- 1Department of Joint Surgery, Third Affiliated Hospital of Zunyi Medical University (The First People’s Hospital of Zunyi), Zunyi, China
- 2Department of Neurology, Third Affiliated Hospital of Zunyi Medical University (The First People’s Hospital of Zunyi), Zunyi, China
- 3Authentication Center for Forensic Medicine and Judicature, Third Affiliated Hospital of Zunyi Medical University (The First People’s Hospital of Zunyi), Zunyi, China
Objective: To investigate the clinical efficacy of arthroscopic capsular release and postoperative intra-articular infusion of cocktail combined with tranexamic acid (TXA) in the treatment of patients with frozen shoulder.
Method: A total of 85 middle-aged and older patients with frozen shoulder who underwent arthroscopic capsular release and received intra-articular infusion of TXA alone (n = 28), cocktail alone (n = 26), and cocktail plus TXA (n = 31) after surgery were retrospective analyzed. The drainage volume within 24 h after surgery, postoperative length of hospital stay, postoperative complications, visual analog scale (VAS), Neer shoulder assessment scale, ASES score, and range of motion (ROM) of the shoulder joint at 1 day, 1 week, 1 month, and 3 months after surgery in all three groups were recorded and compared.
Results: Postoperative length of hospital stay was significantly shorter in the cocktail + TXA and cocktail groups than that in the TXA group. Postoperative drainage volume was significantly higher in the cocktail group compared with TXA + cocktail group (P < 0.05). At 1 day and 1 week after surgery, pain was more pronounced in the TXA group, which was significantly relieved in the cocktail and the cocktail + TXA groups (P < 0.05). Pain was significantly relieved in all the three groups at 1 and 3 months after surgery. Significant functional improvement of the shoulder was achieved in all three groups at 1 week after surgery, the improvement was apparent in the cocktail + TXA groups (P < 0.05), followed by the cocktail group. At 1 month after surgery, patients in the cocktail + TXA groups obtained excellent functional recovery of the shoulder joint. At 3 months after surgery, patients in all the three groups both obtained good recovery of the shoulder joint function, and the recovery was apparent in the cocktail + TXA groups (P < 0.05).
Conclusion: Arthroscopic capsular release and postoperative intra-articular infusion of cocktail combined with TXA has good safety and efficacy in the treatment of middle-age and older patients with frozen shoulder, which can reduce postoperative pain and intra-articular bleeding, promote early postoperative functional exercises and accelerate early postoperative recovery.
Introduction
Frozen shoulder is a common chronic injury disorder of the locomotor system in middle-aged and older people, which is also called adhesive capsulitis, painful stiff shoulder, and periarthritis. The main characteristic of frozen shoulder are limited full range of motion (ROM) in the shoulder joint, chronic pain around the insertion point of the deltoid muscle of the shoulder joint, which seriously affects the patients’ limb function, work ability and patients' quality of life (1). At present, the etiology and pathogenesis of frozen shoulder is not yet clear. Its pathological changes include thickening of capsule of the glenohumeral joint with partial contracture, and some patients may be presented with diffuse inflammation and fibrosis of the ligament tissue surrounding the joint capsule (2). 3D volumetric MR arthrographic assessment of shoulder joint capacity in patients with frozen shoulder showed that the rotator interval, the bicipital groove, and total glenohumeral joint volume were all reduced in patients with frozen shoulder compared with normal controls, extensive adhesion around the joints occurred, resulting in impaired movement of the shoulder joint (3).
Most patients with frozen shoulder can achieve good results by conservative treatments such as physical therapy, intra-articular injection and extracorporeal shock wave therapy. The failure of conservative treatment and the presence of severe symptoms and typical signs of frozen shoulder are all indications for surgical treatment. Severe symptoms include: (1) persistent pain (worsening during the night) and poor sleep quality; (2) joint contractures due to extensive soft-tissue thickening and adhesion; (3) limitation of active and passive movements of the shoulder joint in all directions, that seriously affects people's daily life, such as dressing, washing the face, and touching the lower back. Typical signs include: (1) widespread and local pressure pain in the shoulder joint; (2) joint stiffness, such as limited range of shoulder motion (internal and external rotation, forward flexion, abduction, and posterior extension), and increased pain during activity; (3) local muscle contracture, such as contracture of supraspinatus, infraspinatus and deltoid muscles. The goal of surgery is to improve shoulder joint function and relieve clinical symptoms, such as pain, muscle strength, range of motion of the shoulder joint, ability to perform activities of daily living, and local anatomical pattern. Traditional open surgery has largely been abandoned. Arthroscopic capsular release has the advantages of less trauma, fast postoperative recovery, less pain, and good shoulder joint function recovery (4–6), which is gradually more commonly applied clinically. However, during shoulder arthroscopy, extensive and complete capsular release is required in order to achieve good results, so tissue damage, pain, edema and bleeding are unavoidable. Additionally, active and passive functional exercises are required to prevent re-adhesion after surgery, which increases pain, bleeding and swelling to some extent. Patients may be unwilling to perform functional shoulder exercise due to fear of pain, which affects the functional recovery of the shoulder joint. Reducing postoperative pain, bleeding and swelling, accelerating recovery, and maximizing restoration of shoulder function after arthroscopic capsular release are current research hotspots.
Cocktail formula (7, 8) and tranexamic acid (TXA) (9, 10) has been commonly used for intra-articular infusion following hip and knee replacement surgery to relieve pain, reduce bleeding and improve joint function, which have received good clinical results.
For the treatment of frozen shoulder using manipulation (11) and arthroscopic surgery (12), the use of cocktail formula and TXA have received satisfactory clinical results. However, there are few clinical studies on the use of cocktail combined with TXA in arthroscopic capsular release for the treatment of frozen shoulder, clinical efficacy of the combined application of cocktail and TXA needs to be further investigated. Therefore, in the present study, we retrospectively analyzed the clinical data of patients with frozen shoulder who underwent arthroscopic capsular release and received intra-articular infusion of cocktail combined with TXA in Zunyi First People's Hospital from January 2020 to December 2021, observed postoperative pain, intra-articular bleeding, and functional recovery of the shoulder joint in these patients, and aimed to investigate the clinical efficacy of intra-articular infusion of cocktail combined with TXA in the treatment of patients with frozen shoulder after arthroscopic capsular release, so as to provide ideas and new methods for faster recovery in middle-aged and older patients with frozen shoulder after arthroscopic capsular release.
Materials and methods
Subjects
A total of 85 middle-aged and older patients with frozen shoulder who underwent arthroscopic capsular release and received intra-articular infusion of cocktail combined with TXA after surgery in Zunyi First People's Hospital from January 2020 to December 2021 were retrospective analyzed. All patients met the diagnostic criteria for frozen shoulder.
The inclusion criteria included: (1) age range from 50 to 70 years; (2) patients who had pain in the shoulder joint with limited ROM (< 80° of forward flexion, <30° of posterior extension, <90° of abduction, <40° of external and internal rotation), Neer score of <70, and Visual Analogue Scale (VAS) score of >6; (3) patients whose symptom did not improved obviously after more than 3 months of conservative treatment (physical therapy) and arthrocentesis; (4) patients' quality of life was affected due to pain and functional limitations, and they had a strong subjective need for treatment; (5) patients who had good general condition and could tolerate the surgical procedures; (6) patients who had good compliance and were able to cooperate with treatment and follow-up.
The exclusion criteria included: (1) patients who had coagulation dysfunction; (2) the presence of infection, tumor, systemic arthritis in the shoulder joint; (3) movement was restricted at the shoulder joint due to sequelae of cerebral infarction; (4) patients who had cervical spondylosis, pain in the shoulder joint and rheumatoid arthritis involving the shoulder joint may be caused by cervical spondylosis; (5) patients who were allergic to anesthetic drugs, TXA and cocktail; (6) patients who had poor compliance, were unable to cooperate with treatment, and lost to follow-up; (7) patients who had shoulder osteoarthritis; (8) patients who had recurrent dislocation of the shoulder, SLAP, Bankart and Hill-sachs lesions; (9) patients whose rotator cuff was of poor quality with massive tears, that may lead a longer postoperative immobilization period.
According to the drugs used for intra-articular infusion after surgery, patients were divided into three groups: a TXA group (n = 28), a cocktail group (n = 26), and a cocktail + TXA group (n = 31).
This study was reviewed and approved by the Ethics Committee of the First People's Hospital of Zunyi City (No. 2019-028), and informed consent was obtained from the patients.
Methods
Preoperative preparation
After admission, all patients underwent imaging and relevant preoperative examinations. The extent of adhesions within shoulder joint was identified. The cardiopulmonary function, surgical risk and surgical feasibility in patients were assessed. Each patient completed the visual analog scale (VAS), Neer shoulder assessment scale, and the American Society of Shoulder and Elbow Surgery Shoulder Joint Score (ASES) before surgery to evaluate and record their pain and shoulder joint function.
Surgical methods
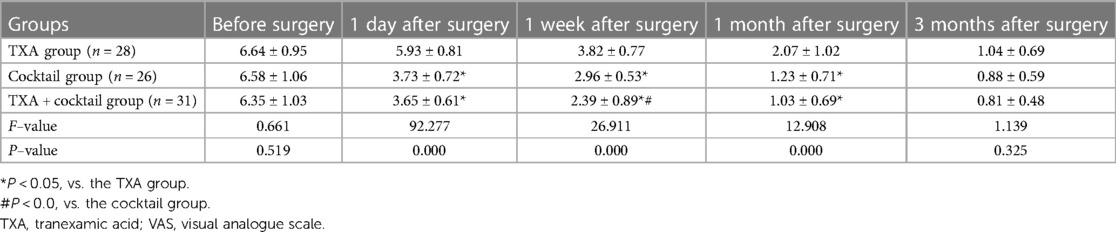
All operations were performed by the same experienced surgeon. All patients received general anesthesia with endotracheal intubation. The surgical table was set into the sitting beach-chair position, and shoulder arthroscopic capsular release was performed. Surgical steps: Step 1: release of the rotator interval composed of long head of the biceps tendon, glenoid lip and the upper edge of the subscapularis, and release of the anterior joint capsule, coracohumeral ligament, superior subscapularis recess, superior and middle glenohumeral ligaments. Particular attention should be paid to release the adhesions at the entrance of the biceps tendon, and protect brachial plexus and vascular bundles during operation. Step 2: release of the anterior inferior joint capsule and the anterior band of the inferior glenohumeral ligament. After this procedure, arthroscopic observation showed that the subscapularis muscle can slide freely during passive external rotation of the glenohumeral joint. If movement was still restricted at the shoulder joint, step 3 was performed. Step 3: release of the posterior joint capsule and the posterior band of the inferior glenohumeral ligament. Care should be taken to protect the underlying axillary nerve (Figure 1A-H).
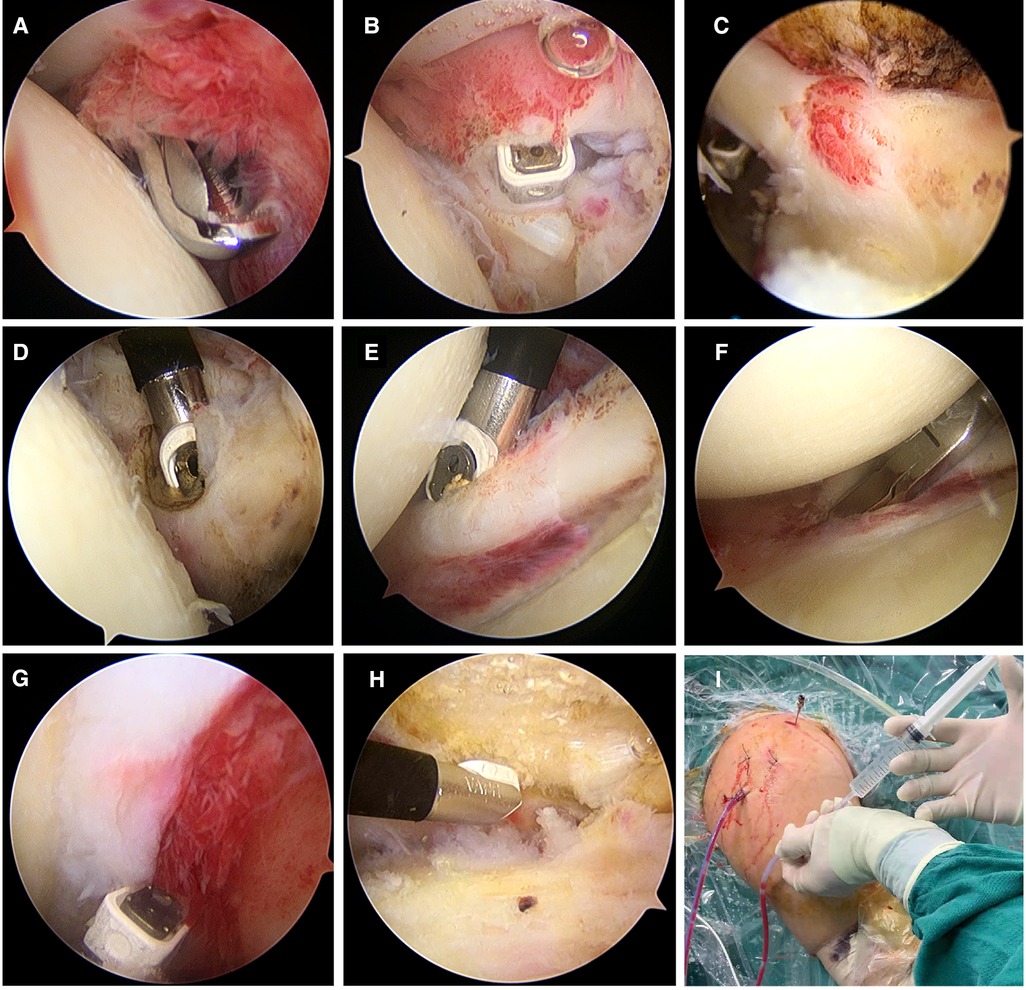
Figure 1. Surgical procedures of arthroscopic capsular release. (A) Clear the inflammatory synovium; (B) Release of the rotator interval; (C) Release of the long head of the biceps tendon; (D) Release of the middle glenohumeral ligament; (E) Release of the anterior band of the inferior glenohumeral ligament; (F) releasing of the anterior and inferior articular capsule; (G) Release of the posterior capsule; (H) Release of the subacromial space; (I) Intra-articular infusion of drugs after surgery.
Intra-articular infusion of cocktail, TXA and cocktail + TXA
After surgery, a drainage tube was placed in the articular cavity. Drugs were then injected via the drainage tube immediately (Figure 1I). Patients in the TXA group were injected with a mixture of 20 ml of 0.9% sodium chloride injection and 1.0 g of TXA injection. Patients in the cocktail group were injected with 1 ml of compound betamethasone, 5 ml of ropivacaine hydrochloride injection, 5 ml of flurbiprofen axetil injection, 0.5 ml of morphine hydrochloride injection, and 4 ml of 0.9% sodium chloride solution. Patients in the TXA + cocktail group were injected with 4 ml of 0.9% sodium chloride solution, 1.0 g of TXA injection, 1 ml of compound betamethasone, 5 ml of ropivacaine hydrochloride injection, 5 ml of flurbiprofen axetil injection, and 0.5 ml of morphine hydrochloride injection. The drainage tube was clamped immediately after injection was completed.
Postoperative management
After operation, ice wrap was applied to the surgical area. The drainage tube was opened after 6 h of intra-articular infusion, the amount of drainage was recorded for 24 h, the drainage tube was then removed. After patients were awakened, they were required to performed active and passive functional exercises such as shoulder extension and adduction, abduction and lifting, internal and external rotation. At 1 day after the operation, patients were instructed to use the affected upper limb to perform activities such as climbing the wall, combing the hair, touching the ears, and holding hands behind the back. Each activity was performed 15 times, 3 times per day, for one month continuously.
Observation indicators
After surgery, drainage volume within 24 h of surgery, postoperative length of hospital stay, postoperative complications, VAS, Neer, ASES scores at 1 day, 1 week, 1 month, and 3 months after surgery were recorded. A goniometer was used to measure and record the maximal ROM of the shoulder joint, including flexion, extension, internal rotation at 90° of elbow flexion, external rotation at 90° of elbow flexion, and abduction before surgery, 1 week, 1 month, and 3 months after surgery.
Statistical analysis
All statistical analyses were performed using SPSS Statistics version 22.0. Continuous variables (such as VAS, Neer, ASES scores) were presented as mean ± standard deviation (SD). For normal distribution data, independent sample t-test was applied to compare the differences between two groups, and one-way analysis of variance test was applied to compare the difference among multiple groups. χ2 test was used to compare the difference in rates between groups. P-value <0.05 was considered significant.
Results
Clinical characteristics of patients included in the study
A total of 85 patients with frozen shoulder were included in the study, there were 38 males and 47 females. In the TXA group, there were 12 males and 16 females, with an average age of 60.79 ± 4.96 years (range, 54–69 years old). In the cocktail group, there were 11 males and 15 females, with an average age of 61.27 ± 4.45 years (range, 54–69 years old). In the cocktail + TXA group, there were 14 males and 17 females, with an average age of 59.97 ± 5.29 years (range 53–70 years old). There was no significant difference between the three groups with respect to sex, age, body mass index, operation time, preoperative VAS, Neer, and ASES scores (P > 0.05, Table 1).
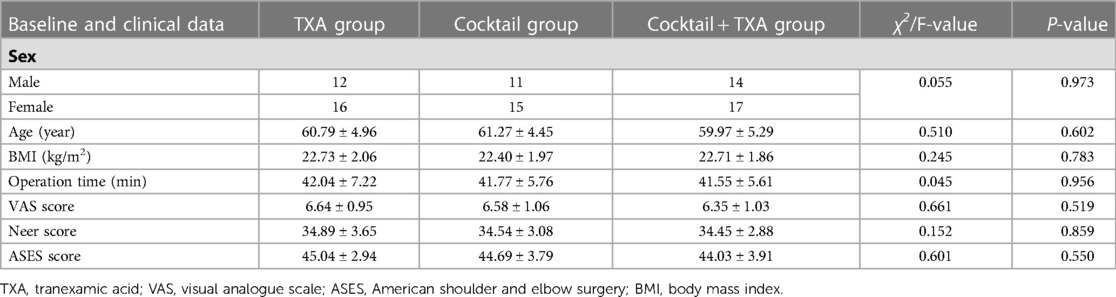
Table 1. Comparison of baseline and clinical data of patients among the three groups before surgery.
Patient's general condition and imaging findings after surgery
Obvious surgical complications were never observed in the three groups. The average postoperative length of hospital stay was 7.39 ± 1.66) days in the TXA group, 5.46 ± 0.95 days in the cocktail group, 5.16 ± 1.04 days in the cocktail + TXA groups. The postoperative length of hospital stay was significantly shorter in the cocktail + TXA and cocktail groups than that in the TXA group (F = 26.519, P = 0.000), while no significant difference was found between between the cocktail + TXA and cocktail groups (P = 0.371, Table 2).

Table 2. Comparison of the average postoperative length of hospital stay and 24-h postoperative drainage volume between the three groups (mean ± SD).
MRI of the shoulder joint at 1 month after surgery showed that the proliferative, adhesive fibrous and synovial tissues surrounding the shoulder joint had been removed (Figure 2).
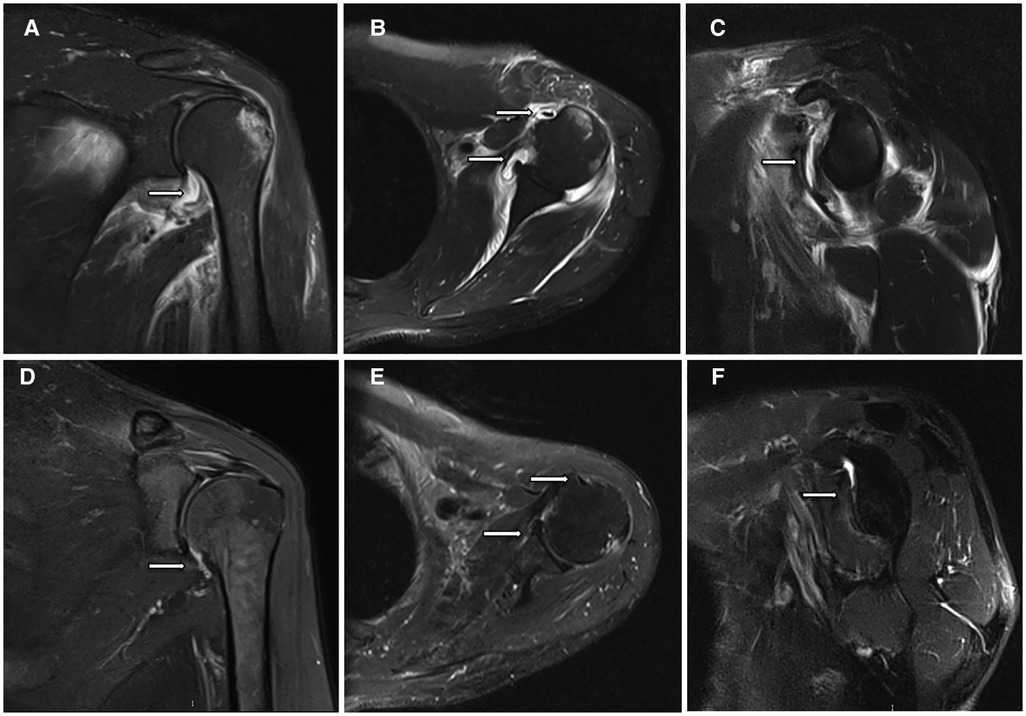
Figure 2. MRI findings of patients with frozen shoulder before and 1 month after arthroscopic capsular release. (A) Thickening and edema of the shoulder capsule (white arrow); (B) Edema and adhesions surrounding the long head of the biceps tendon and rotator interval (white arrow); (C) Thickening of the glenohumeral ligament (white arrows); (D) The articular capsule after release (white arrows); (E) Long head of the biceps tendon and rotator interval after release (white arrows); (F) Removal of the glenohumeral ligament (white arrow).
Drainage volume within 24 h after surgery
The postoperative drainage volume was 11.57 ± 2.86 ml in the TXA group, 19.35 ± 3.55 ml in the cocktail group, and 10.26 ± 2.49 ml in the TXA + cocktail group. No significant difference was found between in the TXA and TXA + cocktail group (P = 0.185). Postoperative drainage volume was significantly higher in the cocktail group compared with the TXA + cocktail group (F = 74.803, P = 0.000, Table 2).
Therapeutic efficacy of intra-articular infusion of cocktail combined with TXA following arthroscopic capsular release
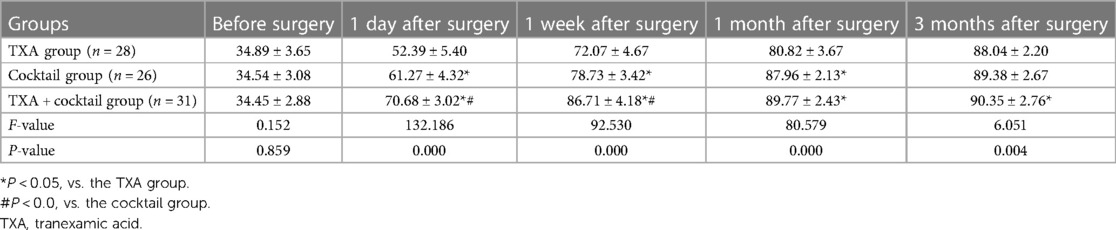
Comparison of the VAS scores between the three groups showed that at 1 day and 1 week after surgery, pain was more pronounced in the TXA group, which was significantly relieved in the cocktail and the cocktail + TXA groups, and pain relief was more apparent in the cocktail + TXA groups (P < 0.05). Good pain relief was achieved in all three groups at 1 and 3 months after surgery (Table 3).
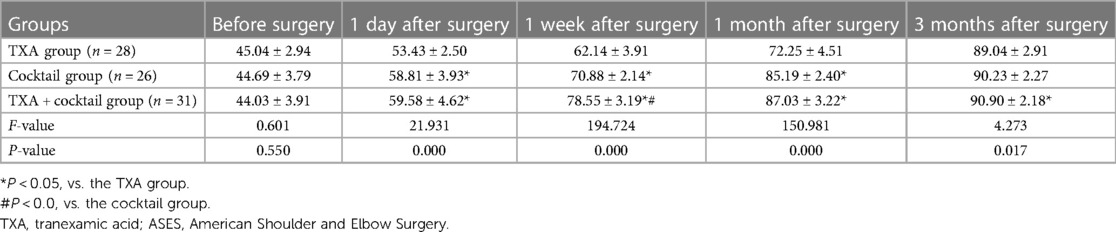
Comparison of the Neer scores between the three groups showed that the shoulder joint function was significantly limited in both the three groups before surgery. Shoulder joint function was improved to varying degrees in both the three groups at 1 day after surgery, obvious functional improvement was observed at 1 week after surgery in the three groups, and good level of shoulder joint function was achieved in the cocktail and the cocktail + TXA groups (P < 0.05). At 1 month and 3 months after surgery, good or excellent level of shoulder joint function was achieved in all the three groups. Patients in the cocktail + TXA groups obtained excellent functional recovery of the shoulder joint, which was better than the TXA group (P < 0.05, Table 4).
Comparison of the ASES scores between the three groups showed that at 1 day after surgery, a certain improvement in the shoulder joint function was achieved in all the three groups. At 1 week after surgery, the shoulder joint function was significantly improved in all the three groups, and the improvement was more apparent in the cocktail + TXA groups (P < 0.05). At 1 month after surgery, the cocktail group and the cocktail + TXA groups both showed good functional improvement. At 3 month after surgery, good functional recovery of the shoulder joint was observed in all three groups, the functional recovery of the shoulder joint was better in the cocktail + TXA group than that in the TXA group (P < 0.05, Table 5).
Shoulder ROM was significantly improved in all the three groups at different time points after surgery compared with before surgery, which was gradually increased over time. At 1week after surgery, patients in the cocktail + TXA groups obtained better shoulder ROM (P < 0.05). At 1 month after surgery, shoulder ROM was greater in the cocktail and the cocktail + TXA groups than that in the TXA group (P < 0.05), and the extension ROM was better in the cocktail + TXA groups than that in the cocktail group (P < 0.05). At 3 month after surgery, the ROM was better in the cocktail + TXA groups than that in the TXA group (P < 0.05), the ROM for internal rotation, external rotation and abduction was better in the cocktail + TXA group than that in the cocktail group (P < 0.05, Table 6).
Discussion
With the aging of the population in China, the number of patients who suffer from frozen shoulder has gradually increased. Frozen shoulder is the most common cause of shoulder pain, limited shoulder ROM and should stiffness in most middle-aged and older patients, which seriously affects patients' quality of life and their ability to carry out everyday activities (13). Frozen shoulder is a self-limiting condition with an average duration of 2–3 years, but a previous study has shown that 20%–50% of patients still have persistent pain and limited shoulder ROM after 3 years of the onset of frozen shoulder (14), and chronic pain over a long period of time can cause markedly stress on the patient's life and psychological well-being. With the development of society, people's demand for health is increasing, so patients' expectations of being cured of frozen shoulder have also gradually increased. At present, most patients are treated conservatively (15), such as partial closure, release and manipulation under anesthesia (16), and intra-articular injection of drugs (17). Most of patients experience significant temporary relief of symptoms after conservative treatment, with increased shoulder ROM, and improved shoulder function under the action of the drugs. However, with the absorption and metabolism of the drugs, local soft tissue adhesions and original lesions persist, resulting in recurrence and prolonged disease duration.
At present, arthroscopic capsular release is gradually popularized and applied in the treatment of frozen shoulder. Studies have shown that application of arthroscopic capsular release has good safety and efficacy, and can remove the proliferative synovium, adhesive fibrous tissues and damaged tissues in the shoulder joint, and repair damaged tissues (18, 19). The main reasons for pain and limited ROM caused by frozen shoulder are local inflammation and soft tissue adhesion. Therefore, after arthroscopic surgery, patients are required to perform shoulder exercises early to restore the shoulder ROM and improve shoulder function. However, surgical trauma can lead to traumatic pain, and general anti-inflammatory and analgesic drugs are not effective in relieving pain, resulting in poor cooperation with postoperative functional exercises and unsatisfactory surgical results. Some researchers have proposed that functional exercises can be performed after peripheral nerve block, this can obviously reduce postoperative pain, but postoperative nerve block often leads to partial dysfunction of the affected limb, and may have a detrimental effect on the patient's active functional exercise (20). Additionally, postoperative intra-articular bleeding may occur, poor drainage of intra-articular bleeding may lead to haematoma formation in the joint cavity, and aggravation of local inflammation, so as functional exercises progress, pain will gradually increase. And gradual organization of the hematoma will increase the risk of re-adhesion of shoulder joint after surgery.
The cocktail formula (21) has stable and long-lasting anti-inflammatory and analgesic effects, and is widely used in hip and knee arthroplasty to relieve postoperative local inflammation and pain, and enable patients to get out of bed early, restore limb function and achieve faster recovery. TXA (22) has a good postoperative hemostatic effect, and is often used in hip and knee arthroplasty to reduce postoperative intra-articular bleeding and accelerate postoperative recovery. Good clinical outcomes have achieved after using cocktail and TXA in hip and knee arthroplasty, but studies on the application of cocktail and TXA in patients with frozen shoulder after arthroscopic capsular release are rare. Therefore, in the present study, intra-articular infusion of cocktail combined with TXA was performed after arthroscopic capsular release to prevent postoperative pain and the risk of intra-articular bleeding.
In the present study, the surgical procedures were smooth in all the three groups, differences in postoperative bleeding, postoperative pain and postoperative functional recovery were compared between three groups after postoperative intra-articular infusion of cocktail alone, TXA alone, and cocktail plus TXA. There was no significant difference in the postoperative drainage volume between the TXA and the cocktail + TXA groups, but the postoperative drainage volume in the cocktail group was relatively increased, indicating that intra-articular infusion of TXA has a good preventive and control effect on postoperative bleeding, and can reduce postoperative intra-articular bleeding. The degree of postoperative pain in the cocktail and cocktail + TXA groups was significantly relieved, and patients could actively perform shoulder functional exercises with good cooperation, but patients in TXA group had obvious postoperative pain and had to perform functional rehabilitation exercises under intravenous analgesia. The results indicate that the cocktail formula has good anti-inflammatory and analgesic effects, which can relieve acute postoperative pain, accelerate the process of postoperative rehabilitation exercises, and promote the functional improvement of the shoulder. Additionally, the degree of pain was higher in the cocktail group than that in the cocktail + TXA group at 1 week after surgery. This may be related to the slower subsidence of inflammation caused by postoperative intra-articular bleeding in the cocktail group. The comprehensive analysis of shoulder joint function using Neer score, ASES score and shoulder ROM measurement showed that all patients in each group obtained significant functional improvement within 1 week after surgery, and the improvement was more obvious in the cocktail + TXA groups, followed by the cocktail group, indicating that at early time point after surgery, the cocktail combined with TXA can reduce postoperative pain and intra-articular bleeding, and accelerate postoperative functional rehabilitation exercise, so as to promote early postoperative functional recovery of the shoulder joint. At 1 month after surgery, excellent level of the shoulder joint function was achieved in the cocktail + TXA groups, good level of shoulder joint function was achieved in the cocktail group, and significant functional improvement was also found in the TXA group, indicating that with the subsidence of inflammation and the absorption of accumulated blood, the degree of pain gradually decreased, the functional exercises performed by patients gradually increased, and the shoulder joint function gradually improved. At 3 months after surgery, recovery of the shoulder joint function was basically good in all three groups, and the recovery was apparent in the cocktail + TXA groups, indicating that with the strengthening of functional exercises, patients in the three groups both achieved good functional recovery after surgery. The above-mentioned findings suggested that intra-articular infusion of cocktail combined with TXA plays a positive role in functional recovery at all time points after arthroscopic capsular release, especially at the early postoperative period.
Arthroscopic capsular release and intra-articular infusion of cocktail combined with TXA in the treatment of middle-aged and older patients with frozen shoulder have the following advantages: (1) less surgical trauma and faster postoperative recovery; (2) good safety and low incidence of postoperative complications; (3) accelerated postoperative rehabilitation: the combination of cocktail and TXA can reduce postoperative pain, and intra-articular bleeding, allow early functional exercises, thus enabling fast-track postoperative rehabilitation; (4) short length of hospital stay, obvious therapeutic efficacy, and high degree of patient satisfaction.
However, this study also has some limitations. This is a retrospective study, with a relatively short follow-up period. Further studies with larger sample size and long follow-up are needed to investigate the postoperative recurrence rate and the changes in shoulder joint function over time, and to further improve the treatment plan.
In conclusion, our findings suggest that arthroscopic capsular release and postoperative intra-articular infusion of cocktail combined with TXA has good safety and efficacy in the treatment of middle-age and older patients with frozen shoulder, which can reduce postoperative pain and intra-articular bleeding, promote early postoperative functional exercises, and accelerate early postoperative recovery. Intra-articular infusion of cocktail combined with TXA is a safe, effective and fast procedure for the treatment of frozen shoulder, that is worthy of clinical promotion.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
XB conceived and designed the study, collected and analyzed the data, and wrote the paper. FB, ZW, YZ, FL, QW were involved in data collection and analysis. All authors contributed to the article and approved the submitted version.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the First People's Hospital of Zunyi City (No. 2019-028). The patients/participants provided their written informed consent to participate in this study.
Ethics statement
This study was reviewed and approved by the Ethics Committee of the First People's Hospital of Zunyi City (No. 2019-028), and informed consent was obtained from the patients.
Funding
The study was supported by Zunyi Science and Technology Bureau & Zunyi First People’s Hospital Joint Science and Technology Research and Development Fund Project [Zunyi Kehe HZ Zi (2019) No.189] the Science and Technology Department of Guizhou Province [Qiankehe Foundation-ZK (2021) General No. 387]; and the Guizhou Provincial Health Commission (gzwjkj2018-2-05).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang QJ, Li BB, Dong LJ, Wang Y. Clinical observation of large manipulation release under brachial plexus anesthesia combined with small acupotomy on scapulohumeral periarthritis. Shiyong Yixue Zazhi. (2021) 37(14):1887–91.
2. Hagiwara Y, Kanazawa K, Ando A, Sekiguchi T, Yabe Y, Takahashi M, et al. Contracted joint capsule affects labral and chondral lesions in patients with frozen shoulder. Knee Surg Sports Traumatol Arthrosc. (2021) 29(8):2640–7. doi: 10.1007/s00167-021-06600-0
3. Ogul H, Tas N, Tuncer K, Polat G, Ogul Y, Pirimoglu B, et al. 3D volumetric MR arthrographic assessment of shoulder joint capacity in patients with primary adhesive capsulitis. Br J Radiol. (2019) 92(1094):20180496. doi: 10.1259/bjr.20180496
4. Vaishya R. The rise of shoulder arthroscopy. J Clin Orthop Trauma. (2019) 10(2):221. doi: 10.1016/j.jcot.2019.02.003
5. Gulbrandsen TR, Khazi ZM, Shamrock AG, An Q, Duchman K, Marsh JL, et al. The impact of resident involvement on postoperative complications after shoulder arthroscopy: a propensity-matched analysis. J Am Acad Orthop Surg Glob Res Rev. (2020) 4(9):e20.00138. doi: 10.5435/JAAOSGlobal-D-20-00138
6. Cui HD, Wang YH, Lv SJ. Arthroscopic capsular release combined with intra-articular infusion for the treatment of patients with frozen shoulder. Zhongguo Jiaoxing Waike Zazhi. (2020) 28(19):1815–7.
7. Li SZ, Zheng DZ, Liu J. Early analgesia of cocktail therapy after total knee arthroplasty with enhanced recovery after surgery program. Zhongguo Zuzhigongcheng Yanjiu. (2021) 25(18):2794–8.
8. Teratani T. Effect of cocktail therapy after arthroscopic rotator cuff repair: a randomized, double-blind trial. J Shoulder Elbow Surg. (2020) 29(7):1310–5. doi: 10.1016/j.jse.2020.03.004
9. Patel NK, Johns W, Vedi V, Langstaff RJ, Golladay GJ. Tourniquet and tranexamic acid use in total knee arthroplasty. Arthroplast Today. (2020) 6(2):246–50. doi: 10.1016/j.artd.2020.02.007
10. Granados ACU, Campos AT, Agustín MR, Lázaro AR, Donate MTE, Sauras ÁC. Influence of intra-articular tranexamic acid on cost savings and early functional outcomes in total knee arthroplasty. Rev Esp Cir Ortop Traumatol (Engl Ed). (2021) 65(4):285–93. doi: 10.1016/j.recote.2021.04.010
11. Xu YS, Yang WY, Lv R, Liu JW, Chen h, Cao XW. Effect of cocktail formula infusion on the recovery in patients with frozen shoulder after joint mobilization. Guangdong Yixue. (2018) 39(4):593–6.
12. Lin TY, Weng XJ, Wang HT, Wang J, Long Y. Therapeutic effect analysis of arthroscopy combined with intracavitary injection in treatment of rotator cuff injury combined with secondary frozen shoulder. Zhongguo Neijing Zazhi. (2019) 25(3):27–32.
13. Nesterenko VA, Karateev AE, Makarov MA, Byalik EI, Makarov SA, Byalik VE, et al. Data from clinical and instrumental examinations of patients with chronic pain in the shoulder joint. Rheumatol Sci Pract. (2020) 58(2):178–82. doi: 10.14412/1995-4484-2020-178-182
14. Mukherjee RN, Pandey RM, Nag HL, Mittal R. Frozen shoulder - a prospective randomized clinical trial. World J Orthop. (2017) 8(5):394–9. doi: 10.5312/wjo.v8.i5.394
15. Nakandala P, Nanayakkara I, Wadugodapitiya S, Gawarammana I. The efficacy of physiotherapy interventions in the treatment of adhesive capsulitis: a systematic review. J Back Musculoskelet Rehabil. (2021) 34(2):195–205. doi: 10.3233/BMR-200186
16. Iqbal M, Riaz H, Ghous M, Masood K. Comparison of spencer muscle energy technique and passive stretching in adhesive capsulitis: a single blind randomized control trial. J Pak Med Assoc. (2020) 70(12(A)):2113–8. doi: 10.5455/JPMA.23971
17. Koraman E, Turkmen I, Uygur E, Poyanlı O. A multisite injection is more effective than a single glenohumeral injection of corticosteroid in the treatment of primary frozen shoulder: a randomized controlled trial. Arthroscopy. (2021) 37(7):2031–40. doi: 10.1016/j.arthro.2021.01.069
18. Crimmins IM, Mulcahey MK, O’Brien MJ. Diagnostic shoulder arthroscopy: surgical technique. Arthrosc Tech. (2019) 8(5):e443–9. doi: 10.1016/j.eats.2018.12.003
19. Sedlinsch A, Berndt T, Rühmann O, Lerch S. Convalescence after arthroscopic capsular release in frozen shoulder. J Orthop. (2020) 20:374–9. doi: 10.1016/j.jor.2020.06.013
20. Surendran S, Patinharayil G, Karuppal R, Marthya A, Fazil M, Mohammed Ali S. Arthroscopic capsular release and continuous upper arm brachial block in frozen shoulder—a midterm outcome analysis. J Orthop. (2020) 21:459–64. doi: 10.1016/j.jor.2020.08.033
21. Qin HH, Yang Q, Zhang YZ. Application of tranexamic acid combined with intra-articular cocktail and TXA mixture perfusion in pri-mary total knee arthroplasty. Shiyong Yixue Zazhi. (2018) 34(8):1343–6.
Keywords: frozen shoulder, arthroscopy, cocktail, tranexamic acid, early postoperative
Citation: Bai X, Bai F, Wang Z, Zhang Y, Liu F and Wang Q (2023) Clinical efficacy of intra-articular infusion of cocktail combined with tranexamic acid in the treatment of middle-age and older patients with frozen shoulder following arthroscopic capsular release. Front. Surg. 10:1035054. doi: 10.3389/fsurg.2023.1035054
Received: 2 September 2022; Accepted: 30 March 2023;
Published: 3 May 2023.
Edited by:
Jaimo Ahn, University of Michigan, United StatesReviewed by:
Natale Calomino, University of Siena, ItalyVikash Raj, All India Institute of Medical Sciences, Deoghar (AIIMS Deoghar), India
© 2023 Bai, Bai, Wang, Zhang, Liu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaojin Bai MjIzNTI1NDI3OEBxcS5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Abbreviations TXA, tranexamic acid; VAS, visual analog scale; ASES score, the American society of shoulder and elbow surgery shoulder joint score; ROM, range of motion.
 Xiaojin Bai
Xiaojin Bai Fan Bai1
Fan Bai1