- Department of Orthopedics, Clinical Medical College of Yangzhou University, Northern Jiangsu People's Hospital, Yangzhou, China
Background: Patella fractures that require surgery are conventionally treated using Kirschner wires (K-wires) and stainless steel wires. In recent years, the nonabsorbable polyester has been reported to have excellent outcomes clinically. Therefore, the goal of our study was to evaluate the effects of Kirschner wires combined with 5-Ethibond on treating patellar fractures.
Methods: From July 2018 to January 2022, 22 patella fracture patients were treated with Kirschner wires combined with 5-Ethibond. Radiographs of the knees were used to evaluate fracture healing and hardware complications. The clinical results were evaluated through the functional score, knee joint range of motion (ROM), and Bostman patella fracture functional score.
Results: The average age of patients was 57.4 ± 11.9 (range 33–74) years. The mean follow-up time was 15.2 ± 7.6 (range 4–36) months. The mean operation time was 56.8 ± 8.7 (range 45–80) min. The entire patients had bony union at an average of 10.5 ± 1.9 (range 8–14) weeks. At the final follow-up, the mean range of postoperative ROM was 123.4° ± 14.6° (range 95°–140°), and the functional score was 28.7 ± 1.2 (range 26–30) points. No patient exhibited internal fixation failure, and no symptomatic implants or skin complications were recorded.
Conclusions: The fixation approach using K-wires combined with 5-Ethibond has a lower complication rate and delivers superior clinical results. This research reveals that such technology is a safe and prospective substitute for conventional metal fixation approaches.
Introduction
Patella fractures account for approximately 1% of all skeletal fractures (1, 2) and are usually caused by the forceful contraction of the quadriceps femoris. These fracture features can be transverse, perpendicular, or stellate. Open reduction and internal fixation (ORIF) is necessary for fractures that have fragment displacement >3 mm, joint incongruence >2 mm, or a disrupted extensor mechanism. The aims of surgical treatment are to achieve the stable fixation of fragments, anatomical reduction of the articular surface, and early restoration of range of motion (ROM) (3, 4).
There are numerous methods for the internal fixation of patella fractures, and tension band wiring (TBW) technology is the most extensively utilized approach. Such technology contains longitudinal Kirschner wires (K-wires) inserted across the fracture and a stainless steel wires (SSW) looped in an eight-like fashion over the anterior patella. Nevertheless, various SSW-related complications have been reported, including wire fatigue failure, wire irritation, and delayed wound healing (5, 6).
Consequently, several modifications have been introduced to avoid steel wire-related complications by using strong suture materials along with other tension band suture techniques (7).
At our department, our team used a modified tension band technology for treating patella fractures with K-wires combined with 5-Ethibond. This retrospective research is intended to clinically investigate the radiographic outcomes of K-wires combined with 5-Ethibond in the therapy of patella fractures.
Materials and methods
Patient characteristics
This research was approved by the Ethical Committee of the Clinical Medical College of Yangzhou University, and every patient offered informed consent. We collected retrospective data from all patients with displaced intra-articular patella fractures between July 2018 and January 2022. Preoperative x-ray and three-dimensional computed tomography (CT) scanning images were acquired to assess patella fractures. The inclusive criteria were as follows: all patients were older than 18 years; the individual with an acute closed patella fracture featuring an articular incongruity >2 mm or a separation of fragment fracture >3 mm; the general physical condition of the patient could withstand the anesthesia and operation; and fractures without any deep infection. The exclusion criteria were individuals who were younger than 18 years, simple or nondisplaced fractures with indications for conservative treatments; patients with open fractures, periprosthetic fractures, and pathologic fractures; patients who were followed up for less than 3 months; the general physical condition of the patients could not withstand the anesthesia and operation; patients receiving revision procedures; patients with knee function limitation or other severe medical conditions before injury; and individuals with multiple concomitant injury of the ipsilateral leg or other systems. Patients were treated with TBW with K-wires and 5-Ethibond. Patients' demographic information and operational information were obtained and analyzed based on the database of our hospital.
Surgical procedures
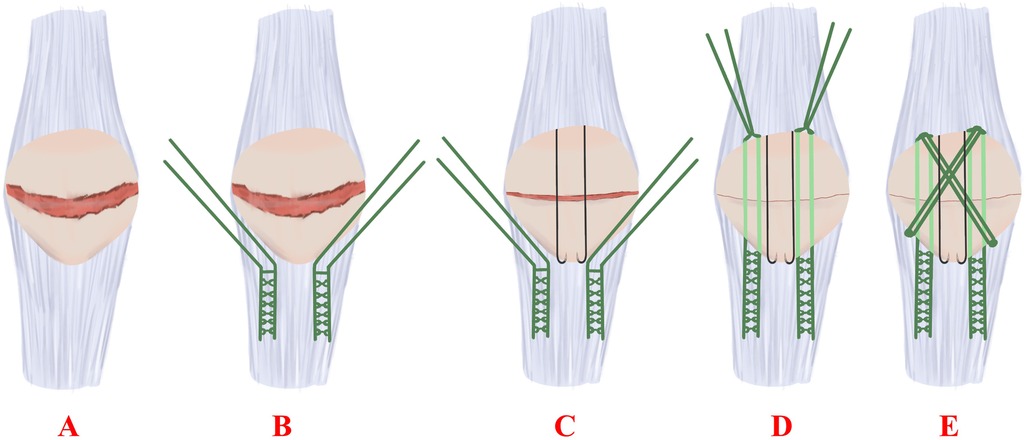
Every patient was treated with a single dosage of cefazolin (50 mg/kg, a maximal dosage of 2 g) antibiotic for antimicrobial prophylaxis within the 30-min incision. After anesthesia, the patient was put on the operation table in the dorsal position. Then, a longitudinal midline incision was made over the knee to expose the fractured site. Following that, the intra-articular hematoma and blood clots were cleaned; afterwards, a 5-Ethibond was introduced in a Krackow manner up and down the medial and lateral edges of the patellar tendon, during which two sharp reduction clamps were used to temporarily maintain reduction. The two or three 1.6-mm K-wires (Youke, Shanghai, China) were introduced in parallel by inserting them from the upper pole to the lower pole of the patella. The remaining four suture limbs passed through the patella. The sutures were afterwards tied at the superior pole with the knee in extension. The remaining 5-Ethibond was then passed through the front of the patella to form an eight-like shape (Figure 1); then, the retinaculum was repaired. During the surgery, the active knee joint displayed stable fracture, and x-ray fluoroscopic results demonstrated an excellent decrease in the fracture.
Postoperative management and evaluation
Postoperatively, x-ray examinations were completed the day after surgery. Generally, flexion in-brace (0°–90°) was allowed for 0–2 weeks postoperatively. Patients were regularly followed up every 4–6 weeks. Before the patient discharged from hospital, we told the patient that the rehabilitation plan was as follows: the knee ROM was progressively elevated, and patients exercised themselves with the objectives of realizing 90° flexion by the 28th day, 120° flexion by the 42nd day, and full ROM eventually. The demographic data of patients includes age, sex, trauma mechanisms, fracture types, and length of follow-up. Follow-up records includes fracture union time, knee joint ROM, Bostman score, and complications.
Radiographic images were analyzed to evaluate the original fracture types, displacements, implant positions, and treatment time.
Statistics
All data were described as the averages ± SD, and our statistic assay was completed via SPSS 26.0.
Results
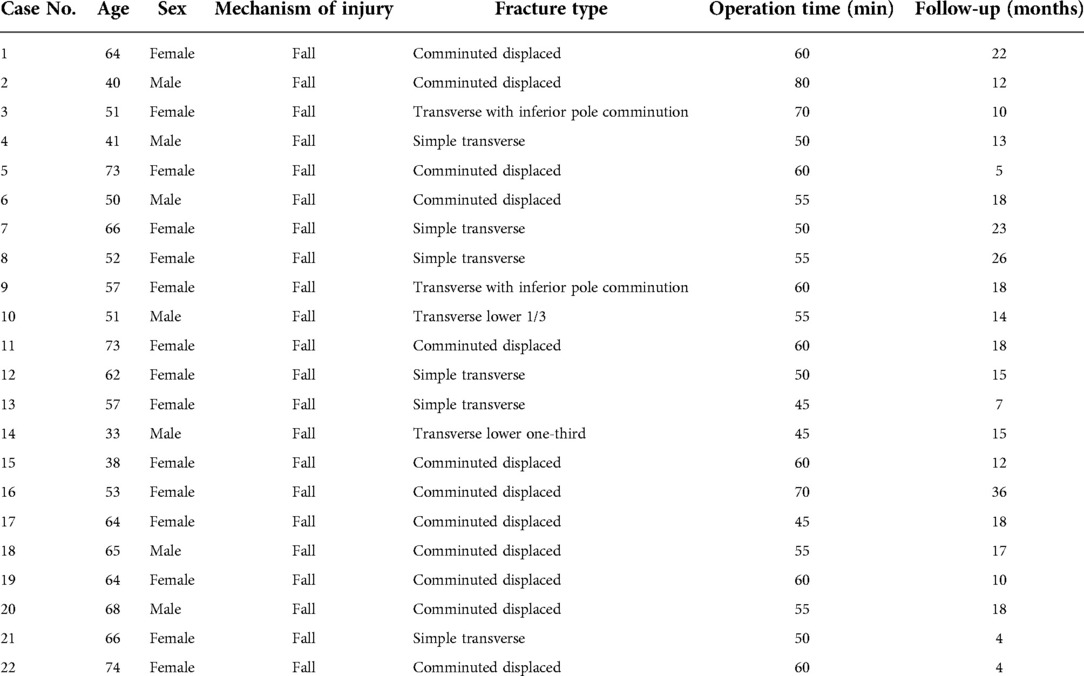
The 22 patients were enrolled in the present research (7 males and 15 females). The average age of the patients was 57.4 ± 11.9 (range 33–74) years. The mean operation time was 56.8 ± 8.7 (range 45–80) min. The mean follow-up time was 15.2 ± 7.6 (range 4–36) months. The demographic information is further demonstrated in Table 1.
All patients had bony union at an average of 10.5 ± 1.9 (range 8–14) weeks. There was no loss of reduction during follow-up. No breakage, loosening, migration, and skin irritation of the inner fixation were observed during the follow-up (Figures 2, 3). At the eventual follow-up, the mean postoperative ROM was 123.4° ± 14.6° (range 95°–140°) (Figure 4); we have not observe the K-wire slippage in all cases so far. The Bostman patella fracture function score was 28.7 ± 1.2 (range 26–30). The clinical outcomes of patients are displayed in Table 2.
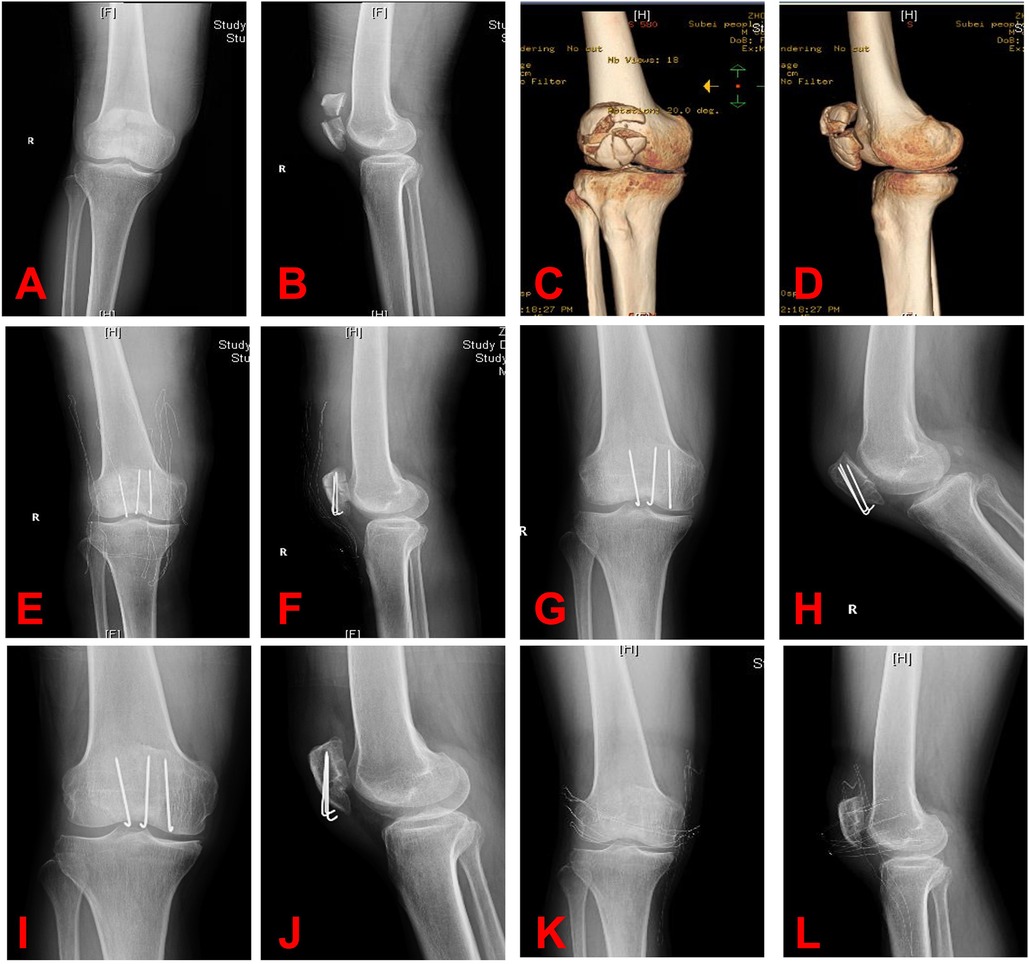
Figure 2. (A–D) Radiographs of comminuted patella fracture. (E,F) In this comminuted patella fracture, we used the 5-Ethibond and three K-wires. (G,H) After 3 months, the radiograph revealed a good union of fracture. (I,J) After 12 months, no breakage, loosening, or migration of the internal fixation was detected, and a good union of fracture was seen. (K,L) Radiograph after implant removal.
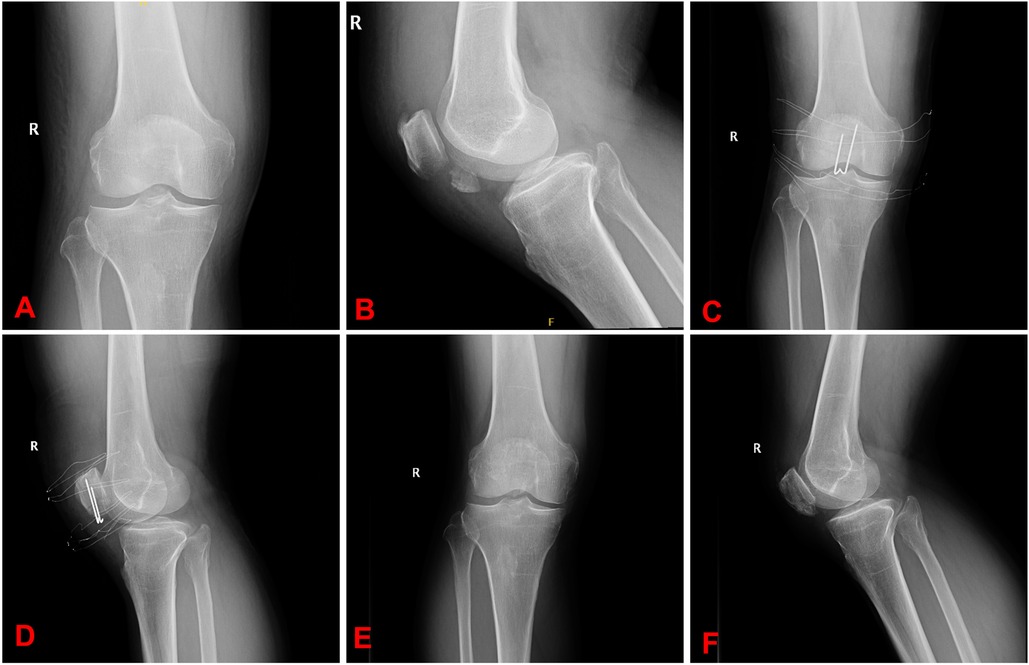
Figure 3. (A,B) Radiographs of distal patellar fracture. (C,D) In this distal patella fracture, we used the 5-Ethibond and three K-wires. (E,F) Radiograph after implant removal.
Discussion
The main aim of operative treatment is to reduce the anatomic articular surface, achieve stable patella fixation, and facilitate early knee mobilization (8). The TBW technology is the most extensively utilized surgical fixation approach to stabilize patella fractures. Traditional tension band construction uses two K-wires and a metal low-gauge wire tension band. After fracture reduction, the K-wires were introduced into the fracture fragments along the subchondral surface via insertion. Then, the stainless steel wire was placed in an eight-like fashion to realize fracture compression. Although stainless steel wires can provide stable fixation, these wires are usually associated with hardware-induced symptoms and other complications (9–11). Meena et al. discovered three probable factors that might break wires: (1) repeated stress on the wires because of a remarkable ROM of knee joints; (2) utilization of thin wires; and (3) utilization of low-quality hardware (12). As a result, it is imperative to explore sutures in the fixation techniques instead of investigating stainless steel wires.
Using sutures can deliver several advantages compared with stainless steel wires (9, 13). Harrell et al. concluded that several loops of Ethibond could replace SSWs, but such a method might not be good for the tension band fixation of fractures (14). Patel et al. compared 5-Ethibond with SSWs in the treatment of patella fractures via the adjusted tension band technology and the Lotke technology in a biomechanical study. The result revealed that the 5-Ethibond was able to withstand loads comparable to those of SSWs for patella fractures (15).
In 2001, Gosal et al. compared patellar fracture fixation based on metal wires or 5-Ethibond. They recorded a 38% hardware removal rate due to pain and hardware failures when metallic implants were utilized, and they did not record any symptoms associated with the utilization of heavy sutures. The suture fixation group, nevertheless, displayed a 6% failure rate, which indicated that the substance and approach utilized could induce fixation failures prior to the use of traditional metal implants (16). This is probably the reason why sutures are not usually suggested for treating patellar fractures. We proposed that the failures of suture fixation were due to the lack of metallic parallel longitudinal intraosseous fixation.
Hence, instead of stainless steel wires, we selected K-wires combined with 5-Ethibond to treat patella fractures in this study.
Lee et al. reported that using the adjusted tension band technology with FiberWire and retaining metal parallel implants like K-wires could achieve good results (17). No patient had broken wires, and nonunion with deformity was observed in one individual. Bryant et al. contrasted fracture fixation technologies with the anterior tension band through cannulated screws by virtue of FiberWire and SSWs. The research outcomes presented no remarkable diversity between the FiberWire group and the SSW group (18).
In our study, to obtain a better stability of fracture fixation, the remaining suture limbs were passed through the patella. Then, sutures were tied at the superior pole with the knee in extension. The remaining 5-Ethibond was then passed through the front of the patella to form a certain shape. The most important discovery of our study was that using K-wires combined with 5-Ethibond was a valid, secure, and easy therapeutic method for patella fractures. The average operation time was 56.8 minutes, which indicated that such a surgical approach might not bring additional technological challenges or tissular injuries. Hence, this method is quite prospective and can be utilized extensively. In the present research, patients received recovery training and full weight bearing training as early as the second day after surgery. Clinically and radiologically, the outcomes revealed that such technology could deliver satisfactory results for patients. No patient experienced the loss of reduction and inner fixation failures, and no patient received a remedial operation. Those outcomes coincide with previously completed research that revealed that nonabsorbable sutures could substitute for metallic wires due to their strength. Hence, the 5-Ethibond can offer similar protective effects as steel wires in antagonizing displacements and improving strength in knee extensor loading.
We believe that the adjusted tension band techniques based on 5-Ethibond are simple and can decrease irritation and the quantity of broken wires. Moreover, these methods may be more valid in contrast to the single use of nonabsorbable polyester due to the probability of early recovery and better life quality.
Nevertheless, there are certain flaws in the present research. First, our study was finished retrospectively. Second, the number patients was insufficient. Third, our team did not complete the biomechanical analysis of our construct to evaluate its biomechanical strength. Fourth, during the research, many patients, even asymptomatic patients, wished to remove implants owing to culture-related reasons. Hence, more high-quality, double-blinded randomized clinical trials with larger sample sizes are warranted to substantiate the benefits of fixation using K-wires combined with 5-Ethibond.
Conclusions
Patella fracture patients treated with K-wires combined with 5-Ethibond presented favorable clinical outcomes. This technique may be a valid fixation approach for healing displaced and comminuted patella fractures.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Northern JiangSu People's Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
YL, JHu, JW, and PC performed the surgery. PZ, JZ, and LY contributed significantly to analysis and manuscript preparation. WZ, JC, JHe, YF, and YZ performed the data analyses. YL and JHu wrote the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Zhan Y, Zhang Y, Xie X, Luo C. Three-dimensional fracture mapping of multi-fragmentary patella fractures (AO/OTA 34C3). Ann Transl Med. (2021) 9(17):1364. doi: 10.21037/atm-21-1814
2. Kumar S, Mittal S, Manhas V, Sharma V. Functional and radiological outcomes following plating for displaced fractures of patella: a pilot study. Injury. (2022) 53(2):691–7. doi: 10.1016/j.injury.2021.11.053
3. Carpenter JE, Kasman R, Matthews LS. Fractures of the patella. Instr Course Lect. (1994) 43:97–108.9097140
4. Adjal J, Ban I. Patella fractures treated with suture tension band fixation. J Orthop Surg Res. (2021) 16(1):179. doi: 10.1186/s13018-021-02309-5
5. Ma XY, Liu B, Zhou DP, Xiang LB. Treatment for transverse patella fractures with minimally invasive techniques (review). Exp Ther Med. (2022) 23(3):192. doi: 10.3892/etm.2022.11115
6. Brusalis CM, Gruskay JA, Bornes TD, Langhans MT, Ricci WM. Open reduction and internal fixation of patella fracture with contoured dorsal plating. J Orthop Trauma. (2021) 35(Suppl 2):S34–5. doi: 10.1097/BOT.0000000000002171
7. Hughes SC, Stott PM, Hearnden AJ, Ripley LG. A new and effective tension-band braided polyester suture technique for transverse patellar fracture fixation. Injury. (2007) 38(2):212–22. doi: 10.1016/j.injury.2006.07.013
8. Yao SH, Lin SF, Lin CH, Chen CH. Loop anchor tension band technique for patella fractures lowers the rate of Kirschner migration. Injury. (2021) 52(6):1556–62. doi: 10.1016/j.injury.2020.11.057
9. Jirangkul P, Kosiyatrakul A. Abstaining from symptomatic implants of modified tension band wiring by nonabsorbable suture fixation for transverse patella fractures. J Orthop Surg Res. (2021) 16(1):367. doi: 10.1186/s13018-021-02494-3
10. Huang PH, Hsu CH, Hsu SL, Liu HC. Treatment of displaced fractures of the patella: tension band wiring technique with the one-end or both-ends K-wire bending fixation method. J Orthop Surg (Hong Kong). (2021) 29(1):2309499020988179. doi: 10.1177/2309499020988179
11. Yao C, Sun J, Wu J, Zhou Z, Liu F, Tao R, et al. Clinical outcomes of Ti-Ni shape-memory patella concentrator combined with cannulated compression screws in the treatment of C2 and C3 patella fracture: a retrospective study of 54 cases. BMC Musculoskelet Disord. (2020) 21(1):506. doi: 10.1186/s12891-020-03536-3
12. Meena S, Nag HL, Kumar S, Barwar N, Mittal S, Singla A. Delayed migration of K-wire into popliteal fossa used for tension band wiring of patellar fracture. Chin J Traumatol. (2013) 16(3):186–8. doi: 10.3760/cma.j.issn.1008-1275.2013.03.012
13. Chatakondu SC, Abhaykumar S, Elliott DS. The use of non-absorbable suture in the fixation of patellar fractures: a preliminary report. Injury. (1998) 29(1):23–7. doi: 10.1016/S0020-1383(97)00114-9
14. Harrell RM, Tong J, Weinhold PS, Dahners LE. Comparison of the mechanical properties of different tension band materials and suture techniques. J Orthop Trauma. (2003) 17(2):119–22. doi: 10.1097/00005131-200302000-00007
15. Patel VR, Parks BG, Wang Y, Ebert FR, Jinnah RH. Fixation of patella fractures with braided polyester suture: a biomechanical study. Injury. (2000) 31(1):1–6. doi: 10.1016/S0020-1383(99)00190-4
16. Gosal HS, Singh P, Field RE. Clinical experience of patellar fracture fixation using metal wire or non-absorbable polyester–a study of 37 cases. Injury. (2001) 32(2):129–35. doi: 10.1016/S0020-1383(00)00170-4
17. Lee BJ, Chon J, Yoon JY, Jung D. Modified tension band wiring using FiberWire for patellar fractures. Clin Orthop Surg. (2019) 11(2):244–8. doi: 10.4055/cios.2019.11.2.244
Keywords: patella fracture, suture, tension band, Kirschner wire, 5-Ethibond
Citation: Liang Y, Hu J, Zhang P, Zhang J, Yang L, Zhang W, Chen J, He J, Fang Y, Zhou Y, Chen P and Wang J (2023) Clinical application of Kirschner wires combined with 5-Ethibond fixation for patella fractures. Front. Surg. 9:968535. doi: 10.3389/fsurg.2022.968535
Received: 14 June 2022; Accepted: 25 November 2022;
Published: 6 January 2023.
Edited by:
Paphon Sa-ngasoongsong, Mahidol University, Thailand© 2023 Liang, Hu, Zhang, Zhang, Yang, Zhang, Chen, He, Fang, Zhou, Chen and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Pengtao Chen MTgwNTEwNjE1MTZAMTYzLmNvbQ== Jingcheng Wang d2FuZ2pjeWFuZ3pob3VAMTYzLmNvbQ==
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Yuan Liang†
Yuan Liang† Jingcheng Wang
Jingcheng Wang