- Department of Thoracic Surgery, The First Affiliated Hospital of USTC, Division of Life Sciences and Medicine, University of Science and Technology of China, Hefei, China
Objective: To compare the short-term outcomes and postoperative quality of life in patients with esophageal cancer between inflatable videoasisted mediastinoscopic transhiatal esophagectomy (IVMTE) and minimally invasive Mckeown esophagectomy (MIME), and to evaluate the value of IVMTE in the surgical treatment of esophageal cancer.
Methods: A prospective, nonrandomized study was adopted. A total of 60 esophageal cancer patients after IVMTE and MIME December 2019 to January 2022 were included. Among them, 30 patients underwent IVMTE and 30 patients underwent MIME. Shortterm outcomes (including the operation time, intraoperative blood loss, postoperative drainage 3 days, total postoperative tube time, postoperative hospital stay, number and number of thoracic lymph node dissection stations, postoperative complications and so on), postoperative quality of life, [including Quality of Life Core Questionnaire (QLQ-C30) and the esophageal site-specific module (QLQ-OES18)] were compared between the 2 groups.
Results: The operation time, intraoperative blood loss, postoperative drainage volume and total postoperative intubation time in IVMTE group were significantly lower than those in MIME group (P < 0.05). A total of 22 patients had postoperative complications, including 7 patients in IVMTE group (23.3%) and 15 patients in MIME group (50.0%). There was significant difference between the two groups (P = 0.032). The physical function, role function, cognitive function, emotional function and social function and the overall health status in the IVMTE group were higher than those in the MIME group at all time points after operation, while the areas of fatigue, nausea, vomiting and pain symptoms in the MIME group were lower than those in the MIME group at all time points after operation.
Conclusion: IVMTE is a feasible and safe alternative to MIME. Therefore, when the case is appropriate, IVMTE should be given priority, which is conducive to postoperative recovery and improve the quality of life of patients after operation.
Introduction
Esophageal cancer (EC) is one of the most common malignant tumors, and its mortality rate is the fourth among all malignant tumors in the world (1, 2). With the development of minimally invasive endoscopic technology, minimally invasive surgery for esophageal cancer mainly includes minimally invasive McKeown esophagectomy, minimally invasive Ivor-Lewis esophagectomy and mediastinoscopic esophagectomy (3–5). The goal of tumor surgical treatment is to pursue a higher quality of life on the basis of ensuring tumor radical resection and surgical safety (6–8). Compared with open esophagectomy, thoracic laparoscopy combined with McKeown esophagectomy can significantly improve the postoperative quality of life of patients with esophageal cancer. In addition, with the continuous development of endoscopic surgery, mediastinoscopy combined with laparoscopy has become a new method for the treatment of esophageal cancer because of its advantages such as less trauma, less postoperative complications and less postoperative pain (9, 10). However, at present, there are few studies at home and abroad on whether inflatable videoasisted mediastinoscopic transhiatal esophagectomy (IVMTE) can further improve the postoperative quality of life without affecting the efficacy and safety of the operation. In this study, a prospective non-randomized study was conducted to analyze the clinical data of 60 patients who underwent IVMTE and minimally invasive McKeown esophagectomy (MIME) in the Department of Thoracic surgery of the First Affiliated Hospital of University of Science and Technology of China from December 2019 to January 2022. The clinicopathological data, perioperative data and short-term postoperative quality of life of the two groups were compared.
Materials and methods
Object of study
In this study, the clinical data of patients with IVMTE and MIME in the Department of Thoracic surgery of the First Affiliated Hospital of University of Science and Technology of China from December 2019 to January 2022 were collected prospectively and non-randomly. All patients received esophageal cancer resection and lymph node dissection. The inclusion criteria were as follows: (1) Postoperative pathological diagnosis of esophageal squamous cell carcinoma, (2) MIME or IVMTE combined with laparoscopic resection of esophageal cancer, (3) Did not receive neoadjuvant therapy before operation, (4) The operation is R0 resection. The exclusion criteria were as follows: (1) Distant metastasis was found during the operation, (2) Conversion to thoracotomy during operation, (3) The case data are incomplete.
Through the inclusion and exclusion criteria, 60 patients were included, including 43 males and 17 females, with an average age of 68.17 ± 8.474 years (range: 52–83 years). Patients were informed of two surgical methods before operation. first, patients were divided into groups according to their wishes, and patients who did not express special wishes decided the surgical methods according to their own conditions: IVMTE group (n = 30) and MIME group (n = 30).
All patients underwent blood routine, biochemistry, coagulation, immunohistochemistry, esophageal barium meal, electronic gastroscope, ultrasonic endoscopy, electrocardiogram, echocardiography, pulmonary function examination, chest + upper abdominal enhanced CT, neck and abdominal B-ultrasound examination to determine the size of the tumor, the depth of invasion, the relationship with surrounding tissues, the location and size of lymph nodes, and exclude distant metastasis and obvious invasion of esophageal tumors. Some patients underwent PET-CT for preoperative staging.
AJCC eighth edition TNM staging system was used for tumor staging. All patients were evaluated according to the American Association of Anesthesiologists (ASA) classification criteria before operation. Postoperative complications were evaluated by Clavien-Dindo surgical complication grading standard. The complications of Clavien-Dindo grade 1–2 were classified as minor complications and Clavien-Dindo grade 3–5 as major complications. This study was approved by the First Affiliated Hospital of University of Science and Technology of China (O.2022-RE-145).
Surgical procedures
IVMTE: After single-lumen endotracheal intubation anesthesia, the patient took the supine position, the shoulder and back pad was high, and the head was tilted back to the right to fully expose the left neck. A 3 cm cervical incision was made along the medial side of the left sternocleidomastoid muscle, cut layer by layer, separated the muscle group, dissociated the cervical esophagus, and marked to protect the recurrent laryngeal nerve. Place incision protective cover, jacket gloves to establish a closed cavity, mediastinal inflatable pressure 8 mmHg (1 mmHg = 0.133 kPa), flow 5 L-6/min, insert operating instruments. Dissociate downward along the left wall of the cervical esophagus in the order of “left-anterior-right posterior” to the level of subCarina or lower pulmonary ligament, and dissect the lymph nodes adjacent to the recurrent laryngeal nerve, esophagus and subCarina. Attention should be paid to the protection of recurrent laryngeal nerve, azygos vein arch and thoracic duct during operation. Abdominal operation and digestive tract reconstruction are the same as MIME.
MIME: The patient first took the left lateral decubitus and left one-lung ventilation. The fourth intercostal 2 cm incision of the right anterior axillary line was selected as the main operating hole, the 7th intercostal 1 cm incision of the midaxillary line was used as the mirror hole, and the 8th intercostal 1.5 cm incision between the posterior axillary line and the scapular line was used as the auxiliary operation hole. The azygos vein was ligated with HEMO-LOCK and then severed. Ultrasonic scalpel and electric hook were used to dissociate the thoracic esophagus. Finally, the lymph nodes adjacent to the recurrent laryngeal nerve, esophagus and Carina were routinely explored. The suspected enlarged lymph nodes were dissected during the operation, and no obvious enlarged lymph nodes were sampled. The horizontal position was taken at the end of the chest operation, and the abdominal operation was the same as that in the mediastinoscopy group. After the tube stomach was made, the incision along the medial edge of the left cervical sternocleidomastoid muscle was made, the cervical esophagus was dissociated, and the esophagus was pulled out through the cervical incision. the cervical esophagus was anastomosed end to side with a circular stapler, and after the anastomosis was completed, the gastric tube and duodenal nutrition tube were placed through the abdominal incision to close the abdominal incision and cervical incision.
Observation indicators
The clinicopathological data and perioperative indexes were collected. The clinicopathological data included sex, age, body mass index (BMI), tumor location, pTNM stage, tumor differentiation, ASA grade and preoperative comorbidities. Perioperative indexes included operation time, intraoperative blood loss, postoperative drainage 3 days, total postoperative tube time, postoperative hospital stay, number of lymph node dissection and number of lymph node dissection stations, postoperative complications and so on.
The quality of life was evaluated by Quality of Life Core Questionnaire (QLQ-C30) and the esophageal site-specific module (QLQ-OES18) evaluation scale of European Organization for Cancer treatment and Research. The evaluation time was 1 day before operation and 1, 2, 4 and 8 weeks after operation. QLQ-C30 is divided into 15 areas and 30 projects. Items 29 and 30 contain 7 grades with a score of 1–7, while the other items have 4 grades. 1–4 points are assigned respectively. The scale included functional areas (social function, cognitive function, physical function, emotional function, role function), symptom areas (fatigue, nausea and vomiting, pain), and general health status. And 6 single items (dyspnea, insomnia, loss of appetite, constipation, diarrhea, economic hardship). Divide the sum of project scores in each area by the number of projects, that is, the rough score in that field. The higher the score of functional index and comprehensive quality of life dimension, the better the function and the higher the quality of life; the higher the score of symptomatic index, the more serious the symptom and the worse the quality of life. The scores of each subscale were calculated as follows: functional subscale: s = {1-(RS-1)/range} * 100; symptom subscale: s = {(RS-1)/range} * 100; general health status subscale: s = {(RS-1)/range} * 100. Among them, RS represents the original score, Range represents the extremely poor score, the functional subscale and symptom subscale have a very poor score of 3, while the total health subscale has a very poor score of 6. The medical staff completed all the scales through face-to-face interview or telephone follow-up.
Statistical analyses
SPSS26.0 statistical software was used for data analysis. The normal distribution data are expressed by , the measurement data are compared by t-test, the counting data are compared by χ2 test, the skewed data are described by median M (P25-P75), and the comparison between the two groups is Wilcoxon rank sum test (statistics is Uc). Repeated measurement analysis of variance was used to compare the quality of life at different time points. P < 0.05 means that the difference is statistically significant.
Result
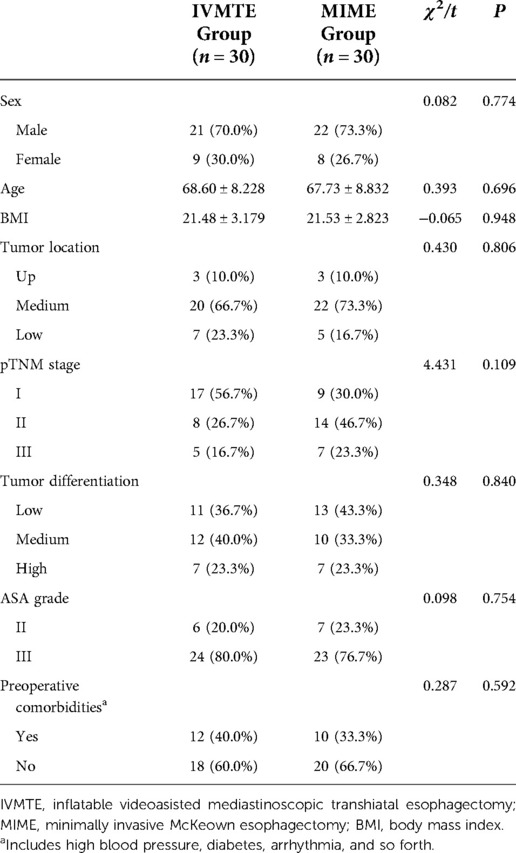
Comparison of clinicopathological data
There was no significant difference in sex, age, BMI, tumor location, pTNM stage, tumor differentiation, ASA grade and preoperative comorbidities between the two groups (P > 0.05, Table 1).
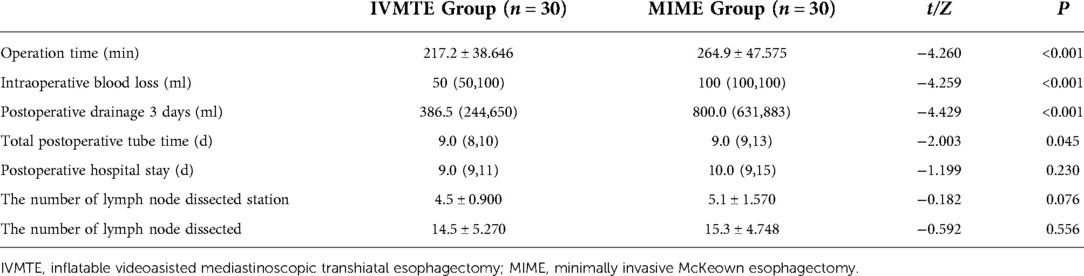
Comparison of perioperative data
The operation time, intraoperative blood loss, postoperative drainage 3 days and total postoperative tube time in IVMTE group were significantly lower than those in MIME group (P < 0.05, Table 2). There was no significant difference in postoperative hospital stay between IVMTE group and MIME group (P > 0.05, Table 2). There was no significant difference in the number of lymph node dissection and number of lymph node dissection stations between the two groups (P > 0.05, Table 2).
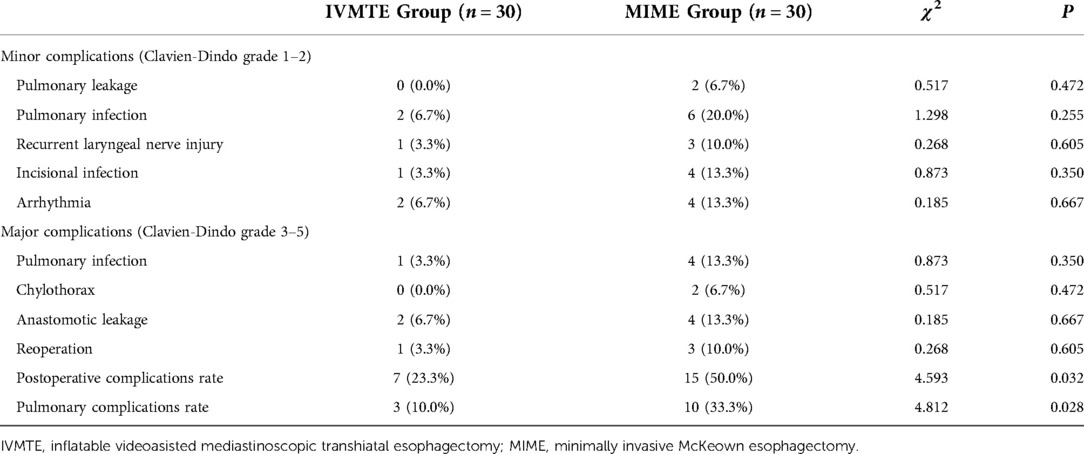
Postoperative complications
A total of 22 patients had postoperative complications, including 7 patients in IVMTE group (23.3%) and 15 patients in MIME group (50.0%). There was significant difference between the two groups (P = 0.032, Table 3). In addition, the incidence of pulmonary complications in the IVMTE group was lower than that in the MIME group, and the results were statistically significant (P < 0.05, Table 3). However, there was no significant difference in pulmonary infection, recurrent laryngeal nerve injury, incision infection and anastomotic leakage between the two groups (P > 0.05, Table 3).
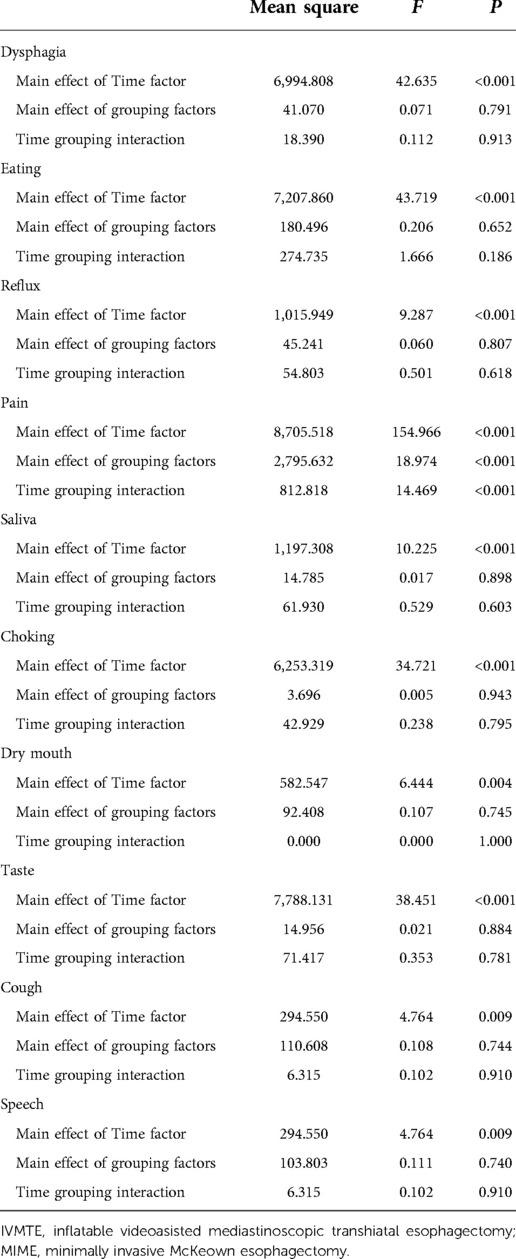
Comparison of quality of life
In terms of QLQ-C30 score, the preoperative functional domain, symptom domain and overall health scores of the two groups were similar, the functional domain and overall health scores decreased significantly 1 week after operation, and the scores increased gradually at 2, 4 and 8 weeks after operation, while the symptom domain scores increased significantly 1 week after operation, and the node scores decreased gradually at 2 weeks, 4 weeks and 8 weeks after operation. The physical function, role function, cognitive function, emotional function and social function and the overall health status in the IVMTE group were higher than those in the MIME group at all time points after operation, while the areas of fatigue, nausea, vomiting and pain symptoms in the MIME group were lower than those in the MIME group at all time points after operation (Table 4 and Figures 1A–I). In addition, the QLQ-OES18 score of the IVMTE group was lower than that of the MIME group at each time point after operation (Table 5 and Figure 2).
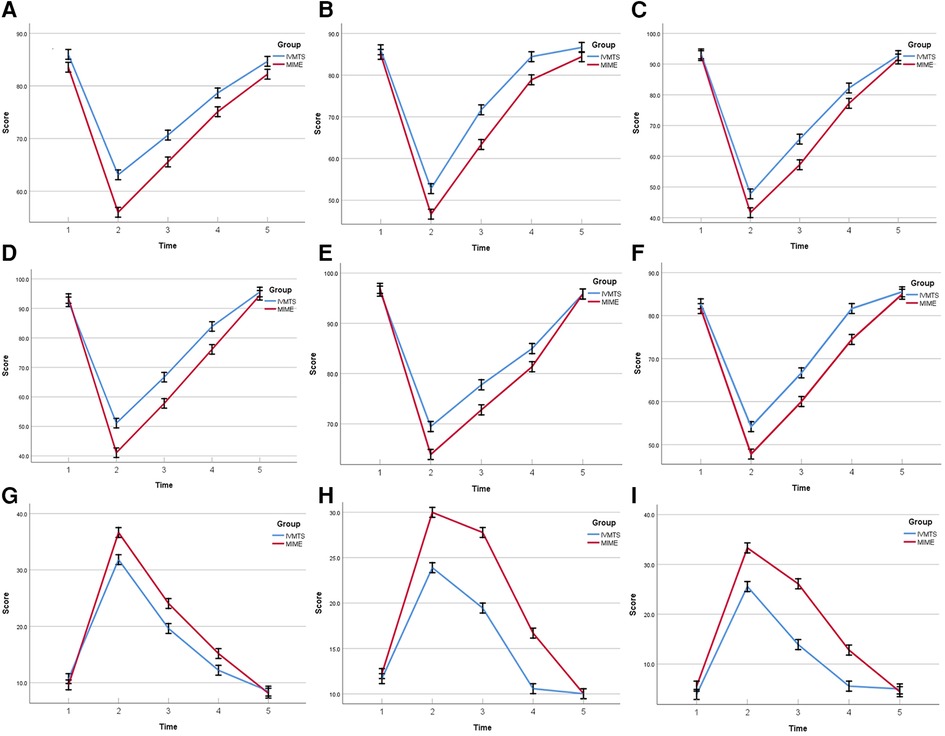
Figure 1. Comparison of QLQ-C30 scores between the two groups before and after operation. (A) Physical function. (B) Role function. (C) Cognitive function. (D) Social function. (E) Emotional function. (F) Global health status. (G) Fatigue. (H) Nausea/vomiting. (I) Pain. IVMTE, inflatable videoasisted mediastinoscopic transhiatal esophagectomy; MIME, minimally invasive Mckeown esophagectomy; Time 1, 1 day before operation; Time 2, 1 weeks after operation; Time 3, 2 weeks after operation; Time 4, 4 weeks after operation; Time 5;, 8 weeks after operation.
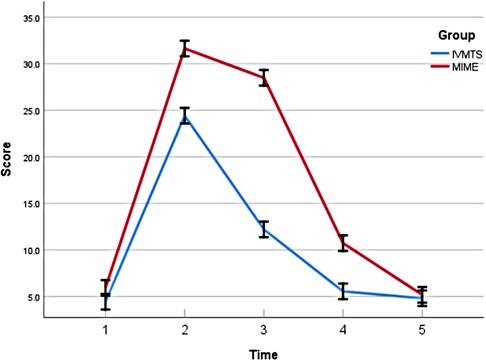
Figure 2. Comparison of QLQ-OES18 scores (pain) between the two groups before and after operation. IVMTE, inflatable videoasisted mediastinoscopic transhiatal esophagectomy; MIME, minimally invasive Mckeown esophagectomy; Time 1, 1 day before operation; Time 2, 1 weeks after operation; Time 3, 2 weeks after operation; Time 4, 4 weeks after operation; Time 5, 8 weeks after operation.
Discussion
With the progress of endoscopic technology, thoracic surgeons pursue minimally invasive surgery to achieve better surgical results and long-term prognosis. At the same time, we also pay attention to the impact of surgical methods on the quality of life of patients. Therefore, how to minimize the impact of surgery on patients is a hot issue concerned by thoracic surgeons. In addition, the impact of different surgical methods on the quality of life of surgical patients is unknown. The results of this study show that the same surgical effect can be achieved compared with MIME, IVMTE, and there are advantages in operation time, intraoperative blood loss, postoperative drainage 3 days and total postoperative tube time. In addition, in terms of postoperative complications, IVMTE is superior to MIME in the overall incidence of complications and the incidence of pulmonary complications. In the study of quality of life, IVMTE has advantages in many functional dimensions, such as physical function, role function and cognitive function, as well as in the overall health status and symptoms such as fatigue, nausea, vomiting and pain.
The pursuit of more minimally invasive surgery on the premise of ensuring the scope of oncology resection has always been the goal of thoracic surgeons. IVMTE can achieve or even better than the surgical effect of MIME and the range of lymph node dissection. In this study, it was found that IVMTE had shorter operation time, less intraoperative blood loss, less drainage 3 days after operation and shorter total time with catheter than MIME. In addition, there was no significant difference between IVMTE and MIME in the number of lymph node dissection stations and enumeration. Jin et al. (11) through a retrospective analysis of 30 MIME patients and 19 IVMTE patients, found that compared with MIME patients, IVMTE patients had shorter average operation time, less intraoperative blood loss, less drainage in the first 3 days after operation and less hospital stay. In addition, Jin et al. (11) found that there was no significant difference in the number and total number of lymph node dissection between the two groups. However, dissection of the right posterior recurrent lymph nodes in the MIME group was more common. Shi et al. (12) found that the operation time, intraoperative blood loss and postoperative hospital stay in IVMTE group were shorter than those in IVMTE group. We analyze the reasons for this result may be as follows: first, there is no need to change the position during the operation, only one position can be performed on the neck and abdomen, and the thoracic and abdominal operations can be performed at the same time, which greatly shortens the operation time and anesthesia time. Second, by inflating the mediastinum and endoscopic magnification, the anatomical structure around the esophagus can be clearly identified and the downstream from the esophagus can be seen, which avoids the blindness of the traditional esophagectomy and effectively reduces the injury of nerves, blood vessels and thoracic ducts during the operation. reduce the risk of surgical bleeding and postoperative tissue exudation. Third, there is no need to place thoracic drainage tube after operation and does not cause damage to the intercostal nerve, reduce postoperative drainage and postoperative pain, make patients get out of bed earlier and accelerate their recovery.
Postoperative complications have always been one of the key factors affecting the quality of life of patients after operation. According to the study of postoperative complications of the two surgical methods, it was found that the total incidence of postoperative complications and the incidence of pulmonary complications in IVMTE group were better than those in MIME group. However, there was no significant difference in postoperative complications such as pulmonary air leakage, pulmonary infection and recurrent laryngeal nerve injury between the two groups. Rezaei et al. (13) through the study of 31 cases of IVMTE and 31 cases of MIME esophageal cancer, found that the incidence of early postoperative complications and postoperative cardiopulmonary complications in IVMTE was lower than that in MIME. Chen et al. (14) found that the incidence of postoperative pulmonary complications in IVMTE was lower than that in MIME through retrospective analysis of propensity matching. We analyze the following possible reasons for this result: first, the failure to choose the transthoracic approach reduces the possible mechanical damage to the heart, lung and other important organs during the operation, and reduces the probability of cardiovascular and pulmonary complications. Second, it avoids intercostal nerve injury and reduces postoperative pain, which is beneficial to patients’ effective cough and expectoration, and promotes the reexpansion of the lung and the oxygenation state of the patients. Third, there is no need to cut off azygos vein and bronchial artery during operation, which avoids liver function injury in some patients with liver insufficiency and reduces the probability of postoperative cough.
With the continuous improvement of social material living standards, while treating diseases, postoperative quality of life has also become an important index for doctors and patients to pay attention to. In this study, we used the QLQ-C30 and QLQ-OES18 scales of the European Organization for Cancer treatment and Research to evaluate the quality of life. The results showed that there was no difference in the scores of preoperative functional areas, symptom areas and overall health status between the two groups, but there were significant advantages in multiple quality of life dimensions between the IVMTE group and the MIME group. The above results show that IVMTE has less influence on all dimensions of postoperative quality of life of patients with esophageal cancer than MIME. On the other hand, it also reflects the advantage of less trauma and faster recovery of IVMTE in patients with esophageal cancer. Through a prospective non-randomized study, Ma et al. (15) found that the scores of emotional function and overall health scale of QLQ-C30 in MIE-SM group were significantly higher than those in MIE-MC group, while the pain score in MIE-SM group was significantly lower than that in MIE-MC group. QLQ-OES18 results showed that the pain score in MIE-SM group was significantly lower than that in MIE-MC group. We believe that the main reasons are: first, because the IVMTE operation time is shorter, the intraoperative blood loss is less and the total postoperative intubation time is shorter, patients can do physical function exercise and receive nutritional support earlier, so that they can return to normal life and work more quickly. Second, IVMTE avoids intercostal nerve injury, lightens postoperative pain, reduces postoperative discomfort, reduces negative emotions, and helps to improve postoperative quality of life. Third, the incidence of postoperative complications in IVMTE group is lower, so that patients can recover their life and work status earlier. In addition, low postoperative complications can reduce patients’ fear of surgery and contribute to the improvement of postoperative quality of life.
This study has the following shortcomings: first, this study is a single-center prospective non-random study, the sample size is relatively small, may have a little bias to the results. Second, this study did not carry out long-term follow-up of the two groups of patients, and whether the two surgical methods can achieve the same long-term prognosis has not been studied. Thirdly, postoperative radiotherapy and chemotherapy may affect the evaluation of postoperative quality of life.
Conclusion
IVMTE can reduce intraoperative bleeding, shorten operation time and reduce postoperative complications, and improve the short-term postoperative quality of life of patients with esophageal cancer. IVMTE is a feasible and safe alternative to MIME. Therefore, when the case is appropriate, IVMTE should be given priority, which is conducive to postoperative recovery and improve the quality of life of patients after operation.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
GW: Conceptualization, Methodology, Software, Investigation, Writing—original draft, Writing—review & editing. XS: Visualization, Investigation. TL: Visualization, Investigation. MX: Software, Validation. MG: Software, Validation. CL Writing—review & editing. MX: Funding acquisition, Writing—review & editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the grants from the National Natural Science Foundation of China and Key research and development projects of Anhui Province (NO. 81973643 and 202004j07020017).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2021. CA Cancer J Clin. (2021) 71(1):7–33. doi: 10.3322/caac.21654
2. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. (2021) 71(3):209–49. doi: 10.3322/caac.21660
3. Shi Y, Wang A, Yu S, Fei X, Liu S, Liao J. Thoracoscopic-laparoscopic Ivor-Lewis surgery vs. McKeown surgery in the treatment of thoracic middle-lower segment esophageal cancer. J Buon. (2021) 26(3):1062–9. PMID: 34268973
4. Xie MR, Liu CQ, Guo MF, Mei XY, Sun XH, Xu MQ. Short-term outcomes of minimally invasive Ivor-Lewis esophagectomy for esophageal cancer. Ann Thorac Surg. (2014) 97(5):1721–7. doi: 10.1016/j.athoracsur.2014.01.054
5. Ye H, Wang X, Li X, Gan X, Zhong H, Wu X, et al. Effect of single-port inflatable mediastinoscopy simultaneous laparoscopic-assisted radical esophagectomy on respiration and circulation. J Cardiothorac Surg. (2021) 16(1):288. doi: 10.1186/s13019-021-01671-z
6. Shanmugasundaram R, Hopkins R, Neeman T, Beenen E, Fergusson J, Gananadha S. Minimally invasive McKeown’s vs open oesophagectomy for cancer: a meta-analysis. Eur J Surg Oncol. (2019) 45(6):941–9. doi: 10.1016/j.ejso.2018.11.017
7. Chen D, Wang W, Mo J, Ren Q, Miao H, Chen Y, et al. Minimal invasive versus open esophagectomy for patients with esophageal squamous cell carcinoma after neoadjuvant treatments. BMC Cancer. (2021) 21(1):145. doi: 10.1186/s12885-021-07867-9
8. Moon DH, Lee JM, Jeon JH, Yang HC, Kim MS. Clinical outcomes of video-assisted thoracoscopic surgery esophagectomy for esophageal cancer: a propensity score-matched analysis. J Thorac Dis. (2017) 9(9):3005–12. doi: 10.21037/jtd.2017.08.71
9. Yin Q, Liu H, Song Y, Zhou S, Yang G, Wang W, et al. Clinical application and observation of single-port inflatable mediastinoscopy combined with laparoscopy for radical esophagectomy in esophageal squamous cell carcinoma. J Cardiothorac Surg. (2020) 15(1):125. doi: 10.1186/s13019-020-01168-1
10. Wang X, Li X, Cheng H, Zhang B, Zhong H, Wang R, et al. Single-port inflatable mediastinoscopy combined with laparoscopic-assisted small incision surgery for radical esophagectomy is an effective and safe treatment for esophageal cancer. J Gastrointest Surg. (2019) 23(8):1533–40. doi: 10.1007/s11605-018-04069-w
11. Jin Y, Lu X, Xue L, Zhao X. Retrospective comparison of two minimally invasive esophagectomy in the treatment of esophageal cancer: pneumatic mediastinoscopy versus thoracoscopy. J Laparoendosc Adv Surg Tech A. (2019) 29(5):638–42. doi: 10.1089/lap.2018.0512
12. Shi K, Qian R, Zhang X, Jin Z, Lin T, Lang B, et al. Video-assisted mediastinoscopic and laparoscopic transhiatal esophagectomy for esophageal cancer. Surg Endosc. (2022) 36(6):4207–14. doi: 10.1007/s00464-021-08754-x
13. Rezaei R, Masuom SHF, Soroush N, Zehi V. Comparison of transhiatal esophagectomy using a mediastinoscope with transhiatal esophagectomy by the classic method. Asian Cardiovasc Thorac Ann. (2021) 29(1):33–7. doi: 10.1177/0218492320963976
14. Chen Z, Huang K, Wei R, Liu C, Fang Y, Wu B, et al. Transcervical inflatable mediastinoscopic esophagectomy versus thoracoscopic esophagectomy for local early- and intermediate-stage esophageal squamous cell carcinoma: a propensity score-matched analysis. J Surg Oncol. (2022) 125(5):839–46. doi: 10.1002/jso.26798
15. Ma J, Wang W, Zhang B, Li X, Wu J, Wu Z. Minimally invasive esophagectomy via sweet approach in combination with cervical mediastinoscopy is a valuable approach for surgical treatment of esophageal cancer. Zhong Nan Da Xue Xue Bao Yi Xue Ban. (2021) 46(1):60–8. doi: 10.11817/j.issn.1672-7347.2021.190568
Keywords: esophageal cancer, minimally invasive esophagectomy, mediastinoscopy, QLQ-C30, surgery
Citation: Wang G, Sun X, Li T, Xu M, Guo M, Liu C and Xie M (2023) Study of the short-term quality of life of patients with esophageal cancer after inflatable videoassisted mediastinoscopic transhiatal esophagectomy. Front. Surg. 9:981576. doi: 10.3389/fsurg.2022.981576
Received: 6 July 2022; Accepted: 11 November 2022;
Published: 6 January 2023.
Edited by:
Kelechi E. Okonta, University of Port Harcourt Teaching Hospital, NigeriaReviewed by:
Jose Belda Sanchis, Hospital de la Santa Creu i Sant Pau, SpainXie Xuan, Sun Yat-sen Memorial Hospital, China
© 2023 Wang, Sun, Li, Xu, Guo, Liu and Xie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mingran Xie eG1yMTk4MUB1c3RjLmVkdS5jbg== Changqing Liu bGl1Y2hhbmdxaW5nYWhAMTYzLmNvbQ==
Specialty Section: This article was submitted to Thoracic Surgery, a section of the journal Frontiers in Surgery
 Gaoxiang Wang
Gaoxiang Wang Xiaohui Sun
Xiaohui Sun Mingran Xie
Mingran Xie