
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 25 January 2023
Sec. Orthopedic Surgery
Volume 10 - 2023 | https://doi.org/10.3389/fsurg.2023.1003022
This article is part of the Research Topic Surgical Innovation and Advancement in Orthopedics View all 57 articles
 Zijun Cai1,2,†
Zijun Cai1,2,† Yuntao Yang1,2,†
Yuntao Yang1,2,† Di Liu1,2
Di Liu1,2 Wenhao Lu1,2
Wenhao Lu1,2 Linyuan Pan1,2
Linyuan Pan1,2 Miao He1,2
Miao He1,2 Wenqing Xie1,2
Wenqing Xie1,2 Dengjie Yu1,2
Dengjie Yu1,2 Hengzhen Li1,2
Hengzhen Li1,2 Hongfu Jin1,2
Hongfu Jin1,2 Yusheng Li1,2*
Yusheng Li1,2* Wenfeng Xiao1,2*
Wenfeng Xiao1,2*
Purpose: To determine the effect of local infiltration anesthesia (LIA) at the donor site combined with a femoral nerve block (FNB) on short-term postoperative pain, functional outcomes, and rehabilitation after arthroscopic hamstring tendon autograft anterior cruciate ligament reconstruction (ACLR).
Methods: This study was a single center, randomized controlled trial. Seventy-three subjects with ACL rupture were enrolled. Participants were randomly allocated to two groups, 47 in the experimental group (Group A) and 26 in the control group (Group B). All operations were performed under FNB. In Group A, 10 ml of 1% ropivacaine was injected precisely at the hamstring donor site. Patients in Group B were treated with the same amount of saline. Preoperatively and postoperatively, pain scores based on the numerical rating scale (NRS) and consumption of opioids were recorded. In addition, knee functions were assessed by the International Knee Documentation Committee Subjective Knee Form (IKDC), the Lysholm score, and the Knee injury and Osteoarthritis Outcome Score (KOOS) preoperatively and postoperatively at 1 and 3 months. In addition, we applied the KNEELAX3 arthrometer to evaluate the stability of the knee preoperatively and postoperatively so that subjective and objective knee conditions were obtained to help us assess knee recovery in a comprehensive manner.
Results: The hamstring donor-site block reduced pain within the first 12 postoperative hours. There were no significant differences between two groups in pain intensity preoperatively and equal to or greater than 24 hours postoperatively. Furthermore, there were no differences between the groups concerning knee functions preoperatively or in the short-term follow-up at 1 and 3 months.
Conclusion: LIA at the donor site can effectively improve the early postoperative pain of patients after ACLR and reduce the use of opioids without affecting the functional outcomes of the surgery.
ACL injuries may account for 50% of sports-related injuries in high school athletes (1). Although there is not a single epidemiological survey that summarizes populations around the world, we can be certain, based on several local studies, that the incidence rate of ACL injuries is high worldwide. In the United States, it affects more than two hundred thousand people each year, with direct and indirect costs greater than $7 billion annually (1). In Sweden, the overall incidence of ACL injury was 78 per 100,000 (2). In Finland, the total ACL injury incidence was about 23.3 per 100,000 person-years (3). Currently, ACLR is standard practice for athletes that wish to return to high-level activities. Hamstring tendon graft ACLR is one of the most common and effective orthopedic procedures. The all-inside technique (AIT) for ACLR is becoming increasingly popular because of its anatomical adaptability, low invasiveness, and rapid rehabilitation (4).
With the progress of modern medicine, the patient's comfort during the treatment process has been continuously considered. The pain has been recognized the fifth vital sign and it has received increasing attention in clinical diagnosis and treatment practice (5). Pain is one of the prominent complaints in patients after ACLR. Compared with other types of orthopedic sports surgery, ACLR causes not only more significant but also longer-lasting pain to patients, often throughout the entire rehabilitation process (6). Reasonable pain management can improve outcomes and a higher pain is often associated with more difficulties during rehabilitation, even in daily activities (7). Pain, together with other factors, are related to knee function.
A reasonable perioperative analgesia approach is necessary for faster rehabilitation and satisfaction. Currently, intravenous or oral opioids are frequently prescribed for postoperative pain control following ACLR (8). However, if the use of these drugs is not strictly controlled, it may not only increase the risk of various complications but also increase the possibility of drug dependence, abuse, and overdose (8). In the USA, it is estimated that opioid-related complications cost $78.5 billion every year (8, 9). There were approximately 49,680 deaths caused by opioid overdose in 2019, accounting for 70.6% of all drug overdose deaths (8, 10). There has been an increasing call to strengthen the management of opioid use and to take into account their possible harm to patients (8, 10). It is urgent to develop a novel and suitable approach to reduce postoperative pain in patients after ACLR that does not rely on opioids.
According to our clinical experience, the main sources of pain after ACLR include the following three points: the skin incision, the graft fixation positions, and the graft donor site. The former two cannot be avoided, so we focused on relieving the pain at the donor site. FNB has been shown to be an effective method for relieving postoperative pain (11). We believe that combining analgesia at the donor site with FNB may result in better outcomes. To date, there have been several relevant studies in favor of our perspective (12–15). However, few studies have compared the effect of injecting or not injecting local anesthesia to perform donor-site block on the postoperative condition of patients. With this study, we hope to fill the gap in knowledge in this area.
Pain assessment is usually derived from subjective statements rather than objective measurements (16). Thus, it is conceivable that the same level of pain may be described as different subjective feelings by different individuals. This problem does exist, but few scholars have suggested that it needs to be addressed in regard to pain-related research. To obtain a more objective pain assessment, a new preoperative evaluation program was introduced. The cold pressor test (CPT) is a research tool that can induce pain perception in humans (17). In this way, we were able to obtain the pain threshold and pain tolerance of each patient before the operation, which helped eliminate the influence of individual differences in pain perception on the study findings (17).
We aimed to determine the effect of LIA at the donor site combined with a FNB on short-term postoperative pain and the functional outcomes and rehabilitation after arthroscopic hamstring tendon autograft ACLR. We hypothesized that the combination of FNB and LIA can achieve better analgesic effect, but it is not enough to directly impact the postoperative rehabilitation speed.
This research was designed as a randomized controlled trial. Patients were designed to be randomized to undergo either a hamstring donor-site block or isotonic sterile water of equal volume, in an around 2:1 ratio. A permuted block randomization scheme was used with block sizes of 3. All operations were performed by the same experienced orthopedic surgeon in our hospital. The study protocol was approved by the institutional ethics committee. Informed consent for participation in the study was obtained from all patients before randomization.
Patients 15–50 years of age who were diagnosed with ACL rupture, usually confirmed by means of history, physical examination, and magnetic resonance imaging, were screened for eligibility. Participants were randomly allocated to two groups (Figure 1). Baseline data were collected. A total of 73 (originally 76) patients with an American Society of Anesthesiologists (ASA) physical status classification of I–III who satisfied the inclusion criteria of our study underwent arthroscopic ACLR using hamstring tendon autografting for ACL tears. Among them, 47 (excluding 3 withdrawing from the study) patients in Group A were given a 1% 10 ml ropivacaine injection right at the donor site, while the other 26 patients in Group B were given the same volume of saline.
The inclusion criteria were primary ACLR and a healthy contralateral knee. Exclusion criteria included refusal of surgical treatment; severe concomitant injuries; concurrently performed other different surgical procedures; weight less than 35 kg; body mass index (BMI) greater than 45 kg/m2; ASA physical class greater than 4; allergy to local anesthetics; preexisting neurologic deficit; undergoing revision surgery; any opioid use within the previous 3 months; inability to understand the NRS; or suffering from serious or chronic conditions that may have an impact on surgical treatment, postoperative recovery or regular follow-up. After returning to the ward after surgery, tramadol was orally administered if the pain at rest exceeded 3 on NRS. A unified analgesic scheme and postoperative rehabilitation plan were adopted during the perioperative period.
The IKDC, the Lysholm score, and the KOOS were used to examine the functional outcomes preoperatively, at the 1-month follow-up, and at the 3-month follow-up. In addition, the degree of anterior tibial translocation was measured with a KNEELAX3 arthrometer (Monitored Rehab Systems, Haarlem, The Netherlands) (18) preoperatively, at the 1-month follow-up, and at the 3-month follow-up. As KT-1000/2000, it was also considered valid and reliable, with very similar operating process (19, 20). Both knees were measured with different anterior force with the maximum of 132 N applied to the proximal tibia at 20° of knee flexion in a supine position. Actually, this helped quantify the Lachman test as a result. The difference in the degree of anterior translocation between the nonaffected side and affected side was expressed as in millimeters (18). To minimize any susceptibility bias, all evaluations were performed by the same person. According to the KNEELAX3 instructions, it is recommended that patients be measured within grade 3 within 6 months after surgery.
Pain management success was assessed by the consumption of opioids (tramadol) during the patient's hospitalization and pain scores on an NRS, an 11-point scale where 0 indicates no pain and 10 indicates the worst imaginable pain (21), which is considered comparable to the visual analog scale (VAS) (22). Opioids were provided only if the patient made a strong request and the NRS score was higher than 3. Patients were asked to give a score based on NRS preoperatively and at 2, 4, 6, 12, 24, 48 h, 1 month, and 3 months postoperatively. CPT was performed before surgery.
AIT for ACLR is becoming increasingly popular and it has been described extensively in previous papers (23, 24). Here, only those parts relevant to the research topic are retained.
All patients received a preoperative FNB using an ultrasound-guided technique. One of the highlights of this study is the process of harvesting the hamstring tendon and subsequent local anesthesia. The medial tibial tuberosity incision was made where the hamstring tendon is removed with our self-developed tendon retriever. The surgeon initially obtained the tendon, while not moving the retriever, and slowly inject the 10 ml of ropivacaine. Then, the analgesic continued to be injected while withdrawing the retriever, and finally, the ropivacaine would fill the entire donor site (Figure 2).

Figure 2. Precise donor-site block steps; (A) ready to retrieve tendon, (B) tendon removed, (C) ropivacaine injected right at the deepest point of tendon removal site, (D) the whole tendon removal site full of ropivacaine.
We designed a novel tendon retriever capable of precisely injecting local anesthetics, as shown in Figure 3. The outer tube body has a hollow channel and a positioning wire perforation along the axis and a plurality of anesthesia channels extending along the axis and with outlets located at different heights of the outer tube body. The inner end of the tendon collection rod body has an opening ring that can form a closed ring with the outer tube body, and the tendon collection rod body has a penetration hole extending along the axis. The inner end of the positioning member has a C-shaped positioning ring, a flexible cross-file is provided inside the C-shaped positioning ring. One set of rings is fixed to the C-shaped positioning ring, and the other set of rings is set on the C-shaped positioning ring. The restriction structure set in the perforation of the positioning wire is used to clamp or release the positioning member, and the C-shaped positioning ring is fixed to the end of the positioning rod.
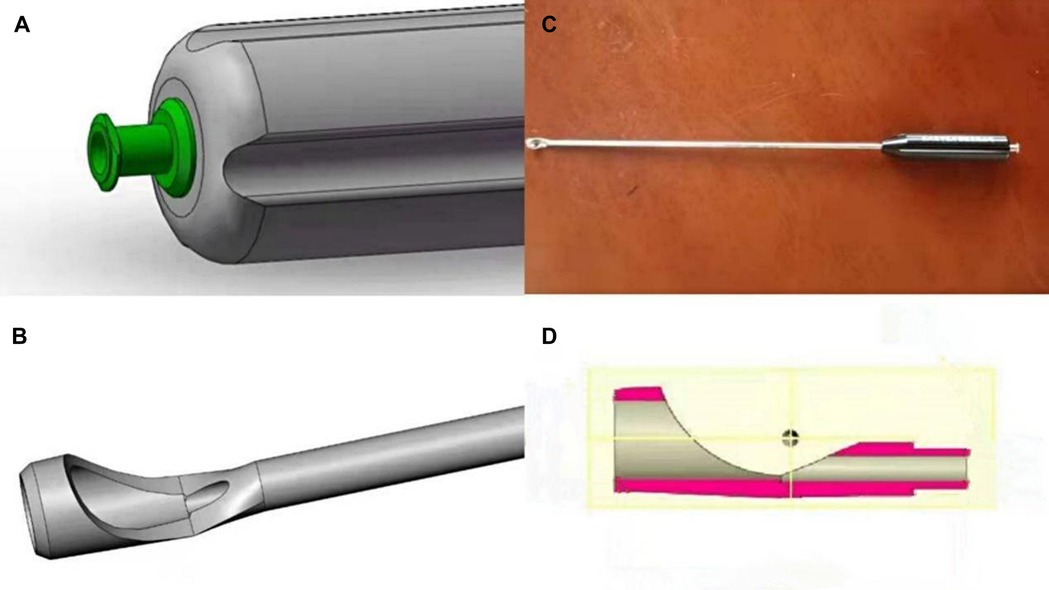
Figure 3. Our novel tendon retriever; (A) end of tendon retriever, (B) top of tendon retriever, (C) overall view, (D) internal structure..
The CPT was first created and utilized as a tool by Edgar A. Hines, Jr. to study blood pressure variability (17). During the test, the patient needs to put the whole palm of their hand into cold water that is constantly circulating through ice. Since this test is based on hemodynamic response to peripheral cold stimulation, it doesn't matter which hand people would use. The experience is made more painful by the presence of the circulating pump that prevents the buildup of a warmer layer of water around the forearm. With the extension of time, the pain in the palm of the hand will become more intense until the patient cannot tolerate it and pulls their hand out of the water. Previous studies have shown that the CPT can be used to help surgeons better cope with pain problems in patients (25). CPT can be used not only to predict the degree of postoperative pain, but also to help standardize the obtained pain data (25).
The general flow of this test is as follows. A bucket full of cold water with ice should be prepared to keep the temperature constant. The water temperature was monitored (maintained at 4°C), as a 2°C difference in temperature can affect tolerance time and pain intensity (25). In addition, the bucket needs to be equipped with a device that allows the water to circulate continuously to avoid the water temperature in the area near the palm of the hand being slightly higher than the preset water temperature. In a word, as the ice melted, the surface temperature of the water was maintained, and in addition the circulating pump could make the temperature anywhere in the water the same. The participant would be briefed by the observer on how to take the test in advance. The patient will be asked to extend their hand into the ice water to ensure that the water floods the straight wrist transverse striae while the observer starts timing. The participant informs the observer immediately when their hand sensation changes from cold to pain, and the time difference between the beginning of the test and the first report of pain is recorded as that participant's “pain threshold” (25, 26). They are instructed to voluntarily withdraw their hand at the point at which the pain becomes “unbearable”—the time between the beginning of the test and this voluntary withdrawal is recorded as that participant's “pain tolerance” (25, 26). To ensure safety, the test is forcibly terminated if the participant does not remove their hand within 3 min.
Within 1 week after surgery, complete knee extension was required during bed rest, quadriceps contraction and straight leg raising training were performed, ankle flexion and extension activities were performed, and passive knee flexion was performed. Partial weight-bearing with crutches when walking on the ground; passive flexion of the knee joint to 90 degrees was started on the 8th day, and full weight-bearing standing and walking with detached crutches were trained; at the end of the 2nd week, passive flexion of the knee joint to 120 degrees and full weight-bearing walking were required; fixed bicycle exercises, terminal extension and balance exercises were performed at 3–6 weeks; at 7–12 weeks, active and passive knee flexion, range of motion consistent with the unaffected side, knee extension and resistance knee extension, and full squatting were performed. Full return to full activities of daily living started 3 months and gradual return to sports started 9 months.
Calculation of the sample size was based on an expected difference of two points on the NRS score between the groups. With a power of 0.80 and α = 0.05, a sample size of at least 25 patients per group was obtained. SPSS 26.0 software was used for statistical analysis of the data. Measures were tested for normality using the D'Agostino test, and normally distributed indicators are expressed as the mean ± standard deviation (SD) and compared between groups using the independent samples t-test; nonnormally distributed indicators are expressed as the median and interquartile range (IQR) and compared between groups using the Mann–Whitney U test. Multifactorial logistic regression analysis was performed to assess the correlation between NRS scores and local anesthesia or not within 48 h preoperatively and postoperatively after adjusting for confounders. Statistical data are expressed as percentages (%), and comparisons between groups were made by the chi-square test or Fisher's exact probability method. P < 0.05 was considered a statistically significant difference.
From 2020 to 2022, 73 patients were included in this study. The baseline characteristics were similar between the two groups concerning gender, age, BMI, time from injury to hospital admission, pain tolerance, and intraoperative tourniquet application time (Table 1). However, the pain threshold was higher in the LIA group (55.87 ± 6.18 vs. 50.85 ± 4.42, P < 0.001). Within the first 12 h after surgery, pain level was significantly lower in Group A than in Group B (P < 0.05). There was no difference in pain scores preoperatively and at the time point greater than or equal to 24 h postoperatively (Table 2), but the consumption of opioids during the patient's hospitalization showed a significant difference between groups (P < 0.05) (Table 3). Since we collected objective data on pain perception (CPT), so standardizing the scores of the NRS based on pain perception could be considered. After regression analysis, there was no change in the conclusion in terms of pain (Table 4). This study showed no differences in functional outcomes between groups at all follow-up time points (Tables 5–7). No complications related to the anesthesia or nerve block were observed.
The most important finding of this study was a statistically significant reduction in postoperative pain scores with the additional use of donor-site block. The significant complications of ACLR consist of infection, hematoma or hemarthrosis, failure of the surgery, etc. (27). However, based on our experience in clinical practice, cases most commonly seen contain quadriceps weakness, restriction of knee flexion or extension, and donor-site or incision pain. Pain can often lead to the exacerbation of the first two issues. Not only is pain subjectively troubling for the patient, but it can also objectively hinder rehabilitation efforts, lead to a decreased range of motion, and have an overall negative effect on surgical outcomes (14).
To date, few studies have been conducted on the effect of LIA at the donor site combined with FNB on short-term postoperative pain and functional outcomes after arthroscopic hamstring tendon autograft ACLR. The reduction of pain level was obvious within 12 hours after ACLR but this effect was no longer working beyond the period. In addition, the additional donor site block after FNB did not affect any other subjective or objective outcomes. However, an assumption should not be made arbitrarily that donor-site LIA did not have any positive effects on functional recovery since the first assessment of function was at 1 month postoperatively. Less pain is often accompanied by a greater range of motion. Additional block could provide comfort to the affected region and a greater range of motion during the immediate postoperative course.
The study we conducted was similar to Bushnell et al. (14) in 2010, and they found a remarkable decrease in VAS score among patients treated with both LIA and FNB compared with FNB alone. Our study makes the same conclusions. However, their study may be associated with some bias because of the absence of opioid consumption records, an insufficient follow-up period, and a lack of baseline pain scores preoperatively. Therefore, we assessed preoperative pain scores as well as the pain threshold and pain tolerance, extended the follow-up time, recorded opioid consumption, and further took into consideration subjective and objective functional outcomes to improve the study design to eventually make a more comprehensive evaluation of the effect of a donor site block. Another highlight of our study is the utilization of the novel tendon retriever that we invented, which ensures precise anesthesia at the donor site. As the core variable in this study, it deserves to be made as accurate as possible. The tools and methods for implementing LIA have not been harmonized between different studies, which may have an impact on the correctness of the trial conclusions. Previous similar studies have always ignored this point.
Considering that gender is one of the confounders of pain (28), the baseline characteristics of the subjects were analyzed. The slight baseline difference between the two groups probably did not bias our results.
The best choice of anesthetic for local infiltration has not yet been determined, with bupivacaine and ropivacaine being commonly used. Bupivacaine has a half-life of 3.5 h, whereas ropivacaine is a long-acting local anesthetic with a similar structure to bupivacaine and a half-life of 4.2 h. Ropivacaine has the advantage of being less toxic, and its blockade of sensation is stronger than its block against movement (29), which is why we selected it.
It was expected that the range of motion would be highly associated with pain intensity. Based on our observations of postoperative patients, patients with less pain did have a greater knee range of motion and were more comfortable moving their knees. Therefore, range of motion was not specifically described in this study.
Less early postoperative pain could be observed without the use of a tourniquet during routine knee arthroscopy (30), suggesting the potential impact of the application of a tourniquet intraoperatively on postoperative rehabilitation, but some studies have noted that a tourniquet use of less than approximately 2 h had no effect on the strength of the lower extremity and pain scores (31, 32). There was no significant difference in the mean tourniquet times between the two groups in this study, so this potential interfering factor was eliminated. It is worth noting that Guler et al. (33) showed that a local anesthetic injection is more beneficial after tourniquet release. Thus, future studies may consider investigating the timing of the injection as a factor in pain control.
Several papers previously reported an abnormal sensation in the lower extremities after surgery. This complication often occurs because of injury to the lateral sural cutaneous or saphenous nerve due to the incision or intraoperative retraction (14). In our study, there were no neurological problems related to the use of the donor-site injection technique.
There are some limitations of this study. There was no intentional blinding of patients, doctors, or nurses in the postanesthesia care unit. Moreover, patient satisfaction during the whole course, speed of recovery, and the immediate postoperative condition of the body and knee could not be presented merely according to our study data.
The simplicity of the donor-site block technique warrants its extensive application. It could effectively improve the early postoperative pain of patients after ACLR and reduce the use of opioids, without affecting follow-up functional outcomes. Future related studies with larger samples may help confirm its beneficial effect.
The data supporting the findings of this study are available from the corresponding author, upon reasonable request.
The studies involving human participants were reviewed and approved by the institutional ethics committee of Xiangya Hospital of Central South University (approval number: 202110105).
ZC: design, manuscript writing. YY: provision of study material, collection, and assembly of data. WX (Wenqing Xie), MH, DL, and DY were responsible for revising the article and data acquisition. WL and HL: provision of relevant references. LP and HJ: data analysis and interpretation. WX (Wenfeng Xiao) and YL: conception, financial support, administrative support. All authors contributed to the article and approved the submitted version.
This work was supported by the National Natural Science Foundation of China (No. 82272611, 82072506, 81874030), National Clinical Research Center for Geriatric Disorders (Xiangya Hospital, No. 2021KFJJ02), National Clinical Research Center for Orthopedics, Sports Medicine and Rehabilitation (No. 2021-NCRC-CXJJ-PY-40), Provincial Clinical Medical Technology Innovation Project of Hunan (No. 2020SK53709), Innovation-Driven Project of Central South University (No. 2020CX045), the Independent Exploration, Innovation Project for Postgraduate Students of Central South University (No. 2021zzts1030, 2021zzts1037, 2021zzts1024) and the Hunan Provincial Innovation Foundation for Postgraduate (CX20210360).
Everyone who contributed significantly to this study has been listed.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Kaeding CC, Léger-St-Jean B, Magnussen RA. Epidemiology and diagnosis of anterior cruciate ligament injuries. Clin Sports Med. (2017) 36(1):1–8. doi: 10.1016/j.csm.2016.08.001
2. Nordenvall R, Bahmanyar S, Adami J, Stenros C, Wredmark T, Felländer-Tsai L. A population-based nationwide study of cruciate ligament injury in Sweden, 2001–2009: incidence, treatment, and sex differences. Am J Sports Med. (2012) 40(8):1808–13. doi: 10.1177/0363546512449306
3. Weitz FK, Sillanpää PJ, Mattila VM. The incidence of paediatric acl injury is increasing in Finland. Knee Surg Sports Traumatol Arthrosc. (2020) 28(2):363–8. doi: 10.1007/s00167-019-05553-9
4. Yang YT, Cai ZJ, He M, Liu D, Xie WQ, Li YS, et al. All-inside anterior cruciate ligament reconstruction: a review of advance and trends. Front Biosci. (2022) 27(3):91. doi: 10.31083/j.fbl2703091
5. Rogers MP, Kuo PC. Pain as the fifth vital sign. J Am Coll Surg. (2020) 231(5):601–2. doi: 10.1016/j.jamcollsurg.2020.07.508
6. Marques FDS, Barbosa PHB, Alves PR, Zelada S, Nunes R, de Souza MR, et al. Anterior knee pain after anterior cruciate ligament reconstruction. Orthop J Sports Med. (2020) 8(10):2325967120961082. doi: 10.1177/2325967120961082
7. Tichonova A, Rimdeikienė I, Petruševičienė D, Lendraitienė E. The relationship between pain catastrophizing, kinesiophobia and subjective knee function during rehabilitation following anterior cruciate ligament reconstruction and meniscectomy: a pilot study. Medicina. (2016) 52(4):229–37. doi: 10.1016/j.medici.2016.07.005
8. Sayegh ET, Otto TS, Garvey KD, Martin A, Lowenstein NA, Matzkin EG. Defining the opioid requirement in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg Glob Res Rev. (2022) 6(1). doi: 10.5435/JAAOSGlobal-D-21-00298
9. Maiese BA, Pham AT, Shah MV, Eaddy MT, Lunacsek OE, Wan GJ. Hospitalization costs for patients undergoing orthopedic surgery treated with intravenous Acetaminophen (iv-apap) plus other iv analgesics or iv opioid monotherapy for postoperative pain. Adv Ther. (2017) 34(2):421–35. doi: 10.1007/s12325-016-0449-8
10. Blendon RJ, Benson JM. The public and the opioid-abuse epidemic. N Engl J Med. (2018) 378(5):407–11. doi: 10.1056/NEJMp1714529
11. Behera SK, Gunupuru B, Sahu L, Das S. Peripheral nerve stimulator versus ultrasound-guided femoral nerve block for knee arthroscopy procedures: a randomized controlled trial. Cureus. (2022) 14(11):e32043. doi: 10.7759/cureus.32043
12. Kristensen PK, Pfeiffer-Jensen M, Storm JO, Thillemann TM. Local infiltration analgesia is comparable to femoral nerve block after anterior cruciate ligament reconstruction with hamstring tendon graft: a randomised controlled trial. Knee Surg Sports Traumatol Arthrosc. (2014) 22(2):317–23. doi: 10.1007/s00167-013-2399-x
13. Faunø P, Lund B, Christiansen SE, Gjøderum O, Lind M. Analgesic effect of hamstring block after anterior cruciate ligament reconstruction compared with placebo: a prospective randomized trial. Arthroscopy. (2015) 31(1):63–8. doi: 10.1016/j.arthro.2014.07.024
14. Bushnell BD, Sakryd G, Noonan TJ. Hamstring donor-site block: evaluation of pain control after anterior cruciate ligament reconstruction. Arthroscopy. (2010) 26(7):894–900. doi: 10.1016/j.arthro.2009.11.022
15. Yung EM, Brull R, Albrecht E, Joshi GP, Abdallah FW. Evidence basis for regional anesthesia in ambulatory anterior cruciate ligament reconstruction: part iii: local instillation analgesia-a systematic review and meta-analysis. Anesth Analg. (2019) 128(3):426–37. doi: 10.1213/ane.0000000000002599
16. Karos K, Alleva JM, Peters ML. Pain, please: an investigation of sampling bias in pain research. J Pain. (2018) 19(7):787–96. doi: 10.1016/j.jpain.2018.02.011
17. Lamotte G, Boes CJ, Low PA, Coon EA. The expanding role of the cold pressor test: a brief history. Clin Auton Res. (2021) 31(2):153–5. doi: 10.1007/s10286-021-00796-4
18. Li B, Wang GB, Wang YF, Zhou BZ. Effects of pre-operative knee laxity on clinical outcomes after partial anterior cruciate ligament reconstruction. Knee. (2018) 25(3):445–52. doi: 10.1016/j.knee.2018.02.012
19. Taketomi S, Inui H, Yamagami R, Kawaguchi K, Nakazato K, Kono K, et al. Length of the tendon within the tibial tunnel affects tibial tunnel widening following anatomic anterior cruciate ligament reconstruction using a bone-patellar tendon-bone graft. J Knee Surg. (2020) 33(5):445–51. doi: 10.1055/s-0039-1681064
20. Taketomi S, Inui H, Yamagami R, Shirakawa N, Kawaguchi K, Nakagawa T, et al. Bone-patellar tendon-bone autograft versus hamstring tendon autograft for anatomical anterior cruciate ligament reconstruction with three-dimensional validation of femoral and tibial tunnel positions. J Knee Surg. (2018) 31(9):866–74. doi: 10.1055/s-0037-1615813
21. Tada M, Yamada N, Matsumoto T, Takeda C, Furukawa TA, Watanabe N. Ultrasound guidance versus landmark method for peripheral venous cannulation in adults. Cochrane Database Syst Rev. (2022) 12(12):Cd013434. doi: 10.1002/14651858.CD013434.pub2
22. Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. (2005) 14(7):798–804. doi: 10.1111/j.1365-2702.2005.01121.x
23. Wilson AJ, Yasen SK, Nancoo T, Stannard R, Smith JO, Logan JS. Anatomic all-inside anterior cruciate ligament reconstruction using the translateral technique. Arthrosc Tech. (2013) 2(2):e99–e104. doi: 10.1016/j.eats.2012.12.002
24. Schurz M, Tiefenboeck TM, Winnisch M, Syre S, Plachel F, Steiner G, et al. Clinical and functional outcome of all-inside anterior cruciate ligament reconstruction at a minimum of 2 years’ follow-up. Arthroscopy. (2016) 32(2):332–7. doi: 10.1016/j.arthro.2015.08.014
25. MacLachlan C, Shipton EA, Wells JE. The cold pressor test as a predictor of prolonged postoperative pain, a prospective cohort study. Pain Ther. (2016) 5(2):203–13. doi: 10.1007/s40122-016-0056-z
26. Birnie KA, Petter M, Boerner KE, Noel M, Chambers CT. Contemporary use of the cold pressor task in pediatric pain research: a systematic review of methods. J Pain. (2012) 13(9):817–26. doi: 10.1016/j.jpain.2012.06.005
27. de Sa D, Shanmugaraj A, Weidman M, Peterson DC, Simunovic N, Musahl V, et al. All-inside anterior cruciate ligament reconstruction-a systematic review of techniques, outcomes, and complications. J Knee Surg. (2018) 31(9):895–904. doi: 10.1055/s-0038-1627446
28. Schindler M, Schmitz S, Reinhard J, Jansen P, Grifka J, Benditz A. Pain course after total knee arthroplasty within a standardized pain management concept: a prospective observational study. J Clin Med. (2022) 11(23). doi: 10.3390/jcm11237204
29. Winnie L, Kao YH, Liao CC, Tamura T, Chang ML, Hsieh KY. Comparative analgesic efficacies of ropivacaine and bupivacaine for postoperative Rectus sheath block in paediatric abdominal surgery: a meta-analysis of randomized controlled trial and retrospective cohort studies. Pain Res Manag. (2021) 2021:5535730. doi: 10.1155/2021/5535730
30. Kirkley A, Rampersaud R, Griffin S, Amendola A, Litchfield R, Fowler P. Tourniquet versus no tourniquet use in routine knee arthroscopy: a prospective, double-blind, randomized clinical trial. Arthroscopy. (2000) 16(2):121–6. doi: 10.1016/s0749-8063(00)90024-0
31. Nicholas SJ, Tyler TF, McHugh MP, Gleim GW. The effect on leg strength of tourniquet use during anterior cruciate ligament reconstruction: a prospective randomized study. Arthroscopy. (2001) 17(6):603–7. doi: 10.1053/jars.2001.24854
32. Johnson DS, Stewart H, Hirst P, Harper NJ. Is tourniquet use necessary for knee arthroscopy? Arthroscopy. (2000) 16(6):648–51. doi: 10.1053/jars.2000.4826
Keywords: anterior cruciate ligament, pain, post-operative rehabilitation, arthroscopy, femoral nerve block, local infiltration analgesia
Citation: Cai Z, Yang Y, Liu D, Lu W, Pan L, He M, Xie W, Yu D, Li H, Jin H, Li Y and Xiao W (2023) The effect of hamstring donor-site block for functional outcomes and rehabilitation after anterior cruciate ligament reconstruction. Front. Surg. 10:1003022. doi: 10.3389/fsurg.2023.1003022
Received: 25 July 2022; Accepted: 2 January 2023;
Published: 25 January 2023.
Edited by:
Paphon Sa-ngasoongsong, Mahidol University, ThailandReviewed by:
Hong Chen, First Affiliated Hospital of Chongqing Medical University, China© 2023 Cai, Yang, Liu, Lu, Pan, He, Xie, Yu, Li, Jin, Li and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yusheng Li bGl5dXNoZW5nQGNzdS5lZHUuY24= Wenfeng Xiao eGlhb3dlbmZlbmdAY3N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.