- 1Department of Orthopedic Surgery, The First Affiliated Hospital of Shandong First Medical University & Shandong Provincial Qianfoshan Hospital, Shandong Key Laboratory of Rheumatic Disease and Translational Medicine, Jinan, China
- 2School of Clinical Medicine, Shandong University, Jinan, China
Objective: To investigate the influencing factors of functional recovery after high tibial osteotomy (HTO).
Methods: A retrospective research was carried on 98 patients who underwent HTO between January 2018 and December 2020. In each case, the medial proximal tibial angle (MPTA), joint line convergence angle (JLCA), femoral tibial angle (FTA), hip-knee-ankle (HKA), weight bearing line (WBL) ratio of the knee joint, opening gap, opening angle, American knee society knee score (KSS), US Hospital for Special Surgery (HSS) score, Lysholm score, and Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) were measured to determine postoperative function and influential factors of pain through logistic regression analysis.
Results: The follow-up time was between 18 and 42 months after operation with an average of 27.66 ± 12.9 per month. Overall functional scores were significantly improved. The influencing factors that may affect the postoperative effect of HTO include age and preoperative WBL ratio of the knee joint (WBL%). After incorporating these two factors into the multivariate logistic regression analysis, for every 1 unit increase in the preoperative WBL%, the probability of postoperative HSS being superior is 1.06 times higher than before [Exp(β): 1.062, 95% CI: 1.01–1.1, p = 0.018]. For every year increase in age, the probability of an excellent HSS score after surgery was 0.84 times higher than that before surgery [Exp(β): 0.843, 95% CI: 0.718–0.989, p = 0.036]. Preoperative WBL% ≥ 14.37 was 17.4 times more likely to be rated as excellent postoperative HSS than that <14.37 [Exp(β): 17.406, 95% CI: 1.621–186.927, p = 0.018].
Conclusion: The postoperative functional scores of the patients significantly improved. Patients with preoperative WBL% ≥ 14.37% had better function after surgery.
Introduction
Osteoarthritis is a joint disease of great concern in the world today and is characterized by synovial hyperplasia and degeneration of articular cartilage with osteophyte formation that can eventually lead to pain, joint loss and disability (1). Degeneration of articular cartilage is most common in the knee joint, mainly in the medial space (2). HTO is based on the concept of force line rearrangement, redistributing weight-bearing and mechanical stress to less disrupted areas and reducing pain, improving function, and achieving articular cartilage recovery (3). This meets the needs of young patients who participate in sports or individuals who want to participate in high-demand activities to avoid prosthesis replacement (4). Historically, HTO was first reported in the 1960s by Jackson et al. (5). In terms of the trend of previous years, an increasing number of literatures related to HTO will be published in the future. HTO combined with cartilage restoration techniques, postoperative prognosis and outcome, and surgical technique research may be the future hotspots in the field of HTO research (6). The main purpose of this study was to re-evaluate the surgical outcome of HTO and the influencing factors affecting the surgical outcome (5, 7–9). This article retrospectively analyzes the clinical data of patients with knee osteoarthritis (KOA) treated with HTO and discusses the factors that affect the postoperative efficacy of HTO.
Materials and methods
General information
The research subjects were patients who underwent medial open HTO due to KOA in the First Affiliated Hospital of Shandong First Medical University from January 2018 to December 2020. The inclusion criteria consisted of (a) medial OA of the knee joint with varus deformity mainly in the tibia; (b) age ≤70 years old (higher requirements for future activities); (c) limited extension of the knee joint ≤10° (flexion > 90°); (d) BWI < 40; and (e) no subchondral bone abrasions. The exclusion criteria consisted of (a) patients with a history of lower extremity fracture or surgery on the operative side; (b) traumatic KOA; (c) combined nerve, muscle, or connective tissue diseases; and (d) patients with incomplete imaging parameters and those lost to follow-up.
Surgical methods
All operations were performed by the same group of physicians, and the anesthesia method used was either intraspinal or general anesthesia. The decision to perform knee arthroscopy is determined according to whether there is a combination of meniscal injury and cartilage injury before surgery. In each case, a 6–8 cm straight incision was made on the medial side of the proximal tibia, exposing the proximal flat joint line layer by layer until the medial tibia and posterior tibial crest were exposed. Two parallel 2.0 cm Kirschner wires were inserted in at 3.5 cm from the upper edge of the tibia and 1.5 cm from the outer edge of the tibia to the upper edge of the tibia to penetrate the contralateral cortex. The horizontal osteotomy was performed close to the distal end of the two Kirschner wires, and approximately 1.0 cm from the lateral cortex was reserved as the hinge point. The starting point of the coronal osteotomy was above the insertion point of the patellar tendon and 110° between the horizontal osteotomy to ensure that the patellar tendon insertion remained attached to the distal side of the osteotomy after the osteotomy was corrected. It was necessary to slowly spread through the bone knife or spreader to achieve the predetermined spread angle in the preoperative plan. The force line was determined by force line rod and x-ray fluoroscopy, and the TomoFix locking plate (Johnson & Johnson) was used for fixation. Different osteotomy gap treatment methods were selected according to the opening angle and bone quality.
Radiographic measurements and follow-up
Radiographic measurements by an independent observer using standard full-length anteroposterior radiographs of both lowed extremities were obtained preoperatively and at least 18 months postoperatively during clinical follow-ups. Imaging parameters included MPTA, JLCA, FTA, HKA, WBL%, postoperative opening gap, and postoperative opening angles (see Figures 1, 2). The postoperative HSS scores were divided into two clinically relevant categories according to the results: excellent ≥85 points and poor <85 points (10).
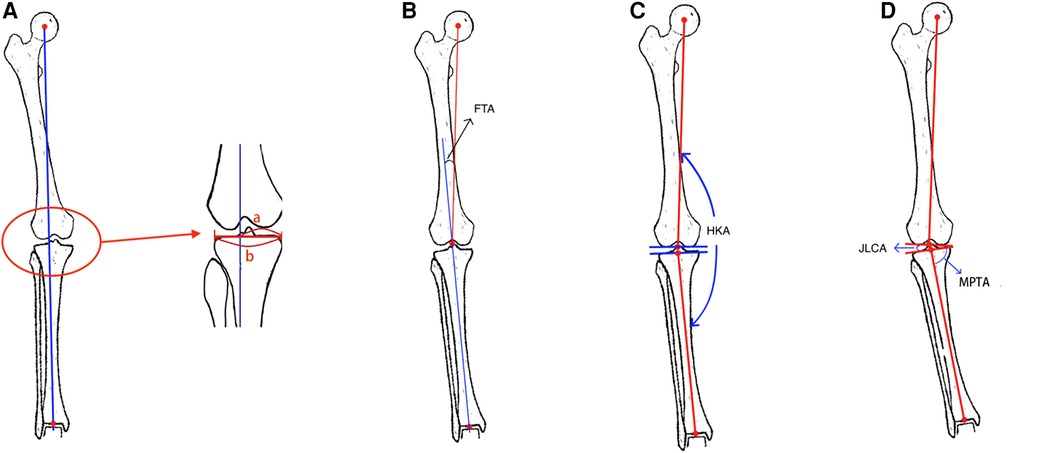
Figure 1. (A) Measurement of the WBL: the line connecting the center of the femoral head and the center of the ankle joint is WBL. Measurement of the WBL ratio of the knee joint: a is the distance between the direction of the medial cortex of the tibia along the proximal tibial joint and the force line, b is the distance between the medial and lateral tibial cortex, the ratio of a and b is WBL ratio of the knee joint. (B) Measurement of the FTA: the angle between the extension line of the tibial mechanical axis and the femoral mechanical axis is the tibiofemoral angle. (C) Measurement of the HKA: the angle between the mechanical axis of the tibia and the mechanical axis of the femor is the hip-knee-ankle angle. (D) Measurement of the JLCA: The angle formed between the running direction lines of the opposite joints of the same joint. Measurement of the MPTA: Draw the running direction line of the proximal tibia joint, and draw a straight line from the center point of the ankle joint to the center point of the knee joint on the tibia knee joint line, and the angle between the two lines is MPTA.
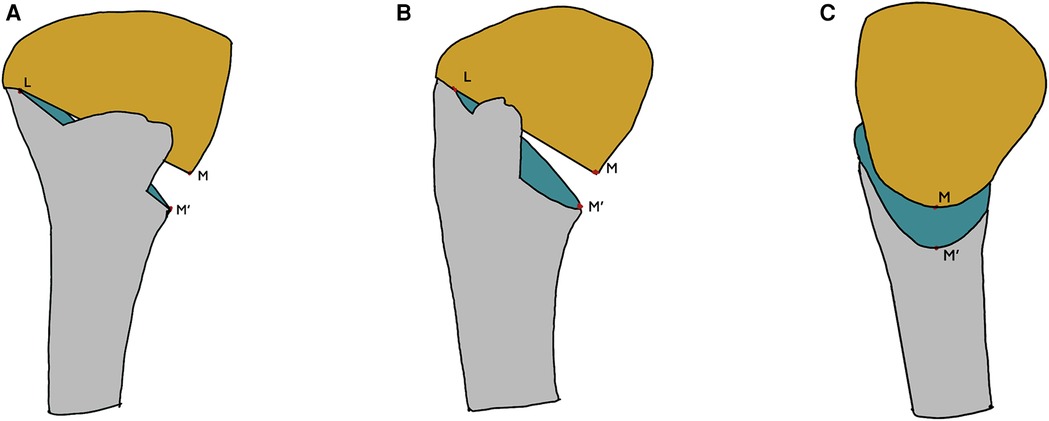
Figure 2. (A) Front view. (B) 45° projection position view. (C) Lateral view. L is the hinge point, M and M’ are the inner cortical points of the upper and lower sections, respectively. Opening gap: the distance between MM’. Opening angle: the angle between LM and LM’.
Statistical methods
Continuous variables, such as preoperative and postoperative imaging parameters and scores, were tested for normal distribution using the Shapiro-Wilk test. Paired t-tests were performed on normally distributed measurement data, and the results were expressed as mean ± standard deviation (). The paired Wilcoxon signed rank test was used to measure skewed distribution of data, and the paired Wilcoxon signed rank test was used, and the results were expressed as medians (interquartile range) [M (IQR)]. Univariate logistic regression analysis was performed on patients’ general demographic data and various imaging parameters. If the independent variable p < 0.05 in the univariate logistic regression appeared in the analysis results, the variable was included in the multiple logistic regression analysis. And differences were considered statistically significant at p < 0.05 to determine which variables were the factors affecting the outcome of the functional score and the degree of preoperative pain. All statistical analyses were performed with IBM SPSS Statistics25.
Results
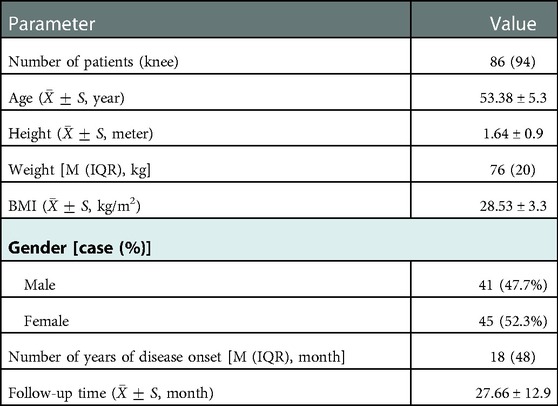
Follow-up
During this period, a total of 98 patients received HTO, 10 patients were lost to follow-up, and 2 patients had incomplete imaging parameters. Finally, 86 patients with 94 affected limbs were included in this study. Among them were 8 bilateral cases, all of which were staged operations (41 males and 45 females; average age of 53.38 ± 5.3 years old) (see Table 1).
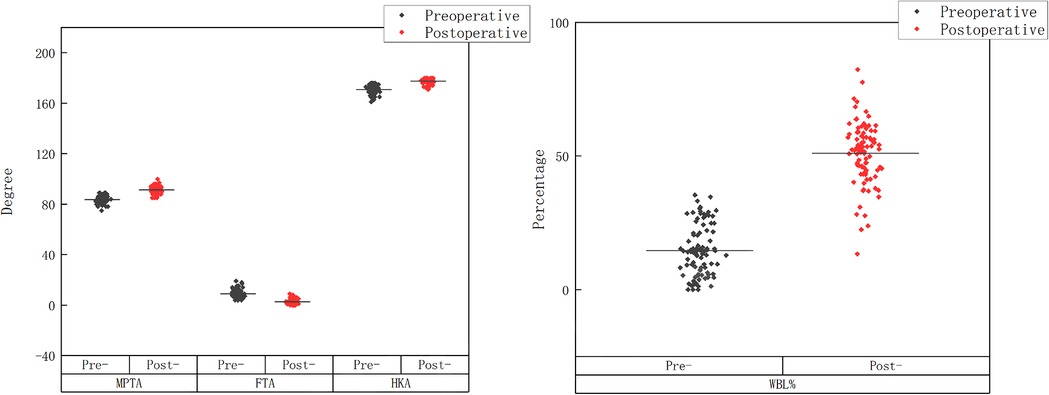
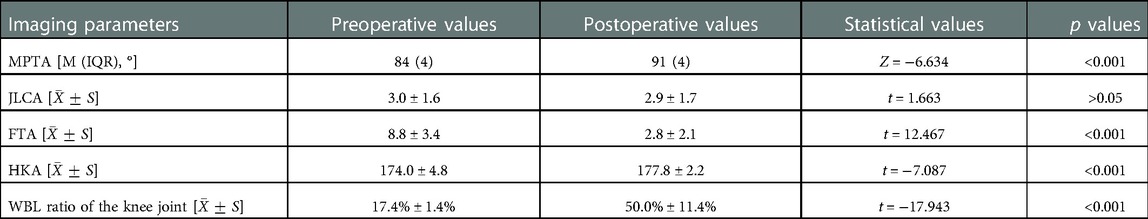
Radiographic improvement
The postoperative imaging indicators were significantly improved compared to the preoperative ones (see Table 2, Figures 3, 4). The postoperative MPTA increased, the FTA angle decreased, the HKA angle increased, the WBL% increased, and the differences were statistically significant.
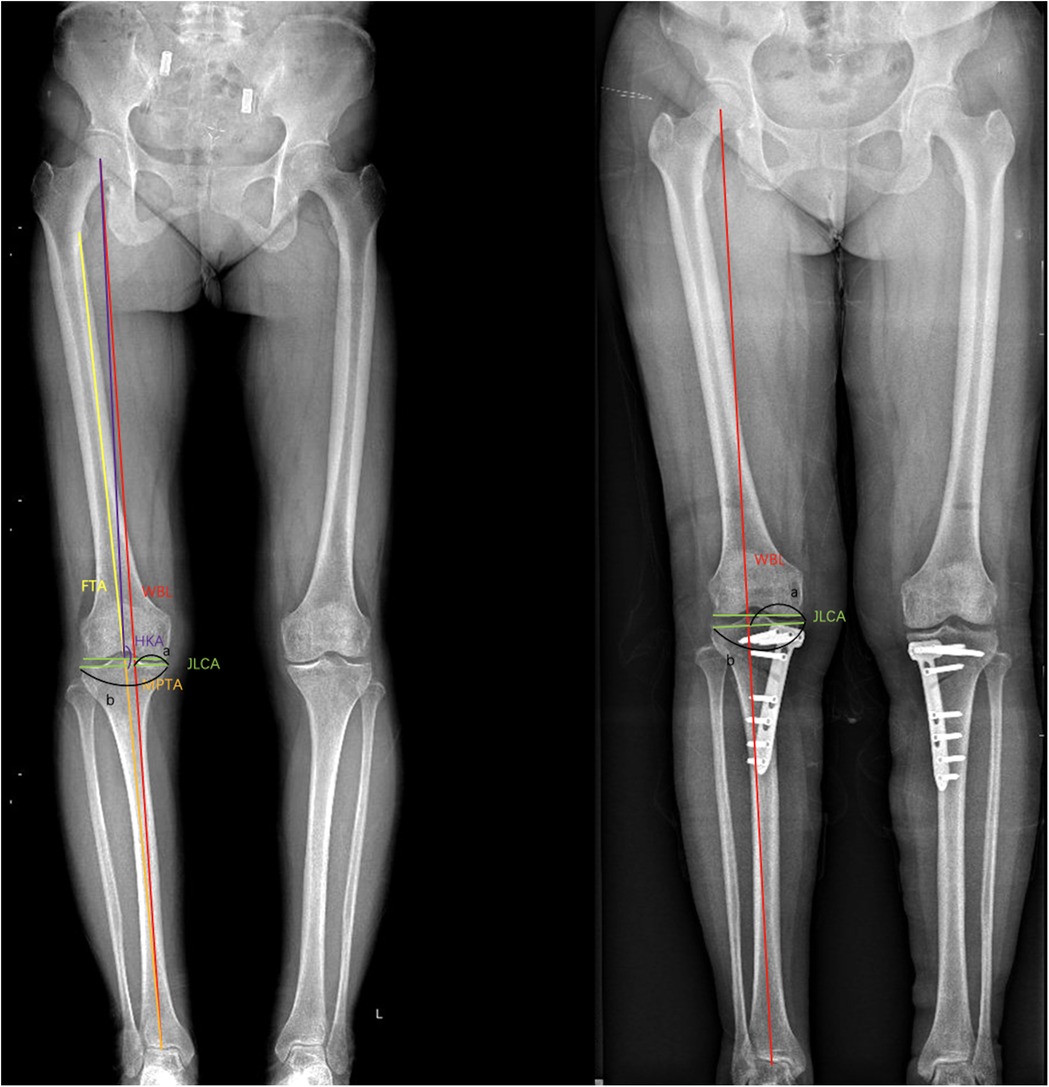
Figure 3. Preoperative and postoperative x-ray comparison. Preoperative WBL ratio of the knee joint: 45%, postoperative WBL ratio of the knee joint: 58%. After operation, the radiographic parameters were significantly improved.
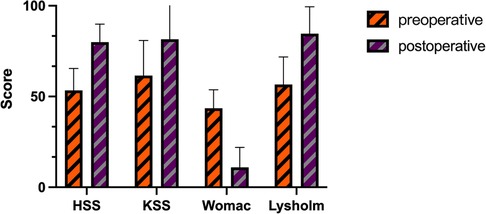
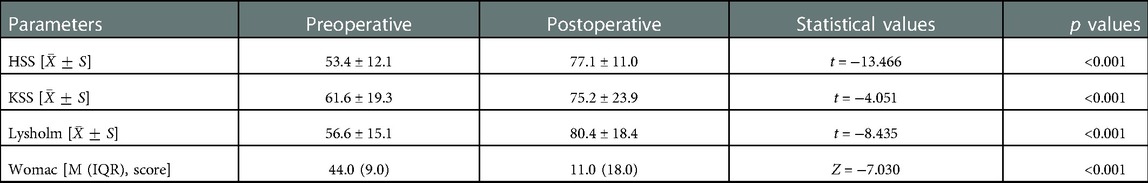
Postoperative clinical function comparison
The HSS, KSS, and Lysholm scores significantly increased before and after HTO, the WOMAC score decreased, the difference was statistically significant (see Table 3 and Figure 5), and knee function improved.
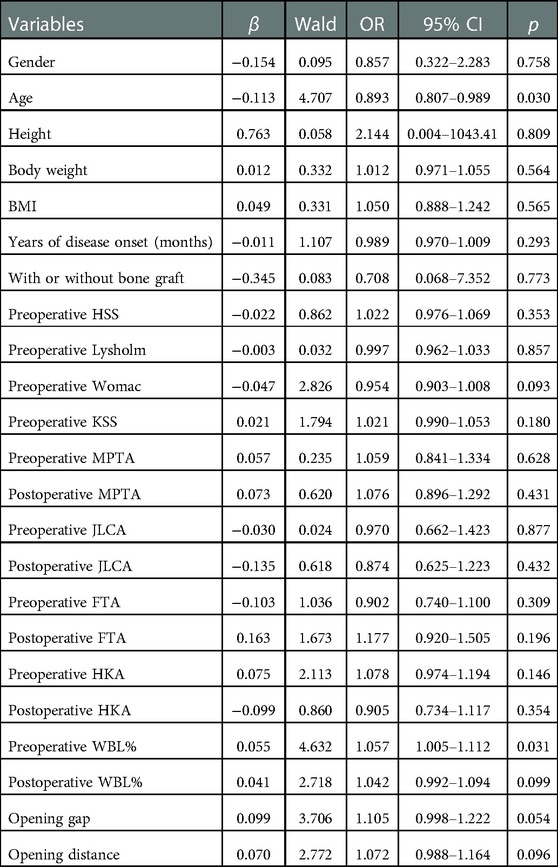
Influencing factors of function after HTO
General information of the patients (age, gender, height, weight, BMI, and age of onset), imaging parameters (MPTA, JLCA, FTA, HKA and WBL%), and whether bone grafting was performed during surgery independent variable screening through univariate logistic regression analysis. Taking the postoperative HSS score category as the following outcome variables, the p value was set to 0.05, and the corresponding independent variables were screened out: age (p = 0.016) and preoperative WBL% (p = 0.031; see Table 4).
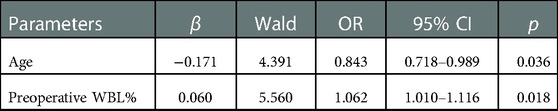
The age and preoperative WBL% were included in the multiple logistic regression analysis, and a statistically significant difference was found between age and the preoperative WBL%. According to the multiple logistic regression analysis, each unit increase in the preoperative WBL% was associated with a 1.06-fold increase in the probability of being classified as excellent in the postoperative HSS score [Exp(β): 1.062, 95% CI: 1.01–1.1, p = 0.018; see Table 5].
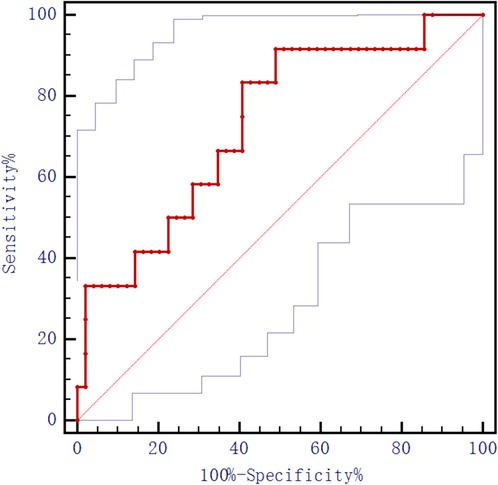
For each year increase in age, the postoperative HSS score was 0.84 times more likely to be classified as excellent [Exp(β): 0.843, 95% CI: 0.718–0.989, p = 0.036]. Taking the postoperative HSS score as a state variable and age as a test variable, an ROC analysis was performed on age, and the result found that the area under the curve was 0.323 with no cutoff value found. Taking the postoperative HSS score as the status variable and the preoperative WBL% as the test variable, the ROC analysis of the preoperative WBL ratio in the knee joint showed an area under the curve of 0.731 with a cut-off value of 14.37% (see Figure 6). The preoperative WBL% continuous variables were classified (≥14.37% and <14.37%) and included in the multiple logistic regression analysis. This study has confirmed that the preoperative WBL% ≥ 14.37% had an excellent probability of a postoperative HSS score compared with the preoperative WBL% < 14.37% 17.4 times [Exp(β): 17.406, 95% CI: 1.621–186.927, p = 0.018; see Table 6] with is a statistically significant difference.
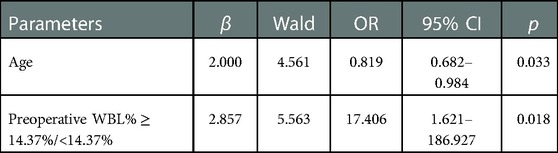
Table 6. Results of multiple logistic regression analysis of age and preoperative WBL% ≥ 14.37%/preoperative WBL% < 14.37%.
Conclusion
The present study found significant improvement in functional scores and imaging in patients after HTO, and found a certain correlation between age, preoperative knee WBL ratio and postoperative functional recovery. Although reports on the influencing factors of postoperative function after HTO are gradually increasing, the influencing factors of postoperative function are still inconclusive. Compared with UKA, HTO reduces pain and improves function by changing the position of the force line and improves the conditions for cartilage repair (11). HTO can effectively solve the biomechanical and structural abnormalities in patients with knee osteoarthritis, improve the knee joint function and quality of life of patients, and slow down the progression of degenerative osteoarthritis (12, 13). Because the lateral closed wedge high tibial osteotomy has a higher chance of complications and a higher risk of damage to the common peroneal nerve, the main application is the medial open wedge high tibial high osteotomy (14, 15). Different surgical methods may have an impact on postoperative function, for the convenience of comparison, this paper only collects patients with medial wedge HTO. Several research studies, including the one conducted by Fujisawa et al. (16), found that the adjustment of postoperative alignment of 62.5% is beneficial in improving the effect of HTO. Martay (17) proposed that the WBL% interval should be adjusted to 50%–60% from the inside to the outside because this is more conducive to postoperative recovery. Yoon (11) reported that the postoperative WBL% can be used as a predictor of deterioration of patellofemoral cartilage status. Although there are many reports on the WBL%, the relationship between preoperative knee WBL ratio and postoperative function of patients is lacking. To a certain extent, this study has illustrated the association between the preoperative WBL% and patient function after HTO, meaning that patients with a higher preoperative WBL% have better postoperative function. The ROC curve analysis of preoperative WBL% and the inclusion of multiple logistic regression analysis showed that the critical value of the WBL% was 14.37%. This is statistically significant with the probability of good recovery for preoperative WBL ≥ 14.37% was 17.4% for WBL < 14.37%. This phenomenon may be related to the degree of preoperative deformity and preoperative function. The more severe the medial cartilage wear before operation, the greater the degree of extra-articular deformity, and the greater the correction angle during operation, the greater the functional improvement after operation.
Previous studies have shown that age is one of the influencing factors affecting the function after HTO (18). Attcan (19) conducted follow-ups for patients over and under 50 years of age that underwent HTO and found that the knee joint scores differed significantly with age and that the difference in follow-up mechanical axis between each age group was also statistically significant. This paper draws similar conclusions. The probability of an excellent postoperative effect is 0.82 times higher for each additional year of preoperative age. However, no relevant critical value was obtained in the ROC curve analysis, and this may be related to the small sample size and short follow-up times.
Consistent with other research findings, it was observed that the clinical function scores and postoperative radiographic parameters of patients after HTO were significantly improved compared with those before operation. In addition, we found that patients with higher preoperative WBL ratios of the knee joint will have better joint function after an operation and that older patients will have worse postoperative results. There are certain limitations to the conduct of this research. First, our study was a retrospective case study, which inherently suffers from various sources of bias, including selection bias, measurement and evaluation bias, and loss to follow-up. Another, our sample size is not large enough. Third, this is a short-term follow-up study and does not provide medium- or long-term follow-up results.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
SL and ZZhao conceptualized and managed the study. ZY, JH, CZ, JW and ZZhang acquired the data. ZY, YG analyzed the data and wrote the original draft. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Natural Science Foundation of Shandong Province (ZR2019MH130).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mobasheri A, Saarakkala S, Finnilä M, Karsdal MA, Bay-Jensen A-C, van Spil WE. Recent advances in understanding the phenotypes of osteoarthritis. F1000Res. (2019) 8(F1000 Faculty Rev):2091–102. doi: 10.12688/f1000research.20575.1
2. Messner K, Maletius W. The long-term prognosis for severe damage to weight-bearing cartilage in the knee: a 14-year clinical and radiographic follow-up in 28 young athletes. Acta Orthop Scand. (1996) 67(2):165–8. doi: 10.3109/17453679608994664
3. Ishimatsu T, Takeuchi R, Ishikawa H, Yamaguchi Y, Maeyama A, Osawa K, et al. Hybrid closed wedge high tibial osteotomy improves patellofemoral joint congruity compared with open wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. (2019) 27(4):1299–309. doi: 10.1007/s00167-019-05350-4
4. Liu X, Chen Z, Gao Y, Jin Z. High tibial osteotomy: review of techniques and biomechanics. J Healthc Eng. (2019) 2019:1–12. doi: 10.1155/2019/8363128
5. Jackson J, Waugh W. Tibial osteotomy for osteoarthritis of the knee. J Bone Joint Surg Br Vol. (1961) 43(4):746–51. doi: 10.1302/0301-620X.43B4.746
6. Zhang H, Fan Y, Wang R, Feng W, Chen J, Deng P, et al. Research trends and hotspots of high tibial osteotomy in two decades (from 2001 to 2020): a bibliometric analysis. J Orthop Surg Res. (2020) 15(1):512. doi: 10.1186/s13018-020-01991-1
7. Robertsson O, Lidgren L. Surgery for knee osteoarthritis in younger patients. Acta Orthop. (2010) 81(2):161–4. doi: 10.3109/1745367090341318
8. Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am Vol. (1993) 75(2):196–201. doi: 10.2106/00004623-199302000-00006
9. Wright J, Heck D, Hawker G, Dittus R, Freund D, Joyce D, et al. Rates of tibial osteotomies in Canada and the United States. Clin Orthop Relat Res. (1995) 319:266–75. doi: 10.1097/00003086-199510000-00029
10. Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am Vol. (1976) 58(6):754–65. doi: 10.2106/00004623-197658060-00003
11. Yoon T-H, Choi CH, Kim S-J, Kim S-H, Kim N-H, Jung M. Effect of medial open-wedge high tibial osteotomy on the patellofemoral joint according to postoperative realignment. Am J Sports Med. (2019) 47(8):1863–73. doi: 10.1177/0363546519851096
12. Kuriyama S, Watanabe M, Nakamura S, Nishitani K, Tanaka Y, Sekiguchi K, et al. Large medial proximal tibial angles cause excessively medial tibiofemoral contact forces and abnormal knee kinematics following open-wedge high tibial osteotomy. Clin Biomech. (2020) 80:105190. doi: 10.1016/j.clinbiomech.2020.105190
13. van Egmond N, Janssen D, Hannink G, Verdonschot N, van Kampen A. Biomechanical comparison of two different locking plates for open wedge high tibial osteotomy. J Orthop Sci. (2018) 23(1):105–11. doi: 10.1016/j.jos.2017.09.014
14. Tabrizi A. A short term follow up comparison of genu varum corrective surgery using open and closed wedge high tibial osteotomy. Malays Orthop J. (2013) 7(1):7. doi: 10.5704/MOJ.1303.009
15. Schubert I, Ferner F, Dickschas J. The effect of open-wedge and closed-wedge high tibial osteotomies on the tibial posterior slope—a study of two hundred seventy-nine cases. Int Orthop. (2020) 44(6):1077–82. doi: 10.1007/s00264-020-04499-9
16. Fujisawa Y, Masuhara K, Shiomi S. The effect of high tibial osteotomy on osteoarthritis of the knee. An arthroscopic study of 54 knee joints. Orthop Clin North Am. (1979) 10(3):585–608. doi: 10.1016/S0030-5898(20)30753-7
17. Martay JL, Palmer AJ, Bangerter NK, Clare S, Monk AP, Brown CP, et al. A preliminary modeling investigation into the safe correction zone for high tibial osteotomy. Knee. (2018) 25(2):286–95. doi: 10.1016/j.knee.2017.12.006
18. Horn A, Boskovic V. Predictors of early recurrence following high tibial osteotomy for infantile tibia vara. Int Orthop. (2021) 45(5):1233–8. doi: 10.1007/s00264-020-04808-2
Keywords: unicompartmental osteoarthritis, medial knee osteoarthritis, high tibial osteotomy, surgical effect, influencing factors
Citation: Yan Z, Gu Y, He J, Zhang C, Wang J, Zhang Z, Zhao Z and Li S (2023) Early surgical outcomes and influencing factors of high tibial osteotomy. Front. Surg. 10:1022636. doi: 10.3389/fsurg.2023.1022636
Received: 18 August 2022; Accepted: 2 January 2023;
Published: 16 February 2023.
Edited by:
Angelo Gabriele Aulisa, Bambino Gesù Children's Hospital (IRCCS), ItalyReviewed by:
Luca Basiglini, Bambino Gesù Children's Hospital (IRCCS), ItalyYou Zhao, University Hospital Regensburg, Germany
© 2023 Yan, Gu, He, Zhang, Wang, Zhang, Zhao and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shufeng Li c2h1ZmVuZ2xpc2RAMTI2LmNvbQ== Zhang Zhao Mjg2NkBzZGhvc3BpdGFsLmNvbS5jbg==
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Zhaolong Yan1
Zhaolong Yan1 Yange Gu
Yange Gu Chenyang Zhang
Chenyang Zhang Jianye Wang
Jianye Wang Shufeng Li
Shufeng Li