. In conclusion, any elderly male presenting with cervical lymphadenopathy should be considered the possibility of prostate cancer, especially when the needle biopsy reveals adenocarcinoma. The prognosis for patients presented with cervical lymphadenopathy as the initial presentation is usually poor. Hormone therapy based on abiraterone may yield a better response in such cases.
Prostate cancer is the second most common form of cancer in men (1). According to the latest data, there were 1,143,300 new cases of prostate cancer worldwide in 2020 (2). The axial skeleton and regional lymph nodes are the most common sites of metastases for prostate cancer,followed by the lungs, bladder, liver and adrenal glands (3). However, distal metastases to the cervical lymph nodes are very rare, especially as an initial presentation for prostate cancer (4), the incidence of this condition is less than 0.15% (5). Besises, the presence of metastatic lymph nodes is a poor prognostic factor in patients with prostate cancer, and the survival rates are significantly reduced in such patients (6). Herein, we report five rare cases presenting with cervical lymph node enlargement as an initial diagnosis between January 2010 and December 2021 in our hospital. We also provide a review of the current literature.
First, we gained approval from the Ethics Committee of the Second Affiliated Hospital at Dalian Medical University, and the permision for publication has been obtained from the patients or their representatives. Next, performed a retrospective review of all patients diagnosed with prostate cancer in our hospital between January 2010 and December 2021. The inclusion criteria were as follows: (1) patients admitted to our hospital with a neck mass as the initial symptom and (2) the primary site was confirmed to be the prostate. There were no restrictions with regards to the department at which the patient first presented. The exclusion criteria were as follows: (1) prostate cancer had been diagnosed in another hospital prior to attendance at our hospital; (2) there was an incomplete set of patient follow-up records. The pathological findings of the prostate biopsies were the gold standard for diagnosing prostate cancer. And the source of the cervical lymph lodes was also confirmed by the pathological outcomes of the needle biopsy. In this research study, we identified 2,248 patients who had been diagnosed with prostate cancer. Of these patients, only five males presented with enlargement of the cervical lymph nodes as the initial manifestation of metastatic prostate cancer and written informed consent was obtained from the patient.
Of 2,248 patients, only five males presented with enlargement of the cervical lymph nodes as the initial manifestation of metastatic prostate cancer. The five patients were all transferred to the Urology Department from other clinics; four from Otorhinolaryngology and one from Oncology. The basic clinical details of these patients are given in Table 1. All five patients had cervical lymphadenopathy as the initial presentation. Four of these patients were referred to the hospital presenting with a palpable painless mass on the left cervical neck, while one patient showed bilateral neck enlargement in the lymph nodes. Mean age at the time of initial diagnosis was 65.4 ± 5.6 years. All of the patients except for case 2 denied any urinary complaints when they were firstly referred to our hospital due to cervical lymphadenopathy; case 2 reported that he found new onset gross painless hematuria, although this was not accompanied by frequent urination, urgency or pain. Case 3 had undergone bilateral partial thyroidectomy four years previously. Case 5 had undergone resection of a gastrointestinal villous tubular adenoma one year previously. The medical and family history of the other patients were unremarkable.
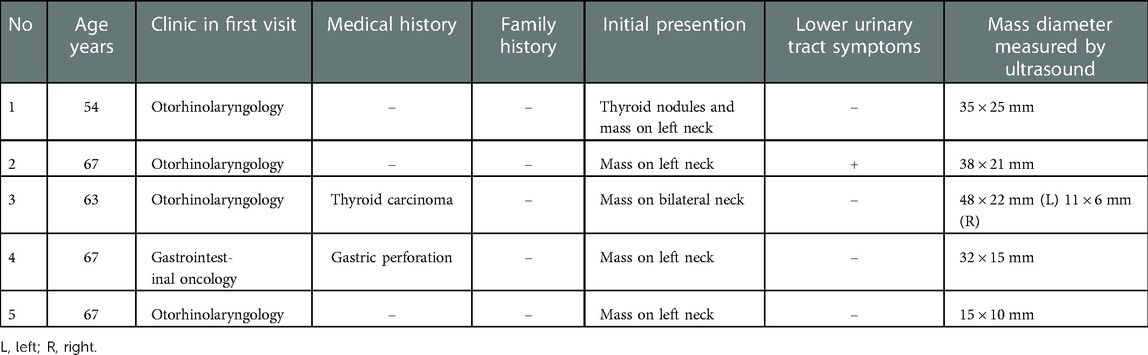
Table 1. The basic characteristics of patients with prostate carcinoma presenting with cervical lymphadenopathy.
All patients underwent regular physical and radiological examinations, although the initial diagnosis was based on the biopsy of suspicious lymph nodes or specific immunohistochemical stains. Immunohistochemical staining of the suspicious lymph nodes showed positive results for prostate-specific antigen (PSA) in all five cases, as shown in Table 2. Then, we examined tumor markers in an attempt to identify the primary lesion, thus revealing PSA level exceeding 100 ng/ml in all patients (Table 2). Except for one case that refused prostate biopsy, the remaining four patients all received ultrasound-guided transperineal treatment for prostate cancer. Pathological analysis revealed malignant prostate carcinoma; Gleason scores were 4 + 4 = 8 points, 5 + 4 = 9 points, 4 + 5 = 9 points, and 5 + 4 = 9 points, respectively. In addition, computer tomography (CT) scans of bone revealed multiple bone metastases in all five cases. CT of the chest, abdomen, and pelvis, were used to investigate the progression of local prostate tumors and the presence of systemic-organ metastases; none of the cases showed evidence of metastases in the distal organs. Furthermore, three cases underwent 18-FDG positron emission tomography computed tomography (PET CT) scans which revealed multiple lymph nodes metastases and multiple bone metastases that were not accompanied by visceral organ metastases.
The five cases were initially treated with hormonal therapy (as shown in Table 3). Cases 1, 2, 3, and 5 were administered with bicalutamide and goserelin, with zoledronic acid to relieve bone complications. Case 4 was treated directly with abiraterone and goserelin directly. The serum PSA of case 1 decreased to 9.03 ng/ml after seven months of treatment; the left neck mass was significantly smaller but more accessible than before. However, Case 1 experienced significant pain symptoms; CT scanning of the bones revealed the further progression of systematic bone metastases, thus leading to the possibility castration-resistant prostate cancer (CRPC). To control disease progression, Case 1 was treated with abiraterone, but eventually died 12 months after first diagnosis due to uncontrollable gastrointestinal bleeding.
Furthermore, the prognosis of case 2 was also poor. Due to economic reasons, the patient refused to implement further treatment options and died 6 months after the initial diagnosis. Case 3 had reported beneficial effects and follow-up checks revealed that the PSA level had fallen to 0.094 ng/Ml after three months of treatment. The cervical lymph nodes had disappeared after 4 months. However, Case 3 progressed to CRPC after 12 months and abiraterone was used for the next stage of treatment. Over 18 months follow-up, the patient remained asympomatic while receiving androgen blockade. Case 4 received abiraterone, prednisolone, and goserelin; clinical follow-up 3 months later revealed a PSA of 0.638 ng/ml; the enlarged cervical lymph node also disappeared after 6 months. The patient was followed up regularly with no progression or recurrence of cancer for 24 months (Figure 1). The prognosis of case 5 was even poorer; he died 8 months after the initial diagnosis. He was initially given goserelin and bicalutamide, with zoledronic acid to target bone metastases. However, five months later, he was re-referred to the hospital due to fever and an incomplete intestinal obstruction. Upon review, the serum PSA level was 32.35 ng/ml. He received antibiotics and gastrointestinal decompression treatment for fever and incomplete intestinal obstruction, For prostate cancer, the patient was given abiraterone, goserelin and zoledronic acid. After one month of treatment, the serum PSA had increased to 59.65 ng/ml. The patient underwent 18-F PSMA PET CT scanning again; results suggested a poor response to hormone therapy and revealed that the range of bone metastases had increased when compared to previous scans; the condition of the multiple lymph nodes was similar to when assessed previously. We also observed multiple newly formed nodules in both lungs, thus excluding the possibility of metastatic cancer. The patient died after two months (Figure 2).
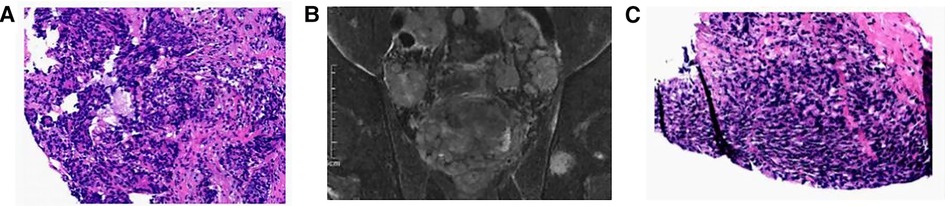
Figure 1. Case 4 (A) under the microscope, fine needle biopsy of the suspicious tissue revealed a large number of cancer cells with indistinct borders and finely granular cytoplasm. Pathology of left cervical lymph nodes revealed adenocarcinoma(HE*40). (B) Mp-MRI revealed prostate cancer. (C) Pathology of ultrasound-guided transperineal biopsy revealed malignant prostate carcinoma, Gleason score was 5 + 4 = 9 points(HE*40).
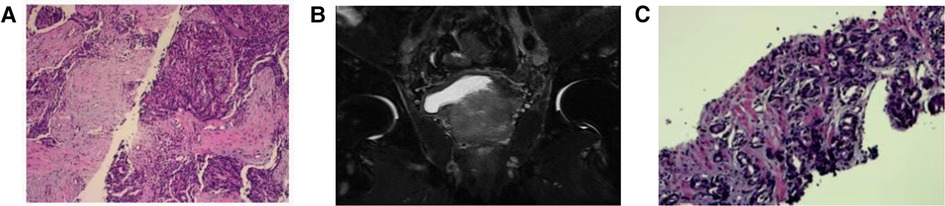
Figure 2. Case 5 (A) the left cervical lymph nodes biopsy revealed a poorly differentiated adenocarcinoma, which was considered to be based on the origin of the prostate, the immunohistochemical results were as follows: AE1/AE3(+), CK7(−), CK20(−), PSA(+), PsAP(+), NKX3.1(+), TTF1(+), TG(−), NapsinA(−), Villin(+), CDX2(−), Syn(−), CgA(−), CD56(−), Ki-67(+, 70%–80%)(HE*40). (B) Mp-MRI revealed prostate cancer. (C) Pathology of ultrasound-guided transperineal biopsy revealed malignant prostate carcinoma, Gleason score was 5 + 4 = 9 points(HE*40).
The most common metastatic sites for prostate cancer are the bones and regional lymph nodes, followed by the lungs, bladder, liver, and adrenal glands (3). Regional lymph node dissemination most frequently occurs to the obturator nodes, along with the perivesical, hypogastric, iliac, presacral, and para-aortic nodes (7). However, distal metastases of prostate cancer to the cervical lymph nodes are rare, especially when presenting as an initial symptom. Michael et al. studied approximately 6,000 patients diagnosed with prostate cancer between 1950 and 1968 at the Mayo Clinic and found that the incidence of prostate cancer metastases to supraclavicular lymph nodes, as an initial manifestation, was <0.1% (5/6000) (8), this was similar to the incidence we observed in our hospital (0.22%, 5/2248). James et al. reported 19 cases with supraclavicular lymph nodes as the initial presentation of metastatic prostate cancer (9). Our literature analysis revealed that a total of 58 cases have been reported from the 1970 s until now. Of these 58 cases, most cases of prostate cancer presented with supraclavicular lymphdenophaty involving left-side cervical lymphadenopathy; only seven patients reported have been reported with supraclavicular lymph nodes on the right side; three of these had simultaneous left cervical lymphadenopathy (9, 10–15). The youngest male reported was only 42 years-of-age (16); the oldest was 87 years-of-age (13). Of the 58 cases, 29 cases received PSA examinations; in each case, the PSA level was abnormal. Of these 29 cases, 26 patients had abnormal PSA levels that exceeded 100 ng/ml.This study not only reported 5 relevant cases, but also systematically summarized the diagnosis, clinical features and prognosis of all 58 patients previously reported in the relevant literature, aiming to improve the knowledge and understanding of these diseases.
The mechanism of metastasis to the supraclavicular lymph nodes remains unclear. A widely accepted theory states that the dissemination of lymph nodes could occur via step-wise progression (17). This process first occurs in the regional lymph nodes as obturator and pelvic lymph nodes, then moves through the retroperitoneal lymph nodes, cysterna chyli, and the thoracic duct, where the lymphatic system reunites with the systematic circulation at the left subclavian vein. Left cervical nodes are situated close to the entry of the thoracic duct into the left subclavian vein. Therefore, prostate cancer can spread to the left jugular trunk via retrograde spread, thus leading to the enlargement of cervical lymph node on the left side (18).
Metastases to the cervical lymph nodes mostly arise from primary cancer in the head and neck, such as the mucosa of the upper aerodigestive tract and the thyroid glands (8). Therefore, such patients are often first encountered in the head-neck surgery department or the otorhinolaryngology department, rather than urology; this may result in misdiagnosis. From reviewing the relevant literature, eight cases attended departments other than urology on their first hospital visit. These cases were referred from several other departments, including the emergency department (7, 19), oncology department (12, 19), internal medicine (13), thoracic surgery (18) and surgical outpatient clinic (15, 18). All five of our current cases were referred from from thyroid surgery and oncology. By summarizing these specific cases, it was evident that needle biopsy of suspicious masses and PSA immunohistochemistry staining were needed for clinicians to consider the prostate as the suspicious primary tumor site.
Hormonal treatment is still the main option for prostate cancer with clavicle lymph node metastasis. But the prognosis of such cases was generally poor. In the present study, only two patients are still alive, with most (60%) showing a poor response to maximal androgen blockade therapy before rapidly developing CRPC and dying after a short duration, which was similar to the previous study (20). Besides, Jones et al. reported 11 metastatic prostatic carcinoma cases presenting with left-sided cervical lymphadenopathy, the mean survival time was only 29.7 months (21). Surprisingly, Michael et al. reported a patient with metastatic cervical lymphadenopathy who was treated with diethylstilbestrol and survived for 12 years (8). Improving early screening for prostate cancer allows earlier detection and treatment of prostate cancer, which may be extremely important to ameliorate the prognosis of such patients. Previous relevant studies have shown that the occurrence of distant lymph nodes metastases is an independent risk factor for poor prognosis of prostate cancer (22), From the data of the study we obtained, it is clear that all patients were already in a state of distant lymph node metastases at the time of initial diagnosis. Therefore, regular serum PSA tests and urological ultrasonography detection are important way to achieve early screening for prostate cancer. Besides, There are some limitations in this study. First of all, this is a single-center retrospective study, which may not reflect the true incidence rate. Secondly, the mechanism of metastasis to the left cervical lymph nodes is not mentioned in the article.
In conclusion, any elderly male patients presenting with an asymptomatic cervical mass as the initial presentation should be considered the possibility of prostate cancer. Needle biopsy and immunohistochemical staining of lymphatic biopsies, and the determination of serum PSA levels are vital for final diagnosis. The overall prognosis of such cases is generally poor, and hormonal therapy including abiraterone may be beneficial.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identififiable images or data included in this article. Informed written consent was obtained from the patient for publication of this report and any accompanying images.
All authors were involved in the writing, reviewing, and editing of the manuscript. And all authors have read and agreed to the published version of the manuscript. All authors contributed to the article and approved the submitted version.
This research was supported by the National Science Foundation (Reference No. 213 81772739)
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Salmon C, Song L, Muir K, et al. Marital status and prostate cancer incidence: a pooled analysis of 12 case-control studies from the PRACTICAL consortium. Eur J Epidemiol. (2021) 36(9):913–25. doi: 10.1007/s10654-021-00781-1
2. Gandaglia G, Leni R, Bray F, et al. Epidemiology and prevention of prostate cancer. Eur Urol Oncol. (2021) 4(6):877–92. doi: 10.1016/j.euo.2021.09.006
3. Rybalova I, Kirsch CFE, Choe SK, et al. Metastatic prostate cancer presenting with hoarseness. Grand Rounds— Oncol Ear Nose Throat. (2005) 5:28–33.
4. Mremi A, Mbwambo OJ, Bright F, et al. Left axillary lymphadenopathy as initial presentation of metastatic prostate cancer: a rare case report. Int J Surg Case Rep. (2021) 82:105889. doi: 10.1016/j.ijscr.2021.105889
5. Albadri ST, Salomão D. Metastatic prostate adenocarcinoma to cervical lymph nodes: an unusual diagnosis on fine-needle aspiration biopsy. J Am Soc Cytopathol. (2021) 10(2):231–8. doi: 10.1016/j.jasc.2020.08.009
6. Dattani SMT, Yamada ML, Dhoot NM, et al. Metastatic prostate cancer presenting as incidental pelvic lymphadenopathy—a report of three cases with literature review. Radiol Case Rep. (2022) 17(6):2247–52. doi: 10.1016/j.radcr.2022.03.053
7. Sehrawat A, Gupta S, Alok T. Prostatic adenocarcinoma incognito manifestation as generalized lymphadenopathy: a rare case report. Indian J Surg Oncol. (2017) 8:91–3. doi: 10.1007/s13193-016-0558-5
8. Warren MM, Furlow WL. Carcinoma of the prostate presenting as a mass in the neck. JAMA. (1970) 213:620–1. doi: 10.1001/jama.1970.03170300064019
9. Butler JJ, Howe CD, Johnson DE. Enlargement of the supraclavicular lymph nodes as the initial sign of prostatic carcinoma. Cancer. (1971) 27:1055–63. 10.1002/1097-0142(197105)27:5<1055::aid-cncr2820270509>3.0.co;2-t5581507
10. Wang H, Chiang PH, Peng JP, et al. Presentation of prostate carcinoma with cervical lymphadenopathy: report of three cases. Chang Gung Med J. (2004) 27:840–4.15796261
11. Ozgür A, Ilker Y, Türkeri LN. Cervical lymph node enlargement on the right side as the initial manifestation of metastatic prostate cancer. Arch Esp Urol. (2003) 56:859–61.
12. Hsieh KH, Tan H, Ching G, Chong PA, et al. Metastatic prostate adenocarcinoma presenting as a large right supraclavicular and anterior chest wall mass. BMJ Case Rep. (2016) 2016. doi: 10.1136/bcr-2016-214797
13. Sepúlveda L, Gorgal T, Pires V, et al. Prostate cancer metastatic to the cervical lymph nodes. Case Rep Urol. (2015) 2015:263978. doi: 10.1155/2015/263978
14. Elabbady A, Kotb AF. Unusual presentations of prostate cancer: a review and case reports. Arab J Urol. (2013) 11:48–53. doi: 10.1016/j.aju.2012.10.002
15. Ahamed SH, Agarwal AK, Raju PPJ. Metastatic prostate carcinoma presenting as supraclavicular lymphadenopathy—is it unusual? Ann R Coll Surg Engl. (2006) 88:W4–5. doi: 10.1308/147870806X129278
16. Lin YY, Lin DS, Kang BH, et al. Neck mass as the first presentation of metastatic prostatic adenocarcinoma. J Chin Med Assoc. (2011) 74:570–3. doi: 10.1016/j.jcma.2011.09.012
17. Dubhashi SP, Kumar H, et al. Prostate cancer presenting as cervical lymphadenopathy. Am J Case Rep. (2012) 13:206–8. doi: 10.12659/AJCR.883334
18. Chan G, Domes T. Supraclavicular lymphadenopathy as the initial presentation of metastatic prostate cancer: a case report and review of literature. Can Urol Assoc J. (2013) 7:E433–5. doi: 10.5489/cuaj.1385
19. Davarci M, Gokce A, Guven EO, et al. Metastatic prostate adenocarcinoma presenting as supraclavicular lymphadenopathy: a report of two cases. Contemp Oncol (Pozn). (2012) 16:53–5. doi: 10.5114/wo.2012.27337
20. Carleton J, van der RP, Dahm P. Metastatic prostate cancer presenting as an asymptomatic neck mass. Prostate Cancer Prostatic Dis. (2005) 8:293–5; discussion 295. doi: 10.1038/sj.pcan.4500805
21. Jones H, Anthony PP. Metastatic prostatic carcinoma presenting as left-sided cervical lymphadenopathy: a series of 11 cases. Histopathology. (1992) 21:149–54. doi: 10.1111/j.1365-2559.1992.tb00363.x
Keywords: metastatic prostate cancer, supraclavicular lymphadenopathy, cervical lymphadenopathy, cervical lymph nodes, case report
Citation: Liu Y, Dai Z, Hao J, Wang L and Liu Z (2023) Cervical lymphadenopathy as initial presentation of metastatic prostate cancer: A retrospective study of five cases and literature review. Front. Surg. 10:1081951. doi: 10.3389/fsurg.2023.1081951
Received: 27 October 2022; Accepted: 10 January 2023;
Published: 30 January 2023.
Edited by:
Sabine Brookman-May, Ludwig Maximilian University of Munich, Germany© 2023 Liu, Dai, Hao, Wang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhiyu Liu bHp5ZG9jdEAxNjMuY29t Liang Wang d2FuZ2xkb2N0QDE2My5jb20=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.