- Gynecological Plastic Surgery Department, Plastic Surgery Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
Purpose: To investigate the shape of labia minora in Chinese adult women.
Methods: Women who visited the Genital Plastic Surgery Center from January 2021 to February 2022 were included and the vulvar regions were photographed. The shape of the labia minora was converted into quantifiable values [left side line segment 1–9 (L1–L9 values) and right side line segment 1–9 (R1–R9 values)]. The 400 enrolled patients were grouped by age, parity, and the types of vulvar surgeries they planned to undergo.
Results: After a graphic-to-digital and digital-to-graphic conversion, the simulated average image of the labia minora in Chinese adult women was constructed based on the mean values of L1–L9 and R1–R9. Comparing the values of Ln and Rn in the four age groups revealed that the mean values of Ln and Rn gradually decreased with age, but only two subgroups showed statistically significant differences (P-value <0.05). When the patients were stratified according to the number of births and whether labiaplasty was planned to perform, there were no significant differences among all groups (P-value >0.05).
Conclusion: To measure and evaluate the labia minora, a new assessing method was used. It is an innovative attempt to transform the simple rough description of the shape of the labia minora into more precise data reflecting the shape features. It allows the comparison of labia minora shape between individuals by comparing quantifiable values. Besides, the average shape of labia minora in Chinese adult women was provided visually. Factors including age, parity, and whether the patient planned to undergo labiaplasty were not significantly associated with the shape of the labia minora.
Introduction
The popularity of female genital plastic surgery is gradually rising, and so is labiaplasty (1). Enlarged labia minora could cause functional, cosmetic, and psychosocial issues (2). In 1984, the first article describing labiaplasty was published and edge trim techniques were used for three patients who felt the protrusion of the labia minora was aesthetically and functionally unsatisfactory (3). Indeed, the length, width, and color of the labia minora can vary widely. The first study regarding genital dimensions in healthy women was published by Lloyd et al. in 2005 (4). When the transverse distance from the interlabial groove to the widest part of the labia minora is greater than 40–50 mm, it could be diagnosed as labia minora hypertrophy (5). Many plastic surgeons have previously measured and described the female vulva and defined the hypertrophic labia minora (5–8). Nevertheless, there is currently no standard for an aesthetically perfect labia minora (9). Culturally projected interpretation biases toward one's genital appearance could cause concerns compelling patients to seek female genital plastic surgeries (10). The general shape of the labia minora has a far-reaching impact on the patient's willingness to undergo labiaplasty and choices of surgical strategies. Female genital parameters have been surveyed in the United Kingdom, China, the United States, Denmark, India, Australia, Israel, etc. (4, 9, 11–15).
Although plastic surgeons and gynecologists have taken measurements of the labia minora, such as the labial length and labial width (16). No scholars have quantitatively analyzed the morphological characteristics of the labia minora. This study is the first morphological study of the labia minora in a large cohort. To provide a better understanding of the morphological features of the labia minora, we present a descriptive study addressing labia minora measurement. Herein, the shape of the labia minora was converted to numerical values for an in-depth comparative analysis of 400 Chinese adult women.
Methods
Patients
Women who visited the Genital Plastic Surgery Center with various surgical intentions were consecutively included in the study. Patients were excluded if they had a history of vulvar surgeries before they visited the Genital Plastic Surgery Center because the labia minora may no longer be in its primitive, non-interventionist state. A total of 400 female patients were included in chronological order. Data were collected on age, the number of births, and surgical information (Supplementary File 4). The included consecutive patients underwent surgeries in the vulvar region in the Genital Plastic Surgery Center between January 2021 and February 2022 and the measurements of the labia minora were all scheduled before surgery. Left side labiaplasty was performed on 21 patients, right side labiaplasty was performed on 28 patients, bilateral labiaplasty was performed on 173 patients, clitoral hood reduction was performed on 185 patients, vaginal tightening surgical procedure was performed on 122 patients, labia majora augmentation was performed on 29 patients, hymen repair was performed on 60 patients, and other procedures in the vulva area such as the excision of pigmented nevus and masses were performed on 22 patients (Supplementary File 4). Labiaplasty included 149 cases of trim labiaplasty and 73 cases of wedge labiaplasty. The vaginal tightening procedures mentioned above refer to the excision of redundant vaginal tissues, the imbrication of the median levator muscles, and the remodeling of the perineal body.
This study was approved by the appropriate institutional research ethics committee. Photographs were obtained with written informed consent, and all data were analyzed anonymously according to the principles in the Declaration of Helsinki 1975 (revised in 2008).
Measurements and statistical analysis
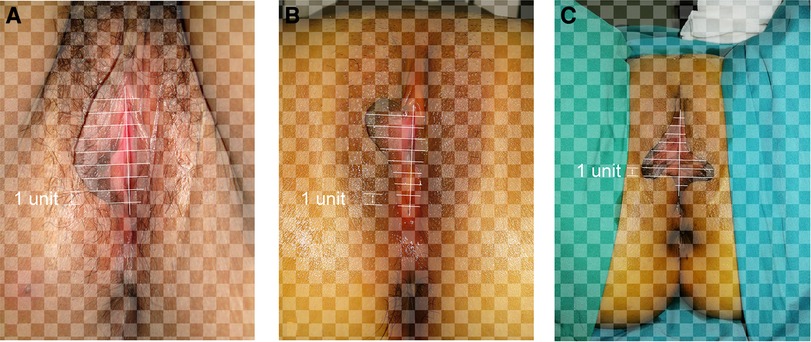
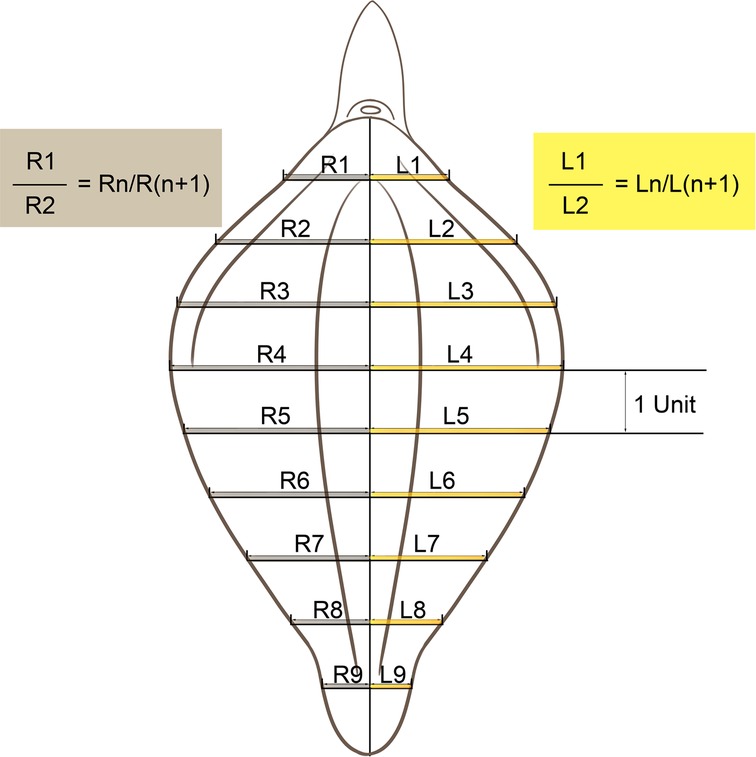
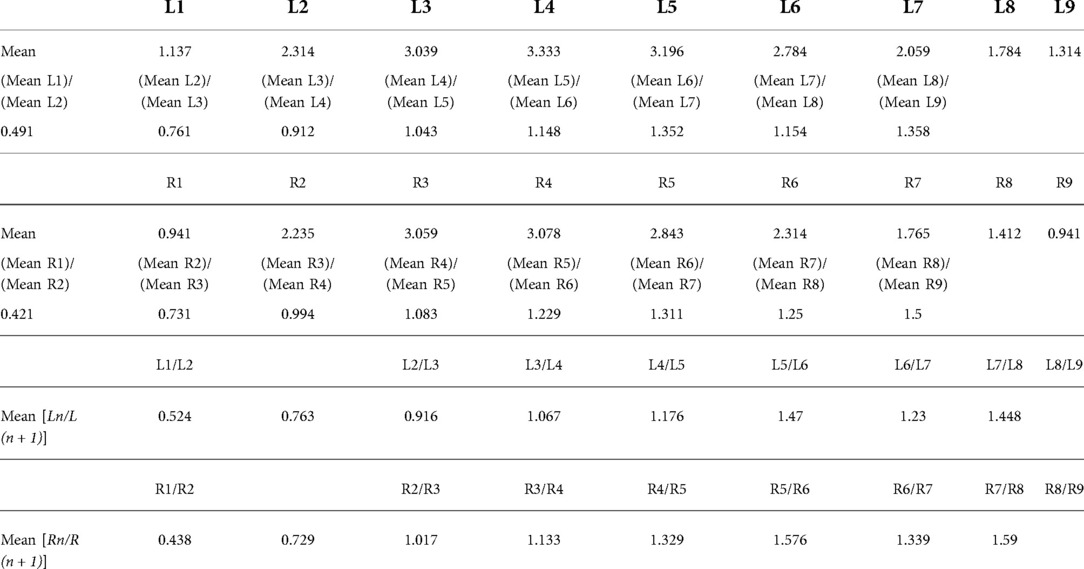
Photographs of the 400 patients were reviewed retrospectively. The labia minora were naturally tiled laterally without traction when photographed. The longitudinal axis of the vaginal vestibule was marked into ten equal segments using Adobe Photoshop software. The length of one segment was set as one unit for measurement and plumb lines were made respectively (Figures 1–3). The well-marked photographs of the labia minora were then measured using ImageJ software. The vertical dimensions between the contour line of the labia minora and the longitudinal axis of the vaginal vestibule were calculated. The measured segments of the left side were named Ln (n = 1–9) and the measured segments of the right side were named Rn (n = 1–9) (Figure 4). In general, L1–L9 represents a series of adjacent line segments on the left and R1–R9 represents a series of adjacent line segments on the right (Figure 4). Moreover, the ratio between adjacent line segments was calculated. L1/L2, L2/L3, L3/L4, L4/L5, L5/L6, L7/L8, and L8/L9 were abbreviated as Ln/L(n + 1) (Figure 4). The same applied to Rn/R(n + 1). The simulated graph of the average shape of the labia minora for adult Chinese women was constructed based on the mean values of Ln and Rn (Figure 5). Levene's test for equality of variances was performed before making comparisons between groups. Statistical significance was defined as P-value <0.05 (Supplementary Files 1–3).
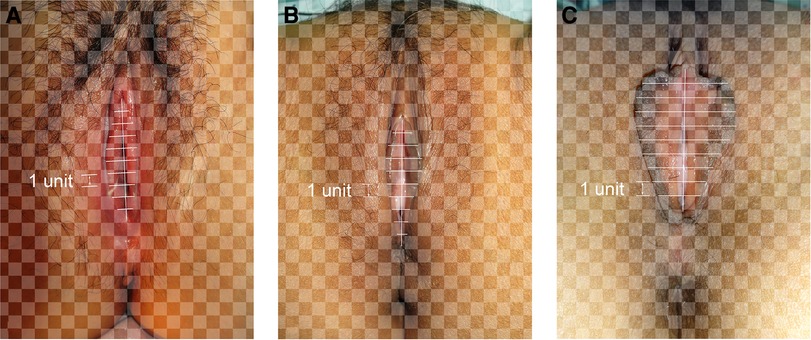
Figure 1. (A) “Small type” labia minora; (B) “willow leaf type” labia minora; (C) “butterfly wing type” labia minora.
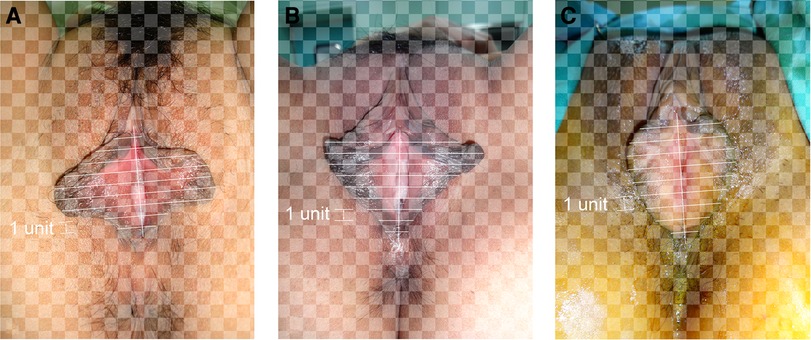
Figure 2. (A) “Protruding type” labia minora; (B) “rhombus type” labia minora; (C) “fan-shaped type” labia minora.
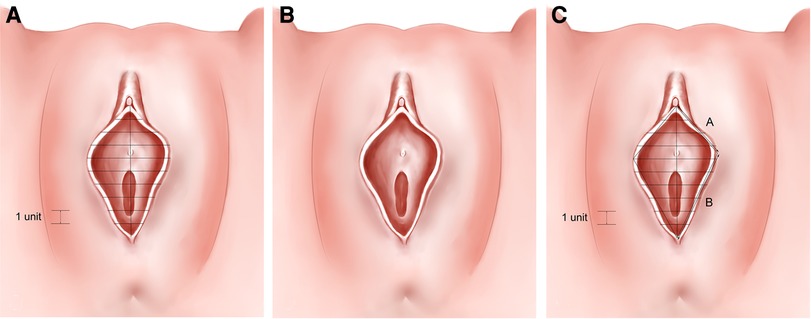
Figure 5. (A–C) Simulation of the average shape of labia minora in 400 patients (based on the mean values of L1–L9 and R1–R9).
Results
Measurements of L1–L9 and R1–R9
The photographic measurement method used on various types of labia minora was shown in Figures 1–3. The maximum values among L1–L9 and R1–R9 in 137 patients (34.25%) fell into the range of L1–L3 or R1–R3. For these patients, the prominent portions of the labia minora were the anterior parts. The maximum values of 187 patients (46.75%) fell into the range of L4–L6 or R4–R6, and the prominent parts were the middle part of the labia minora. 76 patients (19%) had maximum values in the range of L7–L9 or R7–R9. Thus, the anteriorly and medially protruding labia minora were more common than the posteriorly protruding labia minora. Based on the mean values of L1–L9 and R1–R9 in the 400 patients (Table 1), the average shape of the labia minora was constructed (Figure 5). The ratio of the posterior labial distance and the anterior labial distance was 1.498 (7.183/4.794) on the left side and 1.335 (6.942/5.200) on the right side. The former one was closer to the golden ratio (1.618:1).
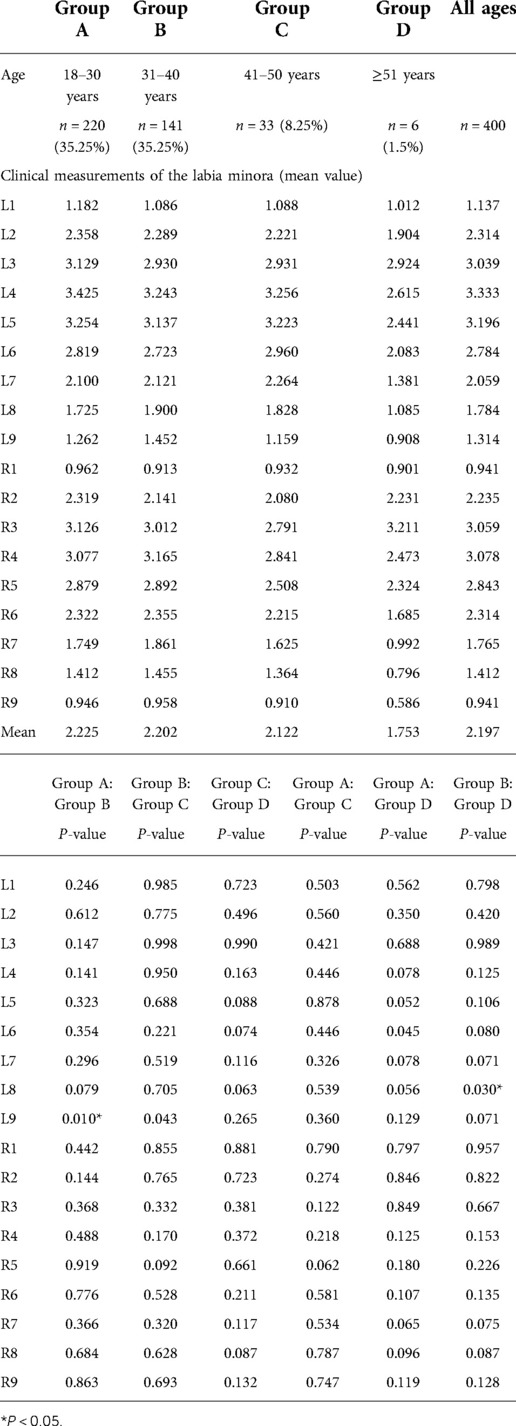
Association between the shape of labia minora and age
The average age of the included patients was 30.53 years, ranging from 18 to 70 years (Supplementary File 4). The 18–30 years was the main subgroup (Group A, n = 220, 55%), while others included the 31–40 years (Group B, n = 141, 35.25%), 41–50 years (Group C, n = 33, 8.25%), and ≥51 years (Group D, n = 6, 1.5%) (Table 2). Comparing the mean values of Ln and Rn in the four age groups revealed that the mean values gradually decreased with age. Independent-samples t-test was performed independently among groups from L1 to L9 (Supplementary File 1). Most groups showed no statistically significant differences (P-value >0.05), except for two subgroups [Group A (L9): Group B (L9), P-value = 0.010; Group B (L8): Group D (L8), P-value = 0.030, as shown in Table 2).
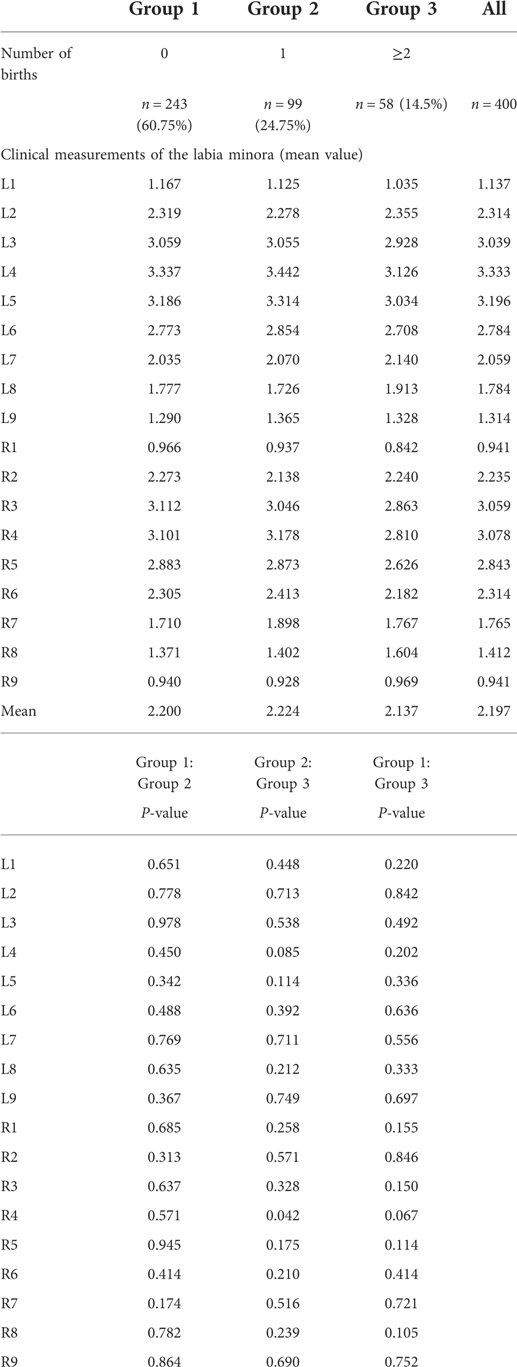
Association between the shape of labia minora and the number of births
The average number of births of the included patients was 0.55. Patients were divided into three groups, including nulliparous women (Group 1, n = 243, 60.75%), primiparous women (Group 2, n = 99, 24.75%), and multiparous women (Group 3, n = 58, 14.5%) (Table 3). Based on the mean values of Ln and Rn for Group 1 to Group 3, the measured values of the labia minora in Group 2 (primiparous women) were the largest, followed by Group 1 (nulliparous women) and Group 3 (multiparous women) (Table 3). Independent sample t-tests were also performed for each group (Supplementary File 2).
Group 1, Group 2, and Group 3 did not differ statistically significantly (P-value >0.05, Table 3). The detailed statistical data and independent samples t-test were shown in Supplementary File 2.
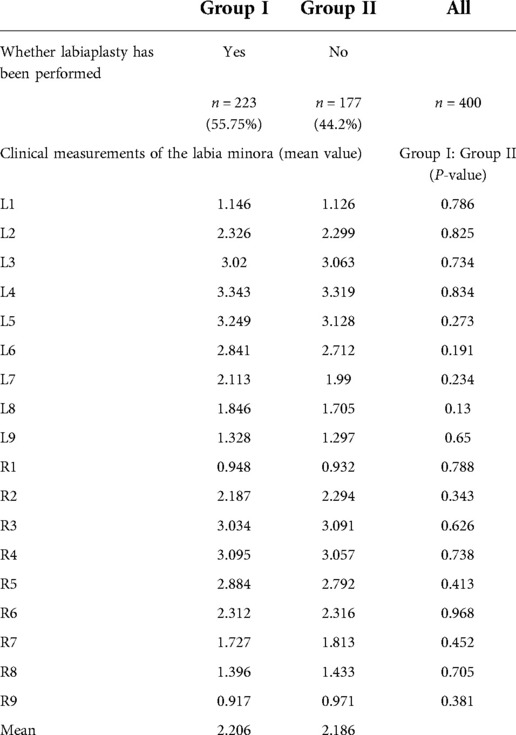
Association between the shape of the labia minora and procedures going to perform
The procedures performed in 223 patients (Group I, 55.75%) included unilateral or bilateral labiaplasty. A total of 177 patients (Group II, 44.2%) did not undergo labiaplasty (Supplementary File 4). Data from Group I and Group II were also compared (Supplementary File 3). Although the values and means of Ln and Rn were different in the two groups, there were no statistical differences (P-value >0.05, Table 4).
Discussion
The purpose of the study is to investigate the morphological features of the labia minora in adult women who had never had genital surgery before the vulvar measurement. After a graphic-to-digital and digital-to-graphic conversion, the average shape of the 400 included patients was constructed (Figure 5). Meanwhile, data were further analyzed to explore the association between the labia minora morphology and factors such as age, parity, and whether they planned to have labia minora surgery.
Female genital cosmetic surgery, particularly labiaplasty, is gaining in popularity (17). However, there has been no unified “aesthetic gold standard” for the shape of the labia minora to date. It is thought that the aesthetics of the female vulva is not determined by one or two structures but by the vulvar region as a whole. Therefore, an aesthetically pleasing labia minora must coordinate with adjacent structures (18). Most previous studies on the size of the labia minora have focused only on the width and length of the labia minora (8, 13, 18, 19). In this study, the shape characteristics of the labia minora were converted into measurable values which can be used for comparative analysis. The values of Ln, Rn, Ln/L(n + 1), and Rn/R(N + 1) reflected the contour of the labia minora and the labia minora characteristics.
The shape features of the labia minora in Chinese adult women could provide a useful supplement to the field of female genital plastic surgery. Simplifying the contours of a body part or organ into geometric figures is a common method for biomorphology (20, 21). In this study, the method used to measure labia minora draws on this strategy. The unit length was set as one-tenth of the longitudinal length of the vaginal vestibule in each patient, making it feasible to compare the shape of the labia minora between patients. The larger the Ln and Rn values, the wider the shape of the labia minora. In contrast, the smaller the Ln and Rn values, the thinner the shape of the labia minora. L1/L2, L2/L3, L3/L4, L4/L5, L5/L6, L7/L8, and L8/L9 represent the trend in the distance between the left labia minora edge and the median axis. Same for Rn/R(n + 1). When Ln/L(n + 1) or Rn/R(n + 1) value is 1, it means that the two adjacent line segments are equal. When Ln/L(n + 1) and Rn/R(n + 1) are greater than 1, the larger the value, the larger the gap between adjacent line segments. On the contrary, when the ratio is less than 1, the smaller the value, the larger the gap between adjacent line segments. Overall, Ln/L(n + 1) and Rn/R(n + 1) determined the protrusion degree of the labia minora when observing the vulva as a whole (Table 1). The average shape of the labia minora in the 400 included patients was constructed based on the mean values of L1–L9 and R1–R9 (Figure 5; Table 1). To some extent, it could represent the general shape of the labia minora in Chinese adult females. The simulated outline of the labia minora was close to a “butterfly wing shape” (Figure 5).
The golden rule is widely used in plastic surgery as a generally accepted aesthetic standard. The labia minora could also refer to the golden ratio to achieve visual beauty (22). For aesthetically pleasing labia minora, there is a golden ratio (1:1.618) between the anterior and posterior labial distances of the labia minora (23). In the present study, the ratio of the posterior labial distance (Line B) and the anterior labial distance (Line A) was 1.498 (7.183/4.794) on the left side and 1.335 (6.942/5.200) on the right side (Figure 5), with the ratio of left labia minora closer to the golden ratio.
The labia minora seemed to acquire a thinner shape with increasing age (Table 2). Nevertheless, no significant differences were found between most age groups when Ln and Rn values were compared, except for two subgroups (Table 2). As a result, it appears that there was no significant relationship between age and labia minora measurements, consistent with previous studies. For instance, Lloyd et al. reported no significant associations between the size of labia minora and age, parity, hormone use, or sexual history (4). In terms of parity, primiparous women (Group 2) had the largest Ln and Rn values (Table 3), implying that the labia minora seemed to be wider for this patient group. In comparison, the smallest value corresponded to Group 3 (number of births ≥2), which means that for females with two and more births, their labia minora appeared to be thinner (Table 3). However, the difference in mean values between the three groups was quite small, and no significant differences were found (P-value >0.05) (Supplementary File 2, Table 3). Patients who planned to undergo labiaplasty usually have a strong subjective desire since labiaplasty is a cosmetic procedure (24, 25). It was mentioned in certain studies that the size of the labia minora was associated with patients’ subjective perception (12, 14, 26). In this study, the association between whether labiaplasty was performed and the shape characteristics of the labia minora was also analyzed (Supplementary File 3). For patients who underwent unilateral or bilateral labia minora surgery, the values of Ln and Rn were larger (Table 4). Their labia minora appeared to be wider and more prominent than patients who did not undergo labiaplasty. However, all P-values were greater than 0.05 and there was no significant difference between Group I and Group II (Table 4). It seems to contradict other previous studies (12, 14, 26). While the exact cause is not known, we speculate that this may be due to uneven grouping and a small sample size in a single medical center. Moreover, the labia minora surgery is not only determined by the shape of the labia minora but also the associated physical symptoms and the patient's wishes. There are many patients seeking labiaplasty who have no physical symptoms, such as hygiene problems, tugging during intercourse, uncomfortable wearing tight clothing, pain during intercourse, erosions, etc. (1, 2, 27). They seek labiaplasty to achieve their “ideal labia minora”. Therefore, patients scheduled for labiaplasty may not have more hypertrophied labia minora than those who were not going to have labiaplasty.
The vaginal vestibule, as an inseparable structure from the labia minora, refers to the area between the two sides of the labia minora (11). The aesthetics of the labia minora is not only associated with the specific value of the width of the labia minora (28). Even if two patients have the same labia minora width, if their vaginal vestibule lengths differ, the shape and aesthetics of the labia minora will also differ. The labia minora and the adjacent vestibule should therefore be regarded as a whole (19, 29). Various factors such as weight and height may affect measurements of labia minora, so a direct comparison of the labia minora width could be uncomprehensive (15, 30, 31). The measurement strategy in the study is helpful to reveal the overall shape features. To our knowledge, no previous studies have quantified the shape features of the labia minora. Related studies usually focused on subjective perceptions, measurements of local structure, and rough generalizations. Herein, we further grouped and analyzed 400 patients at three levels (age, parity, and whether the labiaplasty going to perform). Independent samples t-tests were performed to explore whether the differences between the groups were significant.
Currently available classifications for labia protrusion are based on the distance between the lateral edge of the labia minora and the labia majora, or the distance between the base of the labia minora and the distalmost tip (19). Our finding could help plastic surgeons gain a direct visual cognition and understanding of the labia minora in Chinese adult women. It would be helpful to provide more guidance to plastic surgeons. Even if two patients have the same labia minora width, if the shape of the labia minora differs, the aesthetics of the labia minora and patients’ perceptions will also differ. We believe that the study based on quantifiable data and analysis is important for the further exploration of labia minora morphology.
Despite the fact that the study was only based on retrospective photographs, the combination of in-depth data analysis by image processing software gives this study an advantage over other studies. Although the photographs were not taken from the same distance all the time, the relative sizes of each part of the labia minora were not affected when calculating the values of Ln, Rn, Rn/R(n + 1), and Ln/L(n + 1). Another shortcoming of the study is that although we included patients with different clinical characteristics and surgical plans, bias due to population selection still exists. Since patients were obtained from a single center, the data presented here might be limited and caution is warranted when interpreting our findings. In the future, to correlate morphologic characteristics with surgical outcomes, clinical applications may be required to establish its utility. More large-scale studies from multi-centers are required to further validate our results. New criteria and references for labial morphology may develop subsequently.
Conclusion
The average shape of labia minora in 400 Chinese adult women could provide a visual reference to plastic surgeons. The shape of labia minora was not significantly associated with age, parity, or whether or not the patient was going to undergo labiaplasty. The shape characteristics of the labia minora were converted into numerical values and a new method was provided for measuring and evaluating the shape of the labia minora. Collectively, our findings could be useful for a better understanding of the morphology of labia minora.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Plastic Surgery Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
KC: study design, data analysis and manuscript creation. KW: data collection. YY: data collection. FL: manuscript editing. QL: study design, data analysis, manuscript editing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.961247/full#supplementary-material.
References
1. Gulia C, Zangari A, Briganti V, Bateni ZH, Porrello A, Piergentili R. Labia minora hypertrophy: causes, impact on women's health, and treatment options. Int Urogynecol J. (2017) 28(10):1453–61. doi: 10.1007/s00192-016-3253-8
2. Sorice SC, Li AY, Canales FL, Furnas HJ. Why women request labiaplasty. Plast Reconstr Surg. (2017) 139(4):856–63. doi: 10.1097/PRS.0000000000003181
3. Hodgkinson DJ, Hait G. Aesthetic vaginal labioplasty. Plast Reconstr Surg. (1984) 74(3):414–6. doi: 10.1097/00006534-198409000-00015
4. Lloyd J, Crouch NS, Minto CL, Liao LM, Creighton SM. Female genital appearance: “normality” unfolds. BJOG. (2005) 112(5):643–6. doi: 10.1111/j.1471-0528.2004.00517.x
5. Hamori CA. Aesthetic surgery of the female genitalia: labiaplasty and beyond. Plast Reconstr Surg. (2014) 134(4):661–73. doi: 10.1097/PRS.0000000000000516
7. Pardo J, Solà V, Ricci P, Guilloff E. Laser labioplasty of labia minora. Int J Gynaecol Obstet. (2006) 93(1):38–43. doi: 10.1016/j.ijgo.2006.01.002
8. Chang P, Salisbury MA, Narsete T, Buckspan R, Derrick D, Ersek RA. Vaginal labiaplasty: defense of the simple “clip and snip” and a new classification system. Aesthetic Plast Surg. (2013) 37(5):887–91. doi: 10.1007/s00266-013-0150-0
9. Chalmers DJ, O'Donnell CI, Casperson KJ, Berngard SC, Hou AH, Nuss GR, et al. Normal anatomic relationships in prepubescent female external genitalia. J Pediatr Urol. (2014) 10(6):1117–21. doi: 10.1016/j.jpurol.2014.04.011
10. Goodman M, Fashler S, Miklos JR, Moore RD, Brotto LA. The sexual, psychological, and body image health of women undergoing elective vulvovaginal plastic/cosmetic procedures: a pilot study. Am J Cosmet Surg. (2011) 28(4):219–26. doi: 10.1177/074880681102800404
11. Cao Y, Li Q, Zhou C, Li F, Li S, Zhou Y. Measurements of female genital appearance in Chinese adults seeking genital cosmetic surgery: a preliminary report from a gynecological center. Int Urogynecol J. (2015) 26(5):729–35. doi: 10.1007/s00192-014-2584-6
12. Lykkebo AW, Drue HC, Lam JUH, Guldberg R. The size of labia minora and perception of genital appearance: a cross-sectional study. J Low Genit Tract Dis. (2017) 21(3):198–203. doi: 10.1097/LGT.0000000000000308
13. Agrawal N, Singh P, Ghuman NK, Sharma C, Yadav G, Gothwal M, et al. The anatomical measurements of vulva in Indian women: a cross-sectional prospective study. Int J Gynaecol Obstet. (2022) 158(1):153–61. doi: 10.1002/ijgo.13936
14. Widschwendter A, Riedl D, Freidhager K, Abdel Azim S, Jerabek-klestil S, D'Costa E, et al. Perception of labial size and objective measurements-is there a correlation? A cross-sectional study in a cohort not seeking labiaplasty. J Sex Med. (2020) 17(3):461–9. doi: 10.1016/j.jsxm.2019.11.272
15. Krissi H, Ben-Shitrit G, Aviram A, Weintraub AY, From A, Wiznitzer A, et al. Anatomical diversity of the female external genitalia and its association to sexual function. Eur J Obstet Gynecol Reprod Biol. (2016) 196:44–7. doi: 10.1016/j.ejogrb.2015.11.016
16. Jackson LA, Hare AM, Carrick KS, Ramirez DMO, Hamner JJ, Corton MM. Anatomy, histology, and nerve density of clitoris and associated structures: clinical applications to vulvar surgery. Am J Obstet Gynecol. (2019) 221(5):519.e511–e519. doi: 10.1016/j.ajog.2019.06.048
17. Eserdağ S, Anğın AD. Surgical technique and outcomes of inverted-Y plasty procedure in clitoral hoodoplasty operations. J Minim Invasive Gynecol. (2021) 28(9):1595–602. doi: 10.1016/j.jmig.2021.01.015
18. Xia Z, Liu CY, Zhang M, Zhang Y, Guan A, Li Y, et al. Fused lateral clitoral hood and labia minora: new classification based on anatomic variation of the clitoral hood-labia minora complex (CLC) and simple surgical management. Aesthet Surg J. (2022) 42(8):907–17. doi: 10.1093/asj/sjac039
19. Motakef S, Rodriguez-Feliz J, Chung MT, Ingargiola MJ, Wong VW, Patel A. Vaginal labiaplasty: current practices and a simplified classification system for labial protrusion. Plast Reconstr Surg. (2015) 135(3):774–88. doi: 10.1097/PRS.0000000000001000
20. Rutland JW, Bellaire CP, Yao A, Arrighi-Allisan A, Napoli JG, Delman BN, et al. The expanding role of geometric morphometrics in craniofacial surgery. J Craniofac Surg. (2021) 32(3):1104–9. doi: 10.1097/SCS.0000000000007362
21. Lorenz C, Almeida F, Almeida-Lopes F, Louise C, Pereira SN, Petersen V, et al. Geometric morphometrics in mosquitoes: what has been measured? Infect Genet Evol. (2017) 54:205–15. doi: 10.1016/j.meegid.2017.06.029
22. Hayes JA, Temple-Smith MJ. What is the anatomical basis of labiaplasty? A review of normative datasets for female genital anatomy. Aust N Z J Obstet Gynaecol. (2021) 61(3):331–8. doi: 10.1111/ajo.13298
23. Qiang S, Li FY, Zhou Y, Li Q. Golden section in vulva. Plast Reconstr Surg Glob Open. (2020) 8(5):e2844. doi: 10.1097/GOX.0000000000002844
24. Skoda K, Oswald FE, Shorter L, Pedersen CL. Perceptions of female genitalia following labiaplasty. J Sex Res. (2021) 58(7):943–50. doi: 10.1080/00224499.2020.1808563
25. Bizjak-Ogrinc U, Senčar S. Sutureless laser labiaplasty of labia minora. Sex Med. (2021) 9(5):100406. doi: 10.1016/j.esxm.2021.100406
26. Kreklau A, Vâz I, Oehme F, Strub F, Brechbühl R, Christmann C, et al. Measurements of a ‘Normal vulva’ in women aged 15-84: a cross-sectional prospective single-centre study. BJOG. (2018) 125(13):1656–61. doi: 10.1111/1471-0528.15387
27. Sorice-Virk S, Li AY, Canales FL, Furnas HJ. Comparison of patient symptomatology before and after labiaplasty. Plast Reconstr Surg. (2020) 146(3):526–36. doi: 10.1097/PRS.0000000000007081
28. Hunter JG. Labia minora, labia majora, and clitoral hood alteration: experience-based recommendations. Aesthet Surg J. (2016) 36(1):71–9. doi: 10.1093/asj/sjv092
29. Clerico C, Lari A, Mojallal A, Boucher F. Anatomy and aesthetics of the labia minora: the ideal vulva? Aesthetic Plast Surg. (2017) 41(3):714–9. doi: 10.1007/s00266-017-0831-1
30. Brodie K, Alaniz V, Buyers E, Caldwell B, Grantham E, Sheeder J, et al. A study of adolescent female genitalia: what is normal? J Pediatr Adolesc Gynecol. (2019) 32(1):27–31. doi: 10.1016/j.jpag.2018.09.007
Keywords: labia minora, morphology, shape features, labiaplasty, vulva
Citation: Che K, Wang K, Yuan Y, Li F and Li Q (2022) Quantitative analysis of the labia minora morphology in 400 Chinese women: A new method for assessing the shape of the labia minora. Front. Surg. 9:961247. doi: 10.3389/fsurg.2022.961247
Received: 4 June 2022; Accepted: 2 November 2022;
Published: 28 November 2022.
Edited by:
Jan A. Plock, Aarau Cantonal Hospital, SwitzerlandReviewed by:
Andrea Giannini, University of Pisa, ItalyBorko Stojanovic, University of Belgrade, Serbia
© 2022 Che, Wang, Yuan, Li and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qiang Li bGlxaWFuZ3B1bWNAMTYzLmNvbQ==
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
 Kexin Che
Kexin Che Keke Wang
Keke Wang