- 1Unit of Plastic and Hand Surgery, CHUV University hospital of Lausanne – UNIL, University of Lausanne, Lausanne, Switzerland
- 2Unit of Plastic and Hand Surgery, Hôpital le Bocage CHRU Dijon, Dijon, France
Objectives: To assess long-term sexual outcome and quality of life after perineal reconstruction by pedicled anterolateral thigh (ALT) flaps after Fournier's gangrene. Postoperative surgical outcomes were assessed; quality of life and sexual function were assessed at long term follow-up (>12 months) with 2 scientifically validated questionnaires.
Methods: We conducted a retrospective analysis of a prospectively maintained database. Long-term sexual function and quality of life were assessed by standardized questionnaires. Descriptive statistics were conducted.
Results: 8 patients were included in our study, 5 patients responded to quality of life and sexual function analysis. Surgical outcomes were in line with literature: one minor complication (minor dehiscence requiring a skin graft), one major complication (flap loss, requiring a second, contralateral flap) occurred. No reconstructive failure occurred. Average time to complete wound healing was 17 days (SD ±5). Quality of life scores over 70/100 in four out of five categories; social function was rated lowest: patients reported very few residual complaints. Sexual outcome analysis emphasizes the positive impact of the reconstruction. As expected, Fournier's Gangrene heavily affected patient's sexual health.
Conclusions: Perineal reconstruction with ALT shows excellent quality of life, and good sexual health outcomes. Currently the lack of reliable and relatable data leads to the impossibility to compare different reconstructive procedures. We emphasize that assessing sexual function and quality of life after perineal reconstruction is paramount to weigh reconstructive success.
Introduction
Fournier's Gangrene is a necrotizing soft tissue infection of the perineum, with mortality rates reported as high as 45% (1, 2). Similar to other fulminant necrotizing soft tissue infections, radical debridement with broad spectrum antibiotics is considered the only effective treatment, albeit causing vast soft tissue defects (3). The perineum is a particularly challenging region to reconstruct, given the presence of genito-urinary organs with complex functions to preserve and the proximity of the anus, with therefore increased risk of bacterial contamination. Furthermore, the perineum presents a complex three-dimensional geometry including both convex and concave structures, all involved in dynamic movements.
Reconstructive techniques have been classified over the years following a “reconstructive ladder”, from simplest, e.g. healing by secondary intention or granulation, to most complex, free flap reconstruction. Given the extensive soft tissue defects encountered after Fournier gangrene, specific reconstructive techniques are usually necessary.
Various techniques have been described in perineal reconstruction (4). Skin grafts are invaluable adjuncts to many extensive soft tissue defects, having the advantage of being simple and fast to perform, having and being available to many patients in simple technical settings (5). Grafts do however carry substantial drawbacks in a complex region such as the perineum, both in shape and function. Indeed, the grafted skin usually forms a fibrous, rigid scar with minimal pliability, and remains very sensible to mechanical stress because of its lack of subcutaneous tissue and dermis (6). Moreover, the take rate of grafts in humid, convex/concave areas is oftentimes plagued by graft infection or maceration, leading to partial reconstructive failure (7).
Many disadvantages are avoided using local flaps (8, 9). Albeit more complex, flap surgery offers ample, stable tissue where needed. Literature has reported various donor sites, with a historical preference towards abdominal musculo-cutaneous flaps, namely the vertical rectus abdominis muscle flap (VRAM). Although very potent, it suffers severe abdominal donor site morbidity, with reported herniation rates of up to 66% were described after VRAM harvest (10, 11).
On the other hand, the thigh offers stable, pliable skin with minimal donor site morbidity. The anterolateral thigh flap described by Song has been described in perineal reconstruction from 1992 onwards (12, 13). It allows for a large skin paddle to be harvested and easily reaches the perineum (14). Flaps up to 8 cm allow for primary closure of the thigh and the largest defects can be covered either by larger flaps, or by bilateral flaps if necessary, harvested simultaneously by two teams. If bulk is needed due to particularly aggressive debridement, tailored amounts of vastus lateralis muscle can be harvested to fill dead space along the fascio-cutaneous flap as a combined ALT-VL pedicled flap (14). Harvested muscle has no significant functional impact at long term (15). This ductility made this flap the preferred choice for complex perineal reconstruction in patients who underwent abdomino-perineal resection for oncologic reasons in our institution (16).
The use of ALT flaps after Fournier's gangrene has been described previously; however scarce data describes long-term outcomes, especially functional outcomes (e.g., seating discomfort, walking disorders or chronic pain). Czymek et al. described outcomes and quality of life measures after Fournier's gangrene, however not specifically describing which reconstructive intervention was performed (17). No Fournier-specific study examined perineal reconstruction with thigh flaps measuring quality of life or functional results.
The aim of this retrospective study is to review the functional outcomes and complications in patients undergoing perineal reconstruction after Fournier gangrene with ALT flaps, focusing not only on surgical aspects but also on quality of life, functional and sexual recovery after surgery.
Patients and methods
Data gathering and outcome definition
We analyzed the prospectively maintained department database on perineal reconstruction with cases treated 1 January 1999 to 31 January 2021, accounting for 41 reconstructions. Patients who underwent oncological resections were excluded, including in our analysis only patients with histopathologically confirmed signs of necrotizing gangrene of the genitoperineal area (Fournier's gangrene). Out of these, we excluded all patients with superficial wounds treated by split thickness skin graft, patients with excessive skin laxity allowing for fasciocutaneous advancement flaps or local perforator flaps, or patients who were non eligible for ALT flaps (i.e., anterior access hip replacement, femoral fractures, etc …) and therefore reconstructed with other major musculocutaneous flaps such as myocutaneous gracilis or VRAM. Patient selection occurred chronologically, to reduce patient selection bias.
Data was compiled from the institutions' electronic medical records; patient characteristics, comorbidities, defect size, operation duration, postoperative and long-term complications as well as follow-up duration were assessed.
Surgical outcomes were defined as described in previous series characterizing perineal reconstructions by ALT-VL flap (16). We recorded flap related complications, defined as “major” in case of total or partial flap loss, major wound dehiscence at donor or recipient site involving more than a third of the incision length and persistent perineal dead space requiring additional reconstructive surgical procedures during follow-up. Minor complications comprised local infections resolving by antibiotic therapy alone, seroma or hematoma not requiring drainage, dehiscence at donor or recipient site involving less than a third of the incision length that healed with conservative treatment, debridement, split-thickness skin graft (STSG) or flap advancement. We defined “wound healing” as intact scar/skin, and considered the total healing time if the patient underwent a synchronous secondary surgical procedure.
Functional outcomes
We analyzed long-term outcomes (i.e., >12 months after the initial procedure). Exclusion criteria were defined as loss of follow-up, refusal or inability to answer the questionnaires. We selected two functional questionnaires drafted by the EORTC (European Organization for Research and Treatment of Cancer): QLQ C30 V3 and QLQ-SHQ C22 V1 for global quality of life and sexual health, respectively. QLQ C30 is well established in oncological quality of life studies (18), and SHQ is in the final validation stages for sexual quality of life assessment (19). Although validated in oncological patients undergoing colorectal operations, the similar issues faced by the patients we reconstructed (i.e., large perineal defects, complex recovery, potential loss of function) are well examined by both these questionnaires. Scoring and data analysis was performed according to the published questionnaire summary (19, 20).
Institutional written consent was obtained from all patients regarding retrospective use of data for scientific studies, including use of photographic documentation. The study was designed according to the guidelines of the 1975 Helsinki Declarations.
Surgical technique
Serial debridement was performed until stabilization of the patient in order to obtain a clean, stable wound. Debridement focuses on suprafascial structures, i.e., skin and subcuticular fat; however, cases with progressive infection involving the abdomen needed more aggressive debridement. After obtaining a clean wound, the size and localization of the defect lead to patient selection for flap reconstruction.
Preoperative flap planning was conducted as previously described (14). Markings identifying ALT-perforators by pencil Doppler are performed prior to the reconstruction; patients are placed in lithotomy position in order to access both the thigh and the perineum. Dissection of the ALT perforator flap was converted, when needed to composite ALT-VL flap as described in previous publications (14, 16). This technique allows for a tailored harvest of both coverage, (skin), bulk, (muscle) and eventually tensile component such as fascia lata, allowing reconstruction of the penile suspensory ligament (21).
Once elevated, the flap passes through a subcutaneous tunnel under the sartorius and rectus femoris muscles until reaching the perineum: this leads to a gain of 5 to 8 centimeters and avoids tension on the pedicle (16). Flap inset was performed in layers with deep sutures of the fascia using Vyril 2-0, inverted subcuticular sutures using Vycril 2-0 and Prolene 3-0 suture to the skin.
Postoperative monitoring was performed both clinically and using pencil Doppler. Patients were at bed rest alternating lateral and supine position. Mobilization was started by postoperative day 5, while seating was allowed after full healing and suture removal, usually 3 weeks postoperatively.
Statistical analysis
Descriptive statistics of the patient population, defects to reconstruct and flap characteristics were performed. Data were expressed as mean (± standard deviation). Data compilation and descriptive statistics were conducted on Excel (Microsoft Corp., Redmond, WA, USA).
Results
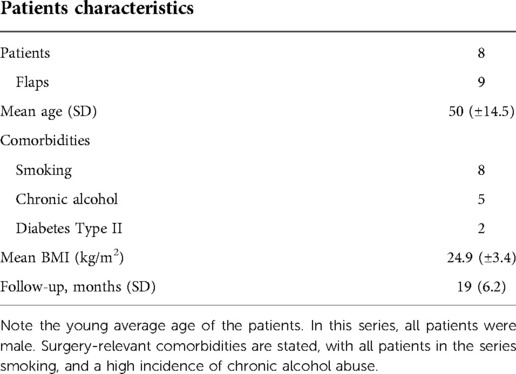
After applications of exclusion criteria, 8 patients who received a reconstruction after Fournier Gangrene using 9 pedicled ALT flaps during the study duration were included in our study. Table 1 describes patient characteristics.
Concerning quality of life evaluation and sexual health, we could asses 5 patients out of 8 in the group under study: two patients deceased at time of evaluation and one patient unable to reply because of cognitive impairment. One patient was lost to long term follow-up. Response rate in the remaining 4 questionnaires was 100%, no items were excluded.
Surgical outcome analysis
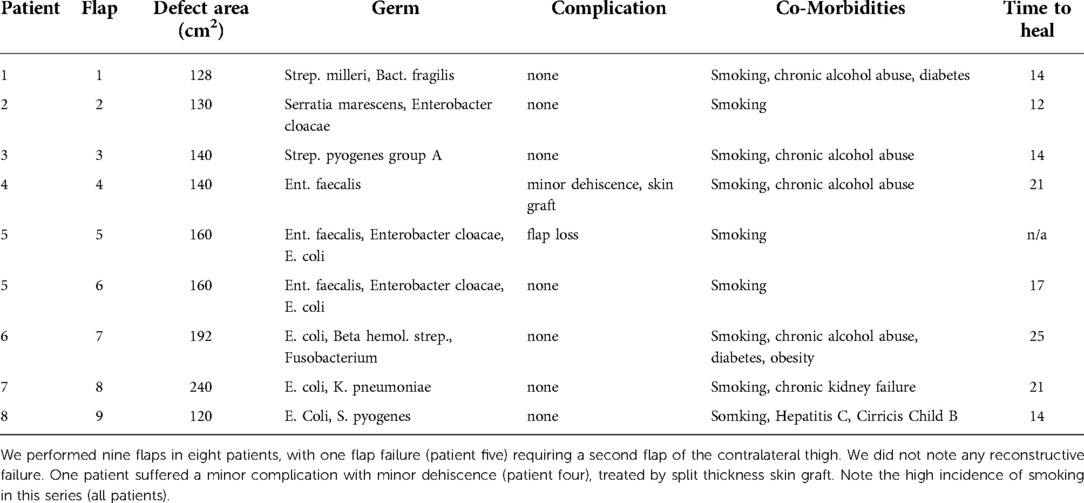
Patient's characteristics are stated in Table 1. Interestingly, all patients were smokers. Alcohol abuse was prevalent in 5 patients, and diabetes type II in 2 patients. Mean BMI was 24.9 kg/m2 (± 3.4). Mean follow-up was 19 months. Outcomes were measured both during the initial hospitalization and during follow up. Defect size to reconstruct, isolated pathogen, patient comorbidities and complications, as well as the time required for complete healing are listed in Table 2. We recorded one minor complication (patient n.4), requiring debridement and split thickness skin grafting after minor dehiscence.
One patient (patient n.5) suffered a major complication after total flap loss due to venous congestion of the flap leading to pedicle thrombosis. Prompt revision in the operating theatre did unfortunately not resolve the issue, and the flap was lost. The voluminous defect (160 cm2) required reconstruction with a second, contralateral flap with uneventful healing.
Time to complete wound healing was in average 17 days (SD ±5) prior to total stitch removal. We did not record any long-term complications in this series: patients were specifically asked for seating discomfort, sciatic or sacral decubitus ulcers, walking disorders or chronic pain both of the perineum and at the donor site. Figure 1 depicts the intraoperative view of perineal and scrotal reconstruction case. Figure 2 shows the same patient at 9 months follow-up.

Figure 1. Typical outcome of perineal reconstruction after Fournier’s gangrene. In this case, the pedicled anterolateral thigh flap was used to reconstruct both the perineum and scrotum. The flap is tunneled under the Sartorius in order to reach the perineum.

Figure 2. 9 Months postoperative view of the same patient. Note excellent mimicry of the thigh skin to a native scrotum.
Functional outcome analysis
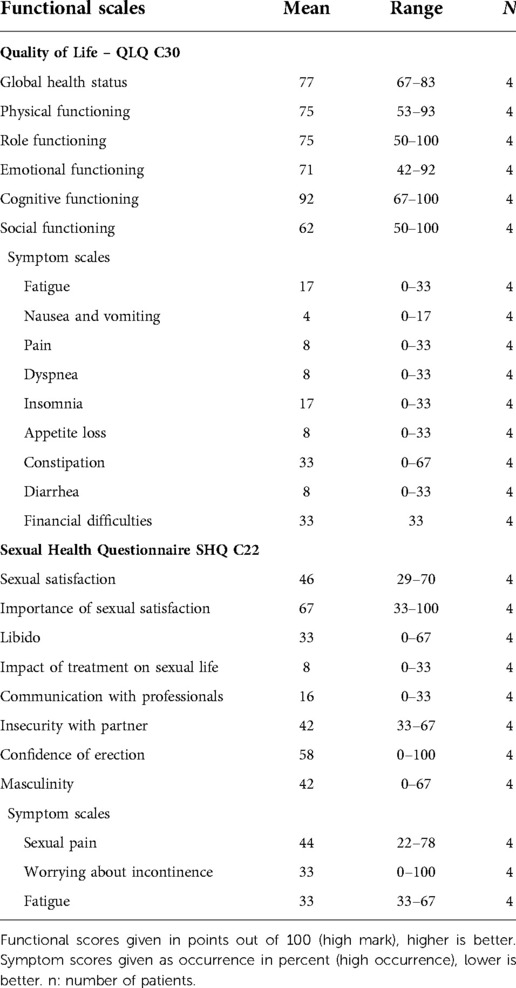
Quality of life scores show excellent functionally (i.e., confidence in erection, satisfaction of sexual life), with mean scores over 70/100 in four out of five categories; social function was rated lowest, although still above average with a mean of 62/100 (Table 3). Patients reported very few residual complaints in the symptom scales. Interestingly, many patients reported financial difficulties even long after the initial surgical procedure.
Sexual outcome analysis emphasizes the positive impact of the reconstruction, with patients reporting a moderately high score (67/100) in their sexual satisfaction. Interestingly, libido scores were relatively low (33/100), especially in comparison to higher scores in confidence of erection (58/100) and importance of sexual satisfaction (67/100). Importantly, patients reported a low score in communication of their sexual health with their tending physicians (16/100), underlining the need to address this issue in specialist consultation.
As expected, Fournier's Gangrene heavily affected patient's sexual health, with a low score on this item (8/100). Residual symptoms (pain, incontinence, fatigue) seemed to occur moderately seldom (33–44/100).
Discussion
Analysis of this series showed extremely satisfactory outcomes, both surgical and in terms of quality of life, underling the essential role of plastic surgery reconstruction after Fournier's gangrene. Although complication rates seem high in comparison with other reconstructive procedures, they align to literature describing perineal reconstruction (11, 14, 16). Moreover, we could note a possible skew due to a complete flap loss in the early stages of the learning curve of our team.
Unlike skin grafts, the ALT offers stable skin allowing much better pliability required to reconstruct a complex three-dimensional anatomical region. Furthermore, its versatility in its ability to include several different tissue types (i.e., muscle, fascia lata) can be a clear advantage in complex reconstructions, such as scrotal reconstruction, penile suspensory ligamentoplasty or filling deep perineal dead space (16, 21).
Its donor site is usually unproblematic, as opposed to abdominal flaps where herniation and bulging are commonplace (11), seldom requiring a skin graft in the largest flaps (over 8–10 cm in width, depending on the patient physiognomy).
Surgical outcomes
In this series, we do note that the complexity of the procedure imposes a learning curve, with an early case suffering complete flap loss. The latter however remain rare, literature stating a flap loss rate under 4% (22). Moreover, the small sample size is more susceptible to single major complications skewing the global outcomes. Complication rates are in line with current literature, and large series of pedicled ALT flaps performed in our institution report similar surgical outcomes (14, 16).
The main advantage of the ALT is the coverage achieved with one operation, showing a particular ductility due to pedicle length and possibility to harvest as purely perforator, or combined fascia or muscle component when necessary. This is a clear advantage and offers as it can be tailored to precisely restore form and function, from creation of a scrotal sac to reconstruction of a suspensory ligament. Where grafts in the perineum usually require extensive physiotherapy and ergotherapy to achieve stable, supple coverage, the ALT offers immediate pliability and better function, minimizing scarring, retraction and chronic wounds.
Even if the ALT has become a workhorse for complex reconstructions, and in our institution it has imposed itself as a reliable and versatile, surgical outcomes alone do not depict the full picture. Functional assessment of patient-related outcomes after reconstruction of perineum and/or genitalia remains a critical point when judging of the effectiveness of reconstruction.
Patient related outcomes
Modern reconstructive surgery restores function and form, and a simple visual analysis of long-term results lacks to assess the actual function of the surgeons work. In this small series, we note the excellent outcome in functional quality of life. Although some items (i.e., moderately lower social function) do score lower, the global quality of life is good despite a life threatening condition in oftentimes polymorbid patients and complex subsequent reconstruction. We infer that the sexual wellbeing can play a major role in both emotional and social health, and may cause lower scores in the functional scales of quality of life. Very few long term symptoms were reported: occasional constipation was one of them but did not seem to relate to the surgical procedure (debridement/reconstruction); notwithstanding constipation being a frequent symptom in the general population, with an incidence of up to 15% worldwide (23). Financial difficulties occurred occasionally, generally matching with the patient's social state.
Sexual health analysis showed a lower global score when compared to global functional parameters, however patients reported residual sexual activity, with moderately high sexual satisfaction (46/100), and above average confidence in their erection (58/100). Fournier's gangrene understandably affected their sexual life negatively (scoring 8/100), however the lack of control group with other means of reconstruction does not allow comparison with other means of reconstruction such as skin grafts, or other flap techniques.
Interestingly, a discrepancy between reported fatigue in QoL and SHQ (17 vs. 33/100) may denote a higher impact of fatigue on sexual health than general quality of life. This could explain globally lower scores in SHQ vs. QoL, since sexual function depends heavily on a good perineal form and function. We infer that the SHQ is an excellent measure of reconstructive success in perineal reconstruction.
Limitations of this study include a small series, with possible confounding bias due to the lack of good quality of life and sexual health data in a comparable, healthy group. This emphasizes the need to systematically assess outcomes in both the general population and after reconstructive surgery. Moreover, our patient population being exclusively male, depicting the increased incidence in male, results do not reflect neither quality of life nor sexual health in women. We do concede the difficulty to extrapolate trends in the small population under study, however the available data is meaningful in assessing function of the patient in his everyday life.
Conclusions
To our knowledge, this is the only study that assesses functional Quality of Life and Sexual Health outcomes in perineal reconstruction after Fournier's gangrene. The ALT shows excellent quality of life outcomes, and moderately good sexual health. This is however the only data that is available after reconstructive surgery after a major sort tissue infection, the lack of reliable, relatable data leads to the impossibility to compare different reconstructive procedures. Our results show that assessing sexual function after reconstructive surgery of the perineum is paramount to analyze both function and form.
Furthermore, the ALT flap offers ample stable, pliable skin to reconstruct the perineum, with good results and complication rates in line with current literature. It is a valid alternative to abdominal flaps without potential donor site comorbidities.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
SAR and DG conducted the data analysis and manuscript redaction under supervision of PGdS and WR. Data collection and patient follow up were conducted by CdS and SAR. All authors contributed to the article and approved the submitted version.
Funding
Open access funding was provided by the University of Lausanne.
Acknowledgments
Sandrine Kueng for the maintenance and administration of the patient database.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yeniyol C O, Suelozgen T, Arslan M, Riza Ayder A. Fournier’s gangrene: experience with 25 patients and use of Fournier’s gangrene severity index score. Urology. (2004) 64:218–22. doi: 10.1016/J.UROLOGY.2004.03.049
2. Hejase MJ, Simonin JE, Bihrle R, Coogan CL. Genital Fournier’s gangrene: experience with 38 patients. Urology. (1996) 47:734–9. doi: 10.1016/S0090-4295(96)80017-3
3. Insua-Pereira I, Ferreira PC, Teixeira S, Barreiro D, Silva Á. Fournier’s gangrene: a review of reconstructive options. Cent Eur J Urol. (2020) 73:74–9. doi: 10.5173/CEJU.2020.0060
4. RJ B MM, A M AM. Reconstruction of perineal defects. Ann R Coll Surg Engl. (2013) 95:539–44. doi: 10.1308/003588413X13629960047155
5. Alwaal A, McAninch JW, Harris CR, Breyer BN. Utilities of split-thickness skin grafting for male genital reconstruction. Urology. (2015) 86:835–9. doi: 10.1016/J.UROLOGY.2015.07.005
6. Brodbeck R, Horch RE, Arkudas A, Beier JP. Plastic and reconstructive surgery in the treatment of oncological perineal and genital defects. Front Oncol. (2015) 5:212. doi: 10.3389/FONC.2015.00212/BIBTEX
7. Yu P, Sanger JR, Matloub HS, Gosain A, Larson D. Anterolateral thigh fasciocutaneous island flaps in perineoscrotal reconstruction. Plast Reconstr Surg. (2002) 109:610–6. doi: 10.1097/00006534-200202000-00030
8. Furr J, Culkin D. Injury to the male external genitalia: a comprehensive review. Int Urol Nephrol. (2017) 49:553–61. doi: 10.1007/S11255-017-1526-X
9. Ünverdi ÖF, Kemaloğlu CA. A reliable technique in the reconstruction of large penoscrotal defect: internal pudendal artery perforator flap. Urology. (2019) 128:102–6. doi: 10.1016/J.UROLOGY.2019.02.028
10. Jain AK, Defranzo AJ, Marks MW, Loggie BW, Lentz S. Reconstruction of pelvic exenterative wounds with transpelvic rectus abdominis flaps: a case series. Ann Plast Surg. (1997) 38:115–23. doi: 10.1097/00000637-199702000-00004
11. Devulapalli C, Wei ATJ, Dibiagio JR, Baez ML, Baltodano PA, Seal SM, et al. Primary versus flap closure of perineal defects following oncologic resection: a systematic review and meta-analysis. Plast Reconstr Surg. (2016) 137:1602–13. doi: 10.1097/PRS.0000000000002107
12. Song Yg, Chen Gz, Song Yl. The free thigh flap: a new free flap concept based on the septocutaneous artery. Br J Plast Surg. (1984) 37:149–59. doi: 10.1016/0007-1226(84)90002-X
13. Luo S, Raffoul W, Luo J, Luo L, Gao J, Chen L, et al. Anterolateral thigh flap: a review of 168 cases. Microsurgery. (1999) 19:232–8. doi: 10.1002/(sici)1098-2752(1999)19:5-232::aid-micr5%3E3.0.co;2-s
14. Di Summa PG, Tremp M, Meyer Zu Schwabedissen M, Schaefer DJ, Kalbermatten DF, Raffoul W. The combined pedicled anterolateral thigh and vastus lateralis flap as filler for complex perineal defects. Ann Plast Surg. (2015) 75:66–73. doi: 10.1097/SAP.0b013e3182a884c8
15. Riva FMG, Tan NC, Liu KW, Hsieh CH, Jeng SF. Anteromedial thigh perforator free flap: report of 41 consecutive flaps and donor-site morbidity evaluation. J Plast Reconstr Aesthet Surg. (2013) 66:1405–14. doi: 10.1016/J.BJPS.2013.06.012
16. Rossi SA, Martineau J, David G, Hübner M, Hahnloser D, Raffoul W, et al. Outcomes of the composite anterolateral thigh flap for perineal reconstruction after postoncological abdominoperineal resection. Dis Colon Rectum. (2022) 65(3):373–81. doi: 10.1097/DCR.0000000000002132. PMID: 34784314
17. Czymek R, Kujath P, Bruch HP, Pfeiffer D, Nebrig M, Seehofer D, et al. Treatment, outcome and quality of life after Fournier’s gangrene: a multicentre study. Colorectal Dis. (2013) 15:1529–36. doi: 10.1111/CODI.12396
18. Nolte S, Liegl G, Petersen MA, Aaronson NK, Costantini A, Fayers PM, et al. General population normative data for the EORTC QLQ-C30 health-related quality of life questionnaire based on 15,386 persons across 13 European countries, Canada and the Unites States. Eur J Cancer. (2019) 107:153–63. doi: 10.1016/J.EJCA.2018.11.024
19. Greimel E, Nagele E, Lanceley A, Oberguggenberger AS, Nordin A, Kuljanic K, et al. Psychometric validation of the European Organisation for Research and Treatment of Cancer-Quality of Life Questionnaire Sexual Health (EORTC QLQ-SH22). Eur J Cancer. (2021) 154:235–45. doi: 10.1016/J.EJCA.2021.06.003
20. Aaronson NK, Ahmedzai S, Bergman B, Bullinger M, Cull A, Duez NJ, et al. The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst. (1993) 85:365–76. doi: 10.1093/JNCI/85.5.365
21. Guiotto M, Watfa W, Raffoul W, Di Summa P. Anterolateral thigh flap with vascularized fascia lata associated with thigh flaps: a case report of an all-in-one reconstruction of the suspensory ligament and penoscrotal district after fournier gangrene. Ann Plast Surg. (2020) 85:e44–7. doi: 10.1097/SAP.0000000000002533
22. Celik N, Wei FC, Lin CH, Cheng MH, Chen HC, Jeng SF, et al. Technique and strategy in anterolateral thigh perforator flap surgery, based on an analysis of 15 complete and partial failures in 439 cases. Plast Reconstr Surg. (2002) 109:2211–6. doi: 10.1097/00006534-200206000-00005
Keywords: fournier gangrene, reconstruction, pedicled anterolateral thigh flap, perineal defect, sexual wellbeing, quality of life
Citation: Rossi SA, de Schoulepnikoff C, Guillier D, Raffoul W and di Summa PG (2022) Quality of life and sexual health after perineal reconstruction in Fournier gangrene using pedicled anterolateral thigh flaps. Front. Surg. 9:994936. doi: 10.3389/fsurg.2022.994936
Received: 15 July 2022; Accepted: 26 August 2022;
Published: 13 September 2022.
Edited by:
Clemens Mathias Rosenbaum, Asklepios Klinik Barmbek, GermanyReviewed by:
Valentin Maurer, University of Hamburg, GermanyAndrea Lisa, Humanitas Research Hospital, Italy
© 2022 Rossi, de Schoulepnikoff, Guillier, Raffoul and Di Summa. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pietro G. di Summa cGlldHJvLmRpLXN1bW1hQGNodXYuY2g=
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Severin Alexander Rossi
Severin Alexander Rossi Camille de Schoulepnikoff1
Camille de Schoulepnikoff1 Wassim Raffoul
Wassim Raffoul