- 1Departments of Gastrointestinal Colorectal Anus Surgery, China-Japan Union Hospital, Jilin University, Changchun, China
- 2Departments of Orthopedics Surgery, China-Japan Union Hospital, Jilin University, Changchun, China
Background: Cystic lymphangioma is a rare benign tumor of the lymphatic system, which is most commonly observed in the neck, head and armpit.Less than 5% of lymphangiomas occur in the abdominal cavity and even less in the retroperitoneum.
Case description: A 65-year-old male patient was diagnosed with an “abdominal mass that had persisted for 1 year, accompanied by abdominal pain, abdominal distension and dyspnea for 7 days”. After abdominal computerd tomography, a giant multilobed abdominal lymphangioma was suspected, which squeezed the intestinal canal and was closely related to the inferior vena cava. The patient underwent an exploratory laparotomy, during which, it was found that the tumor formed extensive adhesions to the transverse colon, small intestine and pelvic wall, and enveloped the abdominal aorta, superior mesenteric artery, inferior mesenteric artery and inferior vena cava to varying degrees. It was diffcult to remove the cyst completely. Postoperative pathology confirmed the diagnosis of retroperitoneal cystic lymphangioma. The patient recovered well after the operation, was eating normally by 5 days postoperatively,and was discharged 10 days postoperatively.The patient was followed up 1 month after postoperatively and no evidence of recurrence was observed.
Conclusion: In this case, we report a patient with giant retroperitoneal cystic lymphangioma who underwent exploratory laparotomy combined with preoperative abdominal computerd tomography and acute abdominal pain, abdominal distension and dyspnea. Because of the large volume of the tumor and its close relationship with the superior mesenteric artery and other blood vessels, the surgeon used scissors to separate the tumor sharply and removed the whole tumor completely.
Introduction
Cystic lymphangioma is a non-cancerous vascular malformed conjunctival tumor consisting of thin-walled cysts. It is a rare benign tumor, which is most commonly observed in the neck, head,and armpit, while >5% of lymphangiomas occur in the abdominal cavity, including the mesentery and the greater omentum.The occurrence in the retroperitoneum is even rarer. Although cystic lymphangioma can occur at any age, it is mainly observed in children, in whom the prognosis is good (1, 2). In adults, cystic lymphangiomas account for approximately 7% of abdominal cysts (3). Retroperitoneal cystic lymphangioma is usually asymptomatic, but in some cases it is characterized by acute abdominal pain and distension caused by nausea, vomiting or intestinal obstruction. The tumor can be identified by imaging examinations such as ultrasound and computed tomography (CT), however histopathological examination remains the gold standard. Complete surgical resection of the tumor is the first choice for treatment (4–6). Here, we report the clinical features, diagnosis, treatment and prognosis of a giant retroperitoneal cystic lymphangioma in a 63-year-old male patient. And this study is in accordance with the principles of CARE guidelines (7).
Case description
The patient, a 65-year-old man, was diagnosed with abdominal swelling that had persisted for 1 year,and was accompanied by abdominal pain, abdominal distension and dyspnea for 7 days. A year prior, the patient found an"abdominal cystic mass (approximately 25 cm × 1.6 cm × 22 cm)” and attended an other hospital. He was admitted to the local hospital 7days prior due to sudden intermittent diffuse abdominal pain with abdominal distension, dyspnea, no fever, nausea, and vomiting. Abdominal CT suggested an “abdominal mass and intestinal obstruction”, and the symptoms did not improve. The patient was admitted to the hospital for further diagnosis and treatment. The patient had had hypertension for 10 years and regularly took levamlodipine besylate tablets for 5 mg/days,which controlled his blood pressure within the normal range. A cardiac stent operation was performed 4 months prior because of myocardial infarction. Physical examination showed: no obvious heart abnormalities,although shortness of breath, obvious abdominal swelling, frog belly, no gastrointestinal type and peristaltic wave were noted,as well as a large mass that could be felt asoccupying most of the abdominal cavity. Regarding tumor markers: CA125:65.47 U/ml (reference value < 35 U/ml), other tumor markers were not abnormal. Abdominal enhanced CT: huge cystic space in the pelvis and abdominal cavity, with an irregular shape, linear septum, (approximately 24.2 cm × 16.7 cm × 27.8 cm), extending along the mesentery of the small intestine (Figures 1A–D). In contrast-enhanced scan, the cystic components were not enhanced, the septum was uniformly enhanced, the intestinal canal was displaced laterally under pressure (Figures 1A, Magi B), and the inferior vena cava was narrowed (Figure 1C). The preliminary diagnosis of the nature of abdominal mass pending diagnosis: cystic lymphangioma? An exploratory laparotomy was performed,during which a large cystic mass of approxmately 30 × 28 × 14 cm was observed retroperitoneally. The surface of the mass was smooth, white and red, with a light yellow exudate on the surface. The tumor formed extensive adhesion with the transverse colon, small intestine and pelvic wall, and enveloped the abdominal aorta, superior mesenteric artery, inferior mesenteric artery and inferior vena cava to varying degrees. We decided to surgically remove the cystic mass completely (Figure 2). Postoperative pathology: microscopically, necrosis and protein exudation in the cystic cavity, chronic inflammation with inflammatory granulation, obvious proliferation of interstitial vessels and fibrous tissue, scattered in clusters of smooth muscle bundles and more inflammatory cells, and occasional giant cells, as well as proliferation of small lymphatic vessels outside the cyst wall, consistent with cystic lymphangioma with chronic inflammation (Figures 3A,B).
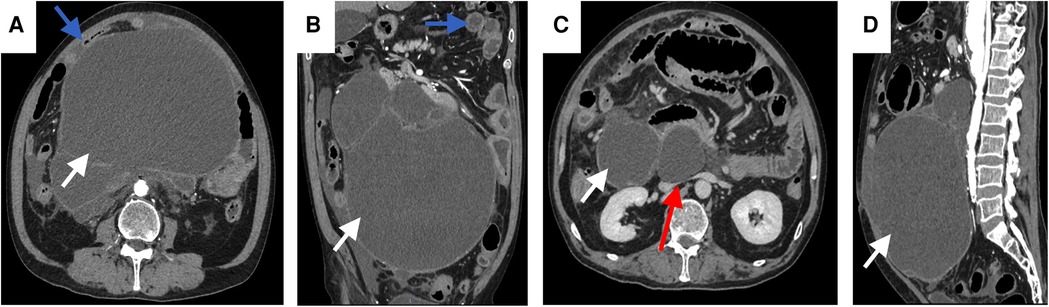
Figure 1. Abdominal enhanced CT axial arterial phase (A), coronary arterial phase (B), axial venous phase (C),and sagittal arterial phase (D) CT images show a retroperitoneal cystic mass (white solid arrow), extending along the mesentery to 24 cm. The tumor oppresses the surrounding intestine (blue solid arrow) and the inferior vena cava (B) (red solid arrow).
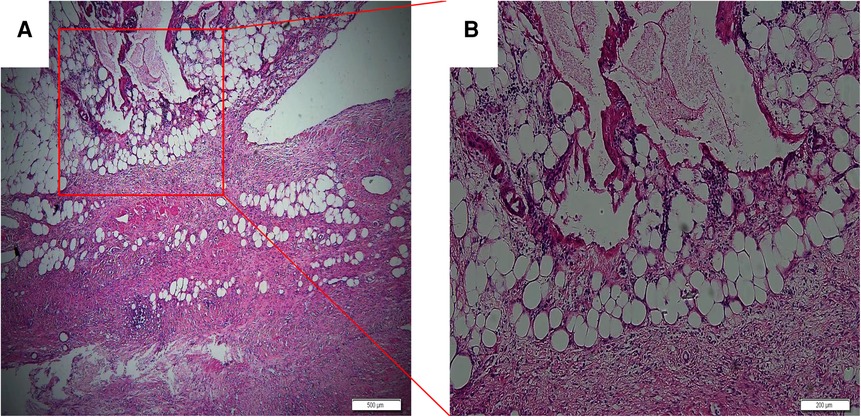
Figure 3. Necrosis and protein exudation in the cystic cavity, obvious proliferation of interstitial vessels and fibrous tissue, cystic lymphatic cavities of different sizes with inflammatory lymphocyte infiltration and lymphoid nodules; (A) hematoxylin and eosin (HE) × 40, scale 500 μm; (B) HE × 100, scale 200 μm.
The patient recovered well and could eat normally 5 days postoperatively. The patient was discharged 10 days after the surgery,at which point,he was in a good condition, with no pain or complications. In the initial recovery stage, he was advised to ingest high-quality protein that was easily absorbed and high in nutrition,and to avoid high-fat, high-fiber, indigestible and absorbed food, The patient was subjected to, regular re-examination and follow-up.
Discussion
Cystic lymphangioma usually occurs in the head, neck and armpit, mostly in children, with no sex-related difference in incidence. Intraperitoneal lymphangioma is a rare intra-abdominal tumor. Less than 5% of lymphangiomas occur in the abdominal cavity, and the incidence of retroperitoneal tumors is even lower (1, 2). The etiology of cystic lymphangioma is unclear, and infection, lymphatic obstruction and surgery may be associated factors (8). According to the histological type, cystic lymphangioma can be divided into cystic, capillary and cavernous.Likewise, based on its clinical manifestations, it can be divided into macrocytic, microencapsulated, and mixed cysts. Microcapsules can be further subdivided into developing-cell microcapsules and closed-cell microcapsules based on whether the cells are open or not (9).Here, we report a case of retroperitoneal giant cyst lymphangioma, which is consistent with other reports suggesting that the most common retroperitoneal lymphangioma is cystic type (10).
The clinical manifestations of retroperitoneal cystic lymphangioma are non specific and are related to the size and location of the tumor and the location of the surrounding tissues and organs, which makes diagnosis challenging. Initially, the tumor is small but asymptomatic; with the growth of the tumor, nausea, vomiting, abdominal pain and abdominal distension may occur due to compression of the abdominal organs, and in severe cases, acute abdominal pain and intestinal obstruction may even cause rupture, infection, bleeding and torsion of related organs and tissues (11–13). In the current case, abdominal contrast-enhanced CT showed a huge retroperitoneal cystic mass, which occupied most of the abdominal cavity and pelvic cavity and squeezed the small intestine, resulting in abdominal pain, abdominal distension, dyspnea and other symptoms, and was admitted as “abdominal mass, intestinal obstruction”. Cystic lymphangioma should be differentiated from abdominal lymphoma, mesenteric cyst, secondary metastasis of a malignant tumor, tuberculosis, echinococcosis, small intestinal adenocarcinoma and mesenteric related tumors (14). Imaging examination plays an important role in the diagnosis of retroperitoneal cystic lymphangioma. Ultrasound has a unique advantage in showing the size, location, content and boundary of the cyst. However, when there is hemorrhage and necrosis in the capsule, the echo of the contents will produce some changes, which will affect the judgment. Abdominal enhanced CT is the first choice.Abdominal enhanced CT can be used to observe the density of the tumor to determine the relationship with the surrounding tissue, blood vessels and organs, which can distinguish retroperitoneal lymphangioma from intraperitoneal lymphangioma. Magnetic resonance(MRI) is more sensitive in showing intra-cyst bleeding and content (15–17). However, a final diagnosis still requires pathological biopsy, which is characterized by abnormally dilated lymphatic vessels lined with flat endothelial cells with smooth muscle, blood vessels, fat and lymphatic matrix (18). CT was considered as cystic lymphangioma, and the final diagnosis was confirmed by postoperative pathology.
Without intervention, the volume of cystic lymphangioma will gradually increase, thus oppressing adjacent tissues, blood vessels, nerves, organs and so on, resulting in related complications (19). In our case, the volume increased by about 13 times over a year, leading to the occurrence of this symptom. Surgical resection of tumor is the first choice for the treatment of retroperitoneal lymphangioma. during the operation, attention should be paid to the relationship between tumor and surrounding tissue, blood vessels, nerves and organs, so as to remove the tumor completely and reduce the postoperative recurrence rate (20, 21). Recently some methods of nonsurgical treatment have emerged. Among them, sclerotherapy is the most commonly used alternative therapy for lymphangiomas that cannot be completely resected or diagnosed as difficult to operate. When compared with surgical resection, sclerotherapy has the advantages of being simple and causing less injury. Besides, several studies have reported that sclerosing agents can effectively treat large cystic lymphangioma, even though their curative effect on microcystic lymphangioma is much lower (22–24). Examples of such common hardeners include OK-432, doxycycline, bleomycin, and ethanol. Notably, OK-432 sclerotherapy can not only induce and activate leukocytes to produce cytokines, which in turn increase endothelial cell permeability, accelerate the speed and flow of lymphatic drainage, and facilitate lymphangioma cystic cavity shrinkage and lesion regression, but also reduce complications and focal fibrosis, making it a promising alternative to surgery, especially for patients with microcystic lymphangioma (25, 26). However, sclerotherapy has been reported to cause some adverse reactions, such as airway obstruction and skin necrosis. Therefore, the effectiveness of sclerotherapy needs to be further evaluated (27, 28). Another notable method is radiofrequency ablation, which destroys diseased tissues at low temperatures while causing less damage to the surrounding tissues. Presently, radiofrequency ablation is the first choice of treatment for treating oral and pharynx microcystic lymphangioma (29, 30). Some studies have also shown that radiofrequency ablation is an effective method for the treatment of superficial microcystic lymphangioma; however, further development and research are needed to better apply it for the treatment of microcystic lymphangioma found in other body parts.
Although the above-mentioned methods have greatly helped in the treatment of lymphangioma, clinicians still find it difficult to obtain optimal results for lymphangiomas with large lesion areas and invasive growth. Importantly, recent studies have shown the efficacy of several drugs in the treatment of lymphangioma, and some of these drugs have been used in treating patients with lymphangiomas, such as sildenafil, propranolol,sirolimus, and several inhibitors targeting the PI3K/AKT/mTOR signaling pathway (PI3K inhibitors, AKT inhibitors, MAPK inhibitors, sorafenib, etc.) (31, 32). However, some studies have demonstrated that sildenafil is not effective in the treatment of microcystic lymphangioma, whereas sirolimus has been demonstrated to have good efficacy in the treatment of microcystic lymphangioma and may become the focus of future research. In addition, studies have also shown that BMP and Wnt modulators, calcium channel blockers, and KATP activators (minoxidil) may also have some therapeutic potential (33).
Since a single treatment cannot achieve satisfactory results, clinicians are encouraged to use multiple methods of combined therapy. Consequently, surgical resection, as the main treatment, can be used to remove a significant volume of large cystic lesions, while the remaining diseased tissues can be treated with sclerotherapy. For instance, bleomycin is currently used in the treatment of residual small cystic diseases and has achieved some efficacy (34). However, sometimes lymphangiomas may require several rounds of sclerotherapy. For tumors that are large or widely enclosed and have invaded their surrounding tissues, blood vessels, and nerves, drugs or sclerotherapy can be taken first to reduce the size of the lesions before resecting them through surgery. Alternatively, postoperative sclerotherapy, drugs, radiofrequency ablation, and other combined therapy can be used. Unfortunately, there are currently no unified guidelines for the diagnosis and treatment of lymphangiomas, and further verification is still needed.
We provided a case report and on the basis of literature review, retroperitoneal cystic lymphangioma was investigated.PubMed was searched using these key words: (“Lymphangioma, Cystic” or “Cystic Lymphangioma” or “Cystic Lymphangiomas” or “Lymphangiomas, Cystic” or “Hygroma” or “Hygromas, Cystic” or “Cystic Hygroma Colli” or “Colli, Cystic Hygroma” or “Hygroma Colli, Cystic” or “Hygroma” or “Hygromas”) and (“Retroperitoneal Space” or “Retroperitoneal Neoplasms” or “Retroperitoneal Fibrosis”). Key words referred to medical subject heading (MeSH). And the search terms used on PubMed were: (([“Lymphangioma, Cystic"(Mesh)] OR ((((((((((([Cystic Lymphangioma(Title/Abstract)] OR [Cystic Lymphangiomas(Title/Abstract)]) OR [Lymphangiomas, Cystic(Title/Abstract)]) OR [Hygroma, Cystic(Title/Abstract)]) OR [Cystic Hygroma(Title/Abstract)]) OR [Cystic Hygromas(Title/Abstract)]) OR [Hygromas, Cystic(Title/Abstract)]) OR [Cystic Hygroma Colli(Title/Abstract)]) OR [Colli, Cystic Hygroma(Title/Abstract)]) OR [Hygroma Colli, Cystic(Title/Abstract)]) OR [Hygroma(Title/Abstract)]) OR [Hygromas(Title/Abstract)]))) AND ([Retroperitoneal(Title/Abstract)] OR ((([“ Retroperitoneal Space"(Mesh)] OR “Retroperitoneal Neoplasms"[Mesh]) OR “Retroperitoneal Fibrosis"[Mesh]))).
We systematically reviewed the studies returned from the literature searches.The inclusion criteria were as follows: (I) retroperitoneal cystic lymphangioma; (II) over 18 years old; (III) full text; (IV) manuscripts written in English. Studies were excluded for any of the following: (I) the study was a review, meeting abstract, non-clinical study, or in vitro study; (II) inferior quality literature or with insufficient outcome indicators; (III) The lesion is not retroperitoneal. Each abstract is carefully reviewed by two different authors (SS and DS). We conducted a systematic review of 240 records and finally included 29 articles involving 34 cases. Detailed characteristics of the reported cases are provided in supplemental (Table 1) (35–63). We made the statistics on the above date.There were 21 males and 13 females, aged from 25 to 76 years old, with an average age of 45.82 years old. 25 cases underwent laparotomy and 9 cases underwent laparoscopic surgery. The average diameter of tumor was 13.44 cm. Among the 34 patients, 1 case had postoperative complications, 20 cases had no postoperative complications, and the other 14 cases had no related data.
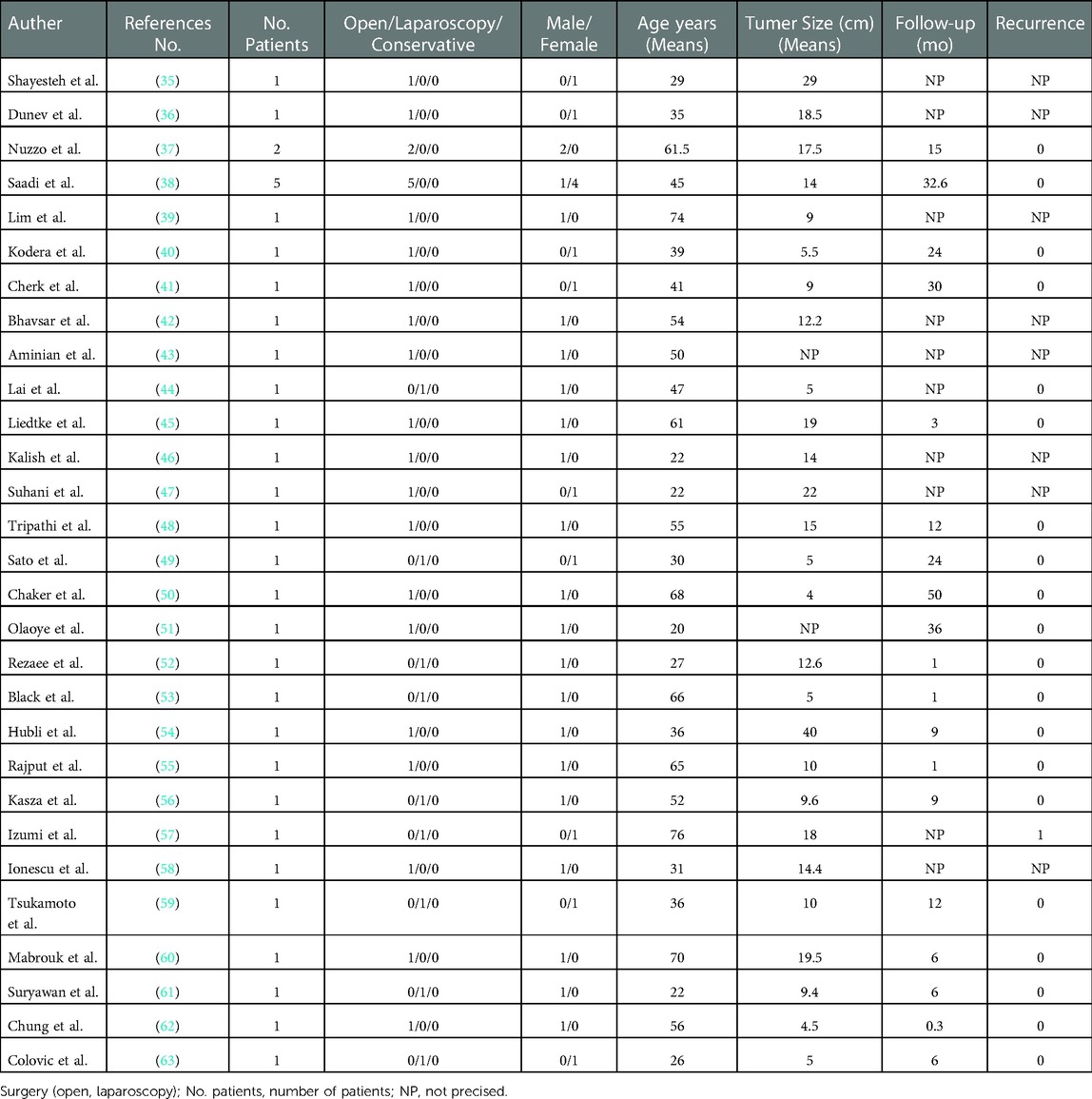
Table 1. Characteristics of the adult cases of retroperitoneal cystic lymphangioma reported in the literature.
Compared with the case reports in the existing literature, our case was first found during the physical examination a year ago, and the patient himself did not have obvious symptoms of discomfort, so there was no follow-up treatment. Preoperative abdominal contrast-enhanced CT showed that the case was a huge retroperitoneal cystic mass of approximately 24.2 cm × 16.7 cm × 27.8 cm. Up to the lower edge of the pancreas, down to the peritoneal reflex, left and right to the two abdominal walls, anterior to the anterior abdominal wall, and back to the front of the spinal lamina, occupying most of the abdominal cavity and pelvic cavity, squeezing the small intestine and oppressing the inferior vena cava. The nature can not be clear, consider the possibility of benign, but do not rule out the possibility of malignant. This time, due to the increase in the size of the cyst, it oppresses the surrounding intestines, causing the diaphragm to move upward, and some cysts rupture and bleeding, which irritates the intestinal tract, resulting in acute abdominal pain, abdominal distension, intestinal obstruction and dyspnea. Because of the critical condition, we decided to carry out exploratory laparotomy. During the operation, a huge retroperitoneal cystic mass was seen, which almost occupied the whole abdominal cavity and pelvic cavity. We found that the tumor was closely wrapped and adhered to the abdominal aorta, superior mesenteric artery, inferior mesenteric artery, inferior vena cava and other blood vessels, and pressed the surrounding intestinal lumen. Part of the tumor ruptured and bleeding could be seen on the surface. As the nature of the tumor was not clear, we decided to remove the tumor as completely as possible. The surgeon uses scissors to separate carefully and sharply to minimize the rupture and bleeding of the tumor and blood vessels. Accurate and meticulous operation during sharp separation of enclosing and adherent blood vessels to reduce the risk of hemorrhagic shock. When the tumor is completely removed, it is removed slowly to avoid sharp fluctuations in blood pressure. The patient recovered well after operation and was discharged smoothly 10 days later.
However, there are still some areas that need to be improved in our program. for example, in this operation, we can first extract the contents of the cyst to reduce the volume of the tumor, reduce the difficulty of the operation, and shorten the duration of the operation. it may make the patient recover faster and better. Secondly, we only use a single surgical resection, sometimes can not achieve satisfactory results, we should use a variety of methods combined treatment, surgical resection as the main treatment, and the remaining lesions can be treated with sclerotherapy. in addition, for invasive and recurrent people, targeted therapy is also essential.
The purpose of this case is to share our process of diagnosis and treatment of this rare abdominal cystic mass, and to provide some help for relevant people, institutions and fields, but the combined treatment of cystic lymphangioma is still lack of unified understanding. we still need to further explore.
Conclusion
In this case, we report a patient with giant retroperitoneal cystic lymphangioma who underwent exploratory laparotomy combined with preoperative abdominal CT and acute abdominal pain, abdominal distension and dyspnea. Because of the large volume of the tumor and its close relationship with the superior mesenteric artery and other blood vessels, the surgeon used scissors to separate the tumor sharply and removed the whole tumor completely.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SS, BS and DS: contributed to the conception and design of the study. SS and CL: contributed to drafting the article. DS and YF: contributed to revising the article critically. All authors contributed to the article and approved the submitted version.
Acknowledgments
We are grateful to the coauthors for the rereading of the article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. de Perrot M, Rostan O, Morel P, Le Coultre C. Abdominal lymphangioma in adults and children. Br J Surg. (1998) 85:395–7. doi: 10.1046/j.1365-2168.1998.00628.x
2. Koenig TR, Loyer EM, Whitman GJ, Raymond AK, Charnsangavej C. Cystic lymphangioma of the pancreas. AJR Am J Roentgenol. (2001) 177:1090. doi: 10.2214/ajr.177.5.1771090
3. Hauser H, Mischinger HJ, Beham A, Berger A, Cerwenka H, Razmara J, et al. Cystic retroperitoneal lymphangiomas in adults. Eur J Surg Oncol. (1997) 23:322–6. doi: 10.1016/s0748-7983(97)90777-0
4. Thiam O, Faye PM, Niasse A, Seye Y, Gueye ML, Sarr IS, et al. Cystic mesenteric lymphangioma: a case report. Int J Surg Case Rep. (2019) 61:318–21. doi: 10.1016/j.ijscr.2019.07.051
5. Alfadhel SF, Alghamdi AA, Alzahrani SA. Ileal volvulus secondary to cystic lymphangioma: a rare case report with a literature review. Avicenna J Med. (2019) 9:82–5. doi: 10.4103/ajm.AJM_203_18
6. Cupido BD, Low G. Incidental cystic lymphangioma of the small bowel mesentery. J Clin Imaging Sci. (2015) 5:55. doi: 10.4103/2156-7514.166358
7. Riley DS, Barber MS, Kienle GS, Aronson JK, von Schoen-Angerer T, Tugwell P, et al. CARE Guidelines for case reports: explanation and elaboration document. J Clin Epidemiol. (2017) 89:218–35. doi: 10.1016/j.jclinepi.2017.04.026
8. Kogo H, Matsumoto S, Uchida E. Single-port laparoscopic-assisted resection for a large abdominal cystic lymphangioma: a case report. Surg Case Rep. (2018) 4:92. doi: 10.1186/s40792-018-0501-9
9. Dubois J, Thomas-Chaussé F, Soulez G. Common (cystic) lymphatic malformations: current knowledge and management. Tech Vasc Interv Radiol. (2019) 22:100631. doi: 10.1016/j.tvir.2019.100631
10. Gachabayov M, Kubachev K, Abdullaev E, Babyshin V, Neronov D, Abdullaev A. A huge cystic retroperitoneal lymphangioma presenting with back pain. Case Rep Med. (2016) 2016:1618393. doi: 10.1155/2016/1618393
11. Yagmur Y, Akbulut S, Gumus S, Babur M, Can MA. Case report of four different primary mesenteric neoplasms and review of literature. Iran Red Crescent Med J. (2016) 18:e28920. doi: 10.5812/ircmj.28920
12. Wei MY, Chua J, Cheng Y, Grossberg P. Small bowel volvulus in an adult with mesenteric lymphangioma and ascariasis. ANZ J Surg. (2018) 88:E859–60. doi: 10.1111/ans.13953
13. Tian C, Zheng Y, Ren X, Li B. A giant abdominal cystic tumour: mesentery cystic lymphangioma. Dig Liver Dis. (2015) 47:816–7. doi: 10.1016/j.dld.2015.05.008
14. Nagano H, Kimura T, Iida A, Togawa T, Goi T, Sato Y. Cystic lymphangioma in the peripheral jejunal mesentery in an adult and excision with laparoscopic-assisted surgery: a case report. World J Surg Oncol. (2019) 17:170. doi: 10.1186/s12957-019-1713-6
15. Hitzerd E, van Hamont D, Pijnenborg JM. Mesenteric lymphangioma mimicking a cystic ovarian mass on imaging. BMJ Case Rep. (2016) 2016:bcr2015213727. doi: 10.1136/bcr-2015-213727
16. Xu X, Zheng C, He X, Zhao Y, Hong T. Gastrointestinal: giant mesenteric cystic lymphangioma. J Gastroenterol Hepatol. (2017) 32:290. doi: 10.1111/jgh.13542
17. Lui SA, Nyo YL, Mali VP. Ileal cystic lymphangioma presenting with acute appendicitis. J Indian Assoc Pediatr Surg. (2018) 23:36–8. doi: 10.4103/jiaps.JIAPS_44_17
18. Okamoto D, Ishigami K, Yoshimitsu K, Irie H, Tajima T, Nishie A, et al. Hemorrhagic mesenteric cystic lymphangioma presenting with acute lower abdominal pain: the diagnostic clues on MR imaging. Emerg Radiol. (2009) 16:327–30. doi: 10.1007/s10140-008-0747-9
19. Zoguéreh DD, N'Tarundenga U, Provendier B, Gazaigne J. A giant retroperitoneal mass in adult. Rev Med Interne. (2003) 24:202–3. doi: 10.1016/s0248-8663(02)00810-x
20. Colbert SD, Seager L, Haider F, Evans BT, Anand R, Brennan PA. Lymphatic malformations of the head and neck-current concepts in management. Br J Oral Maxillofac Surg. (2013) 51:98–102. doi: 10.1016/j.bjoms.2011.12.016
21. Okazaki T, Iwatani S, Yanai T, Kobayashi H, Kato Y, Marusasa T, et al. Treatment of lymphangioma in children: our experience of 128 cases. J Pediatr Surg. (2007) 42:386–9. doi: 10.1016/j.jpedsurg.2006.10.012
22. Leung M, Leung L, Fung D, Poon WL, Liu C, Chung K, et al. Management of the low-flow head and neck vascular malformations in children: the sclerotherapy protocol. Eur J Pediatr Surg. (2014) 24:97–101. doi: 10.1055/s-0033-1354585
23. Farnoosh S, Don D, Koempel J, Panossian A, Anselmo D, Stanley P. Efficacy of doxycycline and sodium tetradecyl sulfate sclerotherapy in pediatric head and neck lymphatic malformations. Int J Pediatr Otorhinolaryngol. (2015) 79:883–7. doi: 10.1016/j.ijporl.2015.03.024
24. Acevedo JL, Shah RK, Brietzke SE. Nonsurgical therapies for lymphangiomas: a systematic review. Otolaryngol Head Neck Surg. (2008) 138:418–24. doi: 10.1016/j.otohns.2007.11.018
25. Jamal N, Ahmed S, Miller T, Bent J, Brook A, Parikh S, et al. Doxycycline sclerotherapy for pediatric head and neck macrocystic lymphatic malformations: a case series and review of the literature. Int J Pediatr Otorhinolaryngol. (2012) 76:1127–31. doi: 10.1016/j.ijporl.2012.04.015
26. Bagrodia N, Defnet AM, Kandel JJ. Management of lymphatic malformations in children. Curr Opin Pediatr. (2015) 27:356–63. doi: 10.1097/MOP.0000000000000209
27. Reismann M, Ghaffarpour N, Luvall E, Jirmo AC, Winqvist O, Radtke J, et al. Dynamic toll-like receptor expression predicts outcome of sclerotherapy for lymphatic malformations with OK-432 in children. J Surg Res. (2014) 187:197–201. doi: 10.1016/j.jss.2013.09.037
28. Ardıçlı B, Karnak İ, Çiftçi AÖ, Tanyel FC, Şenocak ME. Sclerotherapy with bleomycin versus surgical excision for extracervical cystic lymphatic malformations in children. Surg Today. (2016) 46:97–101. doi: 10.1007/s00595-015-1128-0
29. Thottam PJ, Al-Barazi R, Madgy DN, Rozzelle A. Submucosal resection of a microcystic oropharyngeal lymphatic malformation using radiofrequency ablation. Int J Pediatr Otorhinolaryngol. (2013) 77:1589–92. doi: 10.1016/j.ijporl.2013.05.037
30. Ryu NG, Park SK, Jeong HS. Low power radiofrequency ablation for symptomatic microcystic lymphatic malformation of the tongue. Int J Pediatr Otorhinolaryngol. (2008) 72:1731–4. doi: 10.1016/j.ijporl.2008.08.003
31. Blesinger H, Kaulfuß S, Aung T, Schwoch S, Prantl L, Rößler J, et al. PIK3CA Mutations are specifically localized to lymphatic endothelial cells of lymphatic malformations. PLoS One. (2018) 13:e0200343. doi: 10.1371/journal.pone.0200343
32. Boscolo E, Pastura P, Glaser K, Goines J, Hammill AM, Adams DM, et al. Signaling pathways and inhibitors of cells from patients with kaposiform lymphangiomatosis. Pediatr Blood Cancer. (2019) 66:e27790. doi: 10.1002/pbc.27790
33. Kim T, Tafoya E, Chelliah MP, Lekwuttikarn R, Li J, Sarin KY, et al. Alterations of the MEK/ERK, BMP, and Wnt/β-catenin pathways detected in the blood of individuals with lymphatic malformations. PLoS One. (2019) 14:e0213872. doi: 10.1371/journal.pone.0213872
34. Liu X, Cheng C, Chen K, Wu Y, Wu Z. Recent progress in lymphangioma. Front Pediatr. (2021) 9:735832. doi: 10.3389/fped.2021.735832
35. Shayesteh S, Salimian KJ, Fouladi DF, Blanco A, Fishman EK, Kawamoto S. Intra-abdominal lymphangioma: a case report. Radiol Case Rep. (2021) 16:123–7. doi: 10.1016/j.radcr.2020.10.052
36. Dunev VR, Genov PP, Kirilov IV, Mladenov VD. Retroperitoneal cystic lymphangioma-a case report. Urol Case Rep. (2021) 35:101555. doi: 10.1016/j.eucr.2020.101555
37. Nuzzo G, Lemmo G, Marrocco-Trischitta MM, Boldrini G, Giovannini I. Retroperitoneal cystic lymphangioma. J Surg Oncol. (1996) 61:234–7. doi: 10.1002/(SICI)1096-9098(199603)61:3<234::AID-JSO14>3.0.CO;2-7 8637214
38. Saadi A, Ayed H, Karray O, Kerkeni W, Bouzouita A, Cherif M, et al. Retroperitoneal cystic lymphangioma: about 5 cases and review of the literature. Pan Afr Med J. (2016) 25:73. doi: 10.11604/pamj.2016.25.73.10002
39. Lim HJ, Tan JW, Chia CS, Ong CJ. A rare case of retroperitoneal lymphangioma in a 74-year-old Chinese male. J Surg Case Rep. (2021) 2021:rjaa610. doi: 10.1093/jscr/rjaa610
40. Kodera K, Abe K, Kanehira M, Futagawa Y, Okamoto T, Ikegami T. Retroperitoneal lymphangioma mimicking malignant tumor treated by pancreaticoduodenectomy. Clin J Gastroenterol. (2021) 14:1791–7. doi: 10.1007/s12328-021-01492-6
41. Cherk M, Nikfarjam M, Christophi C. Retroperitoneal lymphangioma. Asian J Surg. (2006) 29:51–4. doi: 10.1016/S1015-9584(09)60297-9
42. Bhavsar T, Saeed-Vafa D, Harbison S, Inniss S. Retroperitoneal cystic lymphangioma in an adult: a case report and review of the literature. World J Gastrointest Pathophysiol. (2010) 1:171–6. doi: 10.4291/wjgp.v1.i5.171
43. Aminian A, Jafarian A, Mirsharifi R, Moulavi S, Dashti H, Ali FA. Retroperitoneal cystic lymphangioma. Indian J Surg. (2008) 70:150–1. doi: 10.1007/s12262-008-0043-7
44. Lai EC, Li AC, Leong HT, Lau WY. Retroperitoneal cystic lymphangioma. ANZ J Surg. (2005) 75:365–6. doi: 10.1111/j.1445-2197.2005.03359.x
45. Liedtke KR, Käding C, Döring P, Bekeschus S, Glitsch AS. A case of giant retroperitoneal lymphangioma and IgG4-positive fibrosis: causality or coincidence. SAGE Open Med Case Rep. (2021) 9:2050313X211016993. doi: 10.1177/2050313X211016993
46. Kalish M, Dorr R, Hoskins P. Retroperitoneal cystic lymphangioma. Urology. (1975) 6:503–6. doi: 10.1016/0090-4295(75)90641-x
47. Suhani S, Aggarwal L, Ali S, Thomas S. Giant retroperitoneal lymphangioma: a rare entity. Indian J Surg. (2014) 76:402–4. doi: 10.1007/s12262-013-0989-y
48. Tripathi M, Parshad S, Karwasra RK, Gupta A, Srivastva S, Sarwal A. Retroperitoneal lymphangioma in an adult: a case report of a rare clinical entity. Case Rep Surg. (2015) 2015:732531. doi: 10.1155/2015/732531
49. Sato T, Matsuo Y, Shiga K, Saito K, Morimoto M, Miyai H, et al. Laparoscopic resection of retroperitoneal lymphangioma around the pancreas: a case report and review of the literature. J Med Case Rep. (2015) 9:279. doi: 10.1186/s13256-015-0760-z
50. Chaker K, Sellami A, Ouanes Y, Zehani A, Jallouli W, Ben Chehida MA, et al. Retroperitoneal cystic lymphangioma in an adult: a case report. Urol Case Rep. (2018) 18:33–4. doi: 10.1016/j.eucr.2018.02.019
51. Olaoye IO, Adesina MD. Rare huge retroperitoneal cystic lymphangioma presenting as acute abdomen in an adult. BJR Case Rep. (2018) 4:20170120. doi: 10.1259/bjrcr.20170120
52. Rezaee ME, Alexakos SG, Taylor CE, Santis WF. A rare case of a retroperitoneal lymphangioma causing chronic flank pain in an adult. Urol Case Rep. (2020) 33:101408. doi: 10.1016/j.eucr.2020.101408
53. Black T, Guy CD, Burbridge RA. Retroperitoneal cystic lymphangioma diagnosed by endoscopic ultrasound-guided fine needle aspiration. Clin Endosc. (2013) 46:595–7. doi: 10.5946/ce.2013.46.5.595
54. Hubli P, Rohith M, Sachin BM. A giant retroperitoneal lymphangioma: a case report. J Clin Diagn Res. (2016) 10:PD14–5. doi: 10.7860/JCDR/2016/19989.8142
55. Rajput D, Srikanth K, Gupta A, Kumar A, Edem S, David LE, et al. Large retroperitoneal cystic lymphangioma mimicking mesenteric cyst: a case report. Pan Afr Med J. (2022) 42:115. doi: 10.11604/pamj.2022.42.115.30777
56. Kasza J, Brody FJ, Khambaty F, Vaziri K, Wallace B. Laparoscopic resection of a retroperitoneal cystic lymphangioma in an adult. Surg Laparosc Endosc Percutan Tech. (2010) 20:e114–6. doi: 10.1097/SLE.0b013e3181db79a7
57. Izumi D, Toyama E, Shigaki H, Iwagami S, Baba Y, Hayashi N, et al. Laparoscopic excision of an adult retroperitoneal cystic lymphangioma coexisting with an esophageal hiatus hernia. Clin J Gastroenterol. (2015) 8:130–3. doi: 10.1007/s12328-015-0571-1
58. Ionescu C, Ionescu M, Dumitrascu T. Retroperitoneal cystic lymphangioma in a patient with previous surgery for seminoma. A Case Report. Maedica. (2012) 7:180–2. PMID: 23399992
59. Tsukamoto T, Tanaka S, Yamamoto T, Kakinoki E, Uemichi A, Kubo S, et al. Laparoscopic excision of a retroperitoneal cystic lymphangioma: report of a case. Surg Today. (2003) 33:142–4. doi: 10.1007/s005950300032
60. Mabrouk A, Ennaceur F, Karoui Y, Nejma EB, Jedidi L, Moussa MB. Giant retroperitoneal lymphangioma in a 70-year-old male: a case report. Pan Afr Med J. (2022) 42:153. doi: 10.11604/pamj.2022.42.153.34175
61. Suryawanshi PR, Agrawal MM, Rathod MD, Mandhane AM. Laparoscopic excision of a large retroperitoneal lymphovascular malformation in an adult. J Minim Access Surg. (2017) 13:66–8. doi: 10.4103/0972-9941.181773
62. Chung SH, Park YS, Jo YJ, Kim SH, Jun DW, Son BK, et al. Asymptomatic lymphangioma involving the spleen and retroperitoneum in adults. World J Gastroenterol. (2009) 15:5620–3. doi: 10.3748/wjg.15.5620
Keywords: cystic lymphangioma, retroperitoneal tumor, surgical resection, case report, literature review
Citation: Su T, Li C, Song B, Song D and Feng Y (2023) Case report and literature review: Giant retroperitoneal cystic lymphangioma. Front. Surg. 10:1074067. doi: 10.3389/fsurg.2023.1074067
Received: 19 October 2022; Accepted: 2 January 2023;
Published: 17 January 2023.
Edited by:
Zhaolun Cai, Sichuan University, ChinaReviewed by:
Miltiadis Lalountas, General Hospital Polygyrou Chalkidiki, GreeceFrancisco Sanchez Bueno, Hospital Universitario Virgen de la Arrixaca, Spain
© 2023 Su, Li, Song, Song and Feng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Defeng Song U2RmNjEwNjEzQGpsdS5lZHUuY24= Ye Feng ZmVuZ3llQGpsdS5lZHUuY24=
Specialty Section: This article was submitted to Surgical Oncology, a section of the journal Frontiers in Surgery
 Tieshan Su
Tieshan Su Chaoyuan Li
Chaoyuan Li Bin Song1
Bin Song1 Ye Feng
Ye Feng