- Department of Medical Imaging, National Cheng Kung University Hospital, Tainan, Taiwan
Introduction: Percutaneous transhepatic biliary drainage (PTBD) is a common procedure for biliary obstructive jaundice caused by biliary tract obstruction. In clinical practice, PTBD can be carried out at right- or left-sided approach. However, different hepatic entry site may affect success rates and complications. Couinaud classification of liver anatomy further divides the liver into functionally independent segments (segment 2/3, segment 5/6, and segment 7/8). Therefore, this study aimed to elucidate whether different Couinaud hepatic segments as PTBD entry site are associated with high PTBD success and low complications.
Methods: A total of 617 patients who underwent PTBD were retrospectively reviewed. Univariate and multivariate logistic regression analyses were performed to identify entry segments associated with PTBD success, bilirubin reduction, and complications.
Results: With higher hepatic segment of PTBD entry site (segment 2/3, 5/6, and 7/8), the trend of PTBD success rate (82.0%, 71.7% and 60.7%; P<0.001) and bilirubin reduction (93.2%, 89.5%, and 82.0%; P=0.012) decreased. Furthermore, PTBD entry at segment 7/8 (42.6%) had highest complication rate than segment 5/6 (6.4%) and 2/3 (9.4%). Univariate and multivariate logistic regression analyses showed that PTBD entry segment was an independent factor associated with PTBD success, bilirubin reduction, and complications. Compared to segment 7/8, segment 2/3 and 5/6 had higher odds of PTBD success (aOR=2.699 and aOR=1.454, respectively) and bilirubin reduction (aOR=3.472 and aOR=2.361, respectively) and associated with lower risk of complications (aOR=0.143 and aOR=0.098, respectively). No independent risk factor for PTBD success and bilirubin reduction were identified in intrahepatic tumors. Moreover, for extrahepatic tumors, PTBD entry at segment 2/3 and segment 5/6 was more likely achieve PTBD success (aOR=3.037 and aOR=1.929, respectively), bilirubin reduction (aOR=3.069 and aOR=3.515) and low complications (aOR=0.102 and aOR=0.126, respectively).
Discussion: Good clinical outcomes were observed for PTBD entry at segments 5/6 and 2/3. In contrast, segment 7/8 had the lowest success rate, smallest bilirubin reduction, and the highest complication rate. For patients with obstructive jaundice, PTBD entry in hepatic segments 2/3 and 5/6 is recommended to achieve high success rates and low complications.
Introduction
Obstructive jaundice occurs when blockage of the biliary drainage system prevents the passage of bile from the liver to the small intestine, leading to conjugated hyperbilirubinemia. The most common causes of biliary tree obstruction are malignancies, gallstones, and fibrosis, manifesting symptoms as pain, nausea, vomiting, and jaundice (1). Such obstructions affect a large portion of the population worldwide, with impaired quality of life and significant morbidity and mortality (1–3). In the US, the incidence of biliary obstruction is approximately 5 cases per 1,000 people (4). The symptoms of obstructive jaundice, including abdominal pain, cholangitis, and pruritus, can be relieved by procedures that decompress the affected areas of the biliary circulation (5). Although surgical resection of malignant obstructive jaundice or endoscopic removal of gallstones is usually the mainstay of treatment, it is not always feasible due to the small number of eligible patients and the higher incidence of postoperative complications.
With advances in technology, percutaneous transhepatic biliary drainage (PTBD) has been considered as an effective palliative treatment of obstructive jaundice, especially when surgery is assessed to be infeasible (6, 7). PTBD is used to decompress intra- and extrahepatic biliary ducts in cases of malignant or benign obstruction to alleviate symptoms, decrease serum bilirubin before starting chemotherapy, or to facilitate biliary stent placement (5). Under imaging guidance using fluoroscopy with or without ultrasound, a needle is used to puncture the liver at the chosen location and is directed to the appropriate segmental duct (5). Nevertheless, the in-hospital mortality rate in patients receiving PTBD for obstructive jaundice is still high, with even reported mortality rates as high as nearly 20% (8, 9). For unresectable biliary tract obstruction, higher mortality is associated with preoperative clinical factors (eg, older patients, men, and these with increasing comorbidities) and, in particular, with inexperienced operator (lower-volume PTBD providers) (9).
PTBD can be performed via either the right (subcostal or intercostal) or left ductal (subxiphoid) approach. The chosen approach is presently viewed as a personal preference, with advantages and disadvantages for each (5). However, the few studies comparing PTBD efficacy, effects on quality of life, and complications between the two approaches report conflicting results. A randomized controlled trial including 64 patients found that self-reported quality of life following PTBD was higher for left than for right access (10). In contrast, a study including 50 PTBD patients reports no significant difference in quality of life, success rates, or complications between the left and right approaches (11). Other studies investigating complications after PTBD report a slightly higher rate of hemobilia following the left approach (12) and more cases of cholangitis and fever with the right approach (13), but the differences were not statistically significant in either study. While one study of 36 PTBD procedures observed no differences in efficacy or safety between the 2 approaches(14), our previous study including 446 PTBD patients showed that the left approach had better clinical outcomes and fewer complications (15).
Several factors may contribute to these conflicting results. Many of the study cohorts were relatively small, lowering the statistical power. In addition, the anatomical classification of the liver entry site as left or right lobe may be too broad to identify entry-site effects. The Couinaud system of liver classification divides the liver into 8 functionally independent segments, each with its own vascular inflow, biliary drainage, and lymphatic drainage (16, 17). Segments 2–4 compose the left hepatic lobe, and segments 5–8 compose the right hepatic lobe. No study has investigated the effect of PTBD entry site using liver segments to designate the entry site. Therefore, this study aims to expand the understanding of the treatment outcomes of patients with obstructive jaundice according to different segments of PTBD entry. In a large cohort of 617 patients, we determine and compare the technical success rates, degree of bilirubin reduction, and complication rates between PTBD entry in segments 2/3, 5/6, and 7/8.
Materials and methods
Study design and patients
This retrospective study was approved by the Institutional Review Board (IRB) of National Cheng Kung University Hospital (IRB number: B-ER-110-392). The requirement of written informed consent was waived by the IRB due to the retrospective nature of the study. Patients who presented to National Cheng Kung University Hospital with obstructive jaundice between 2008 and 2020 were retrospectively screened. Inclusion criteria were age > 20 years and treatment with PTBD. Exclusion criteria were missing clinical information (e.g., demographic data, procedure time, duct diameter, indications for obstruction, presence of ascites, obstruction level, hepatic puncture site) and missing data regarding final treatment outcomes (PTBD success and bilirubin reduction) or complications. In this study, all PTBD procedures were conducted with placement of an around 8 Fr small pigtail drainage catheter and were performed by interventional radiologists with more than 10 years of experience in biliary intervention. Postoperative complications were graded according to the Clavien-Dindo classification. Bilirubin reduction was defined as normalization of bilirubin or a serum total bilirubin concentration of ≤3 mg/dl or decrease in bilirubin levels by ≥30% within 2 weeks of biliary drainage.
Statistical analysis
All statistical analyses were performed using IBM SPSS statistical software version 22 for Windows (IBM Corp., Armonk, New York, USA). Continuous variables are expressed as the mean ± standard deviation (SD), and categorical variables are presented as frequency and percentage. Differences between continuous variables were examined using one-way ANOVA. Categorical variables were compared using the Chi-square test or Fisher's exact test. Univariate and multivariate logistic regression analyses were performed to identify risk factors associated with PTBD success, bilirubin reduction, and complications. Results are expressed as the odds ratio (OR) with 95% confidence interval (CI). Stratified analyses were performed based on malignancy and adjusted for significant risk factors identified in univariate analysis. Two-sided P < 0.05 was considered statistically significant.
Results
Patient characteristics and PTBD outcomes and complications
Demographic data and clinical outcomes of 617 patients with obstructive jaundice who received PTBD are shown in Table 1. The mean patient age was 67.14 ± 13.61 years, and 55.6% of the patients were male. Most patients (85.6%) underwent PTBD in the hospital ward. The mean targeted bile duct diameter was 5.30 ± 2.55 cm, and the mean PTBD procedure time was 43.92 ± 78.70 min. The most common indication for PTBD was malignant biliary obstruction (79.1%), and the remainder were stones (11.8%) and fibrosis (9.1%). Most of the 488 malignant biliary obstructions were located in the extrahepatic (369; 77.0%) or intrahepatic (112; 23.0%) bile ducts. Obstructions were at the common bile duct (CBD) (45.2%), common hepatic duct (CHD) (32.3%), lobar (20.7%), and segmental (1.8%) levels. Only a subset of patients had a small (7%) or moderate/massive amount (3.6%) of ascites before PTBD. The PTBD puncture was performed at the segmental (31.2%), subsegmental (51.8%), or sub-subsegmental (17.0%) level of the intrahepatic duct. Based on the Couinaud classification of liver segments, the patients were further grouped according to the liver segment of PTBD entry, as follows: segment 2/3, N = 383; segment 5/6, N = 173; and segment 7/8, N = 61. No statistically significant difference was observed in age, sex, surgery time, surgical department, obstruction level, or ascites between the three groups (all P > 0.05). In addition, no significant difference in malignant extrahepatic or extrahepatic bile duct obstruction was observed between the three groups (P = 0.061). The PTBD liver puncture levels differed significantly between the three groups (P < 0.001). The puncture level in the segment 2/3 group was located primarily in the intrahepatic subsegmental ducts (60.8%), followed by segmental (25.8%) and sub-subsegmental ducts (13.3%). In contrast, the most common puncture level in the Segment 7/8 group was segmental ducts (65.6%), followed by subsegmental (29.5%) and sub-subsegmental ducts (4.9%). In the Segment 5/6 group, the proportion of puncture levels in segmental, subsegmental and sub-subsegmental ducts was relatively equal.
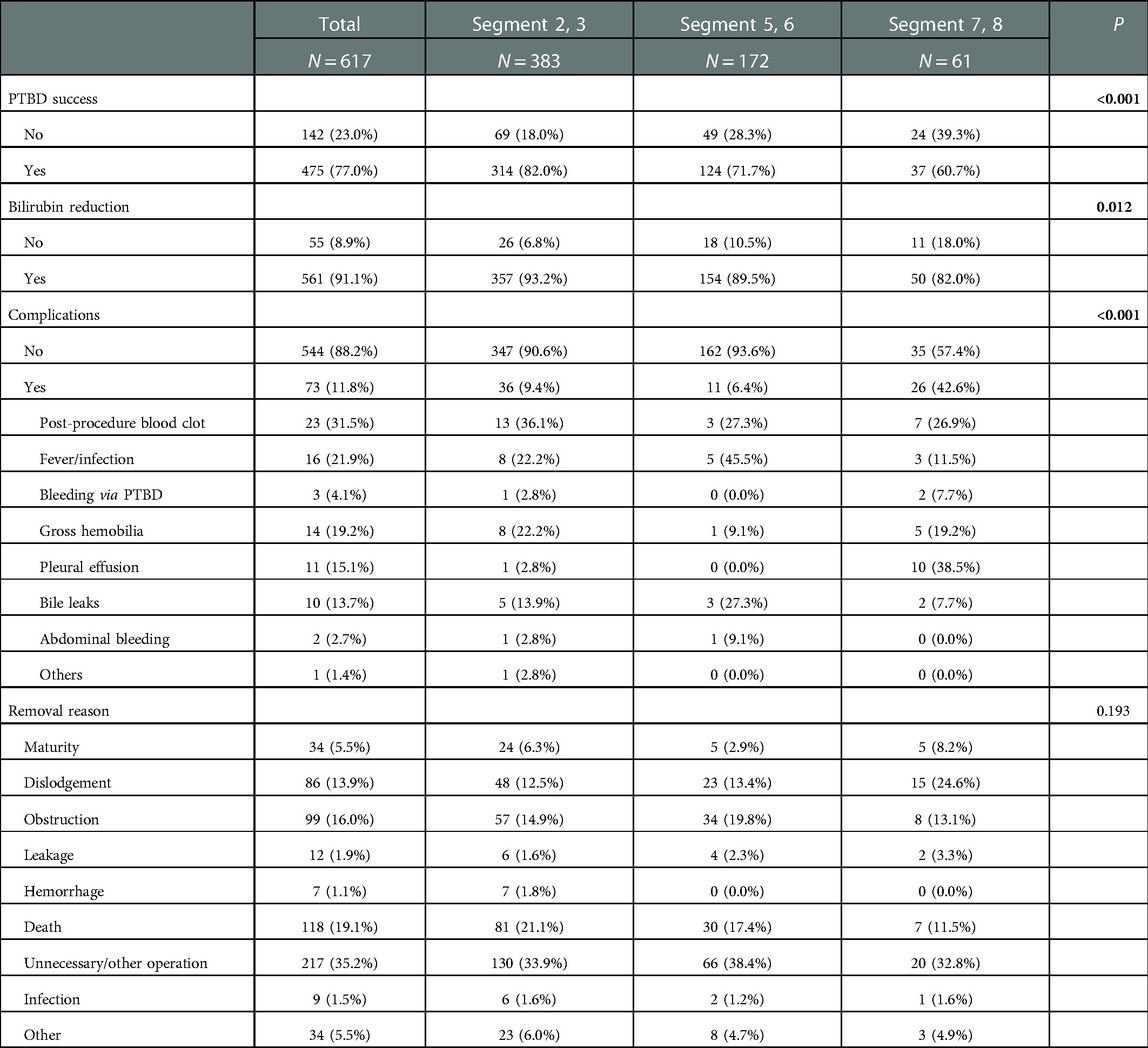
The clinical outcomes, including PTBD success, bilirubin reduction, and complications, are shown in Table 2. The PTBD success rate tended to decrease with increasing PTBD hepatic segment height (segment 2/3, 82.0%; segment 5/6, 71.7%; segment 7/8, 60.7%; P < 0.001). The observed PTBD success rates were consistent with the level of serum bilirubin reduction (segment 2/3, 93.2%; segment 5/6, 89.5%; segment 7/8, 82.0%; P = 0.012). However, the segment 7/8 group had the highest complication rate of 42.6%, while the segment 5/6 group had the lowest complication rate of only 6.4%. The most frequent PTBD complications in the total cohort were post-procedure blood clot (31.5%), fever/infection (21.9%), and gross hemobilia (19.2%). Most complications were grade I-II. Only 10 patients experienced complications of Clavien-Dindo grade III. No patients underwent PTBD had severe complications (grade > IV) based on the Clavien–Dindo classification. In the Segment 2/3 group, blood clot (36.1%) was the most frequent complication. Fever/infection (45.5%) was the most frequent complication in the segment 5/6 group, while pleural effusion (38.5%) was the most frequent complication in the segment 7/8 group. In summary, PTBD entry in hepatic segment 5/6 had similar good success rates and low complication rates as did segment 2/3 entry. PTBD entry in hepatic segment 7/8 was associated with the lowest success rates and highest complication rates.
Factors associated with PTBD success, bilirubin decrease, and complications
Univariate and multivariate logistic regression analyses were performed to identify independent risk factors for PTBD success, bilirubin reduction, and complications. As shown in Table 3, ascites was an independent risk factor for bilirubin reduction. Absence of ascites before PTBD was significantly associated with a higher rate of bilirubin reduction (aOR, 3.437; 95% CI, 1.703–6.937; P, 0.001). In addition, the liver segment of PTBD entry was an independent risk factor associated with PTBD success, bilirubin reduction, and complications. Compared to Segment 7/8, the adjusted odds of PTBD success were significantly higher in with Segment 2/3 entry (aOR, 2.699; 95% CI, 1.484–4.908; P, 0.001). Segment 5/6 entry also had a higher odds ratio, although it did not reach statistical significance (aOR, 1.454; 95% CI, 0.884–3.000; P, 0.246). Similarly, entry at Segment 2/3 (aOR, 3.472; 95% CI, 1.584–7.609; P, 0.002) and Segment 5/6 (aOR, 2.361; 95% CI, 1.013–5.503; P, 0.047) had significantly higher adjusted odds of bilirubin reduction than did Segment 7/8. The odds of complications were higher for Segment 7/8 entry than for Segment 2/3 (aOR, 0.143; 95% CI, 0.074–0.276; P < 0.001) and Segment 5/6 (aOR, 0.098; 95% CI, 0.043–0.224; P < 0.001). These results suggest that hepatic segments 2/3 and 5/6 are better PTBD entry sites for optimizing success rates and minimizing complications.
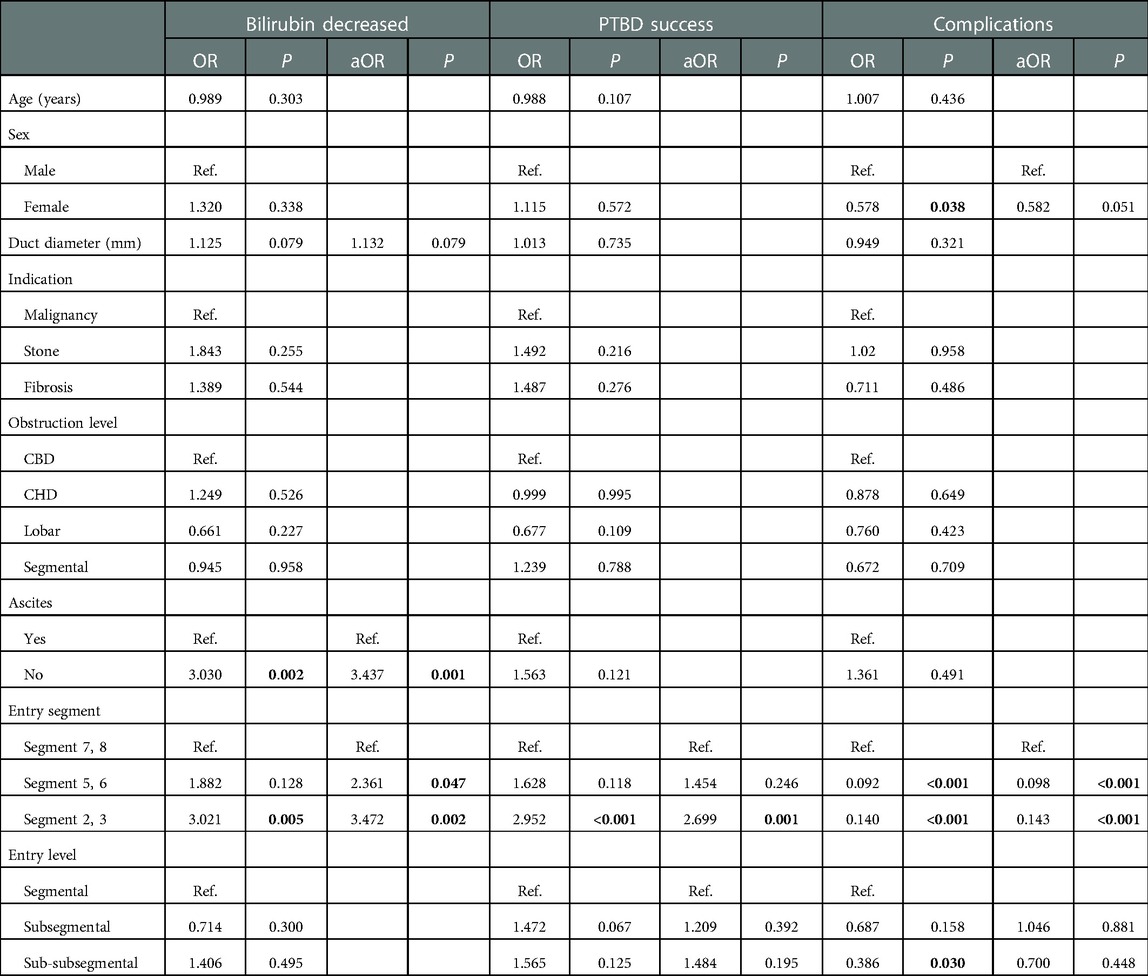
Table 3. Logistic regression analysis of factors associated with PTBD success, bilirubin reduction, and complications.
Biliary tract malignancies are primarily tumors of the intrahepatic and extrahepatic bile ducts. Promoting biliary drainage to decompress the biliary tract and improve quality of life is one goal of biliary malignancy treatment. Accordingly, we compared the factors associated with PTBD success, bilirubin reduction, and complications between patients with intra- and extrahepatic tumors. Multivariate logistic regression analysis showed that PTBD entry in segment 2/3 was more likely to achieve PTBD success (aOR, 3.037; 95% CI, 1.306–7.058; P, 0.010) and bilirubin reduction (aOR, 3.069; 95% CI, 1.011–9.314; P, 0.048) in patients with extrahepatic tumors (Table 4). For malignancies in the extrahepatic bile duct, PTBD entry in segment 5/6 also had a higher likelihood of bilirubin reduction (aOR, 3.515; 95% CI, 0.974–12.684; P, 0.055). No independent risk factors for bilirubin reduction or PTBD success were identified in malignancies in the intrahepatic bile duct. PTBD entry in segments 2/3 and 5/6 had a lower likelihood of complications in both intrahepatic tumors (aOR, 0.142; 95% CI, 0.027–0.742; P, 0.021 and aOR, 0.114; 95% CI, 0.015–0.848; P, 0.034, respectively) and extrahepatic tumors (aOR, 0.126; 95% CI, 0.051–0.310; P < 0.001 and aOR, 0.102; 95% CI, 0.035–0.298; P < 0.001, respectively). In addition, ascites before PTBD remained an independent risk factor for bilirubin reduction in patients with extrahepatic tumors, with an adjusted odds ratio of 3.363 (95% CI, 1.356–8.342; P, 0.009).
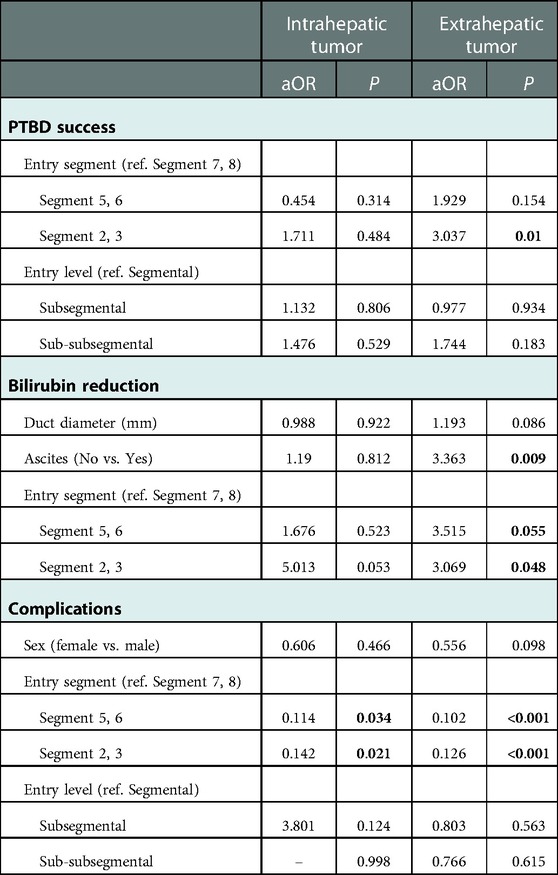
Table 4. Adjusted association of intrahepatic/extrahepatic tumors with PTBD success, bilirubin reduction, and complications.
Discussion
In a large cohort of patients who underwent PTBD for obstructive jaundice, we observed that the liver segment of PTBD entry is an independent factor associated with PTBD success, bilirubin reduction, and complications. Equally good clinical outcomes (high PTBD success and bilirubin reduction; low complication rates) were observed for entry at liver segment 5/6 and liver segment 2/3. However, PTBD entry at liver segment 7/8 was associated with the lowest success rate, smallest bilirubin reduction, and the highest rate of complications. These results suggest that PTBD entry in hepatic segments 2/3 and 5/6 optimizes success rates and minimizes complications. As the first study to investigate PTBD success based on Couinaud liver segment classification, these results confirm that such entry site designation provides more detailed information regarding PTBD success according to entry site than does left/ right lobe designation.
The clinical success rate of PTBD (77.0%) for our total cohort is comparable to that of other studies, reporting rates of 87.5% (18), 76.5% (19), and 76% (11). Importantly, we observed that the clinical success of PTBD varied with the site of entry. While our previous study showed a significantly greater PTBD clinical success rate for left than right lobe access (15), the segmental designation used in the present study allowed us to identify a significant difference in success rates for sites within the right lobe. Entry into liver segment 7/8 (right lobe) had a significantly lower clinical success rate (60.7%) than did segments 5/6 (right lobe) (71.7%) and 2/3 (left lobe) (82%). This finding indicates further access options for successful PTBD, including segments 2/3 as well as 5/6.
We observed significantly lower complication rates with PTBD entry at segment 2/3 (9.4%) and 5/6 (6.4%) than at segment 7/8 (42.6%). Rafiq et al. observed more complications with right-sided (subcostal or intercostal) than left-sided (sub-xiphoid) PTBD, although the differences were statistically insignificant, possibly due to their small cohort size (n = 31) (13). The similar result in our much larger cohort not only confirms that fewer complications occur in left-side PTBD but also shows that the high complication rate for right-sided PTBD is due to entry at segment 7/8. One possible reason for the high complication rate associated with segment 7/8 entry is that this region is affected by respiratory movements. Catheters may become malpositioned in response to respiratory movements and can gradually be pulled out of the liver. One study reports that PTBD catheter dislodgement occurred only on the right side, noting that its displacement was due to continuous motion of the catheter in the intercostal space during respiration (13). Another study also reports a higher incidence of catheter dislodgement in right-sided PTBD, and the authors suggest that the high incidence may be due to the small volume of the intercostal space and greater movement of the catheter within the liver during respiration, leading to displacement of the internal section of the catheter (11). PTBD entry at Segment 5/6 is thus recommended in cases involving an atrophic or high-riding left hepatic lobe (segment 2/3).
This study has several limitations. The retrospective nature of this study limits the data available for analysis, including information regarding quality of life after PTBD. The PTBD procedures were performed by many operators with varied levels of experience, which may have affected the PTBD success rates or complication rates.
Conclusion
PTBD entry in hepatic segment 7/8 has the lowest clinical success rate and highest complication rate. Despite previous reports of lower PTBD efficacy for right-sided entry, we observed that PTBD entry in hepatic segments 2/3 (left hepatic lobe) or 5/6 (right hepatic lobe) optimizes clinical success and minimizes complications. For studies of PTBD efficacy, Couinaud liver segment classification of entry sites provides more detailed results than does left/ right lobe designation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by This retrospective study was approved by the Institutional Review Board (IRB) of National Cheng Kung University Hospital (IRB number: B-ER-110-392). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
YCH: conceptualized and designed this study, performed statistical analysis, interpreted the data, and drafted the manuscript. HYE, CMC, and CYL: collected, analyzed and validated the clinical data. YSL: contributed to the study conceptualization, data interpretation, and supervision of the project. HSH: statistically analyzed the data, interpreted the data, drafted the manuscript and supervised the project. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to thank Convergence CT for providing English editing to improve English grammar and language usage.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Coucke EM, Akbar H, Kahloon A, Lopez PP. Biliary Obstruction. In: Statpearls. Treasure island (FL): StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC (2022). https://www.ncbi.nlm.nih.gov/books/NBK539698/#article-18277.s2
2. Bjornsson E, Gustafsson J, Borkman J, Kilander A. Fate of patients with obstructive jaundice. J Hosp Med. (2008) 3:117–23. doi: 10.1002/jhm.272
3. Abraham NS, Barkun JS, Barkun AN. Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. Gastrointest Endosc. (2002) 56:835–41. doi: 10.1067/mge.2002.129868
4. Taylor T, Wheatley M. Jaundice in the emergency department: meeting the challenges of diagnosis and treatment. Emerg Med Pract. (2018) 20:1–24.
5. Chandrashekhara SH, Gamanagatti S, Singh A, Bhatnagar S. Current status of percutaneous transhepatic biliary drainage in palliation of malignant obstructive jaundice: a review. Indian J Palliat Care. (2016) 22:378–87. doi: 10.4103/0973-1075.191746
6. van Delden OM, Lameris JS. Percutaneous drainage and stenting for palliation of malignant bile duct obstruction. Eur Radiol. (2008) 18:448–56. doi: 10.1007/s00330-007-0796-6
7. Huang P, Zhang H, Zhang XF, Lv W, Lou S. Comparison of endoscopic ultrasonography guided biliary drainage and percutaneous transhepatic biliary drainage in the management of malignant obstructive jaundice after failed ERCP. Surg Laparosc Endosc Percutan Tech. (2017) 27:e127–e31. doi: 10.1097/SLE.0000000000000485
8. Sha J, Dong Y, Niu H. A prospective study of risk factors for in-hospital mortality in patients with malignant obstructive jaundice undergoing percutaneous biliary drainage. Medicine. (2019) 98:e15131. doi: 10.1097/MD.0000000000015131
9. Rees J, Mytton J, Evison F, Mangat KS, Patel P, Trudgill N. The outcomes of biliary drainage by percutaneous transhepatic cholangiography for the palliation of malignant biliary obstruction in England between 2001 and 2014: a retrospective cohort study. BMJ Open. (2020) 10:e033576. doi: 10.1136/bmjopen-2019-033576
10. Castiglione D, Gozzo C, Mammino L, Failla G, Palmucci S, Basile A. Health-related quality of life evaluation in “left” versus “right” access for percutaneous transhepatic biliary drainage using EORTC QLQBIL-21 questionnaire: a randomized controlled trial. Abdom Radiol. (2020) 45:1162–73. doi: 10.1007/s00261-019-02136-7
11. Behera RK, Srivastava DN, Kumar P, Pal S, Ranjan N, Garg P, et al. Right-sided versus left-sided percutaneous transhepatic biliary drainage in the management of malignant biliary obstruction: a randomized controlled study. Abdom Radiol. (2021) 46:768–75. doi: 10.1007/s00261-020-02651-y
12. Rivera-Sanfeliz GM, Assar OS, LaBerge JM, Wilson MW, Gordon RL, Ring EJ, et al. Incidence of important hemobilia following transhepatic biliary drainage: left-sided versus right-sided approaches. Cardiovasc Intervent Radiol. (2004) 27:137–9. doi: 10.1007/s00270-003-0022-0
13. Rafiq S, Khan A, Suhail J, Choh N, Shaheen F. Complications of left and right sided percutaneous transhepatic biliary drainage. Adv Med Sci. (2019) 6:5. doi: 10.18203/2349-3933.ijam20193286
14. Kim YH, Cha SJ. US-guided percutaneous transhepatic biliary drainage: comparative study of right-sided and left-sided approach. J Korean Radiol Soc. (2002) 46:115. doi: 10.3348/jkrs.2002.46.2.115
15. Liu YS, Lin CY, Chuang MT, Tsai YS, Wang CK, Ou MC. Success and complications of percutaneous transhepatic biliary drainage are influenced by liver entry segment and level of catheter placement. Abdom Radiol. (2018) 43:713–22. doi: 10.1007/s00261-017-1258-5
16. Bismuth H. Surgical anatomy and anatomical surgery of the liver. World J Surg. (1982) 6:3–9. doi: 10.1007/BF01656368
17. Couinaud C. Surgical anatomy of the liver revisited. C. Couinaud 15 rue spontini F 75116 Paris. Paris: Claude Couinaud, Paris (1989).
18. Lee TH, Choi JH, Park do H, Song TJ, Kim DU, Paik WH, et al. Similar efficacies of endoscopic ultrasound-guided transmural and percutaneous drainage for malignant distal biliary obstruction. Clin Gastroenterol Hepatol. (2016) 14:1011–19 e3. doi: 10.1016/j.cgh.2015.12.032
Keywords: couinaud, hepatic segment, hepatic lobe, obstructive jaundice, complications
Citation: Hsu Y, Lee H, Chang C, Lin C, Liu Y and Huang H (2023) Clinical outcomes of percutaneous transhepatic biliary drainage at different Couinaud's hepatic entry segments for treating obstructive jaundice. Front. Surg. 10:1039106. doi: 10.3389/fsurg.2023.1039106
Received: 7 September 2022; Accepted: 2 January 2023;
Published: 24 January 2023.
Edited by:
Airazat M. Kazaryan, Østfold Hospital, NorwayReviewed by:
Dmitry Panchenkov, Moscow State University of Medicine and Dentistry, RussiaGeorgy Ivakhov, Pirogov Russian National Research Medical University, Russia
Khachatur Badalyan, National Institute of Health Named After Academician S. KH. Avdalbekyan, Armenia
© 2023 Hsu, Lee, Chang, Lin, Liu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Han-Sheng Huang aDEwOTMzQGhvdG1haWwuY29t
Specialty Section: This article was submitted to Surgical Oncology, a section of the journal Frontiers in Surgery
 Ya-Chun Hsu
Ya-Chun Hsu Han-Sheng Huang
Han-Sheng Huang