
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg., 01 August 2022
Sec. Visceral Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.946917
 Yi Jin1,†
Yi Jin1,† Runwen Liu2,†
Runwen Liu2,† Yonghua Chen1
Yonghua Chen1 Jie Liu2
Jie Liu2 Ying Zhao3
Ying Zhao3 Ailin Wei4
Ailin Wei4 Yichuan Li5
Yichuan Li5 Hai Li6
Hai Li6 Jun Xu7
Jun Xu7 Xin Wang1*‡
Xin Wang1*‡ Ang Li1*‡
Ang Li1*‡
Background: The achievement rate of the critical view of safety during laparoscopic cholecystectomy is much lower than expected. This original study aims to investigate and analyze factors associated with a low critical view of safety achievement.
Materials and Methods: We prospectively collected laparoscopic cholecystectomy videos performed from September 2, 2021, to September 19, 2021, in Sichuan Province, China. The artificial intelligence system, SurgSmart, analyzed videos under the necessary corrections undergone by expert surgeons. Also, we distributed questionnaires to surgeons and analyzed them along with surgical videos simultaneously.
Results: We collected 169 laparoscopic cholecystectomy surgical videos undergone by 124 surgeons, among which 105 participants gave valid answers to the questionnaire. Excluding those who conducted the bail-out process directly, the overall critical view of safety achievement rates for non-inflammatory and inflammatory groups were 18.18% (18/99) and 9.84% (6/61), respectively. Although 80.95% (85/105) of the surgeons understood the basic concept of the critical view of safety, only 4.76% (5/105) of the respondents commanded all three criteria in an error-free way. Multivariate logistic regression results showed that an unconventional surgical workflow (OR:12.372, P < 0.001), a misunderstanding of the 2nd (OR: 8.917, P < 0.05) and 3rd (OR:8.206, P < 0.05) criterion of the critical view of safety, and the don't mistake “fundus-first technique” as one criterion of the critical view of safety (OR:0.123, P < 0.01) were associated with lower and higher achievements of the critical view of safety, respectively.
Conclusions: The execution and cognition of the critical view of safety are deficient, especially the latter one. Thus, increasing the critical view of safety surgical awareness may effectively improve its achievement rate.
Minimally invasive surgery is widely implemented in the surgical field owing to its advantages such as smaller incision, less postoperative pain, and shorter recovery time compared with the laparotomy method (1–4). Laparoscopic cholecystectomy (LC) is currently the gold standard for the treatment of symptomatic gallstone (5). The number of surgical patients who underwent LC in the United States is approximately 750,000–1,000,000 yearly (6). Although LC is a simple and routine surgical procedure, previous studies reported that LC is associated with major bile duct injury (BDI) rates of 0.15%–0.36% and an overall biliary complication rate of 1.5% (7–12). BDI significantly affects the quality of life, life expectancy, and financial situation of patients (13–16). Surgeons bear extreme psychological pressure and face the risk of lawsuit from patients (17, 18). Safe cholecystectomy techniques such as critical view of safety (CVS), intraoperative cholangiography, and bail-out have been proposed to decrease the incidence of BDI (6). The Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) consensus and Tokyo Guidelines 2018 indicated that the achievement of CVS is an effective technique for decreasing BDI (19, 20). The findings from retrospective multicenter studies indicated that a routine achievement of CVS could significantly decrease the incidence of BDI to 2 patients in every 1,000,000 people (21–24).
Previous studies reported that CVS was highly feasible (85%–95%) (21–23). However, the actual achievement rate of CVS was significantly lower than expected (25, 26). A survey of 343 samples obtained from American surgeons showed an initial CVS achievement rate of 15.9% (25). Another study conducted in Stanford University, comprising 1,051 videos obtained from 31 surgeons, showed a CVS achievement rate below 10% (26). In order to increase the achievement rate of CVS and decrease the incidence of BDI, Nakazato et al. (27) requested every participating surgeon to perform four LC procedures recorded: twice before and twice after a curriculum focused on CVS, which indicated that a structured curriculum on achieving a quality CVS improved their frequency of achieving CVS during LC. In addition, Mascagni et al. (25) performed a short intraoperative time-out, and the results showed that time-out was associated with an improved CVS achievement rate. Although the application of the above methods had significantly improved the achievement rate of CVS, there were still more than half of LC surgeries without routine CVS. Therefore, it is imperative to comprehensively explore the factors that affect the further improvement of CVS. Nevertheless, due to the complex nature of causes affecting CVS achievement, including both cognitive and executive factors, there is still a lack of this type of study.
Therefore, the current study sought to achieve the following two aims through reviewing and analyzing results obtained from a recently organized multi-institution artificial intelligence–assisted LC video competition: (1) to evaluate the cognition of surgeons in terms of surgical safety from questionnaire and explore the executive status from corresponding surgical videos; (2) to explore factors affecting the achievement of CVS from both cognitive and executive aspects.
A multi-institution LC surgical video competition was launched in the southwest regions of China (Sichuan Province) at the beginning of September 2021. The recruitment criteria for participation were as follows: (1) videos collected prospectively between September 2, 2021, and September 19, 2021; (2) The videos should comprise one and only complete LC procedure; (3) The surgical video used in the competition must be performed by the participant; (4) The videos were further assigned to an inflammatory group or a non-inflammatory group according to the Parkland Grading System (28).
SurgSmart, an intelligent surgical quality control system that could automatically recognize surgical phases, inflammatory status, critical division actions and CVS status, was used to analyze all the participating videos. Three well-trained experts reviewed the results and made necessary corrections on the customized platform (https://www.withai.com/events/202109-completion/) to ensure the accuracy of the analysis results by SurgSmart. Videos with a Parkland score ≥3 were assigned to the inflammatory group, whereas videos with a Parkland score <3 were assigned to the non-inflammatory group. The LC procedure was divided into seven surgical phases—establish access (EA), adhesion lysis (AL), mobilize hepatocystic triangle (MHT), dissect gallbladder from liver bed (DGB), extract the gallbladder (EG), clear the operative region (COR), and idle time (ID)—based on our previous study (29). The ID was defined as the period when the camera was aimed away from the abdomen or indicated no action in the abdomen. CVS was defined by Strasberg et al. (30) for the first time and comprised three criteria, namely, C1 (clearly dissecting the hepatocystic triangle before cutting the cystic duct/artery), C2 (dissecting the lower 1/3 of the cystic plate before cutting the cystic duct/artery), and C3 (before cutting the cystic duct/artery, both structures should be clearly dissected) (31). The score system of CVS is presented in Supplementary Table 1. The CVS status was divided into three classes according to the sum score, namely, achieved (5/6), medium (3/4), and low (0/1/2). Supplementary Figure 1 is an example of the surgical report processed by the SurgSmart algorithm, including Parkland score, the identification of surgical phases, and the evaluation of CVS achievement.
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of West China Hospital of Sichuan University (No. 2022-316).
All participants received a Web-based survey (https://www.wjx.cn/) on September 20, 2021. Each participant had only one chance to respond to the survey, and surgeons who had not responded before September 21, 2021, were excluded. The survey comprised seven modules as presented in the Appendix in the Supplementary file. Module A investigated participants’ cognition on the appropriate time to complete an LC procedure in both easy and difficult conditions. Module B explored the balance between delicacy and efficiency in each of the surgical phases in both conditions. The balance was expressed using a scale of 0–10, with higher scores representing more stress on efficiency. Module C comprised a single-choice question that evaluated the conventional operating order around MHT. Implemental frequency of 10 randomly presented operation guidance were investigated in module D. The surgeons were requested to grade each guidance on a 4-point scale including “never,” “occasional,” “often,” and “always” according to the frequency with which they would apply in daily practice. Modules E and F were designed to evaluate the current knowledge of CVS in different levels. Module E focused on the basic concept of CVS. Then, apart from those who replied that they were unaware of CVS’s basic concept, the other participants were asked to select the exact CVS criteria from ten pieces of guidance relevant to the decrease of BDI in module F. The last module was optional, focusing on the number of BDI that participants had experienced in their career. The content filled in the questionnaire was not included in the final video scoring.
Data were analyzed using IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY) and Microsoft Excel (Microsoft Corp., Redmond, WA). Data were presented as means and percentages. Differences between groups were determined by using the Mann–Whitney U test for numeric or ordinal variables, and using the χ2 test or Fisher’s exact test for categorical variables. The Cohn Bach's alpha of each module was evaluated. Multivariate logistic regression analysis relevant to the status of CVS was performed. In this analysis, variables were screened and selected according to the integration of cognition and execution parameters, and forwarding enrollment was based on the likelihood ratio test results. A P value of <0.05 was considered statistically significant.
ResultsA total of 169 LC surgical videos on procedures performed by 124 surgeons were collected, including 102 videos in the non-inflammatory group and 67 videos in the inflammatory group. Notably, 105 participants gave valid answers to the questionnaire. The participants were recruited from 67 different hospitals in the southwest regions of China.
As shown in Table 1, over 70% of the surgeons enrolled in both groups of the present study were in their 30s, all of whom were males. Attending surgeons accounted for more than 50% of all participants. The post of an attending surgeon is like an intermediate professional title of doctors in China. Attending surgeons are board-certified and capable of operating LC on their own. The results showed that 56.9% of the surgeons in the non-inflammatory group had a caseload of above 200 LC, whereas 65.7% of the surgeons in the inflammatory group had a caseload of above 200 LC. However, there is no significant difference in all baseline characteristics between two groups.
The results on surgical videos for all participants are given in Table 2. The inflammatory group had a significantly longer operation time (from establishing access to extracting the gallbladder and clearing the operative region) (46.98 min vs. 20.91 min, P < 0.001) and a longer surgical phase operation time (except EA) compared with those of the non-inflammatory group. MHT was the longest surgical phase in both groups. Out of the 169 surgical videos, 9 videos performed bail-out process directly; therefore, the other 160 surgical videos were used for subsequent CVS analysis. The overall CVS achievement rates were 18.18% and 9.84% for the non-inflammatory group and the inflammatory group, respectively. Although over 50% of the surgeons in both groups fulfilled the C3 criterion, the achievement rates of C1 and C2 were still low ranging from 11.5% to 27.9%. However, there was no significant difference in CVS achievement between the two groups.
A total of 105 surgeons gave a valid response to the questionnaire. Among them, 39 participants each performed two LC surgical videos, both with and without severe inflammation. The dataset comprised 85 surgeons in the non-inflammatory group and 59 surgeons in the inflammatory group. The Cronbach's alpha of each part of the questionnaire ranged between 0.777 and 0.861 (see Supplementary Table 2).
As shown in Figure 1, most surgeons reported that the estimated duration of LC with severe inflammation should be longer compared with the duration of LC without severe inflammation (58–68 min vs. 25–35 min). The results of delicacy-efficiency scale for different steps indicated that more surgeons preferred efficiency compared with delicacy in secondary surgical steps such as AL, DGB, and EG. Notably, a high number of surgeons chose either a fully efficient or a fully delicate approach when mobilizing the hepatocystic triangle, indicating a more controversial concept among surgeons performing such a critical task.
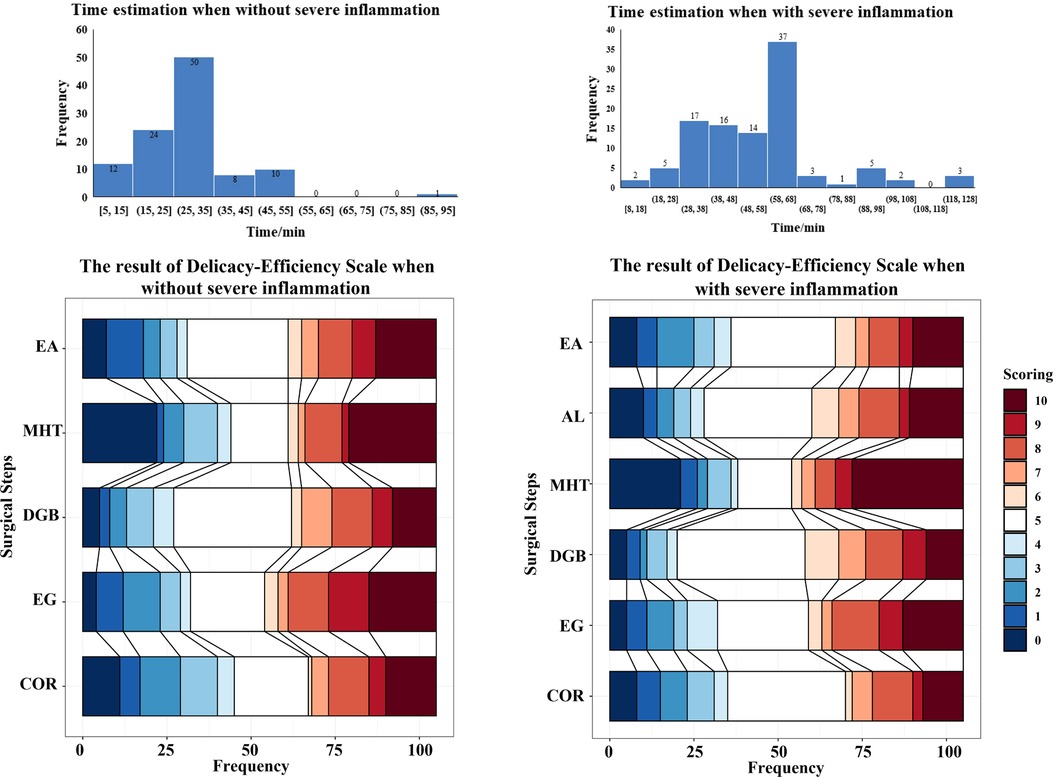
Figure 1. Time estimation and delicacy-efficiency scale. EA, Establish access; AL, adhesion lysis; MHT, mobilize hepatocystic triangle; DGB, dissect gallbladder from liver bed; EG, extract the gallbladder; COR, clear the operative region; the scoring of the Delicacy-Efficiency Scale ranged from 0 to 10, with a higher score (red blocks) representing more stress on efficiency and a lower score (blue blocks) representing delicacy. Five points (white block) represent keeping an equal balance between delicacy and efficiency in a particular step.
Although 80.95% of the surgeons had chosen the right concept of CVS as shown in Figure 2, only very few surgeons (3 in the non-inflammatory group and 3 in the inflammatory group, see Supplementary Table 2) could command all the three criteria in an error-free manner. The results in Figure 2 also showed that 57.14% of the surgeons claimed that they applied the routine surgical workflow that meets the requirement of CVS, whereas 42.86% of the surgeons applied other surgical workflows in daily practice. Further, the surgeons were presented with questions investigating the conventionality of each safety-proof guidance. The results also showed that 77.14% of the surgeons reported that they considered C3 routinely during surgery. However, only 25.71% and 35.24% of the surgeons reported that C2 and C1 were considered routinely during surgery, respectively. And the proportion of participants who routinely considered C2 and C1 during surgery shared similar trend with the proportion of participants harboring corresponding criterion as one of the requirements of achieving CVS (see Figure 2 and Supplementary Table 2).
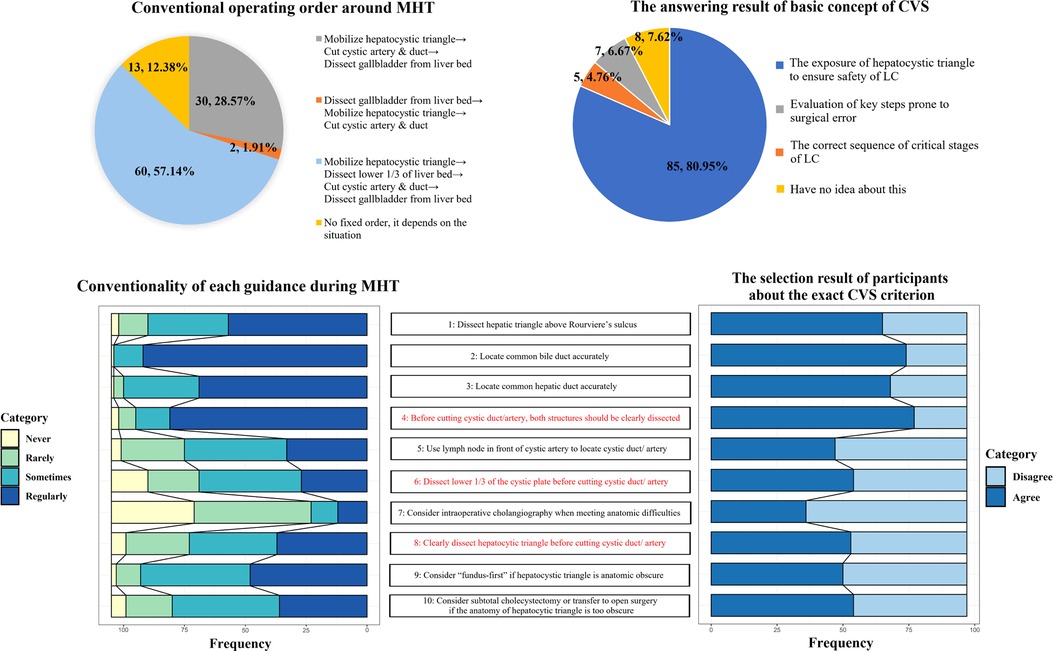
Figure 2. The operation habit and the cognition of CVS of participants. CVS, critical view of safety; MHT, mobilizing hepatocystic triangle; LC, laparoscopic cholecystectomy.
As shown in Figure 3, half of the surgeons (N= 51) who reported the experience of BDI (N = 102) admitted that they had experienced BDI. Details of these data are presented in Supplementary Table 2.
Multivariate logistic analysis through forwarding variant enrollment based on likelihood ratio test results was conducted to explore factors that affect the achievement of CVS. The results showed that unconventional surgical workflow in daily practice (OR: 12.372, P < 0.001) and a misunderstanding of the 2nd (OR: 8.917, P < 0.05) and 3rd (OR: 8.206, P < 0.05) criterion of CVS were associated with a low achievement of CVS (Table 3). Notably, the surgeons who did not choose the “fundus-first technique for hepatocystic triangle in obscure” as one of the CVS criteria had a better achievement of CVS (OR: 0.123, P < 0.01).
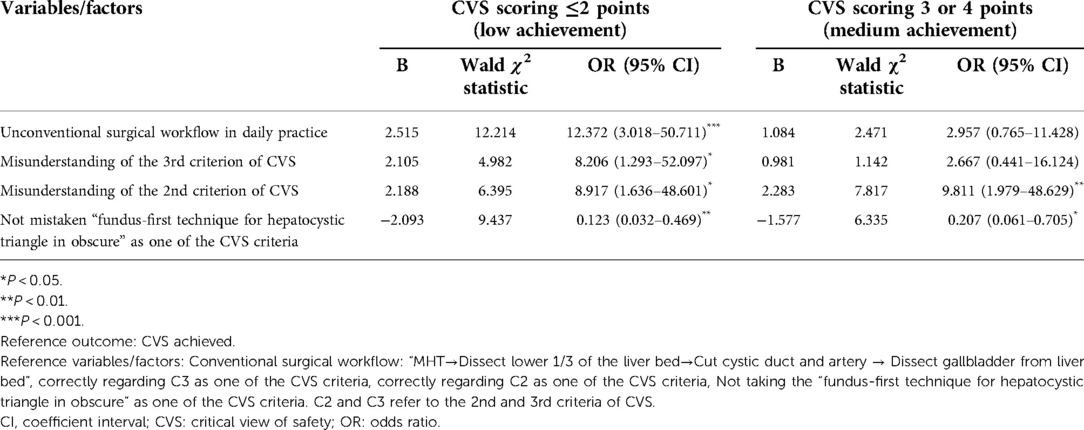
Table 3. Multivariate logistic regression differentiating odd ratio relevant to low achievement of critical view of safety (CVS).
Minimally invasive instruments and techniques have developed quickly; however, the incidence of BDI has not reduced in the present decade. Approximately 49% of surgeons experienced a major BDI in British Columbia, Canada (32). The results of our study indicated that 50% of surgeons had experienced BDI in their career. CVS is an intraoperative exposure technique initially introduced by Strasberg et al. (30) more than two decades ago. Several studies report that CVS is an accessible and effective technique to reduce the incidence of BDI (33–36). However, the achievement rate of CVS was significantly lower than expected and varied significantly in different institutions (25, 26, 37). Few studies have conducted a comprehensive analysis on the causes of low CVS achievement. Therefore, our study sought to explore factors that affect the achievement of CVS from both cognitive and executive aspects, showing that cognitive factors had a more significant effect on CVS compared with executive factors.
Currently, the achievement rate of CVS is not satisfactory. A total of 1,051 LC surgical videos from 31 surgeons were analyzed, and the findings indicated that only 9% cases fulfilled all three criteria of CVS (26). Moreover, no difference in CVS achievement was observed between low-severity cases and high-severity cases (26). Similarly, findings from a surgical improvement study conducted in France indicated an initial CVS achievement rate of 15.9% in 172 cases (25). In addition, the results from an analysis of a prospectively collected data deposited in the LC10000 database seen in Supplementary Figure 2 (https://lc10000.withai.com/) comprising 415 surgical videos showed that the overall achievement rate of CVS in the southwest regions of China was only 5%. In our study, although surgeons submitted surgical videos that they considered good, the actual achievement rates of CVS in the non-inflammatory group and the inflammatory group were 18.18% and 9.84%, respectively. These findings indicated that low achievement of CVS was a global problem, and therefore, further studies should explore ways to improve the achievement rate.
Some institutions have conducted research on surgeons' understanding of CVS, and the findings showed that the correct cognition rate of CVS was very low. A study conducted by Gupta et al. (38) indicated a significant discrepancy between self-cognition and actual cognition of CVS. In this study, most surgeons (88.3%) reported that they knew about CVS but only 11.5% knew about it correctly (38). A survey conducted in South America comprising 446 surgeons showed that the percentage of surgeons who correctly identified all three criteria of CVS was 21.8% (39). A large-sample survey conducted in the Netherlands, where CVS is routinely required during LC, indicated that although 98.2% of the surgeons claimed that they incorporated the CVS technique into daily practice, only 16.9% of the surgeons correctly selected all three criteria of CVS (40). In our study, although 80.95% of the surgeons knew about the basic concept of CVS, only a small percentage of these surgeons (3 in the non-inflammatory group and 3 in the inflammatory group, but one person submitted a video for each of the two groups) could command all three criteria in an error-free way. These findings indicated that the cognition rate of CVS was significantly lower than expected. In addition, the results indicated a significant difference in cognition at various regions/institutions.
In our study, questionnaires and analysis of surgical videos were first combined for in-depth research to explore the association between cognition and execution of CVS during LC. The results from the questionnaires indicated that 79.38% of the surgeons considered C3 as a criterion of CVS. However, only 54.64% of surgeons considered C1 and 55.67% of surgeons considered C2 as criteria of CVS. The results from an analysis of LC videos from these surgeons indicated that the achievement rate of C3 was significantly higher than that of C1 and C2. The results showed that surgeons had significant cognitive differences for each criterion of CVS, and these differences were ultimately reflected in their daily practice. Multivariate regression analysis was conducted in this study based on all parameters from the questionnaire and surgical videos. The results indicated that an incorrect understanding of essential CVS criteria was associated with a low achievement of CVS (scoring ≤2 points). Therefore, improving the cognition of CVS among surgeons may effectively increase the achievement of CVS.
Previous studies reported that education could improve the achievement of CVS. Findings from a previous study comprising 10 surgeons showed that although CVS was adequately achieved (score>4) by only two of the surgeons enrolled in the study initially, training five surgeons significantly increased the quality of CVS (from 1.75 points to 3.75 points, P< 0.05) (41). Nakazato et al. (27) reported that a structured curriculum for safe LC significantly increased the quality and frequency of achieving CVS. The study recommended routine application of this curriculum worldwide to improve the achievement rate of CVS (27). The increase of CVS achievement after education can decrease over time, indicating some decay in knowledge retention over time (42). Wong et al. (42) reported that continued educational interventions should be conducted to enhance long-term retention of knowledge. Moreover, current research on education does not provide regular feedback on the cognition of CVS in surgeons. Therefore, surgeons with a low understanding of CVS after group education should receive more individualized cognitive interventions.
Although education significantly improves the achievement rate of CVS, there are still 18%–58% LC procedures not achieving CVS (27, 43, 44). The effect of education on further improvement of CVS in some countries with high CVS penetration, such as the Netherlands, is very limited (44). Studies are currently exploring other approaches to improve the CVS achievement rate (19, 25, 43, 45–47). Mascagni et al. (25) demonstrated that performing a short intraoperative time-out significantly improved the achievement rate of CVS. Chen CB and colleagues (43) reported that a combination of focused education and intraoperative time-out could improve CVS scores and its knowledge. According to SAGES and other guidelines, indocyanine green is recommended to help avoid bile duct injury in complex situations where dissection is impossible to get a clear CVS view (19, 47). In addition, indocyanine green can also help our AI to identify the bile duct structure and its variation. At present, we are also carrying out some related studies and may combine anatomical recognition with indocyanine green for model optimization in the future. A few studies have reported promising application of AI techniques such as computer vision and deep learning for automated identification of CVS with high accuracy (26, 48–50), which can be utilized as a quality control system in future. These findings indicated that interventions and feedback in surgery were important for improving CVS achievement.
Although our study is the first comprehensive research deeply investigating the status of CVS in China from both cognitive and executive aspects, it has some limitations. First, because it is a voluntary surgical video contest, there is a limit to the sample size. The study has a small sample size and lacks global data, which may not be representative of the overall CVS achievement. Then, there is the Hawthorne effect in the analysis of videos. Surgeons selected surgeries they thought better during the video recruitment period to participate in the competition, so the CVS achievement rate may be higher than usual, which may not fully reflect the actual situation in daily practice. In addition, due to the gap between the number of doctors of different professional titles, the research results can only roughly reflect the overall situation but cannot accurately reflect the CVS completion of doctors of different professional titles. In the near future, we plan to promote SurgSmart to analyze and evaluate the daily practice of surgeons of varied professional titles in a wider range, so we can obtain more comprehensive and objective data.
In summary, low cognition and achievement rate of CVS is a global problem that must be solved. Additionally, cognitive factors have a more significant effect on CVS compared with executive factors. Thus, improving awareness of CVS and accurately grasping the requirement of the three criteria may effectively improve the achievement rate of CVS.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of West China Hospital of Sichuan University (No. 2022-316). The patients/participants provided their written informed consent to participate in this study.
All authors have approved the final article and agreed to be accountable for the content of the work. YJ and RL were mainly involved in the drafting of the article. XW and AL chiefly contributed to the design of the study and gave final approval of the version to be published. YC, JL, and YZ primarily helped with the analysis and interpretation of data. AW, YLi, HL, and JX mainly contributed to the collection of data for providing important intellectual content and performed a critical revision of the manuscript. In conclusion, each author made substantial contributions to this research in different ways. All authors contributed to the article and approved the submitted version.
This work was supported by the Fund of the High-Quality Development of Guang'an People's Hospital (21FZ001), Key Project of Science & Technology Department of Sichuan Province (22ZDYF1920), Regional Innovation Cooperation in Sichuan Province (2022YFQ0068), Science and technology project of Sichuan Province (2021YFS0109) and Union Project of Science & Technology Department of Chongqing(cstc2021jscx-msxmX0011).
The authors express their thanks to Chengdu Withai Innovations Technology Company for providing technical support for this surgical competition.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.946917/full#supplementary-material.
1. de Rooij T, van Hilst J, van Santvoort H, Boerma D, van den Boezem P, Daams F, et al. Minimally invasive versus open distal pancreatectomy (LEOPARD) A multicenter patient-blinded randomized controlled trial. Ann Surg. (2019) 269(1):2–9. doi: 10.1097/sla.0000000000002979
2. Lee W-J, Chan C-P, Wang B-Y. Recent advances in laparoscopic surgery. Asian J Endosc Surg. (2013) 6(1):1–8. doi: 10.1111/ases.12001
3. Nguyen NT, Varela JE. Bariatric surgery for obesity and metabolic disorders: state of the art. Nat Rev Gastroenterol Hepatol. (2017) 14(3):160–9. doi: 10.1038/nrgastro.2016.170
4. Syn NL, Kabir T, Koh YX, Tan HL, Wang LZ, Chin BZ, et al. Survival advantage of laparoscopic versus open resection for colorectal liver metastases a meta-analysis of individual patient data from randomized trials and propensity-score matched studies. Ann Surg. (2020) 272(2):253–65. doi: 10.1097/sla.0000000000003672
5. Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy – the new gold standard. Arch Surg. (1992) 127(8):917–23. doi: 10.1001/archsurg.1992.01420080051008
6. Brunt LM, Deziel DJ, Telem DA, Strasberg SM, Aggarwal R, Asbun H, et al. Safe cholecystectomy multi-society practice guideline and state of the art consensus conference on prevention of bile duct injury during cholecystectomy. Ann Surg. (2020) 272(1):3–23. doi: 10.1097/sla.0000000000003791
7. Schwaitzberg SD, Scott DJ, Jones DB, McKinley SK, Castrillion J, Hunter TD, et al. Threefold increased bile duct injury rate is associated with less surgeon experience in an insurance claims database. Surg Endoscopy Other Intervent Tech. (2014) 28(11):3068–73. doi: 10.1007/s00464-014-3580-0
8. Tornqvist B, Stroemberg C, Akre O, Enochsson L, Nilsson M. Selective intraoperative cholangiography and risk of bile duct injury during cholecystectomy. Br J Surg. (2015) 102(8):952–8. doi: 10.1002/bjs.9832
9. Barrett M, Asbun HJ, Chien H-L, Brunt LM, Telem DA. Bile duct injury and morbidity following cholecystectomy: a need for improvement. Surg Endoscopy Other Intervent Tech. (2018) 32(4):1683–8. doi: 10.1007/s00464-017-5847-8
10. Fong ZV, Pitt HA, Strasberg SM, Loehrer AP, Sicklick JK, Talamini MA, et al. Diminished survival in patients with bile leak and ductal injury: management strategy and outcomes. J Am Coll Surg. (2018) 226(4):568–76. doi: 10.1016/j.jamcollsurg.2017.12.023
11. Lilley EJ, Scott JW, Jiang W, Krasnova A, Raol N, Changoor N, et al. Intraoperative cholangiography during cholecystectomy among hospitalized medicare beneficiaries with non-neoplastic biliary disease. Am J Surg. (2017) 214(4):682–6. doi: 10.1016/j.amjsurg.2017.06.021
12. Pucher PH, Brunt LM, Davies N, Linsk A, Munshi A, Rodriguez HA, et al. Outcome trends and safety measures after 30 years of laparoscopic cholecystectomy: a systematic review and pooled data analysis. Surg Endoscopy Other Intervent Tech. (2018) 32(5):2175–83. doi: 10.1007/s00464-017-5974-2
13. Sharma S, Behari A, Shukla R, Dasari M, Kapoor VK. Bile duct injury during laparoscopic cholecystectomy: an Indian e-survey. Ann Hepatobiliary Pancreat Surg. (2020) 24(4):469–76. doi: 10.14701/ahbps.2020.24.4.469
14. Flum DR, Cheadle A, Prela C, Dellinger EP, Chan L. Bile duct injury during cholecystectomy and survival in medicare beneficiaries. J Am Med Assoc. (2003) 290(16):2168–73. doi: 10.1001/jama.290.16.2168
15. Tornqvist B, Zheng Z, Ye W, Waage A, Nilsson M. Long-term effects of iatrogenic bile duct injury during cholecystectomy. Clin Gastroenterol Hepatol. (2009) 7(9):1013–8. doi: 10.1016/j.cgh.2009.05.014
16. Savader SJ, Lillemoe KD, Prescott CA, Winick AB, Venbrux AC, Lund GB, et al. Laparoscopic cholecystectomy-related bile duct injuries – a health and financial disaster. Ann Surg. (1997) 225(3):268–73. doi: 10.1097/00000658-199703000-00005
17. Dai H-S, Liang L, Zhang C-C, Cheng Z-J, Peng Y-H, Zhang Y-M, et al. Impact of iatrogenic biliary injury during laparoscopic cholecystectomy on surgeon’s mental distress: a nationwide survey from China. HPB (Oxford). (2020) 22(12):1722–31. doi: 10.1016/j.hpb.2020.03.019
18. Alkhaffaf B, Decadt B. 15 Years of litigation following laparoscopic cholecystectomy in England. Ann Surg. (2010) 251(4):682–5. doi: 10.1097/SLA.0b013e3181cc99fd
19. Pucher PH, Brunt LM, Fanelli RD, Asbun HJ, Aggarwal R. SAGES Expert Delphi consensus: critical factors for safe surgical practice in laparoscopic cholecystectomy. Surg Endoscopy Other Intervent Tech. (2015) 29(11):3074–85. doi: 10.1007/s00464-015-4079-z
20. Wakabayashi G, Iwashita Y, Hibi T, Takada T, Strasberg SM, Asbun HJ, et al. Tokyo guidelines 2018: surgical management of acute cholecystitis: safe steps in laparoscopic cholecystectomy for acute cholecystitis (with videos). J Hepatobiliary Pancreat Sci. (2018) 25(1):73–86. doi: 10.1002/jhbp.517
21. Avgerinos C, Kelgiorgi D, Touloumis Z, Baltatzi L, Dervenis C. One thousand laparoscopic cholecystectomies in a single surgical unit using the “critical view of safety” technique. J Gastrointest Surg. (2009) 13(3):498–503. doi: 10.1007/s11605-008-0748-8
22. Sanjay P, Fulke JL, Exon DJ. “Critical view of safety” as an alternative to routine intraoperative cholangiography during laparoscopic cholecystectomy for acute biliary pathology. J Gastrointest Surg. (2010) 14(8):1280–4. doi: 10.1007/s11605-010-1251-6
23. Tsalis K, Antoniou N, Koukouritaki Z, Patridas D, Christoforidis E, Lazaridis C. Open-access technique and “critical view of safety” as the safest way to perform laparoscopic cholecystectomy. Surg Laparosc Endoscopy Percutan Tech. (2015) 25(2):119–24. doi: 10.1097/SLE.0000000000000055
24. Yegiyants S, Collins JC. Operative strategy can reduce the incidence of major bile duct injury in laparoscopic cholecystectomy. Am Surg. (2008) 74(10):985–7. doi: 10.1177/000313480807401022
25. Mascagni P, Rodriguez-Luna MR, Urade T, Felli E, Pessaux P, Mutter D, et al. Intraoperative time-out to promote the implementation of the critical view of safety in laparoscopic cholecystectomy: a video-based assessment of 343 procedures. J Am Coll Surg. (2021) 233(4):497–505. doi: 10.1016/j.jamcollsurg.2021.06.018
26. Korndorffer JR J, Hawn MT, Spain DA, Knowlton LM, Azagury DE, Nassar AK, et al. Situating artificial intelligence in surgery A focus on disease severity. Ann Surg. (2020) 272(3):523–8. doi: 10.1097/sla.0000000000004207
27. Nakazato T, Su B, Novak S, Deal SB, Kuchta K, Ujiki M. Improving attainment of the critical view of safety during laparoscopic cholecystectomy. Surg Endoscopy Other Intervent Tech. (2020) 34(9):4115–23. doi: 10.1007/s00464-019-07178-y
28. Madni TD, Leshikar DE, Minshall CT, Nakonezny PA, Cornelius CC, Imran JB, et al. The Parkland grading scale for cholecystitis. Am J Surg. (2018) 215(4):625–30. doi: 10.1016/j.amjsurg.2017.05.017
29. Cheng K, You J, Wu S, Chen Z, Zhou Z, Guan J, et al. Artificial intelligence-based automated laparoscopic cholecystectomy surgical phase recognition and analysis. Surg Endoscopy Other Intervent Tech. (2022) 36(5):3160–8. doi: 10.1007/s00464-021-08619-3
30. Strasberg SM, Hertl M, Soper NJ. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg. (1995) 180(1):101–25. PMID: 8000648
31. Strasberg SM, Brunt LM. Rationale and use of the critical view of safety in laparoscopic cholecystectomy. J Am Coll Surg. (2010) 211(1):132–8. doi: 10.1016/j.jamcollsurg.2010.02.053
32. Francoeur JR, Wiseman K, Buczkowski AK, Chung SW, Scudamore CH. Surgeons’ anonymous response after bile duct injury during cholecystectomy. Am J Surg. (2003) 185(5):468–75. doi: 10.1016/s0002-9610(03)00056-4
33. Sgaramella LI, Gurrado A, Pasculli A, de Angelis N, Memeo R, Prete FP, et al. The critical view of safety during laparoscopic cholecystectomy: strasberg yes or No? An Italian Multicentre study. Surg Endoscopy Other Intervent Tech. (2021) 35(7):3698–708. doi: 10.1007/s00464-020-07852-6
34. Kaya B, Fersahoglu MM, Kilic F, Onur E, Memisoglu K. Importance of critical view of safety in laparoscopic cholecystectomy: a survey of 120 serial patients, with no incidence of complications. Ann Hepatol Biliary-Pancreat Surg. (2017) 21(1):17–20. doi: 10.14701/ahbps.2017.21.1.17
35. Derici S, Degirmenci AK, Cevlik AD. Safe surgery in laparoscopic cholecystectomy. Haseki Tip Bul-Med Bull Haseki. (2017) 55(3):235–8. doi: 10.4274/haseki.87587
36. Heistermann HP, Tobusch A, Palmes D. Prevention of bile duct injuries after laparoscopic cholecystectomy. “the critical view of safety”. Zentralbl Chir. (2006) 131(6):460–5. doi: 10.1055/s-2006-957031
37. Booij KAC, de Reuver PR, Nijsse B, Busch ORC, van Gulik TM, Gouma DJ. Insufficient safety measures reported in operation notes of complicated laparoscopic cholecystectomies. Surgery. (2014) 155(3):384–9. doi: 10.1016/j.surg.2013.10.010
38. Gupta V, Lal P, Vindal A, Singh R, Kapoor VK. Knowledge of the culture of safety in cholecystectomy (COSIC) among surgical residents: do we train them well for future practice? World J Surg. (2021) 45(4):971–80. doi: 10.1007/s00268-020-05911-6
39. Gimenez ME, Houghton EJ, Zeledon ME, Palermo M, Acquafresca P, Finger C, et al. The critical view of safety prevents the appearance of biliary injuries? Analysis of a survey. Abcd-Arq Bras Cir Dig Braz Arch Dig Surg. (2018) 31(2):e1380. doi: 10.1590/0102-672020180001e1380
40. van de Graaf FW, van den Bos J, Stassen LPS, Lange JF. Lacunar implementation of the critical view of safety technique for laparoscopic cholecystectomy: results of a nationwide survey. Surgery. (2018) 164(1):31–9. doi: 10.1016/j.surg.2018.01.016
41. Stefanidis D, Chintalapudi N, Anderson-Montoya B, Oommen B, Tobben D, Pimentel M. How often do surgeons obtain the critical view of safety during laparoscopic cholecystectomy? Surg Endosc Other Interv Tech. (2017) 31(1):142–6. doi: 10.1007/s00464-016-4943-5
42. Wong HJ, Kojima Y, Su B, Attaar M, Wu H, Campbell M, et al. Long-term retention after structured curriculum on attainment of critical view of safety during laparoscopic cholecystectomy for surgeons. Surgery. (2022) 171(3):577–83. doi: 10.1016/j.surg.2021.08.063
43. Chen CB, Palazzo F, Doane SM, Winter JM, Lavu H, Chojnacki KA, et al. Increasing resident utilization and recognition of the critical view of safety during laparoscopic cholecystectomy: a pilot study from an academic medical center. Surg Endosc Other Interv Tech. (2017) 31(4):1627–35. doi: 10.1007/s00464-016-5150-0
44. Nijssen MAJ, Schreinemakers JMJ, van der Schelling GP, Crolla RMPH, Rijken AM. Improving critical view of safety in laparoscopic cholecystectomy by teaching interventions. J Surg Educ. (2016) 73(3):442–7. doi: 10.1016/j.jsurg.2015.11.015
45. Honda G, Iwanaga T, Kurata M, Watanabe F, Satoh H, Iwasaki K-i. The critical view of safety in laparoscopic cholecystectomy is optimized by exposing the inner layer of the subserosal layer. J Hepatobiliary Pancreat Surg. (2009) 16(4):445–9. doi: 10.1007/s00534-009-0060-3
46. Cardenas G, Fornaguera I, Diaz del Gobbo R, Ginesta C. Direct gallbladder indocyanine green injection technique to achieve critical view of safety in laparoscopic cholecystectomy. Cir Esp. (2021) 99(9):678–82. doi: 10.1016/j.ciresp.2020.12.020
47. Wang X, Teh CSC, Ishizawa T, Aoki T, Cavallucci D, Lee S-Y, et al. Consensus guidelines for the use of fluorescence imaging in hepatobiliary surgery. Ann Surg. (2021) 274(1):97–106. doi: 10.1097/sla.0000000000004718
48. Mascagni P, Vardazaryan A, Alapatt D, Urade T, Emre T, Fiorillo C, et al. Artificial intelligence for surgical safety: automatic assessment of the critical view of safety in laparoscopic cholecystectomy using deep learning. Ann Surg. 2022 275(5):955–61. doi: 10.1097/sla.0000000000004351
49. Mascagni P, Fiorillo C, Urade T, Emre T, Yu T, Wakabayashi T, et al. Formalizing video documentation of the critical view of safety in laparoscopic cholecystectomy: a step towards artificial intelligence assistance to improve surgical safety. Surg Endosc Other Interv Tech. (2020) 34(6):2709–14. doi: 10.1007/s00464-019-07149-3
Keywords: laparoscopic cholecystectomy (LC), critical view of safety (CVS), cognition, execution, surgical safety
Citation: Jin Y, Liu R, Chen Y, Liu J, Zhao Y, Wei A, Li Y, Li H, Xu J, Wang X and Li A (2022) Critical view of safety in laparoscopic cholecystectomy: A prospective investigation from both cognitive and executive aspects. Front. Surg. 9:946917. doi: 10.3389/fsurg.2022.946917
Received: 18 May 2022; Accepted: 11 July 2022;
Published: 1 August 2022.
Edited by:
Peter C Ambe Universität Witten/Herdecke, GermanyReviewed by:
Alexander Reinisch, University of Giessen, Germany© 2022 Jin, Liu, Chen, Liu, Zhao, Wei, Li, Li, Xu, Wang and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ang Li YW5nbGlAc2N1LmVkdS5jbg== Xin Wang d2FuZ3hpbkB3aXRoYWkuY29t
†These authors have contributed equally to this work and share first authorship.
‡These authors have contributed equally to this work
Specialty Section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
Abbreviations: AL, adhesion lysis; BDI, bile duct injury; COR, clear the operative region; CVS, critical view of safety; DGB, dissect gallbladder from liver bed; EA, establish access; EG, extract the gallbladder; ID, idle time; LC, laparoscopic cholecystectomy; MHT, mobilize hepatocystic triangle.
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.