
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
METHODS article
Front. Surg., 06 January 2023
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.951820
This article is part of the Research TopicClinical Application of Medical Imaging for Functional Evaluation in OrthopaedicsView all 21 articles
 Yufeng Lu1
Yufeng Lu1 Xue Wang2
Xue Wang2 Bo Yang3
Bo Yang3 Zhaochen Xu1
Zhaochen Xu1 Baogang Zhang1
Baogang Zhang1 Bin Jia1
Bin Jia1 Jinlong He1
Jinlong He1 Liang Qi1
Liang Qi1 Min Wang1
Min Wang1 Feng Qiao1*
Feng Qiao1*
Purpose: Open-wedge high tibial osteotomy (HTO) is a common surgical treatment for medial osteoarthritis in young and active patients. The accuracy of osteotomy is closely associated with postoperative efficacy. The accuracy of digital preoperative planning is higher than that of the preoperative manual measurement and several computer software with varying accuracy and convenience are used for digital preoperative planning. This study aimed to use the SolidWorks software for HTO preoperative planning and to determine its accuracy and reliability in HTO preoperative planning.
Methods: We reviewed the data of 28 patients with 54 with medial compartment knee arthritis who underwent open-wedge HTO preoperative planning using SolidWorks between June 2019 and March 2021. The standard anteroposterior standing whole-leg radiographs were assessed before and 6 weeks after the surgery. The correction angle, weight-bearing line (WBL) ratio, mechanical femorotibial angle (mFTA), and medial proximal tibial angle (MPTA) before and after the surgery were compared. The clinical results were evaluated using the Knee Society score.
Results: At 6 weeks after the surgery, the WBL ratio was corrected from 16.8% to 50.5%, mFTA was corrected from 6.4° varus to 1.2° valgus, and MPTA was corrected from 83.4° to 89.3°. No significant difference was observed between the predicted correction angle before the surgery and the correction angle measured 6 weeks after the surgery (t = −1.745, p = 0.087). The knee score and function score of Knee Society increased from 76.4 and 80.7 before surgery to 95.0 and 95.7, respectively.
Conclusions: The SolidWorks software showed high accuracy and reliability in preoperative planning of open-wedge HTO in patients with medial compartment knee arthritis.
High tibial osteotomy (HTO) is an effective method for the treatment of medial single-compartment knee osteoarthritis as it corrects the weight-bearing line (WBL) of the lower limbs (1). Currently, lateral closing wedge HTO and open-wedge HTO (OWHTO) are most commonly used. Compared with lateral closing wedge HTO, OWHTO is less traumatic, simpler, more convenient for the intraoperative adjustment of lower limb alignment, more accurate in deformity correction, and easily convertible to total knee arthroplasty without the need for fibula osteotomy (2). OWHTO is widely used and has achieved a favorable outcome in young and active patients with medial compartment knee arthritis.
Previous studies have reported that the accuracy of limb alignment correction is important in determining the success of HTO. Both over-correction and under-correction can affect the clinical outcome and survival rate of patients with medial compartment knee arthritis after HTO. According to the biomechanical studies performed by Hsu et al. (3), the medial compartment of the knee joint with a 1.2° mechanical femorotibial angle (mFTA) varus deformity can share 75% of the weight in a single-leg weight-bearing. To improve the accuracy of OWHTO, designing the correction angle and the opening gap preoperatively is necessary to determine the target WBL passing through a certain point of the tibial plateau in standing whole-leg radiographs. Currently, the most commonly used preoperative planning methods are the Miniaci method (4–7), Dugdale–Noyes method (8, 9), and Coventry method (10). Studies have reported that the Miniaci method is reliable, convenient, and simple to measure the opening angle and gap. It is most commonly used for OWHTO preoperative planning. Because of the wide applications of the picture archiving and communication system (PACS), orthographic images can be magnified at desirable magnification using the computer, thus making radiographic measurement convenient in preoperative planning. Studies have reported that the use of PACS for preoperative planning is highly reliable (11–13). In recent years, several computer software has originated to assist surgeons in HTO preoperative planning, such as the Materialise OrthoView software, Osteotomy Master (14), Biomet Orthosize, mediCAD (15, 16), and PreOPlan (16), which can be used to import patients' full-length orthographic images of lower limbs to calculate the opening angle and gap of the osteotomy. The accuracy of osteotomy has been greatly improved using these techniques. Recently, computer navigation (17) and three-D printing individualized osteotomy templates (18) have been developed to improve the accuracy of osteotomy but they are expensive and cumbersome for preoperative planning.
Since 2019, researchers are using the SolidWorks software in our institution for OWHTO preoperative planning, and good results have been achieved. This study aimed to evaluate the accuracy and reliability of the SolidWorks software for preoperative planning in patients undergoing medial OWHTO by comparing the preoperative and postoperative WBL ratio and opening angle.
The study protocol was approved by the Institutional Review Board of our hospital (approval no. 202109009). Written informed consent was obtained from all participants.
We reviewed the medial open-wedge HTO performed by our center from June 2019 to April 2021.
The subject inclusion criteria were as follows: (1) age <45 years, (2) preoperative plan to use the SolidWorks software, (3) preoperative planning to design the knee joint weight line at 50% of the tibial plateau, and (4) knee varus deformity, varus <15°, knee joint Medial pain, osteoarthritis grade K-L 0-I grade; and (5) no restriction of the knee joint movement.
The study exclusion criteria were as follows: (1) presence of lesions in the lateral compartment of the knee joint; (2) knee joint ligament injuries, including medial and lateral laxity, instability of varus and valgus, and anterior and posterior cruciate ligament injuries; (3) obese patients, with BMI >30 kg/m2, and (4) inflammation arthritis such as rheumatoid arthritis.
Using these criteria, 54 knees of 28 patients (15 women and 13 men) were included. There were a total of 26 left knees and 28 right knees. Of the 26 bilateral HTOs, 25 were performed bilaterally at one stage. One case underwent a procedure on the right side first, followed by that on the left side after 5 months. The mean patient age at the time of index operation was 32.6 ± 7.7 years (range: 18–44 years). The mean follow-up was 25.6 ± 6.8 months (range: 4–26 months) (Table 1).
The preoperative plan was completed by a senior orthopedic surgeon Qiao Feng. All patients were taken preoperatively with a standard anteroposterior full-length lower limb weight-bearing radiography.
We input the standard plain AP standing whole-leg radiographs into the SolidWorks 2016 (Dassault Systemes, USA) and corrected the radiograph magnification so that the software measured according to the scale marked on the radiograph.
The following measurements were made:
1. Draw a line from the center of the femoral head to the midpoint of the tibial plateau and extend it distally beyond the ankle joint. We defined this line as the target weight-bearing line (Figure 1).
2. Mark the lateral hinge point. We selected a point 15-mm distal to the lateral tibial plateau and an 8-mm medial to the proximal lateral cortex of the tibia as the lateral hinge point. Make a concentric circle with a lateral hinge point as the center, passing through the center of the ankle joint and the target weight-bearing line (Figure 2).
3. The osteotomy site was marked. We took the medial edge of the tibial plateau as the center, with a radius of 40 mm for the concentric circles, and the intersection with the medial cortex of the tibia was marked as the osteotomy site (Figure 3).
4. A line was made connecting the lateral hinge point and the center of the ankle joint, with a line connecting the lateral hinge point and the intersection of the target weight-bearing line and the circle. The angle formed by the two lines served as the predicted correction angle.
5. Concentric circle was made with the lateral hinge point as the center and pass through the osteotomy site, and intersects the target WBL and the line from the lateral hinge point to the center of the ankle joint. The distance between the two intersection points was considered as the predicted correction gap (Figure 4).

Figure 1. The target weight-bearing point (O) was set at 50% of the tibial plateau, and L1 represents the target weight-bearing line.
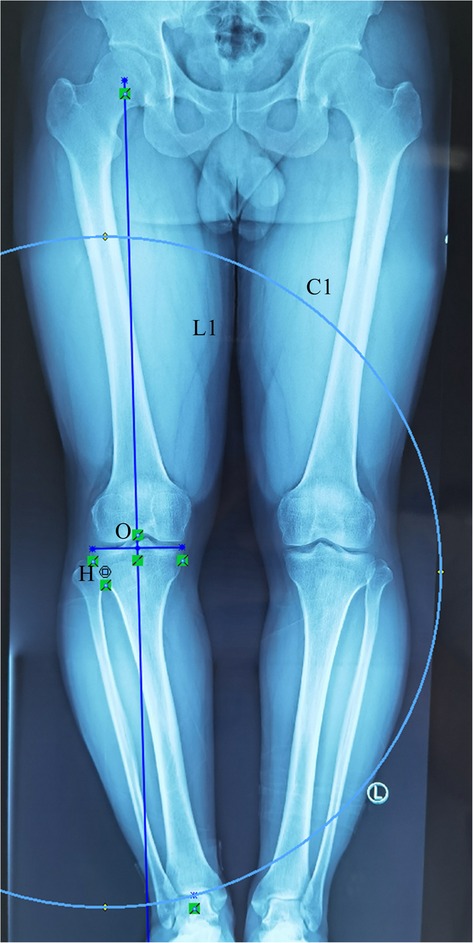
Figure 2. The site 15-mm distal to the lateral tibial plateau and 8-mm medial to the lateral cortex of the proximal tibia were selected as the hinge point (H). With point H as the center, a concentric circle was drawn through the center of the ankle joint (C1).
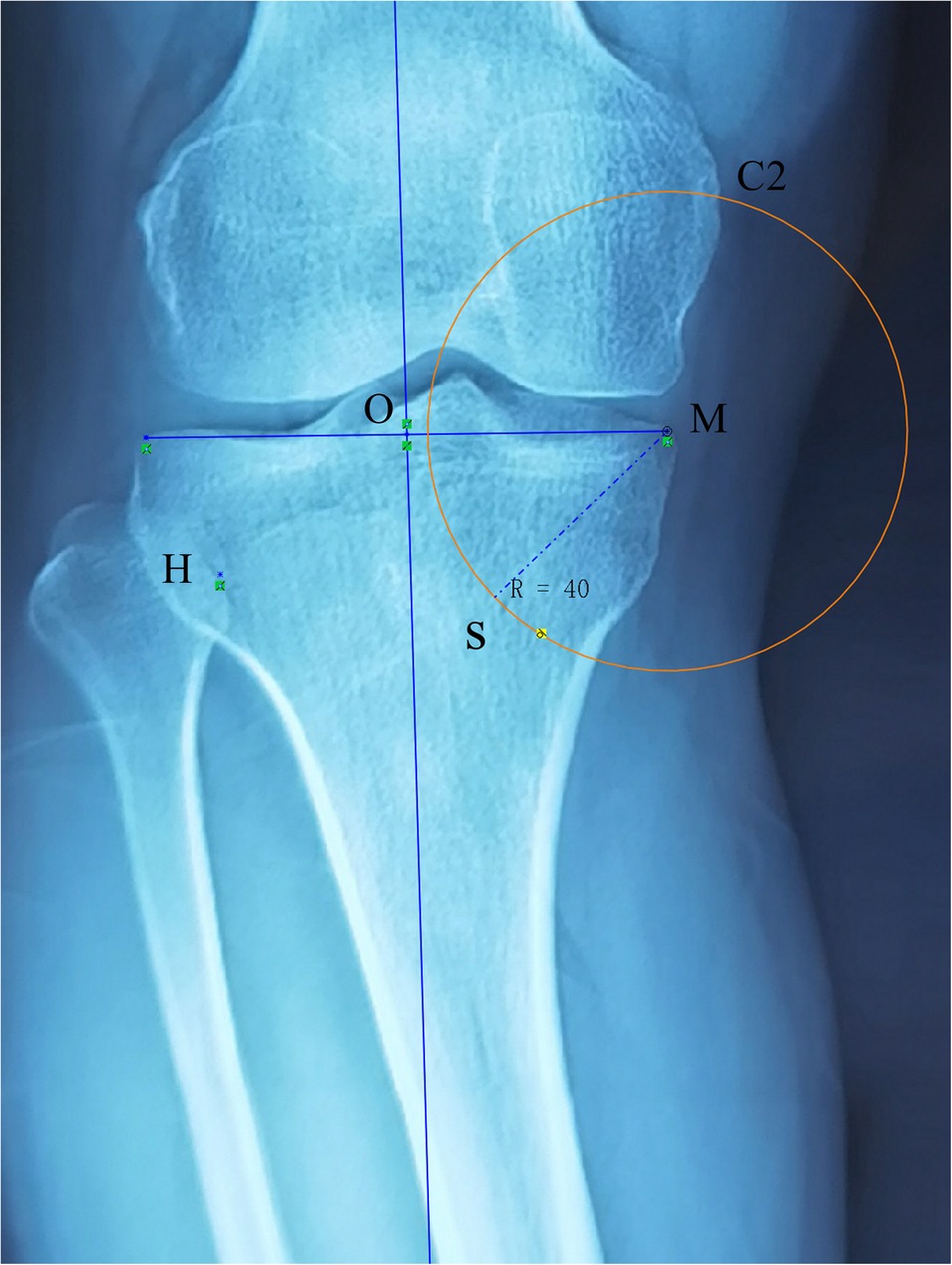
Figure 3. Point M represents the medial border of the tibial plateau. With M as the center and a concentric circle was drawn with a radius of 40 mm, which intersected at point S of the medial cortex of the tibia. Point S was selected as the osteotomy site.
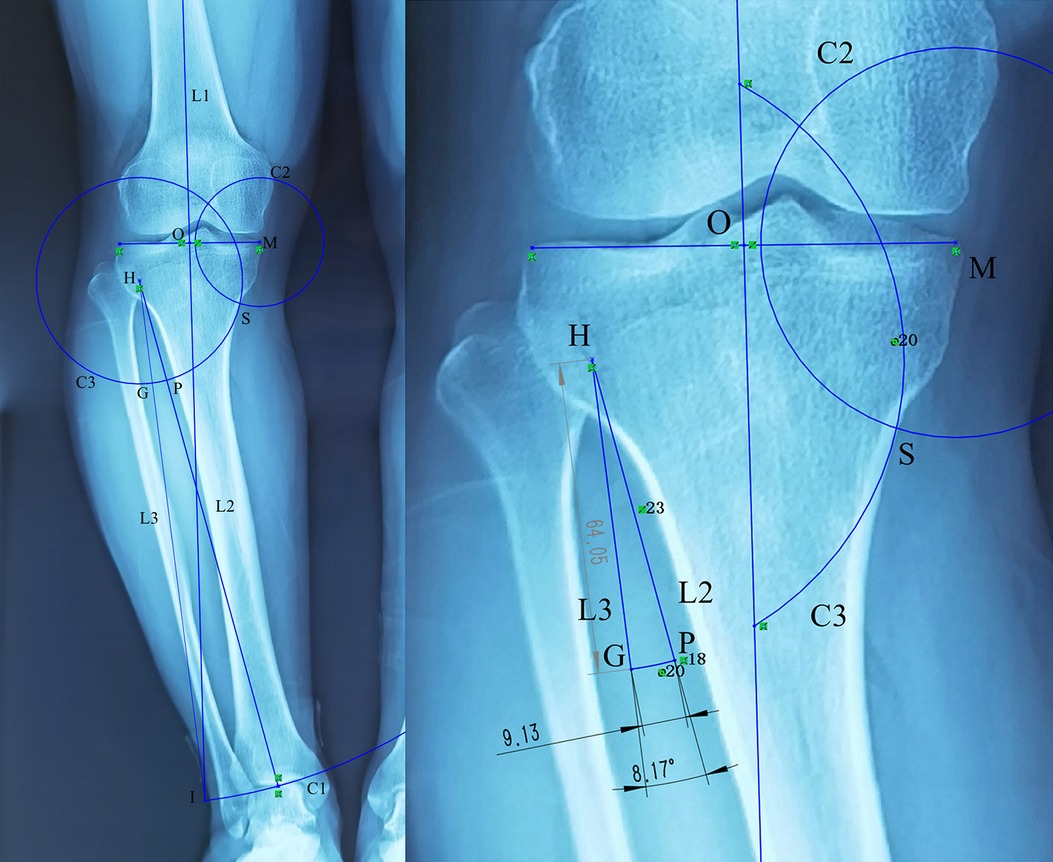
Figure 4. The H point was used as the center, and the distance from the H point to the ankle joint center (L2) was used as the radius to draw a concentric circle, L1 intersected at the I point, and line segment HI (L3) was drawn. The angle formed by L2 and L3 indicates the correction angle. Taking point H as the center, HS was used as the radius to draw a concentric circle that intersected L2 at point P and L3 at point G, while the length of the line segment PG indicated the length of the correction gap.
All surgeries were performed by the same senior orthopedic surgeon. The patient was asked to lay down in a supine position, the affected limb was routinely disinfected, and the tourniquet was applied. Create a longitudinal incision on the anterior medial side of the tibia with a length of 4 cm–6 cm. The skin was cut subcutaneously and the deep fascia sequentially. The 4-cm distal end of the medial tibial plateau was used as the osteotomy site (using a 4-cm long-cut Kirschner wire to determine under fluoroscopy), and a ф 2.0 Kirschner wire was inserted oriented medially to laterally, to the target hinge point (approximately 15-mm distal to the lateral tibial plateau, 8-mm inside the outer edge of the tibia). After fluoroscopy confirmed the correct position, the osteotomy line parallel to the tibial slope on the sagittal plane was marked. The pes anserinus tendons were dissected and the superficial medial collateral ligament was freed and retracted along the designed osteotomy line. Next, 2 Kirschner wires were inserted again on the marked osteotomy line, and 1 Kirschner wire was inserted into the posterior side of the tibial tubercle. After a blunt retractor was inserted posterior to the medial collateral ligament and the tibia to protect the neurovascular structures posterior to the incision line, an oscillating saw with 0.9-mm-thick saw blade was used to perform biplane osteotomy. During the sawing process, as per the preoperative plan, the sawing depth was controlled by the length scale of the saw blade. Then, stepwise insertion of 3–5 coupled chisels was performed into the osteotomy line and the spreader was finally used to gradually open out the medial cortex carefully, and then a trimmed tape was prepared during the operation, keeping the length exactly equal to the distance calculated preoperatively using the SolidWorks plus Saw blade thickness. When the opening reached the target distance, the laminar spreader was inserted into the posteromedial cortex of the tibia to maintain the realignment position. Finally, the TomoFix plate and locking screws (TomoFix, Synthes GmbH, Switzerland) were used to fix the osteotomized tibia. We did not use intraoperative fluoroscopy to examine the mechanical axis. The pes anserinus was not reconstructed when the wound was closed. If the tension of the medial collateral ligament was excessively large, the pie-crusting technique was used to loosen it until the tension was appropriate. None of the patients' lateral hinges were broken during the operation. We performed structural bone grafting for an opening distance >15 mm. On the first day after the operation, quadriceps and range-of-motion exercises were initiated. Full weight-bearing was allowed on the second day of surgery.
All measurements were performed on the AP standing whole-leg radiographs using picture archiving and communication systems (PACS) (Synapse, Fujifilm Inc., Tokyo Japan) before surgery and at 6 -weeks postoperative follow-up. (1) The percentage of the WBL passing through the tibial plateau (calculated from the medial plateau) (Figure 5); the acceptable postoperative range was set to 50 ± 5% (range: 45%–55%), and percentages lower or higher than this range were defined as under- or over-correction, respectively. (2) Mechanical femorotibial angle (mFTA). (3) Mechanical medial proximal tibial angle (mMPTA). (4) The correction angle. (5) Preoperative correction distance. Due to the occlusion of the plate, the correction distance of the osteotomy site on the medial tibia cannot be measured after the operation.
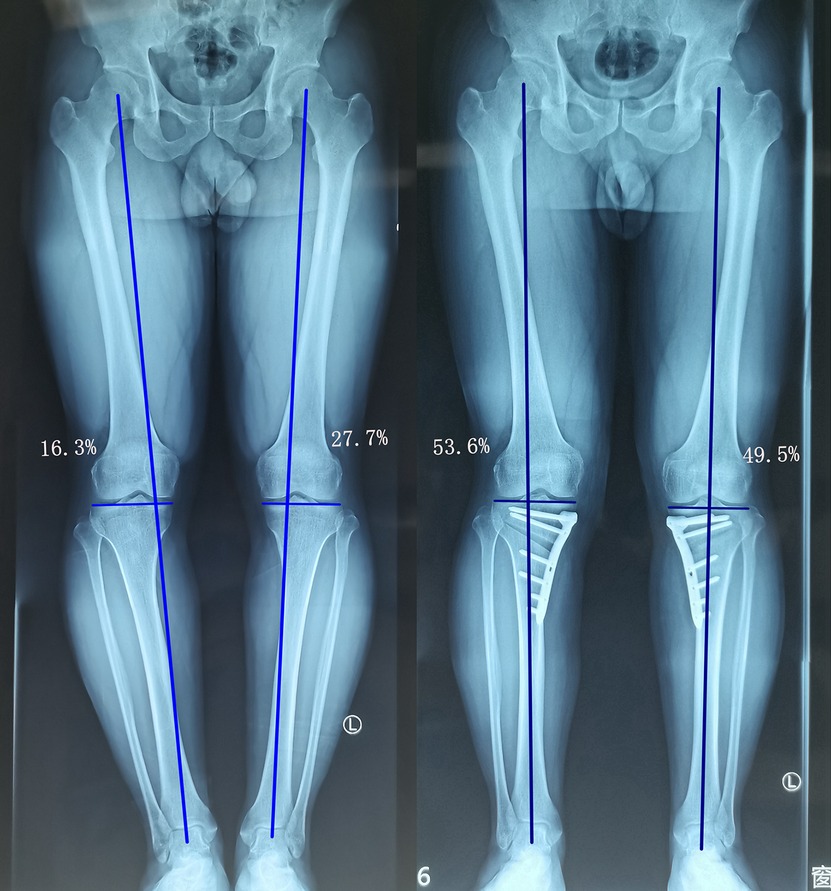
Figure 5. A 37-year-old man presented with medial compartment osteoarthritis (K-L grade I) and varus deformity in both knees. The WBL ratios of the left and right sides were 27.7% and 16.3% preoperatively, and 49.5% and 53.6% postoperatively, respectively.
All measurements were performed by 2 observers who did not participate in the operation. After 3 weeks, the measurement was performed again. The intraclass correlation coefficient (ICC) was applied to determine the reliability of the measurement. The ICC values were characterized as follows: poor agreement (<0.40), fair to good agreement (0.40–0.75), and excellent agreement beyond chance (>0.75). The measurement data used the mean value of the first measurement of the 2 observers.
Clinical outcome assessment used the knee social score (KSS) pre-operatively and at the final follow-up. The KSS comprises two parts: a knee score, which includes pain, stability, and a range of motion (ROM), and a function score, which includes the patient's ability to walk and climb stairs and the need for ambulatory aids.
Statistical analysis was performed using PASW Statistics ver.18.0 (SPSS Inc., Chicago, IL, USA). All measurement data were expressed as mean ± standard deviation. The paired t-test was used to compare the preoperative and postoperative parameters. P < 0.05 was set to indicate a statistically significant difference.
The Kolmogorov–Smirnov test showed that all data followed the normal distribution pattern. ICC and interclass correlation coefficients for the reproducibility of all parameters were >80% (Table 2).
The WBL ratio on the tibial plateau was corrected from the preoperative mean of 16.8% ± 13.0% (range, −37.3% to 36.7%) to the postoperative mean of 50.5% ± 4.4% (range, 40.6% to 62.3%) (t = 53, p < 0.001) (Table 3).
Forty-three knees of correction were found to be within the acceptable range (79.6%, 49.3% ± 2.6%), 2 knees were under-corrected (3.7%, 41.8% ± 1.7%), and 9 knees were over-corrected (16.7%, 58.1% ± 1.8%) based on the WBL on the tibial plateau.
The mFTA was varus 6.4 ± 2.8° before the surgery and valgus 1.2 ± 1.3° after the surgery (Table 3). The preoperatively planned opening angle was 8.5 ± 3.5°, and the postoperative measurement correction angle was 8.8 ± 2.9°. No statistical difference was observed in the preoperative opening angle and postoperative correction angle (t = 1.745, P = 0.087) (Table 3). The average planned preoperative opening gap was 8.9 ± 3.7 mm. The KSS was significantly improved after the surgery (95.0 ± 3.6) compared with the preoperative KSS (76.4 ± 8.2). The functional score was improved after the surgery (95.7 ± 4.9) compared with the preoperative functional score (80.7 ± 9.1) (Table 3).
Digital preoperative planning has become the mainstream in OWHTO. He et al. (14) used the OsteoMaster software for preoperative planning, and the operation time and the number of x-ray fluoroscopy were significantly reduced compared with the traditional Miniaci method. The accuracy, depth, open height, correction angle, FTA, and WBL ratio of osteotomy were not reduced compared with the traditional Miniaci method. Kim et al. (11) used PACS technology for preoperative planning of open-wedge HTO and used the Miniaci method to measure the preoperative tibial plateau WBL ratio, correcting angle, and opening distance and to compare them with those of the last postoperative follow-up. No statistical difference was found between parameters obtained by preoperative planning and postoperative x-ray radiography, indicating that PACS technology can be used for HTO preoperative planning.
Lee et al. (19) used the PACS-photoshop method and the Real-size paper template method for OWHTO preoperative planning, compared the two methods prospectively, and found that the former is highly reliable. Later, they (20) reviewed 72 cases treated by open-wedge HTO using the PACS-Photoshop method for preoperative planning. The postoperative measurement average correction gap was 10.8 mm; the correction gap of <10.8 mm was divided into one group, and that higher than 10.8 mm was divided into another group. By comparing the postoperative correction gap with the measured preoperative correction gap, they found that when the correction gap is large, the difference between the postoperative and preoperative WBL ratios increases. However, it did not deviate toward the side of either over-correction or under-correction. Schröter et al. (16) studied the inter-group reliability of the digital software PreOPlan and mediCAD for open-wedge HTO preoperative planning and found that both the software preoperative plans have a high degree of inter-group reliability, and are unaffected by the experience of the measurer. They (15) used the mediCAD digital software for OWHTO preoperative planning and closed distal femur osteotomy (DFO) preoperative planning for severe knee varus osteoarthritis, and good imaging and clinical results were obtained.
Some studies recently reported the use of 3D-planned patient-specific instrumentation (PSI) (21) and navigation system (22) to perform open-wedge HTO and a more accurate WBL ratio, especially tibial slope was obtained. However, Tardy et al. (23) performed a multi-center non-randomized controlled prospective observational study by comparing the parameters of 126 patients in the navigation group, PSI group, and traditional group using the Miniaci method in 11 centers. The results showed that none of the 3 techniques were superior in achieving target correction at 1 year. All the 3 techniques were reliable and precise in HTO planning.
The SolidWorks software is a powerful engineering drawing software. We have developed its imaging measurement function in the medical field. SolidWorks can mark equidistant points by making concentric circles. When SolidWorks measures the length, the accuracy can reach 0.0000001 mm and when it measures the angle, the accuracy can reach 0.0001°. However, the accuracy of PACS measuring length is only 0.01 mm, while the accuracy of measuring angle length is 1°. SolidWorks uses the principle that all radii of concentric circles are equal in length to reduce the measurement steps and the measurement errors. Compared with PACS, SolidWorks not only reduced the errors and improved the accuracy of the measurement but also reduced the measurement steps and improved the efficiency of the measurement. When compared to other 2D digital measurement software, SolidWorks measurement accuracy is the highest.
When open-wedge HTO is used to treat medial knee osteoarthritis, the optimal position of the lower limb WBL on the tibial plateau is debatable. Most studies (4, 5, 11, 14, 18, 22) have used the Fujisawa point as the target load line passing point of the tibial plateau. We used the Fujisawa point as the target point for performing open-wedge HTO in patients aged >45 years and having K-L grade II or higher for medial knee osteoarthritis. However, young and active patients <45 years of age and K-L grade did not exceed grade I for medial knee osteoarthritis when 50% of the tibial plateau was the target point. The short-term results of all cases were desirable but the long-term results will need follow-up.
Yoon et al. (5) compared the use of PACS for preoperative planning and intraoperative use of a cable method for open-wedge HTO using the tibial plateau target WBL ratio ±5° as the acceptable range of correction and found that the acceptable range of the intraoperative wire method was 55%, whereas that of the PACS method was 71.8%. Miniaci et al. (24) reported that only 50% of their cases were within the acceptable range (±10%) of correction after proximal tibial osteotomy. Kim et al. (11) used the PACS method for preoperative planning of OWHTO, and the acceptable range of correction (±5%) after surgery was 70%, under-correction was 20%, and over-correction was 10%. Using the SolidWorks software, we achieved the acceptable WBL ratio (±5%) of 79.6%, the under-correction of 3.7%, and the over-correction of 16.7%. The advantage of using the SolidWorks method is that fluoroscopy is not required to determine the alignment of the lower extremities during the surgery, thus reducing the x-ray radiation damage and the surgical time.
This study has several limitations. First, this study is a retrospective study having a small sample size and short follow-up time. Further studies using a large sample size and more patients are required to confirm the study findings. It would be best to perform a prospective randomized controlled study with a longer follow-up time to obtain more reliable results. Second, Sabharwal et al. (25) reported that the standing full-length anteroposterior radiograph magnification rate of the lower limbs was 4.6%. Their minimum patient-to-tube distance was 203 cm, whereas the minimum distance in our image center was 180 cm. Therefore, our magnification may be greater, which may be the reason for obtaining overall large values including the WBL ratio. Third, during the surgery, we controlled the posterior slope of the tibia by making the sagittal plane osteotomy line parallel to the tibial joint line and ensuring that the two osteotomy planes of the tibial tubercle were parallel. However, we did not compare the posterior tibial slope before and after the surgery. Finally, we kept the WBL in the center of the tibial plateau, which is debatable.
The SolidWorks software showed high accuracy and reliability in preoperative planning of open-wedge HTO in patients with medial compartment knee arthritis.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Review Board of Xi'an Honghui Hospital (approval no. 202109009). The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
LY participated in the study design, and drafted the manuscript. XZ, ZB, JB, QL, and WM followed up with patients and provided the data. WX and HJ performed postoperative radiograph measurements. YB Interpreted and analyzed the data. QF designed the study and supervised the whole study process, and helped to review the manuscript. All authors contributed to the article and approved the submitted version.
The study was supported by a grant from Shaanxi Provincial Key Research and Development Project (CN) (grant no. 2019SF-214) and Traditional Chinese Medicine Inheritance and Innovation and “Qin Medicine” Development Key Scientific Research Project (2021-04-22-006).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.951820/full#supplementary-material.
1. Lee OS, Ahn S, Ahn JH, Teo SH, Lee YS. Effectiveness of concurrent procedures during high tibial osteotomy for medial compartment osteoarthritis: a systematic review and meta-analysis. Arch Orthop Trauma Surg. (2018) 138(2):227–36. doi: 10.1007/s00402-017-2826-4
2. Wu L, Lin J, Jin Z, Cai X, Gao W. Comparison of clinical and radiological outcomes between opening-wedge and closing-wedge high tibial osteotomy: a comprehensive meta-analysis. PLoS One. (2017) 12(2):e0171700. doi: 10.1371/journal.pone.0171700
3. Hsu RW, Himeno S, Coventry MB, Chao EY. Normal Axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res. (1990) 255:215–27. doi: 10.1097/00003086-199006000-00029
4. Elson DW, Petheram TG, Dawson MJ. High reliability in digital planning of medial opening wedge high tibial osteotomy, using Miniaci's method. Knee Surg Sports Traumatol Arthrosc. (2015) 23(7):2041–8. doi: 10.1007/s00167-014-2920-x
5. Yoon SD, Zhang G, Kim HJ, Lee BJ, Kyung HS. Comparison of cable method and Miniaci method using picture archiving and communication system in preoperative planning for open wedge high tibial osteotomy. Knee Surg Relat Res. (2016) 28(4):283–8. doi: 10.5792/ksrr.16.052
6. Jiang X, Xie K, Han X, Ai S, Wu H, Wang L, et al. HKA angle-A reliable planning parameter for high tibial osteotomy: a theoretical analysis using standing whole-leg radiographs. J Knee Surg. (2022) 35(1):54–60. doi: 10.1055/s-0040-1712945
7. Blackburn J, Ansari A, Porteous A, Murray J. Reliability of two techniques and training level of the observer in measuring the correction angle when planning a high tibial osteotomy. Knee. (2018) 25(1):130–4. doi: 10.1016/j.knee.2017.11.007
8. Herman BV, Giffin JR. High tibial osteotomy in the ACL-deficient knee with medial compartment osteoarthritis. J Orthop Traumatol. (2016) 17(3):277–85. doi: 10.1007/s10195-016-0413-z
9. Sivertsen EA, Vik J, Meland ASV, Nerhus TK. The Dugdale planning method for high tibial osteotomies underestimates the correction angle compared to the Miniaci method. Knee Surg Sports Traumatol Arthrosc. (2021). doi: 10.1007/s00167-021-06663-z. [Epub ahead of print]34244828
10. Coventry MB, Ilstrup DM, Wallrichs SL. Proximal tibial osteotomy. A critical long-term study of eighty-seven cases. J Bone Joint Surg Am. (1993) 75(2):196–201. doi: 10.2106/00004623-199302000-00006
11. Kim HJ, Lee HJ, Shin JY, Park KH, Min SG, Kyung HS. Preoperative planning using the picture archiving and communication system technique in high tibial osteotomy. J Orthop Surg (Hong Kong). (2017) 25(1):2309499016684701. doi: 10.1177/2309499016684701
12. Kim YT, Choi JY, Lee JK, Lee YM, Kim JI. Coronal tibiofemoral subluxation is a risk factor for postoperative overcorrection in high tibial osteotomy. Knee. (2019) 26(4):832–7. doi: 10.1016/j.knee.2019.05.011
13. Kim JE, Kim DH, Lee JI, Choi HG, Jung YS, Lee SH, et al. Difference of preoperative varus-valgus stress radiograph is effective for the correction accuracy in the preoperative planning during opening-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. (2021) 4:1035–44. doi: 10.1007/s00167-020-06076-4
14. He A, Mao Y, Zhou Y, Kong Q, Zhang H, Chen Y, et al. Preoperative planning by osteotomy master software helps to improve the accuracy of target limb alignment in high tibial osteotomy. J Orthop Surg Res. (2020) 15(1):504. doi: 10.1186/s13018-020-02033-6
15. Schröter S, Nakayama H, Yoshiya S, Stöckle U, Ateschrang A, Gruhn J. Development of the double level osteotomy in severe varus osteoarthritis showed good outcome by preventing oblique joint line. Arch Orthop Trauma Surg. (2019) 139(4):519–27. doi: 10.1007/s00402-018-3068-9
16. Schröter S, Ihle C, Mueller J, Lobenhoffer P, Stöckle U, van Heerwaarden R. Digital planning of high tibial osteotomy. Interrater reliability by using two different software. Knee Surg Sports Traumatol Arthrosc. (2013) 21(1):189–96. doi: 10.1007/s00167-012-2114-3
17. Schröter S, Ihle C, Elson DW, Döbele S, Stöckle U, Ateschrang A. Surgical accuracy in high tibial osteotomy: coronal equivalence of computer navigation and gap measurement. Knee Surg Sports Traumatol Arthrosc. (2016) 24(11):3410–7. doi: 10.1007/s00167-016-3983-7
18. Kuriyama S, Morimoto N, Shimoto T, Takemoto M, Nakamura S, Nishitani K, et al. Clinical efficacy of preoperative 3D planning for reducing surgical errors during open-wedge high tibial osteotomy. J Orthop Res. (2019) 37(4):898–907. doi: 10.1002/jor.24263
19. Lee YS, Kim MK, Byun HW, Kim SB, Kim JG. Reliability of the imaging software in the preoperative planning of the open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. (2015) 23(3):846–51. doi: 10.1007/s00167-013-2700-z
20. Lee OS, Lee ES, Lee YS. Disparity between preoperative target correction amount and postoperative correction amount in open wedge high tibial osteotomy. Knee Surg Relat Res. (2019) 31(2):126–31. doi: 10.5792/ksrr.18.034
21. Kim HJ, Park J, Shin JY, Park IH, Park KH, Kyung HS. More accurate correction can be obtained using a three-dimensional printed model in open-wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc. (2018) 26(11):3452–8. doi: 10.1007/s00167-018-4927-1
22. Ribeiro CH, Severino NR. Moraes de barros fucs PM. Opening wedge high tibial osteotomy: navigation system compared to the conventional technique in a controlled clinical study. Int Orthop. (2014) 38(8):1627–31. doi: 10.1007/s00264-014-2341-y
23. Tardy N, Steltzlen C, Bouguennec N, Cartier JL, Mertl P, Batailler C, et al. Is patient-specific instrumentation more precise than conventional techniques and navigation in achieving planned correction in high tibial osteotomy? Orthop Traumatol Surg Res. (2020) 106(8S):S231–6. doi: 10.1016/j.otsr.2020.08.009
24. Miniaci A, Ballmer FT, Ballmer PM, Jakob RP. Proximal tibial osteotomy. A new fixation device. Clin Orthop Relat Res. (1989) 246:250–9. doi: 10.1097/00003086-198909000-00035
Keywords: open-wedge high tibial osteotomy, solidworks, preoperative planning, correction angle, weight-bearing line ratio
Citation: Lu Y, Wang X, Yang B, Xu Z, Zhang B, Jia B, He J, Qi L, Wang M and Qiao F (2023) Application of SolidWorks software in preoperative planning of high tibial osteotomy. Front. Surg. 9:951820. doi: 10.3389/fsurg.2022.951820
Received: 24 May 2022; Accepted: 27 September 2022;
Published: 6 January 2023.
Edited by:
Tsung-Yuan Tsai, Shanghai Jiao Tong University, ChinaReviewed by:
Chen Zhu, The First Affiliated Hospital of University of Science and Technology of China Anhui Provincial Hospital, China© 2023 Lu, Wang, Yang, Xu, Zhang, Jia, He, Qi, Wang and Qiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Feng Qiao cWlhb2ZlbmdoaHl5QDE2My5jb20=
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.