
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 01 November 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.957730
This article is part of the Research TopicAdvances in Proctology and Colorectal SurgeryView all 45 articles
Background: Intestinal neuronal dysplasia (IND) is a rare condition mainly affecting the children. Constipation and abdominal distension have been reported as common manifestations. In addition, the reports about adult cases are scarce.
Case report: A 31-year-old man presented with pain in his left hip and intermittent fever for 1 month. The whole abdomen CT and pelvic contrast-enhanced MRI revealed a left psoas abscess (PA). The patient has been given anti-infective treatment and underwent CT-guided drainage of left PA with a temporary drain. But the patient's condition did not improve significantly. Then, the colonoscopy revealed that it may be the PA secondary to inflammatory bowel disease. But the pathology was not in line with inflammatory bowel disease. We finally performed an ileostomy surgery and took the whole layer of intestinal wall for biopsy. The pathological result revealed that a large number of proliferative ganglion cells and circuitous hyperplastic nerve fibers were found in the submucosa and muscular layer of the intestinal wall. Given pathological results and clinical manifestations, the patient was diagnosed with IND-B.
Conclusion: In this case, we first report an extremely rare case of adult IND manifesting as PA. So, this unusual case provides a new supplement to adult cases of IND.
Intestinal neuronal dysplasia (IND) is a rare anomaly of the enteric nervous system, with an estimated incidence of approximately one in 7,500 newborns (1). This disorder is a frequent cause of gut dysmotility and pseudo-obstruction which shows the clinical features similar to Hirschsprung's disease (HD). But, IND is a distinct clinical entity genetically different from HD (2). Due to IND mainly affecting children, few adult cases have been reported. Here, we report an extremely rare case of adult IND with psoas abscess (PA) as the initial symptom.
A 31-year-old man came to our hospital with left hip pain and intermittent fever for 1 month. For nearly a year, the patient occasionally has abdominal distention which alleviated after defecation. The frequency of defecation was about once every two days. The mass was seen as a reddish skin color around the anterior superior iliac spine which was painful and palpated.
The laboratory examination revealed white blood cell 13.25 × 109/L (3.5–9.5), neutrophil percentage 85% (40–75), platelet 420 × 109/L (125–350), C-reactive protein 82.6 mg/L (0–10) and erythrocyte sedimentation rate 48 mm/h (0–20). The tumor-related biomarkers (AFP, CEA, PSA, CA19–9, ferritin), serum tuberculosis antibodies and T-cell spot test for tuberculosis infection (T-TB.Spot) were within normal limits. The whole abdomen CT and pelvic contrast-enhanced MRI were performed. The imaging revealed a left PA (Figures 1A,B) Colonoscopy revealed mucosal stiffness and multiple polyps on the ascending colon (Figure 1C). Then, the mucosal biopsy of ascending colon was performed. To sum up, we think that it may be the PA secondary to inflammatory bowel disease. But pathology was not in line with the typical manifestations of inflammatory bowel disease.
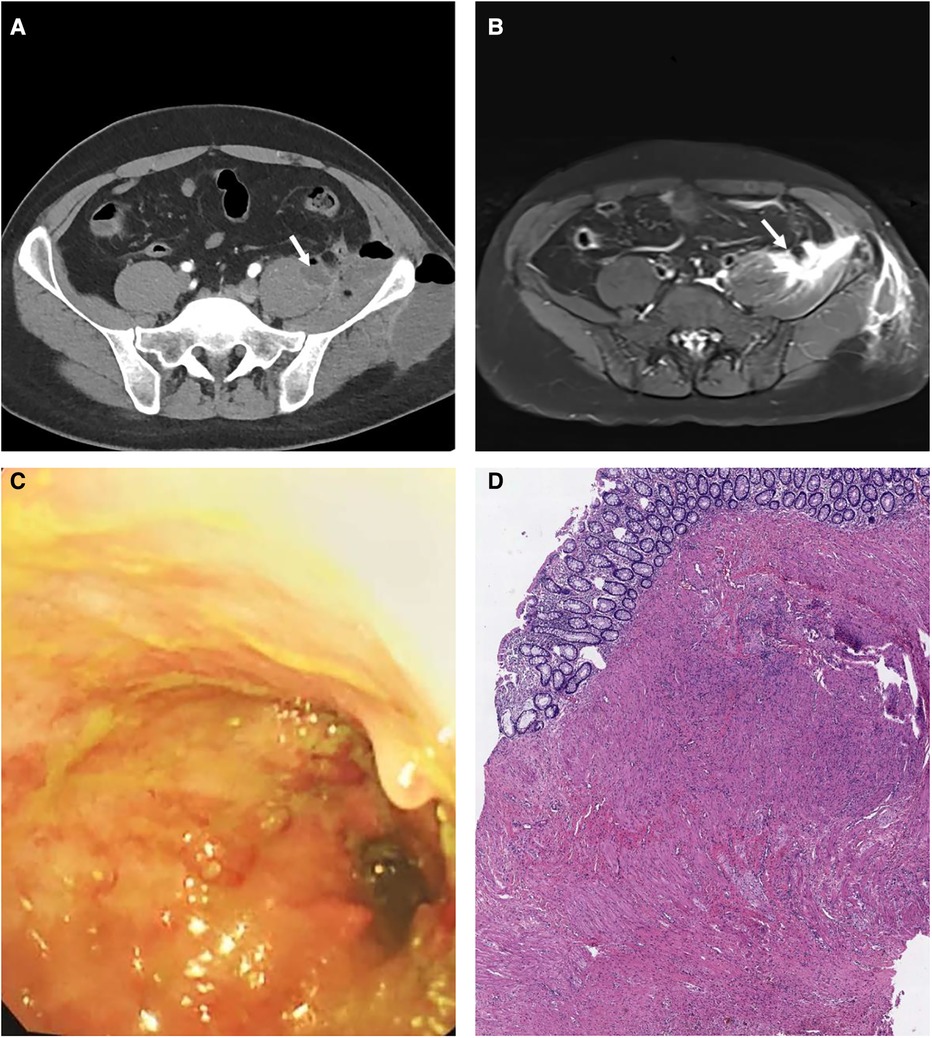
Figure 1. The abdominal CT showed patchy low-density shadow of the left pelvic wall soft tissue (A). The pelvic MRI showed that the lower part of the left psoas major muscle, the left pelvic wall and the left buttock were thickened with multiple high signal shadows (B). Colonoscopy showed multiple filling defects and local lumen stenosis in the terminal ileum, ileocecum and the beginning of the ascending colon (C). The pathological results revealed that a large number of proliferative ganglion cells and circuitous hyperplastic nerve fibers were found in the submucosa and muscular layer of the colon wall (D).
Since admission, the patient was given piperacillin sodium plus tazobactam for anti-infective treatment, but the patient's condition did not improve significantly. Then, the patient underwent CT-guided drainage of left PA with temporary drain placement and drained 450 ml pus. The patient still had intermittent pain and fever. We finally decided to perform a laparoscopic exploration. During the operation, we found the sigmoid colon with slight expansion and severely adhering to the surrounding tissue. Later, we performed a temporary ileostomy surgery and tried to take the whole layer of intestinal wall (descending colon, sigmoid colon about 0.5 cm in diameter) for biopsy. In addition, the primary closure was done after full thickness biopsy. The patient recovered well and was discharged two weeks after the operation. Moreover, followed up for 6 months after operation, the fever and pain in his left hip was no recurrence without specific treatment. The temporary stoma was scheduled to be closed one year after surgery.
The result of mucosal biopsy was scattered infiltration of lymphocytes, plasma cells and eosinophils in the colonic mucosa. The Haematoxylin and Eosin staining technique has been used for hystopathological diagnosis. The pathological results revealed that a large number of proliferative ganglion cells and circuitous hyperplastic nerve fibers were found in the submucosa and muscular layer of the intestinal wall (Figure 1D). Given pathological results and clinical manifestations, the patient was diagnosed with IND-B.
Swiss pathologist Meier-Rule first proposed the pathological phenomenon of colonic neuronal dysplasia in 1971 (3). It is classified into two clinical and histologically subtypes as types A or B. IND type B (IND-B), which comprises >95% of IND cases, is a pathological entity of the group of gastrointestinal neuromuscular diseases characterized by hyperplasia of the submucosal nerve plexuses (4) and presents as chronic constipation usually during childhood (5). In addition, the etiopathogenesis of IND-B is widely debated. It is mainly recognized as genetic alterations resulting in intestinal neuronal system development disorder (6, 7). However, IND-B can also be understood as a secondary phenomenon due to congenital intestinal obstructions or local inflammatory processes (8).
There had been several adult cases reported in the past few years. In addition, constipation and abdominal distension were a common manifestation in reported adult cases (9, 10). Referring to the relevant literature, the adult IND with PA as the initial symptom is reported for the first time in our case. The PA is an infectious disease with nonspecific clinical presentation which frequently leads to diagnostic difficulty. The PA is mostly secondary abscess. The most common etiologies of PA were vertebral osteomyelitis, colorectal cancer, gastrointestinal tract infection and Crohn's Disease (11, 12). Therefore, when the patient was admitted to the hospital, we first measured the tumor-related biomarkers, serum anti-tuberculosis antibodies and T-cell spot test for tuberculosis infection (T-TB.Spot). The above indexes all indicated negative results. And combining with imaging examinations, some possible diseases such as tuberculosis, tumor or vertebral osteomyelitis were excluded. In addition, we also took into account the diagnosis of Crohn's disease. In our case, both colonoscopy and barium enema revealed marked stenosis of colon, but the result of mucosal biopsy did not conform to the pathological manifestations of Crohn's disease. The above imaging and related examination results made the diagnosis more difficult, coupled with long-term anti-infective treatment did not have a good effect. Finally, we decided to explore the abdominal cavity and perform full-thickness biopsy of colon wall. Pathologic examination of the specimen showed that there were a large number of proliferated ganglion cells and nerve fibers in the submucosa and muscular layer of the colon wall, which can be considered as an important reference index in the process of diagnosis. Combining the clinical manifestations with the results of pathological and laboratory investigations, the diagnosis of IND-B was established.
Due to the rarity of adult cases and the non-specificity of symptoms, the diagnosis of adult IND is more difficult than that of infants. And early diagnosis remains a great challenge for IND. The auxiliary diagnostic methods include barium enema, anorectal manometry and rectal mucosa biopsy. However, the histological examination remains the gold standard of the diagnosis. Usually, it is necessary to include a sufficient amount of submucosa in the suction biopsy specimens. In this case, it is worth noting that the rectal mucosal biopsy of the patient was negative. Thus, full-thickness biopsy of colon wall can be considered as an important reference index in the diagnosis of IND.
According to the latest report, blood Sox 10 promoter methylation can be used as a noninvasive and efficient diagnosis method for IND (13). Recently, an endoscopic device has been developed to obtain full-thickness biopsies from the bowel wall without laparotomy and anesthesia (14). It is a promising minimally invasive procurement of intestinal full-thickness biopsies for the diagnosis of intestinal neuropathies.
In conclusion, for patients with PA, physicians should consider IND as a possible diagnosis after excluding other more common causes. So, this unusual case of psoas major abscess provides a new supplement to adult cases of IND. More importantly, a non-invasive diagnostic method with a high degree of accuracy needs to be developed. No matter for the diagnosis and treatment of IND in infants and adults, further exploration is needed and attention should be paid to individual treatment.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
BR, BZ, and SC: collected the data and drafted the manuscript. HH and DS: reviewed and modified the manuscript. All authors contributed to the article and approved the submitted version.
This research was supported by National Natural Science Foundation of China, under Grant No. 81770537 and 82070554.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Granero Cendón R, Millán López A, Moya Jiménez MJ, López Alonso M, De Agustín Asensio JC. Intestinal neuronal dysplasia: association with digestive malformations. Cir Pediatr. (2007) 20(3):166–8.
2. Tou JF, Li MJ, Guan T, Li JC, Zhu XK, Feng ZG. Mutation of RET proto-oncogene in Hirschsprung’s disease and intestinal neuronal dysplasia. World J Gastroenterol. (2006) 12(7):1136–9. doi: 10.3748/wjg.v12.i7.1136
3. Meier-Ruge W. Casuistic of colon disorder with symptoms of Hirschsprung’s disease (author’s transl). Verh Dtsch Ges Pathol. (1971) 55:506–10.4130757
4. Knowles CH, De Giorgio R, Kapur RP, Bruder E, Farrugia G, Geboes K, et al. The London classification of gastrointestinal neuromuscular pathology: report on behalf of the Gastro 2009 International Working Group. Gut. (2010) 59(7):882–7. doi: 10.1136/gut.2009.200444
5. Schappi MG, Staiano A, Milla PJ, Smith VV, Dias JA, Heuschkel R, et al.: A practical guide for the diagnosis of primary enteric nervous system disorders. J Pediatr Gastroenterol Nutr 2013, 57(5):677–86. doi: 10.1097/MPG.0b013e3182a8bb50
6. O'Donnell AM, Puri P. A role for Pten in paediatric intestinal dysmotility disorders. Pediatr Surg Int. (2011) 27(5):491–3. doi: 10.1007/s00383-010-2828-6
7. Wang D, Gao N, Zhou T, Zhang Q, Wang J, Li A. Effect of Neuroligin1 and Neurexin1 on the colonic motility in a mouse model of neuronal intestinal dysplasia. Gastroenterol Res Pract. (2020) 2020:9818652. doi: 10.1155/2020/9818652
8. Sacher P, Briner J, Hanimann B. Is neuronal intestinal dysplasia (NID) a primary disease or a secondary phenomenon? Eur J Pediatr Surg. (1993) 3(4):228–30. doi: 10.1055/s-2008-1063549
9. Ahmad T, Riaz M, Khan A, Khan MM. Hirschsprung’s disease: a rare entity in adults. J Coll Physicians Surg Pak. (2019) 29(7):674–6. doi: 10.29271/jcpsp.2019.07.674
10. Škába R, Hoch J, Jech Z, Kynčl M, Campr V. Hirschsprungs disease in adults two case reports and review of the literature. Rozhl Chir. (2018) 97(3):133–8.
11. Ouellette L, Hamati M, Flannigan M, Singh M, Bush C, Jones J. Epidemiology of and risk factors for iliopsoas abscess in a large community-based study. Am J Emerg Med. (2019) 37(1):158–9. doi: 10.1016/j.ajem.2018.05.021
12. Sato T, Kudo D, Kushimoto S. Epidemiological features and outcomes of patients with psoas abscess: a retrospective cohort study. Ann Med Surg. (2021) 62:114–8. doi: 10.1016/j.amsu.2021.01.040
13. Liu YR, Ba F, Cheng LJ, Li X, Zhang SW, Zhang SC. Efficacy of Sox10 promoter methylation in the diagnosis of intestinal neuronal dysplasia from the peripheral blood. Clin Transl Gastroenterol. (2019) 10(12):e00093. doi: 10.14309/ctg.0000000000000093
Keywords: intestinal neuronal dysplasia, psoas abscess, inflammatory bowel disease, case report, constiption
Citation: Ren BB, Zhang B, Chen SX, Han HQ and Sun DQ (2022) Intestinal neuronal dysplasia presenting as psoas abscess: A case report. Front. Surg. 9:957730. doi: 10.3389/fsurg.2022.957730
Received: 31 May 2022; Accepted: 10 October 2022;
Published: 1 November 2022.
Edited by:
Renato Pietroletti, University of L’Aquila, Italy© 2022 Ren, Zhang, Chen, Han and Sun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Da-Qing Sun c2RxY2hyaXMyMDE5QHRtdS5lZHUuY24=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.