- Department of Orthopaedics, The First Affiliated Hospital of Jinan University, Guangzhou, China
Objective: This systematic review and meta-analysis aimed to estimate re-revision rates of retained femoral components after revision of total hip arthroplasty (THA).
Methods: Papers were searched in the PubMed, Embase, Web of Science, and Cochrane Library databases with predetermined keywords from January 2000 to January 2022. The studies reporting the re-revision rates of retained stems after revision THA were identified. Pooled rates of re-revision for any reason and aseptic loosening were calculated using a random-effects model or a fixed-effects model based on the results of heterogeneity assessment after the Freeman–Tukey double-arcsine transformation. A meta-regression was performed to explore potential sources of heterogeneity.
Results: There were 20 studies with 1,484 hips that received the isolated cup revision with the femoral component retained. The pooled re-revision rate of retained stems was 1.75% [95% confidence interval (CI) 0.43%–3.65%]. The re-revision rate of retained stems due to aseptic loosening was 0.62% (95% CI, 0.06%–1.55%). The meta-regression showed that the fixation type (cemented or cementless) was related to the re-revision rate for any reason and the re-revision rate for aseptic loosening.
Conclusion: Based on the existing evidence, the isolated cup revision with a stable stem in situ yields low re-revision rates. The cement status of retained stems may influence the survivorship of stems.
Introduction
Total hip arthroplasty (THA) is one of the most effective treatments for end-stage hip disorders (1). However, despite the good clinical outcomes of THA, the revision procedure of failed THA is a heavy burden. Over 50,000 revision THA procedures are performed annually in the United States, and the frequency is estimated to double by 2030 (2). Periprosthetic osteolysis and aseptic loosening are the most common causes of failure in primary THA (3). However, the mechanism is different between the femoral stem and the acetabular cup, resulting in a linear rate of loosening for femoral components while an exponentially increasing rate for acetabular components over time (4, 5). The isolated cup loosening is reported to account for over 20% of all revision THA in the United States (6). Surgeons may encounter a loose cup with a stable stem during revision THA. In the scenario of a failed cup combined with a well-positioned and stable stem, isolated cup revision with the stem retained can avoid the risk of femoral fracture and destruction of bone stock, reduce blood loss and cost, and save operative time. A previous study of the United States National Inpatient Sample database from 2009 to 2013 investigated the epidemiology of 308,723 revision THA procedures and found that the number of isolated cup revision procedures was 44,687 (14.5%) (7). In 2019, the United Kingdom National Joint Registry demonstrated that isolated cup revision accounted for 26% (1,840/7,060) of all single-stage hip revision procedures (8)1. On the other hand, retaining a stem in revision may preclude the exposure of the acetabular component and compromise the restoration of hip geometry. It also carries the risk of re-revision due to the failure of the stem.
Several observational studies have assessed the outcomes of isolated cup revision with a retained stem (9–11). Most researchers recommended that the selection criteria for patients who were about to undergo an isolated cup revision should be rigorous. The stability of stems must be ensured. Chen et al. reported a minimum 5-year follow-up study of 57 retained stems after isolated cup revision and found that all acetabular and femoral components were stable (12). Kim et al. also reported an optimal survival rate of 98.9% in 227 retained stems at 30.3 years (13). However, in the study by McGonagle et al. (10), 28 of 227 retained stems (12.3%) had failed 5.1 years after the isolated cup revision. The clinical outcomes of isolated cup revision were uncertain and these studies involved a relatively small sample size. The overall survivorship of retained stems has not been well established. To our knowledge, there has been no systematic review or meta-analysis on this topic. Hence, we conducted a systematic review and meta-analysis to evaluate the fate of the retained femoral stem in revision THA.
Materials and methods
We conducted this systematic review and meta-analysis following the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) Statement protocol (14, 15).
Search strategy and eligibility
PubMed, Embase, Web of Science, and Cochrane Library databases were searched from January 2000 to January 2022. The search keywords were: revision AND hip AND (arthroplasty OR replacement) AND (unrevised OR retain OR isolated OR retention). We developed specific search strategies for each database and references to the identified studies were checked for potential eligibility.
We included publications that reported the outcomes of revision THA with femoral stems retained.
The following exclusion criteria were used: (1) publication year before 2000; (2) unclear etiology of index revision; (3) primary THA with oncological pathology; (4) number of retained stems of <10; (5) follow-up duration of <2 years; (6) index revision related to a debridement, antibiotics and implant retention procedure; (7) femoral stem being removed and reimplanted during operation.
Non-English language reports, case reports, conference abstracts/posters, or reviews were excluded. After dropping the duplicates, two orthopedic surgeons independently reviewed the titles and abstracts to screen potentially eligible studies. The full texts were then read independently by the same two surgeons to identify the final list of publications. If there was a disagreement, a third senior orthopedic surgeon was consulted for a final assessment and consensus.
Data extraction
After the final list of included studies was set, data were extracted, including information on the publication, patient characteristics, follow-up duration, time intervals between primary THA and index revision, fixation type of retained stems (cemented or cementless), number of re-revision stems, number of re-revision stems due to aseptic loosening and hip function score. The primary outcome of interest was the re-revision of retained stems, and the secondary outcome was the re-revision of the retained stems due to aseptic loosening. If the necessary information could not be extracted from the original paper, we contacted the corresponding author to request additional information.
Assessment of quality and bias
The quality of the included studies was assessed independently by the two surgeons. In this regard, the Newcastle-Ottawa Scale was used (16). Publication bias is estimated by funnel plots and Egger's test (17).
Statistical analysis
The R package (rmeta, RRID: SCR_002270, version #4.1.3) was used for statistical analysis, with P < 0.05 as the threshold of statistical significance. The rates of primary and secondary outcomes with 95% confidence intervals (CIs) were pooled using the Freeman–Tukey double-arcsine transformation (18, 19). The heterogeneity was assessed using the I2 statistic and the Q test. If I2 < 50% and the P-value for the Q test >0.05, the studies were interpreted as minimally heterogeneous and a fixed-effects model was used for the meta-analysis. If I2 > 50% or the P-value for the Q test <0.05, the data were considered highly heterogeneous and a random-effects model was used. The sensitivity analysis was conducted by the leave-one-out analysis. The meta-regression was utilized to identify the potential sources of heterogeneity based on predetermined factors, including the year of publication, sample size, mean age of recruited patients, gender distribution, follow-up duration, time intervals between primary THA and index revision, and fixation type. In the first univariate model, each of the predetermined factors was analyzed individually, and the factors with a crude P-value less than 0.1 were extracted into the final multivariable model. If a potential factor was confirmed in the final model, subgroup analysis would be performed subsequently. Other results were presented as a descriptive summary.
Results
Overview of search results
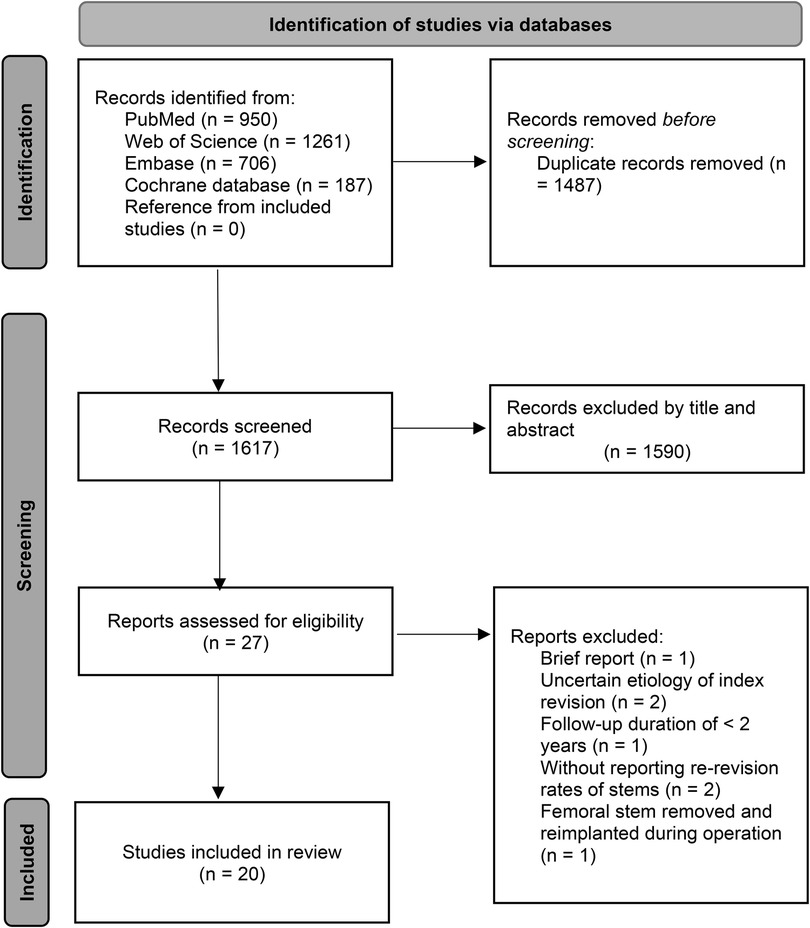
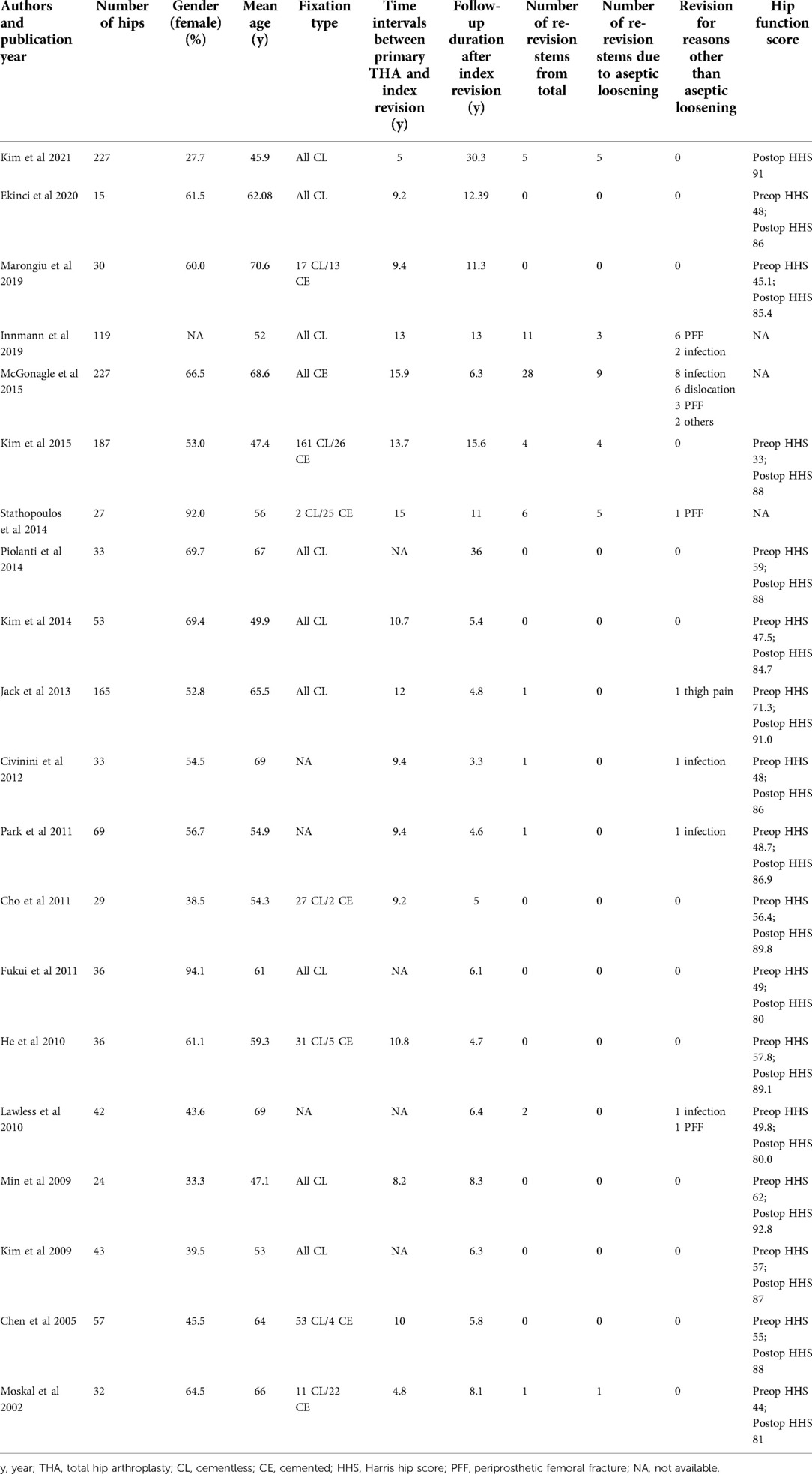
There were 3,104 studies identified in the initial search. After deleting duplicates, the titles and abstracts of 1,617 papers were reviewed. Twenty-seven articles were assessed for eligibility by full-text reading. Finally, 20 retrospective cohort studies were included in the analysis (9, 10, 12, 13, 20–35) (Figure 1). A total of 1,484 hips underwent isolated cup revision with the stem retained. The mean follow-up duration of the studies was 12.2 years (weighted average according to the sample size) (Table 1).
Assessment of quality and bias
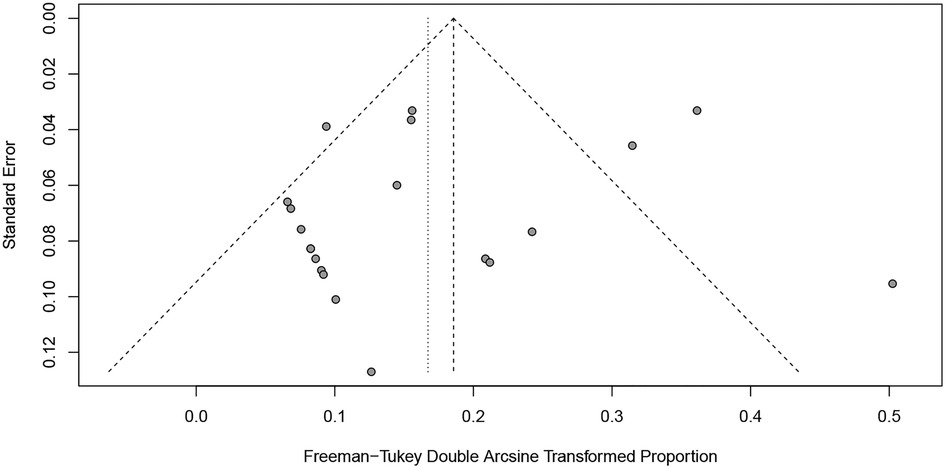
The Newcastle-Ottawa rank for all included cohort studies was represented in Table 2. Overall, the funnel plots for the primary outcome and the secondary outcome showed no evidence of possible publication bias (Figures 2, 3), which was also consistent with the formal test (Egger's test, P for the primary outcome = 0.2511; P for the secondary outcome = 0.4440).
Primary outcome
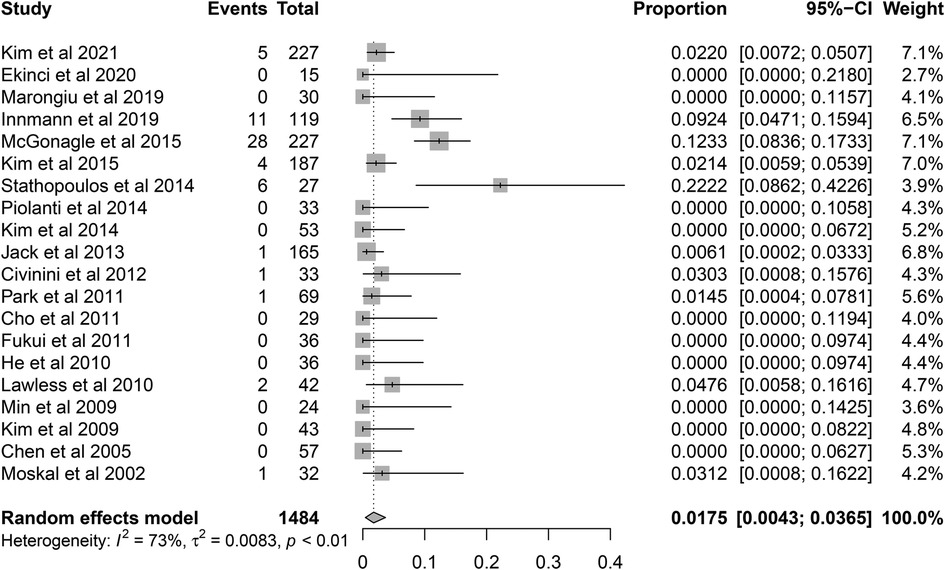
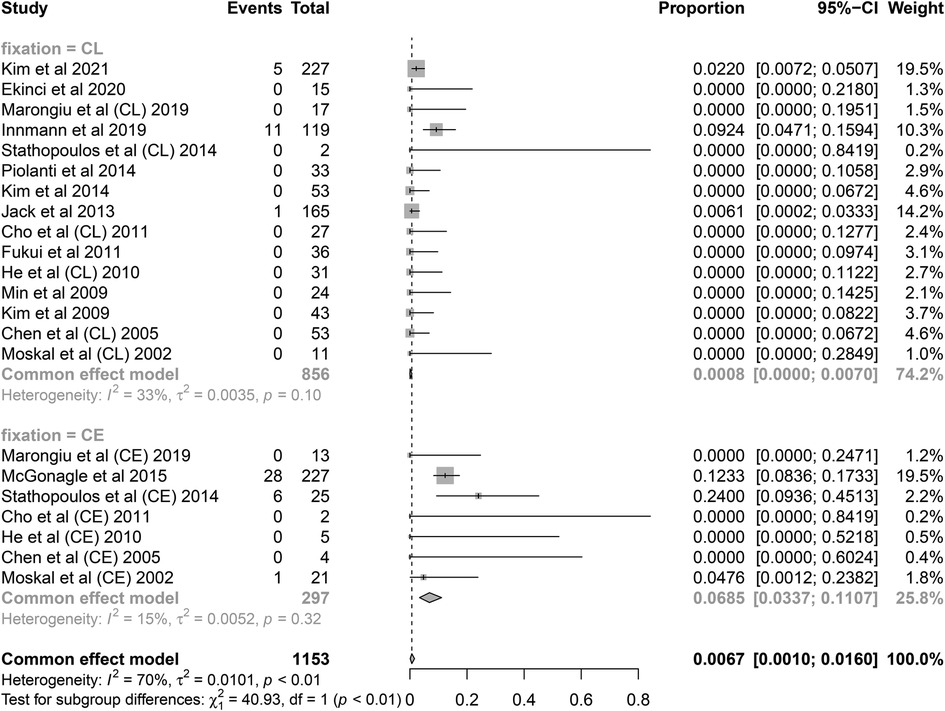
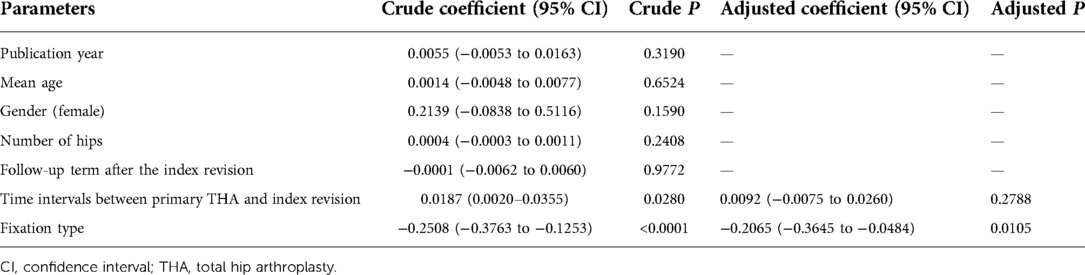
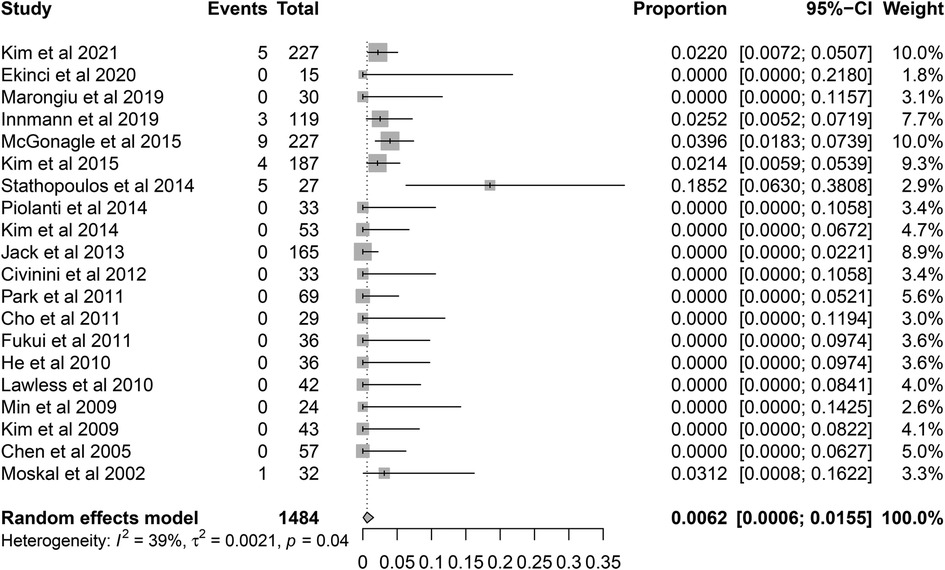
A total of 60 re-revision cases of retained stems for any reason were observed. The pooled re-revision rate was 1.75% (95% CI 0.43%–3.65%) with relatively high heterogeneity (I2 = 72.3%, P < 0.001) (Figure 4). The results were robust to the leave-one-out analysis (Figure 5). The meta-regression was performed to explore the potential sources of heterogeneity. At the first univariate step, fixation type and time intervals between primary THA and index revision were extracted with a crude P-value less than 0.1. In the next multiple regression model, the fixation type was finally identified as the only potential factor (Table 3). The subsequent subgroup analysis based on the fixation type showed that the re-revision rate was 0.08% (95% CI, 0%–0.7%; heterogeneity, I2 = 33%, P = 0.10) in cementless stems while that was 6.9% (95% CI, 3.4%–11.1%; heterogeneity, I2 = 15%, P = 0.32) in cemented stems. The inter-subgroup difference was of statistical significance (P < 0.001) (Figure 6).
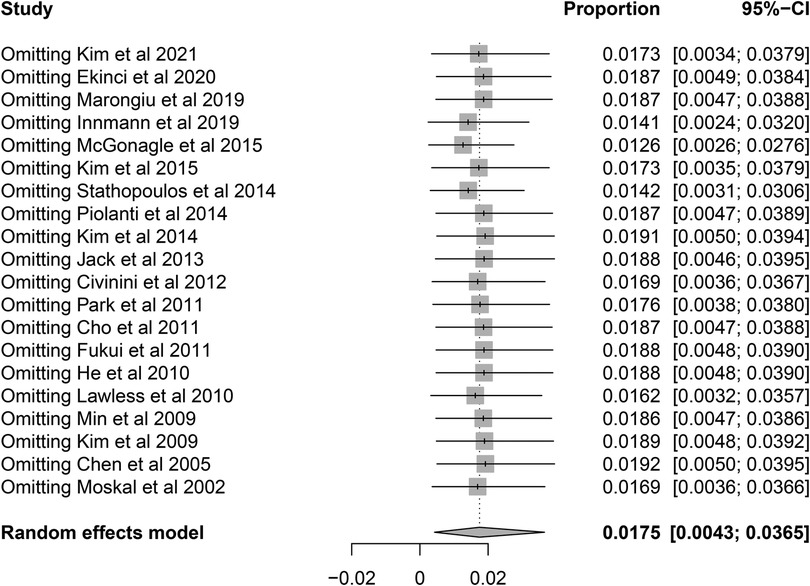
Figure 5. Sensitivity analysis for the re-revision rate of retained stems using leave-one-out analysis.
Secondary outcome
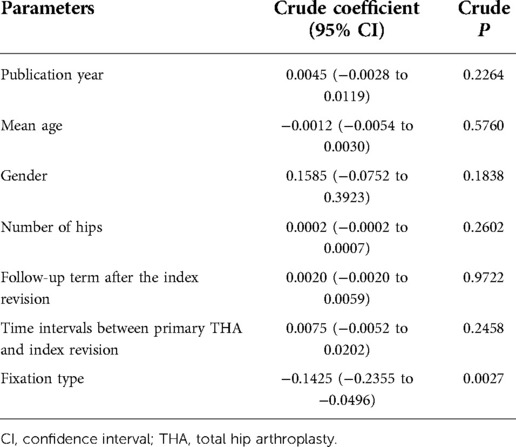
Among the 60 re-revision stems, a total of 27 cases (45%) were reported due to aseptic loosening. Pooled analysis showed that the rate of re-revision due to aseptic loosening was 0.62% (95% CI, 0.06%–1.55%) with a moderate heterogeneity (I2 = 38.8%, P = 0.0398) (Figure 7). The results were also robust to the leave-one-out analysis (Figure 8). The univariate meta-regression model also showed that the fixation type was the only potential source of heterogeneity (Table 4).
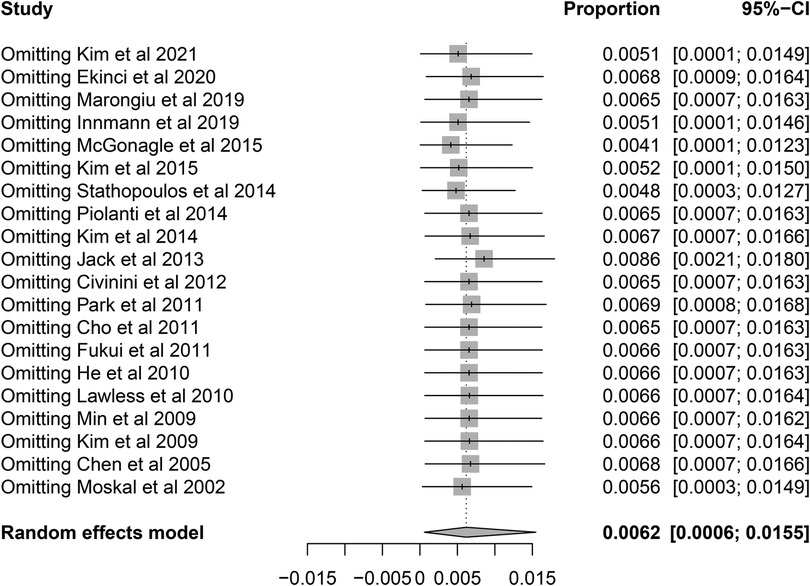
Figure 8. Sensitivity analysis for the re-revision rate of retained stems for aseptic loosening using leave-one-out analysis.
Discussion
This is the first systematic review and meta-analysis to analyze the re-revision rates of unrevised femoral components during revision THA. We found that the retained stems after isolated cup revision represented favorable results with a pooled re-revision rate of 1.75% for any reason and 0.62% for aseptic loosening, respectively. Furthermore, our data indicated that revision THA with cemented stems retained might have a higher re-revision rate than those with cementless stems retained.
Our research is of clinical relevance for surgeons in deciding whether to remove or retain a stable stem when facing the common dilemma that only the cup is loosened as the survival rates of cups are much lower when compared with stems. Retaining a stable stem is an attractive option for the obvious advantages such as less surgical time, lower risk of intraoperative fracture, less impairment on the bone stock of the proximal femur, and less blood loss and cost. Poon and Lachiewicz (36) reported that, when compared with revision of both the cups and stems, the blood loss was 52% less and the surgical time was 35% shorter in isolated cup revision. Lim et al. compared the outcomes of isolated cup revision with a matched total revision group and found that the hip function and survivorship were similar between the two groups (37). Nevertheless, removing a well-fixed stem can facilitate the exposure and the selection of type and size of the revision prostheses and enhance the longevity of both cups and stems by the newer-generation implants, which is called “fresh start” (23, 36, 38). The present review aggregated the existing evidence on the controversy to evaluate the survivorship of the retained stable stems during revision THA.
We found that, during a relatively considerable follow-up term, the retained stems showed high survivorship with a re-revision rate of 1.75%. The two highest re-revision rates of the studies were 22.2% by Stathopoulos et al. (23) and 12.3% by McGonagle et al. (10), respectively, and they were within the published range. There were two previous studies with a sample size of over 1,000 revision THAs and a follow-up of over 10 years. Philpott et al. reported a stem survivorship of 77% in 1,176 revision THAs with a minimum 10-year follow-up (39). Springer et al. reported an overall survivorship of 82% at 10 years of 1,100 revision THAs (40). Our data on the re-revision rate of stems due to aseptic loosening (0.62%) was similar to those reported by Hasegawa et al. (2.2%) (41) and Imbuldeniya et al. (0.7%) (42). These results revealed that isolated acetabular revision was a reliable procedure in the presence of a well-fixed stem. We also noted that the pooled re-revision rates seemed to be lower than those reported by the large-sample cross-sectional studies, which might be partly due to the discreet selection of patients. Many studies emphasized that the accurate and secure fixation and proper alignment of a stem was the prerequisite for stem retention. Surgeons should assess the stem stability not only by radiographs but also intraoperatively. Ekinci et al. and Cho et al. confirmed the stability of the stem by conducting traction and rotational forces on stems and detecting the fine movements between stems and adjacent host bone during the revision procedure (20, 29). Hernigou et al. recommended that the osteolysis around the retained stems should be less than 10 cm2 to achieve longer survivorship (43). Kim et al. and Innmann et al. further restricted the indication that the osteolysis should be in Gruen zones 1 and/or 7 (13, 21). Cautiously screening patients meeting the indication could improve the survivorship of the surgeries. In addition, the pooled calculation of re-revision rates was based on retrospective data and thus could not reflect the total number of hips undergoing the isolated cup revision with the stem retained. Therefore, further studies with longer follow-ups, larger sample sizes, and higher levels of evidence are needed to demonstrate a more accurate survival rate of retained stems.
Our meta-regression reflected that fixation type would influence the fate of the retained stems. The retained stems with cemented fixation might be associated with a higher risk of re-revision than those with cementless fixation. When compared to the cementless technique, cementing may increase the risk of periprosthetic osteolysis due to cement particles (44). Emerson et al. investigated the radiographic findings of cemented and cementless stems in 180 primary THA cases and found a higher incidence of osteolysis in cemented stems (45). The authors stated that cementless stems were more resistant to osteolysis. Several meta-analyses have investigated the influence of cement status on stem survivorship. Toci et al. included seven studies and found that cementless stems were related to a lower revision rate (5.53% vs. 8.91%) when compared with cemented stems in primary THA, but the difference was not statistically significant (46). Another meta-analysis suggested that older patients might benefit more from cemented fixation while younger patients benefit more from cementless fixation in primary THA (47). Due to a paucity of publications, no study has so far compared the outcome of a cemented retained stem with that of a cementless retained stem directly. The implication of our results should be validated by future comparative studies. Other factors that may affect the outcomes of retained stems during revision THA have also been discussed. The re-revision rate reported by Stathopoulos et al. was the highest among the included studies. The majority of failed retained stems (90%) in their studies belonged to patients with developmental dysplasia of the hip (23). The authors attributed the relatively high failure rate of retained stems to the poor pre-existing femoral bone quality. Several studies have identified that the rate of hip instability or dislocation after isolated cup revision might be associated with surgical approaches (48, 49). Moskal et al. recommended a standard modified direct lateral approach to avoid excessive soft tissue release (35).
Several limitations should be noted in this research. First, the methodology contained the bias of possibly inevitably missing relevant studies. However, we identified and included all eligible studies on the re-revision rates of retained stems from main databases. Second, the heterogeneity of the pooled analysis was relatively high. We, therefore, performed a meta-regression to explore potential sources and found that the type of fixation could influence the results. The subsequent subgroup analysis also reduced the heterogeneity. Third, though the stratification based on fixation type showed a positive result in the comparison between cemented and cementless stems, the statistical analysis might not be sufficiently rigorous due to the relatively small sample size of failed stems. Fourth, the data were from retrospective studies rather than the registers or prospective studies. The pooled analysis could not reflect the cross-sectional panorama of unrevised stems after revision THA, which would introduce a bias in the estimation of re-revision rates. Thus, the results should be interpreted with caution.
Conclusion
Based on the available evidence, the isolated cup revision while retaining a stable stem in situ yields low re-revision rates. Retained stems with cemented fixation might have a higher risk of re-revision than those with cementless fixation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
HL, SH, and NL contributed to the conception and design of the study. TZ and WW contributed to the methodology of the study. HL and TZ completed the data extraction. HL, WG, CW, and SP performed the statistical analysis. HL wrote the first draft of the manuscript. TZ, WW, CW, SP, and SH wrote sections of the manuscript. HL, SH, and NL reviewed and edited the manuscript. SH and NL claimed the funding. All authors contributed to the article and approved the submitted version.
Funding
This study was funded by the Joint Training Program of Guangdong-Hong Kong-Macao Greater Bay Area Bone and Joint Disease Research Center: Shenzhen Key Labortory of Musculoskeletal Tissue Reconstruction and Function Restoration, Number ZDSYS20200811143752005.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnote
1https://reports.njrcentre.org.uk/hips-revision-procedures-components/H21v1NJR?reportid=471D9229-25EC-4D5F-B220-425F3DCD3518/defaults=DC__Reporting_Period__Date_Range=%22MAX%22,J__Filter__Calendar_Year=%22MAX%22,H__Filter__Joint=%22Hip%22.
References
1. Bayliss LE, Culliford D, Monk AP, Glyn-Jones S, Prieto-Alhambra D, Judge A, et al. The effect of patient age at intervention on risk of implant revision after total replacement of the hip or knee: a population-based cohort study. Lancet. (2017) 389:1424–30. doi: 10.1016/s0140-6736(17)30059-4
2. Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. (2007) 89:780–5. doi: 10.2106/jbjs.F.00222
3. Jonas K, Nils W, Alexander D, Stefan B, Henning W, Thilo F. The etiology of revision total hip arthroplasty: current trends in a retrospective survey of 3450 cases. Arch Orthop Trauma Surg. (2020) 140:1265–73. doi: 10.1007/s00402-020-03514-3
4. Cooper RA, McAllister CM, Borden LS, Bauer TW. Polyethylene debris-induced osteolysis and loosening in uncemented total hip arthroplasty. A cause of late failure. J Arthroplasty. (1992) 7:285–90. doi: 10.1016/0883-5403(92)90050-z
5. Schulte KR, Callaghan JJ, Kelley SS, Johnston RC. The outcome of Charnley total hip arthroplasty with cement after a minimum twenty-year follow-up. The results of one surgeon. J Bone Joint Surg Am. (1993) 75:961–75. doi: 10.2106/00004623-199307000-00002
6. Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ. The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am. (2009) 91:128–33. doi: 10.2106/jbjs.H.00155
7. Gwam CU, Mistry JB, Mohamed NS, Thomas M, Bigart KC, Mont MA, et al. Current epidemiology of revision total hip arthroplasty in the United States: national inpatient sample 2009 to 2013. J Arthroplasty. (2017) 32:2088–92. doi: 10.1016/j.arth.2017.02.046
8. National Joint Registry for England. Wales and Northern Ireland 18th Annual Report (2021). Available from: http://www.njrcentre.org.uk (Accessed September 19, 2022).
9. Marongiu G, Podda D, Mastio M, Capone A. Long-term results of isolated acetabular revisions with reinforcement rings: a 10- to 15-year follow-up. Hip Int. (2019) 29:385–92. doi: 10.1177/1120700018802750
10. McGonagle L, Siney PD, Raut VV. Fate of the unrevised cemented stem following cup only revision: 227 hips at an average of 6 years follow-up. Orthop Traumatol Surg Res. (2015) 101:781–4. doi: 10.1016/j.otsr.2015.08.005
11. Kubota Y, Kaku N, Tagomori H, Kataoka M, Tsumura H. Isolated acetabular revision with femoral stem retention using computed tomography-based navigation. Orthop Traumatol Surg Res. (2019) 105:1311–7. doi: 10.1016/j.otsr.2019.08.002
12. Chen XD, Waddell JP, Morton J, Schemitsch EH. Isolated acetabular revision after total hip arthroplasty: results at 5-9 years of follow-up. Int Orthop. (2005) 29:277–80. doi: 10.1007/s00264-005-0674-2
13. Kim YH, Park JW, Jang YS. Long-term survival (up to 34 years) of retained cementless anatomic femoral stem in patients <50 years old. J Arthroplasty. (2021) 36:1388–92. doi: 10.1016/j.arth.2020.10.055
14. Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. (2019) 10:Ed000142. doi: 10.1002/14651858.Ed000142
15. Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Br Med J. (2015) 350:g7647. doi: 10.1136/bmj.g7647
16. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25:603–5. doi: 10.1007/s10654-010-9491-z
17. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
18. Miller JJ. The inverse of the Freeman–Tukey double arcsine transformation. Am Stat. (1978) 32:138. doi: 10.1080/00031305.1978.10479283
19. Murray FF, John WT. Transformations related to the angular and the square root. Ann Math Stat. (1950) 21:607–11. doi: 10.1214/aoms/1177729756
20. Ekinci M, Bilgin Y, Sayar Y, Ergin ON, Salduz A, Akgul T, et al. The survival of well-fixed cementless femoral component after isolated acetabular component revision. Indian J Orthop. (2020) 54:885–91. doi: 10.1007/s43465-020-00147-x
21. Innmann MM, Peitgen DS, Merle C, Bruckner T, Gotterbarm T, Moradi B, et al. Long-term survival of retained cementless hip stems at an average of 13 years after isolated cup revision. J Bone Joint Surg Am. (2019) 101:265–9. doi: 10.2106/jbjs.18.00159
22. Kim YH, Park JW, Kim JS. Isolated revision of an acetabular component to a ceramic-on-ceramic bearing in patients under 50 years of age. Bone Joint J. (2015) 97-b:1197–203. doi: 10.1302/0301-620x.97b9.35748
23. Stathopoulos IP, Lampropoulou-Adamidou KI, Vlamis JA, Georgiades GP, Hartofilakidis GC. One-component revision in total hip arthroplasty: the fate of the retained component. J Arthroplasty. (2014) 29:2007–12. doi: 10.1016/j.arth.2014.05.005
24. Piolanti N, Andreani L, Parchi PD, Bonicoli E, Niccolai F, Lisanti M. Clinical and radiological results over the medium term of isolated acetabular revision. Sci World J. (2014) 2014:148592. doi: 10.1155/2014/148592
25. Kim Y, Kim Y-H, Hwang K-T, Choi I-Y. Isolated acetabular revision with ceramic-on-ceramic bearings using a ceramic head with a metal sleeve. J Arthroplasty. (2014) 29:2420–3. doi: 10.1016/j.arth.2014.03.007
26. Jack CM, Molloy DO, Walter WL, Zicat BA, Walter WK. The use of ceramic-on-ceramic bearings in isolated revision of the acetabular component. Bone Joint J. (2013) 95-b:333–8. doi: 10.1302/0301-620x.95b3.30084
27. Civinini R, Carulli C, Matassi F, Nistri L, Innocenti M. A dual-mobility cup reduces risk of dislocation in isolated acetabular revisions. Clin Orthop Relat Res. (2012) 470:3542–8. doi: 10.1007/s11999-012-2428-y
28. Park YS, Moon YW, Lim BH, Shon MS, Lim SJ. A comparative study of the posterolateral and anterolateral approaches for isolated acetabular revision. Arch Orthop Trauma Surg. (2011) 131:1021–6. doi: 10.1007/s00402-011-1258-9
29. Cho HJ, Han SB, Park JH, Park SW. An analysis of stably fixed femoral components retained during revision total hip arthroplasty. J Arthroplasty. (2011) 26:1239–44. doi: 10.1016/j.arth.2011.02.015
30. Fukui K, Kaneuji A, Sugimori T, Ichiseki T, Kitamura K, Matsumoto T. Should the well-fixed, uncemented femoral components be revised during isolated acetabular revision? Arch Orthop Trauma Surg. (2011) 131:481–5. doi: 10.1007/s00402-010-1152-x
31. He C, Feng JM, Yang QM, Wang Y, Liu ZH. Results of selective hip arthroplasty revision in isolated acetabular failure. J Surg Res. (2010) 164:228–33. doi: 10.1016/j.jss.2009.06.023
32. Lawless BM, Healy WL, Sharma S, Iorio R. Outcomes of isolated acetabular revision. Clin Orthop Relat Res. (2010) 468:472–9. doi: 10.1007/s11999-009-1104-3
33. Min BW, Song KS, Cho CH, Bae KC, Lee KJ. Femoral osteolysis around the unrevised stem during isolated acetabular revision. Clin Orthop Relat Res. (2009) 467:1501–6. doi: 10.1007/s11999-008-0499-6
34. Kim YS, Kim YH, Hwang KT, Choi IY. Isolated acetabular revision hip arthroplasty with the use of uncemented cup. J Arthroplasty. (2009) 24:1236–40. doi: 10.1016/j.arth.2009.05.032
35. Moskal JT, Shen FH, Brown TE. The fate of stable femoral components retained during isolated acetabular revision: a six-to-twelve-year follow-up study. J Bone Joint Surg Am. (2002) 84:250–5. doi: 10.2106/00004623-200202000-00012
36. Poon ED, Lachiewicz PF. Results of isolated acetabular revisions: the fate of the unrevised femoral component. J Arthroplasty. (1998) 13:42–9. doi: 10.1016/s0883-5403(98)90074-2
37. Lim JW, Ridley D, Johnston LR, Clift BA. Acetabulum-only revision total hip arthroplasty is associated with good functional outcomes and survivorship. J Arthroplasty. (2017) 32:2219–2225.e1. doi: 10.1016/j.arth.2017.02.007
38. Laffosse JM. Removal of well-fixed fixed femoral stems. Orthop Traumatol Surg Res. (2016) 102:S177–87. doi: 10.1016/j.otsr.2015.06.029
39. Philpott A, Weston-Simons JS, Grammatopoulos G, Bejon P, Gill HS, McLardy-Smith P, et al. Predictive outcomes of revision total hip replacement—a consecutive series of 1176 patients with a minimum 10-year follow-up. Maturitas. (2014) 77:185–90. doi: 10.1016/j.maturitas.2013.10.019
40. Springer BD, Fehring TK, Griffin WL, Odum SM, Masonis JL. Why revision total hip arthroplasty fails. Clin Orthop Relat Res. (2009) 467:166–73. doi: 10.1007/s11999-008-0566-z
41. Hasegawa M, Tone S, Naito Y, Wakabayashi H, Sudo A. Minimum ten-year results in revision total hip arthroplasty using titanium fully porous long stem. Int Orthop. (2021) 45:1727–33. doi: 10.1007/s00264-021-05030-4
42. Imbuldeniya AM, Walter WK, Zicat BA, Walter WL. The S-ROM hydroxyapatite proximally-coated modular femoral stem in revision hip replacement: results of 397 hips at a minimum ten-year follow-up. Bone Joint J. (2014) 96-b:730–6. doi: 10.1302/0301-620x.96b6.33381
43. Hernigou P, Dupuy N, Pidet O, Homma Y, Flouzat Lachaniette CH. Alumina heads minimize wear and femoral osteolysis progression after isolated simple acetabular revision. Clin Orthop Relat Res. (2012) 470:3094–100. doi: 10.1007/s11999-012-2363-y
44. Vaishya R, Chauhan M, Vaish A. Bone cement. J Clin Orthop Trauma. (2013) 4:157–63. doi: 10.1016/j.jcot.2013.11.005
45. Emerson RH Jr, Head WC, Emerson CB, Rosenfeldt W, Higgins LL. A comparison of cemented and cementless titanium femoral components used for primary total hip arthroplasty: a radiographic and survivorship study. J Arthroplasty. (2002) 17:584–91. doi: 10.1054/arth.2002.32696
46. Toci GR, Magnuson JA, DeSimone CA, Stambough JB, Star AM, Saxena A. A systematic review and meta-analysis of non-database comparative studies on cemented versus uncemented femoral stems in primary elective total hip arthroplasty. J Arthroplasty. (2022) 37(9):1888–94. doi: 10.1016/j.arth.2022.03.086
47. Moskal JT, Capps SG, Scanelli JA. Still no single gold standard for using cementless femoral stems routinely in total hip arthroplasty. Arthroplast Today. (2016) 2:211–8. doi: 10.1016/j.artd.2016.02.001
48. Jones CP, Lachiewicz PF. Factors influencing the longer-term survival of uncemented acetabular components used in total hip revisions. J Bone Joint Surg Am. (2004) 86:342–7. doi: 10.2106/00004623-200402000-00018
Keywords: retained femoral component, revision total hip arthroplasty, systematic review and meta-analysis, meta-regression, re-revision rate
Citation: Li H, Zhuang T, Wu W, Gan W, Wu C, Peng S, Huan S and Liu N (2022) Survivorship of the retained femoral component after revision total hip arthroplasty: A systematic review and meta-analysis. Front. Surg. 9:988915. doi: 10.3389/fsurg.2022.988915
Received: 7 July 2022; Accepted: 21 September 2022;
Published: 13 October 2022.
Edited by:
Songqiao Liu, Southeast University, ChinaReviewed by:
Peifu Tang, People’s Liberation Army General Hospital, ChinaRyan Chapman, University of Rhode Island, United States
© 2022 Li, Zhuang, Wu, Gan, Wu, Peng, Huan and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Songwei Huan am51aHVhbkAxNjMuY29t Ning Liu bGl1bmluZzA3OUAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Hua Li†
Hua Li† Wenyi Gan
Wenyi Gan Sijun Peng
Sijun Peng Ning Liu
Ning Liu