
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 10 October 2022
Sec. Cardiovascular Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.972264
Objective: This study aims to compare clinical outcomes between mini-sternotomy and full median sternotomy for aortic valve replacement using propensity-matching methods.
Methods: From August 2014 to July 2021, a total of 1,445 patients underwent isolated aortic valve surgery, 1,247 via full median sternotomy and 198 via mini-sternotomy. To reduce the impact of potential confounding factors, a propensity score based on 18 variables is used to obtain 198 well-matched case pairs, which include 231 aortic valve regurgitations and 165 aortic stenosis cases.
Result: Occurrences of in-hospital mortality (P = 0.499), stroke (P > 0.999), renal failure (P = 0.760), and paravalvular leakage (P = 0.224) are similar between the two groups. No significant difference in operation, cardiopulmonary bypass, and aortic cross-clamp times are found between the two groups. However, compared with the full sternotomy group, the mini-sternotomy group has less postoperative 24-hour drainage (131.7 ± 82.8 ml, P < 0.001) and total drainage (459.3 ± 306.3 ml, P < 0.001). The median mechanical ventilation times are 9.4 [interquartile range (IQR) 5.4–15.6] and 9.8 (IQR 6.1–14.4) in mini-sternotomy and full sternotomy groups (P = 0.284), respectively. There are no significant differences in intensive care unit stay and postoperative stay between the two groups. For either aortic valve regurgitations or aortic stenosis patients, significantly less postoperative 24-h and total drainage are still found in the mini-sternotomy group compared with the full sternotomy group.
Conclusions: Mini-sternotomy for aortic valve replacement is a safe procedure, with not only cosmetic advantages but less postoperative drainage compared with full sternotomy. Mini-sternotomy should be considered for most aortic valve operations.
Aortic valve replacement (AVR) is the one of most frequent cardiac surgery in the world. Currently, most AVRs are performed safely with full median sternotomy (FS), but the sternotomy-related complications such as markedly visible midline scar, postoperative pain, and respiratory tract infection make some patients not accept this conventional surgical approach. To reduce surgical trauma, several minimally invasive approaches have been developed for AVR since 1993 and have been associated with optimal outcomes compared with full sternotomy (1–4). The most common minimally invasive approach involves a mini-sternotomy (MS) with less spreading of the incision, not interfering with the diaphragm and less tissue dissection. Many studies have documented that MS may be associated with less bleeding, fewer transfusion requirement, shorter intensive care unit (ICU) and hospital stay despite longer operative, cardiopulmonary bypass (CPB), and cross-clamp times (5–9). Even though definitive clinical evidence is still lacking, the advantages of less pain, less bleeding, and improved cosmesis are generally accepted by patients and cardiac surgeons (10, 11).
Despite these potential advantages of MS for AVR, full sternotomy remains the most widely used approach in isolated aortic valve operation. Therefore, to evaluate the potential benefits of a mini-sternotomy approach, we performed a propensity-matched comparison of short-term outcomes in patients who had mini-sternotomy aortic valve surgery compared with patients who accepted full sternotomy.
We identified 1,445 patients who underwent isolated aortic valve surgery, including 1,247 patients via full median sternotomy and 198 patients via mini-sternotomy, from August 2014 to July 2021 at Fuwai Hospital in Beijing. The study protocol was reviewed and approved by the Ethics Committee of Fuwai Hospital on November 24, 2020 (Approval No. 2020-1402). Patients fulfilling these criteria were excluded: (1) Age <18 years; (2) Undergoing concomitant operations, such as mitral valve surgery, ascending aorta replacement, or coronary artery bypass grafting; (3) Active endocarditis. Diagnoses were decided based on echocardiography. Patients are divided into two groups: the FS group (1,247 patients) and the MS group (198 patients). Figure 1 shows the flow chart. Data are retrieved acquired by reviewing each patient's medical records, including operative reports, examination reports, and outpatient clinic notes.
All patients included in the study were operated on by surgeons with similar seniority in the same department of cardiovascular surgery. The patients are in the supine position. Skin is incised from the sternal angle to the level of the third intercostal space, approximately 5–7 cm. The manubrium is divided from the suprasternal notch to the right fourth intercostal space forming a J. The pericardium is opened to expose the ascending aorta, aortic root, and right atrial appendage. The aorta is cannulated conventionally and the right atrial appendage is cannulated using a flat venous cannula. After activated clotting time >450 s, CPB is initiated. The ascending aorta is cross-clamped. The approach to the aortic valve is via an oblique aortotomy carried into the noncoronary cusp above the sinotubular junction. Cold blood cardioplegia was administered through the coronary ostium. The diseased valve is excised, and a suitably sized aortic valve prosthesis is inserted using horizontal mattress interrupted sutures. After the resumption of heartbeat, ventricular epicardial pacing wires are inserted, and the patient is weaned off CPB. Usually, the pleura is complete, drainage tubes are placed into the anterior mediastinum and posterior pericardial space (Figure 2).
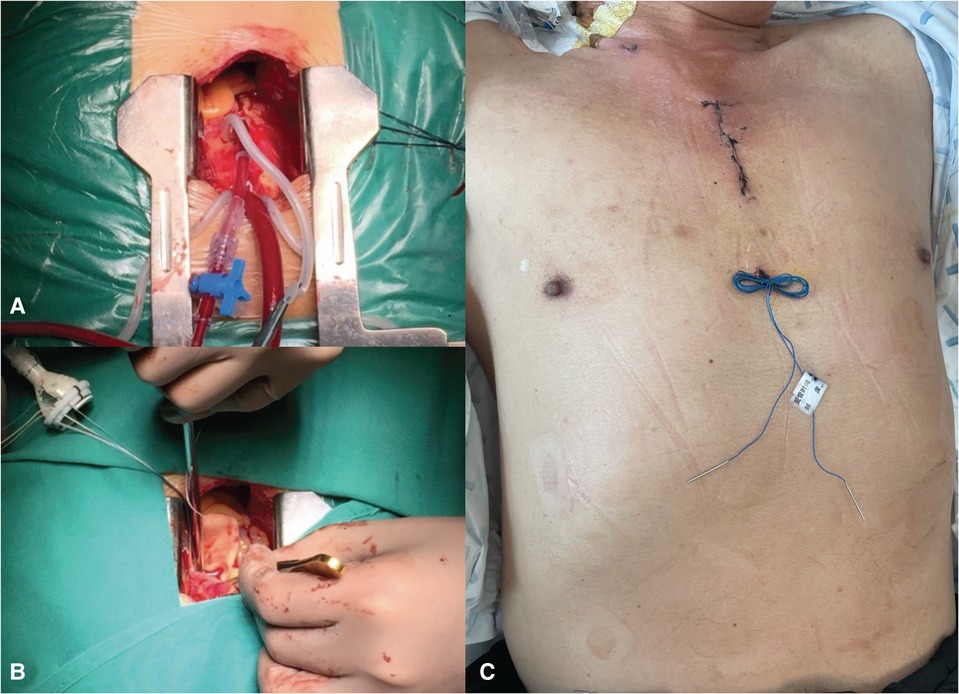
Figure 2. The mini-sternotomy AV replacement procedure. (A) The pericardium was opened to expose the ascending aorta, aortic root, and right atrial appendage. The aorta was cannulated conventionally. (B) The approach to the aortic valve was via an oblique aortotomy carried into the noncoronary cusp above the sinotubular junction. A suitably sized aortic valve prosthesis was inserted using horizontal mattress interrupted sutures. (C) Skin was incised from the sternal angle to the level of the fourth intercostal space, approximately 5–6 cm. AV, aortic valve.
Statistical analysis is performed using SPSS (version 24.0; SPSS Inc., Chicago, IL, United States). Categorical data are presented as numbers (percentage) and continuous variables as means and standard deviations or medians with interquartile ranges (IQRs). A 1:1 propensity score matching (PSM) of FS and MS minimized this potential bias. The propensity scores are estimated with multivariable logistic regression models. Standardized mean differences for all baseline covariates are less than 10% in the matched sample, which suggests a balance of covariates between the FS and MS groups. The matched covariates included gender, age, weight, smoking, aortic valve regurgitation, aortic valve stenosis, history of diabetes, hypertension, previous stroke, atrial fibrillation, chronic renal dysfunction, preoperative lab test (hemoglobin, platelet count, and activated partial thromboplastin time), EUROSCORE, SINOSCORE, preoperative left ventricular end diastolic diameter, and left ventricular ejection fraction. The final PSM sample consists of 198 well-matched pairs of full median sternotomy and mini-sternotomy patients. All patients only accepted isolated aortic valve replacement procedures, including 231 aortic valve regurgitations and 165 aortic stenosis cases. The significant difference is assessed using Pearson's chi-square or Fisher's exact test for categorical variables. Continuous variables are compared using the Student's paired t-test or Wilcoxon signed-rank test between the two groups. The α < 0.05 (alpha error level) is considered to be statistically significant.
The demographic and clinical characteristics of patients are presented in Table 1. Briefly, patients in the FS group were at a significantly younger age than those in the MS group (P = 0.033), and patients with mini-sternotomy had more weight than patients with full median sternotomy (P = 0.030). Compared with MS group, FS group had a more EUROSCORE [4 (IQR 3–5) vs. 2 (IQR 0–3), P < 0.001) and SINOSCORE [9 (IQR 7–10) vs. 4 (IQR 4–7), P < 0.001). There were no statistically significant differences in aortic valve regurgitation, aortic valve stenosis, history of diabetes, hypertension, and previous stroke between the two groups. After PSM adjustment, all clinical covariates were well balanced.
After PSM, we compared the perioperative variables between the two groups. No statistically significant differences in CPB, aortic cross-clamp time, and operative time were found, but the MS group tends to have less CPB time (89.8 ± 42.7 vs. 94.2 ± 41.9, P = 0.078). Patients from the FS group had more 24-h (P < 0.001) and total drainage (P < 0.001); however, there are no significant differences in transfusion events including plasma, red blood cell (RBC), and platelets between the two groups. Compared with patients in the FS group, there were no significant more reoperation, intra-aortic balloon pump (IABP), hemofiltration, and re-intubated events in the MS group. The mechanical ventilation time (MVT), ICU stay, and postoperative stay in MS group are similar to those of FS group. Moreover, no significant difference between postoperative stroke and acute renal failure was found between the two groups. There were four in-hospital deaths in the FS group and the number became two after PSM, while there is no in-hospital death in the MS group (P = 0.211). Even with no significant difference, FS group tends to have more incision infections (four patients before PSM, one patient after PSM). Paravalvular leakage in the MS group was similar to that in the FS group (P = 0.459). Details are shown in Table 2.
In aortic valve regurgitations patients, significantly less postoperative 24-h (129.2 ± 87.3 vs. 195.4 ± 98.5, P < 0.001) and total drainage (429.3 ± 216.5 vs. 694.8 ± 208.5, P < 0.001) are found in the mini-sternotomy group compared with full sternotomy group. In aortic stenosis patients, the results are similar (24-h drainage: 142.6 ± 79.8 vs. 188.3 ± 91.2, P < 0.001; total drainage: 472.3 ± 244.6 vs. 622.4 ± 214.5, P < 0.001). Table 3 shows these details.
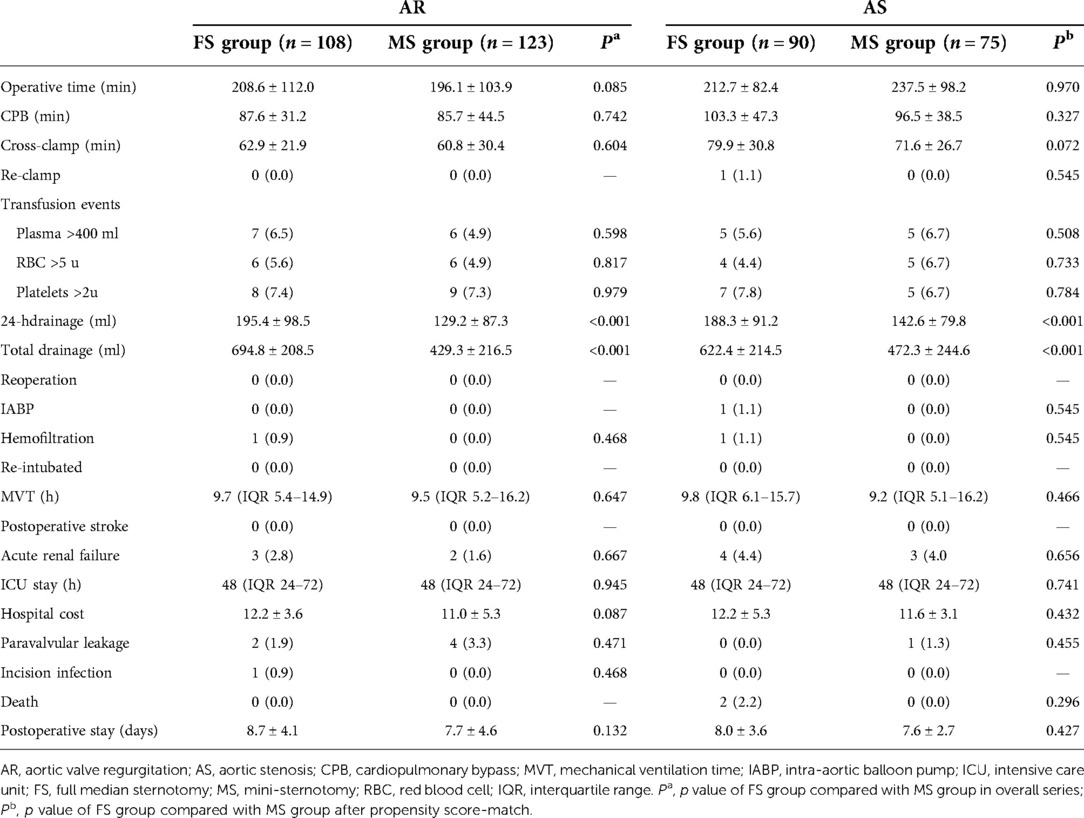
Table 3. In-hospital outcomes in propensity score-matched pairs for aortic valve regurgitation and aortic stenosis subgroup.
Patients are increasingly aware of minimally invasive options for cardiac surgery. However, concerns have been raised that aortic valve replacement with mini-incision may result in longer operative, CPB, and aortic clamp time, increasing the risk of postoperative adverse events (12, 13). In this case, the benefits of cosmesis and less bleeding might not be worth the increased risk of complications. Even though some studies reported that compared with standard full median sternotomy, mini-sternotomy has shown excellent outcomes in terms of postoperative complications and hospital stay, controversies still exist. Our study weighted by propensity-matching methods compared clinical outcomes between MS and FS for aortic valve replacement and confirmed that the mini-sternotomy procedure is safe, and associated with low perioperative complications.
In general, minimal access valve operations mean a reduction of working space and poor exposure, which make a large technical challenge, reflecting the longer operative, aortic cross-clamp, and CPB times. Nair et al. reported the results of an randomized controlled trial (RCT) study, which shows aortic cross-clamp and CPB times were significantly prolonged by MS (14). That has raised some concerns regarding the safety of mini-sternotomy especially in high-risk patients, for the longer CPB and cross-clamp times might increase the risk of perioperative complications. Our study indicates that there are no significant differences in operation, aortic cross-clamp, and CPB times between MS and FS group. Since 2004, minimal access valve operations have been made in our centers and many surgeons have completed training in the mini-incision technique. Even for some senior surgeons, less operative time in MS aortic valve replacement than FS approach because only half of the manubrium and shorter incision need to be closed. In this study, no mini-incisions were converted to full sternotomy.
A retrospective propensity-matched analysis of data concluded that MS is safe and does not increase the risk of postoperative complications (15). Even two meta-analyses concluded that aortic valve replacement with mini-incision approaches is superior in certain aspects of postoperative recovery (16, 17). Our study shows similar results that compared with patients in the FS group, no significant more IABP, hemofiltration, postoperative stroke, acute renal failure, and in-hospital death are found in the MS group. Our result shows less postoperative drainage in the MS group, which is likely due to the smaller mediastinal dissection required for the less invasive approach. Some similar results had been reported (6, 18). To prevent bias, we analyzed patient classification, and in either aortic valve regurgitations or aortic stenosis subgroup, patients with mini-sternotomy have significantly less postoperative 24-h and total drainage compared to those with full sternotomy.
Generally, the rate of incision infection was higher in the patients who underwent full median sternotomy procedures, but in our study, only one patient in the FS group had incision infection and the difference was not statistically significant. In a word, this study shows no disadvantages of mini-sternotomy and less postoperative drainage. So, mini-sternotomy for aortic valve replacement is a safe procedure.
This study still has several limitations. It is based on a retrospective analysis of a single center; thus, it only reflects single-center experience. The decision as to whether to perform MS or FS was likely based on multiple factors that may not have been completely collected in this retrospective review. We used propensity score matching to reduce the impact of potential confounding factors. However, after matching, there were only 198 cases in each group. In the future, more cases from multicenter will be enrolled to confirm the conclusion.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
X-qW contributed to the project design and clinical supervision. SH contributed to making ideas and echo supervision. RL contributed to the statistical analysis and writing of the manuscript. JC and JS contributed to the follow-up of patients and data collection. Statistical analysis was supervised by JS. All authors contributed to the article and approved the submitted version.
This study was supported by the CAMS Innovation Fund for Medical Sciences (CIFMS): I2M-C/T-B-061 and Chinese Academy of Medical Sciences: 2019-RC-HL-003.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Rao PN, Kumar AS. Aortic valve replacement through right thoracotomy. Tex Heart Inst J. (1993) 20:307–8. PMID: 8298332; PMCID: 325118
2. Cosgrove DM, Sabik JF. Minimally invasive approach for aortic valve operations. Ann Thorac Surg. (1996) 62:596–7. doi: 10.1016/0003-4975(96)00418-3
3. Von Segesser LK, Westaby S, Pomar J, Loisance D, Groscurth P, Turina M. Less invasive aortic valve surgery: rationale and technique. Eur J Cardiothorac Surg. (1999) 15:781–5. doi: 10.1016/S1010-7940(99)00119-0
4. Ruttmann E, Gilhofer TS, Ulmer H, Chevtchik O, Kocher A, Schistek R, et al. Propensity score-matched analysis of aortic valve replacement by mini-thoracotomy. J Heart Valve Dis. (2010) 19:606–14. PMID: 21053740
5. Merk DR, Lehmann S, Holzhey DM, Dohmen P, Candolfi P, Misfeld M, et al. Minimal invasive aortic valve replacement surgery is associated with improved survival: a propensity-matched comparison. Eur J Cardiothorac Surg. (2015) 47:11–7. doi: 10.1093/ejcts/ezu068
6. Furukawa N, Kuss O, Aboud A, Schönbrodt M, Renner A, Meibodi KH, et al. Ministernotomy versus conventional sternotomy for aortic valve replacement: matched propensity score analysis of 808 patients. Eur J Cardiothorac Surg. (2014) 46:221–6. doi: 10.1093/ejcts/ezt616
7. Tabata M, Umakanthan R, Cohn LH, Bolman RM 3rd, Sheakar PS, Chen FY, et al. Early and late outcomes of 1000 minimally invasive aortic valve operations. Eur J Cardiothorac Surg. (2008) 33:537–41. doi: 10.1016/j.ejcts.2007.12.037
8. Brown ML, McKellar SH, Sundt TM, Schaff HV. Ministernotomy versus conventional sternotomy for aortic valve replacement: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. (2009) 137:670–9. doi: 10.1016/j.jtcvs.2008.08.010
9. Brinkman WT, Hoffman W, Dewey TM, Culica D, Prince SL, Herbert MA, et al. Aortic valve replacement surgery: comparison of outcomes in matched sternotomy and port access groups. Ann Thorac Surg. (2010) 90:131–5. doi: 10.1016/j.athoracsur.2010.03.055
10. Johnston DR, Atik FA, Rajeswaran J, Blackstone EH, Nowicki ER, Sabik JR III, et al. Outcomes of less invasive J-incision approach to aortic valve surgery. J Thorac Cardiovasc Surg. (2012) 144:852–8. doi: 10.1016/j.jtcvs.2011.12.008
11. Shekar PS. Minimal access aortic valve surgery through an upper hemisternotomy approach. Oper Tech Thorac Cardiovasc Surg. (2010) 15:321–35. doi: 10.1053/j.optechstcvs.2010.11.001
12. Flameng W, Herregods MC, Hermans H, Van der Mieren G, Vercalsteren M, Poortmans G, et al. Effect of sutureless implantation of the perceval S aortic valve bioprosthesis on intraoperative and early postoperative outcomes. J Thorac Cardiovasc Surg. (2011) 142:1453–7. doi: 10.1016/j.jtcvs.2011.02.021
13. Folliguet TA, Laborde F, Zannis K, Ghorayeb G, Haverich A, Shrestha M. Sutureless perceval aortic valve replacement: results of two European centers. Ann Thorac Surg. (2012) 93:1483–8. doi: 10.1016/j.athoracsur.2012.01.071
14. Nair SK, Sudarshan CD, Thorpe BS, Singh J, Pillay T, Catarino P, et al. Mini-stern trial: a randomized trial comparing mini-sternotomy to full median sternotomy for aortic valve replacement. J Thorac Cardiovasc Surg. (2018) 156(6):2124–32. doi: 10.1016/j.jtcvs.2018.05.057
15. Attia RQ, Hickey GL, Grant SW, Bridgewater B, Roxburgh JC, Kumar P, et al. Minimally invasive versus conventional aortic valve replacement: a propensity-matched study from the UK national data. Innovations (Phila). (2016) 11:15–23. doi: 10.1097/imi.0000000000000236
16. Lim JY, Deo SV, Altarabsheh SE, Jung SH, Erwin PJ, Markowitz AH, et al. Conventional versus minimally invasive aortic valve replacement: pooled analysis of propensity-matched data. J Card Surg. (2015) 30:125–34. doi: 10.1111/jocs.12493
17. Phan K, Xie A, Di Eusanio M, Yan TD. A meta-analysis of minimally invasive versus conventional sternotomy for aortic valve replacement. Ann Thorac Surg. (2014) 98:1499–511. doi: 10.1016/j.athoracsur.2014.05.060
Keywords: mini-sternotomy, aortic valve replacement, MS, FS, cosmetic incision
Citation: Liu R, Song J, Chu J, Hu S and Wang X-q (2022) Comparing mini-sternotomy to full median sternotomy for aortic valve replacement with propensity-matching methods. Front. Surg. 9:972264. doi: 10.3389/fsurg.2022.972264
Received: 18 June 2022; Accepted: 12 September 2022;
Published: 10 October 2022.
Edited by:
Enyi Shi, China Medical University, ChinaReviewed by:
Vito Domenico Bruno, University of Bristol, United Kingdom© Liu, Song, Chu, Hu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xianqiang Wang bGh0ZnV3YWlAMTYzLmNvbQ==
Specialty Section: This article was submitted to Heart Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.