- The Department of Orthopedics, Beijing Chaoyang Hospital, Capital Medical University, Beijing, China
Background: Irreparable rotator cuff tears (IRCT) are defined as defects that cannot be repaired due to tendon retraction, fat infiltration, or muscle atrophy. One surgical remedy for IRCT is superior capsular reconstruction (SCR), which fixes graft materials between the larger tuberosity and the superior glenoid.
Patients and methods: The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) criteria were followed for conducting the systematic review and meta-analysis. From their inception until February 25, 2022, Pubmed, Embase, and Cochrane Library's electronic databases were searched. Studies using cadavers on SCR for IRCT were also included. The humeral head's superior translation and subacromial peak contact pressure were the primary outcomes. The humeral head's anteroposterior translation, the kind of graft material used, its size, and the deltoid load were the secondary outcomes.
Results: After eliminating duplicates from the search results, 1,443 unique articles remained, and 20 papers were finally included in the quantitative research. In 14 investigations, the enhanced superior translation of the humeral head was documented in IRCTs. In 13 studies, a considerable improvement following SCR was found, especially when using fascia lata (FL), which could achieve more translation restraints than human dermal allograft (HDA) and long head of bicep tendon (LHBT). Six investigations reported a subacromial peak contact pressure increase in IRCTs, which could be rectified by SCR, and these studies found a substantial increase in this pressure. The results of the reduction in subacromial peak contact pressure remained consistent regardless of the graft material utilized for SCR. While there was a statistically significant difference in the change of graft material length between FL and HDA, the change in graft material thickness between FL and HDA was not significant. The humeral head's anterior-posterior translation was rising in IRCTs and could be returned to its original state with SCR. In five investigations, IRCTs caused a significant increase in deltoid force. Furthermore, only one study showed that SCR significantly decreased deltoid force.
Conclusion: With IRCT, SCR might significantly decrease the glenohumeral joint's superior and anterior-posterior stability. Despite the risks for donor-site morbidity and the longer recovery time, FL is still the best current option for SCR.
Introduction
Irreparable rotator cuff tears (IRCT) are defined as defects that cannot be completely repaired due to tendon retraction, fat infiltration, or muscle atrophy (1–4). These defects present a significant challenge to shoulder surgeons who attempt to fully repair the tearing tendons (5–7). Due to abnormal superior humeral head translation and narrowing of the subacromial space, IRCT may result in functional deficits and/or pain in patients (8–10), which can cause severe pain, loss of function, reduced range of motion, and affect patients' quality of life (11–14).
Recently, superior capsular reconstruction (SCR), which was first reported as a surgical alternative to IRCT by Mihata in 2013, has been used (15). The graft was utilized in this surgical surgery to adhere laterally to the larger tuberosity and medially to the superior glenoid. The graft's biomechanical function was as a static stabilizer that diminishes the pressure at the subacromial contact pressure and prevents superior translation of the humeral head (16, 17). As a new arthroscopic technique, the selection of graft materials was disputed (18–20). SCR with fascia lata(FL) showed a significant reduction in pain and functional improvements, such as range of motion, and rates of return to work and sports (21–23). Despite these good results, donor-site morbidity and prolonged surgical time concern many surgeons (24–26). Therefore, several alternative grafts have been applied, such as the long head of the bicep tendon(LHBT), human dermal allograft(HDA), xenograft, and synthetic graft materials (27–34). However, which graft material is optimal for SCR is still subject to debate.
Therefore, we conducted a systematic review and meta-analysis to:
(1) review the literature regarding biomechanical outcomes of SCR for IRCT; (2) compare the biomechanical outcomes of various grafts used in SCR.
Materials and methods
The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) standards were followed in conducting the systematic review and meta-analysis (35). The review followed the methods recommended by the Cochrane Handbook for Systematic Reviews of Interventions (36). There has never been a protocol for systematic reviews or meta-analyses, as far as we are aware.
Eligibility criteria
Research was taken into consideration for review if it met the following inclusion criteria:
• Cadaveric study
• Undergoing SCR for IRCT
• Reporting biomechanical outcomes: The primary outcomes were superior translation of humeral head and subacromial peak contact pressure. Secondary outcomes included anteroposterior translation of humeral head, the type of grafts, the side of grafts and deltoid load.
Exclusion criteria:
• Studies involving animals or operative techniques
• Duplicates and relevant research
• Case reports
• Full text not available
• Non-English articles
Search strategy
From their inception until February 25, 2022, the electronic databases of Pubmed, Embase, and Cochrane Library were searched. The terms “"Superior capsular reconstruction” OR “superior capsule reconstruction” OR “irreparable rotator cuff"” were utilized as the search strategy and appeared in the title, abstract, or keywords fields. In case any were overlooked by the initial search, all references in the included studies were cross-referenced for inclusion by two authors (ZX and JJ).
Trial selection
After duplicates were eliminated, all records' titles and abstracts were initially reviewed by ZX and JJ. Each potentially suitable article's whole text was examined, and disagreements were settled by a third independent reviewer (ZB).
Data extraction
Two reviewers (ZX and JJ) separately compiled trial information (year of publication, nation of origin, and number of samples), intervention and control features, as well as primary and secondary outcome data, by using a standardized data extraction form. When more information was necessary, trial authors were contacted.
Risk of bias assessment
Potential publication bias was examined using contour enhanced funnel plots and Egger's regression test using RStudio software version 2021.09.2(R Foundation for Statistical Computing, Vienna, Austria).
Methodological risk of bias of studies was performed through a checklist proposed by Towns and Black (37). The recommended scoring criteria was maintained, resulting in a total of 26 items with a possible maximum score range of 0 to 26, with higher scores indicating a reduced risk of bias.
Statistical analysis
All subjects' and outcome parameters' weighted means and standard deviations were computed for continuous data. By comparing to the IRCT as a shared control, standard mean differences between the SCR groups and the intact rotator cuff groups were calculated.
All statistical analyses were conducted by the Meta package as part of RStudio software version 2021.09.2(R Foundation for Statistical Computing, Vienna, Austria). A random effects model was used in a meta-analysis to aggregate outcome measures from various studies. As summary statistics, relative risks (RR) with matching 95% confidence intervals were applied. For superior translation of the humeral head, subacromial peak contact pressure, graft material size, and deltoid load, forest plots were made. The various grafts were to be the subject of a subgroup analysis. If the I2 statistic was higher than 50% or the p-value for the Chi2 statistic was less than 0.05, statistical heterogeneity was deemed to be significant. Results of individual trials were presented in cases where meta-analysis was not feasible.
Results
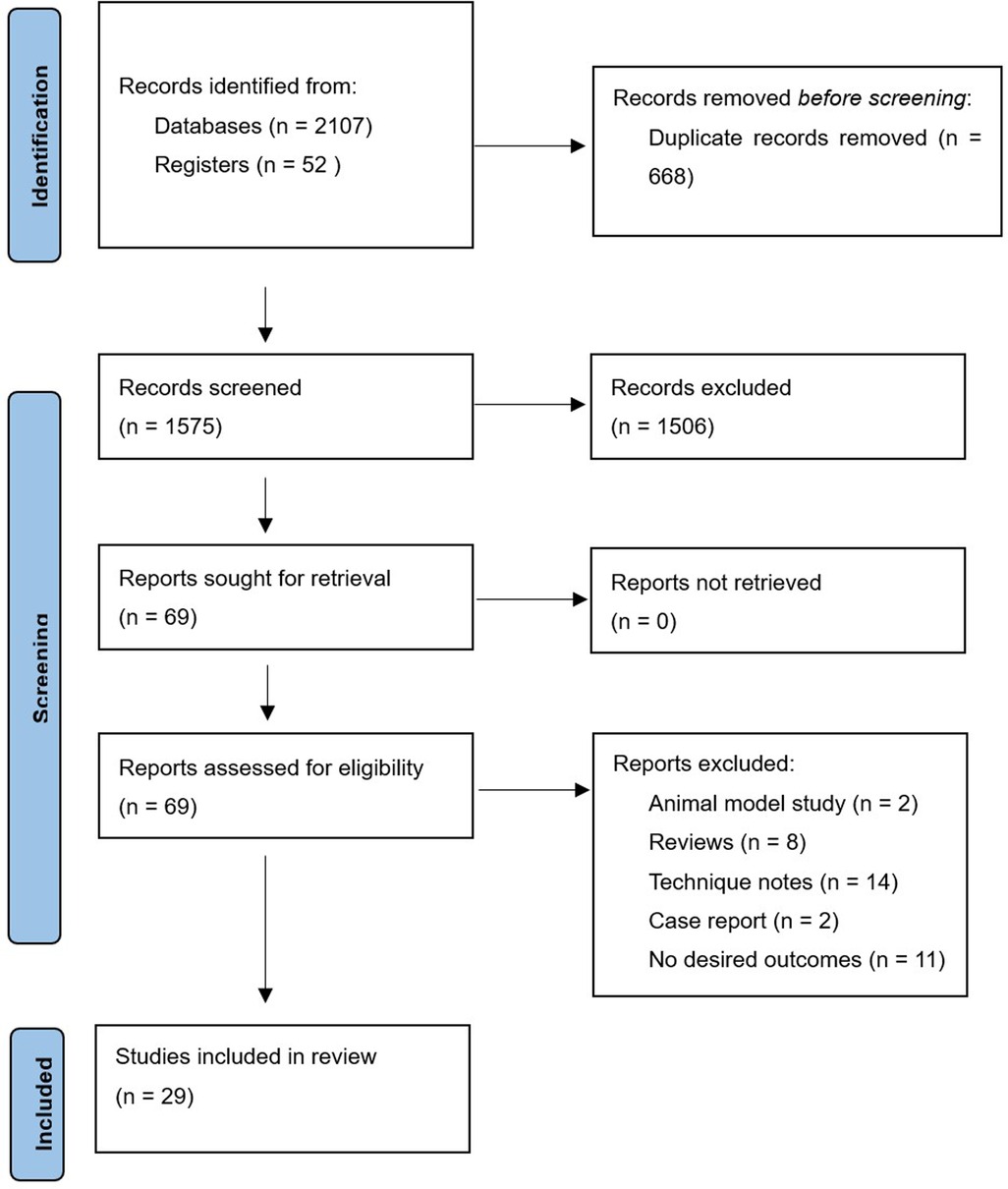
After duplicates were removed, the initial search produced 1,575 original items, of which 69 were thought to be potentially eligible. In the final analysis, 29 cadaveric investigations were considered (8, 15, 17, 21, 27, 38–61). Figure 1 illustrates the flow diagram.
Characteristics of included trials are summarized in Table 1. The 29 trials that were featured were published between 2012 and 2022. The listed studies' sample sizes range from 5 to 15 people. Every study made use of dissected, soft tissue-free cadaveric shoulders for the shoulders. The capsule, coracoacromial ligament, four rotator cuff tendons, pectoralis major tendinous insertion, latissimus dorsi, and three deltoid heads were all still there. However, the loading conditions used in these investigations varied significantly. Of these, 20 studies achieved the balanced system: deltoid, 40N; pectoralis major, 20N; latissimus dorsi, 20N; supraspinatus, 10N; subscapularis, 10N; infraspinatus, 5N; teres minor, 5N. The unbalanced loading condition was achieved by removing the loads from latissimus dorsi and pectoralis major, and added an additional 40N to the deltoid. Two studies reduced deltoid load by half (balanced system: 20N; unbalanced system: 40N) (49, 52). The loading conditions were not properly displayed in the other six experiments (46–48, 51, 53, 56). Therefore, only 20 studies were involved in the quantitative research (8, 15, 17, 21, 27, 38–45, 50, 54, 55, 57–60).
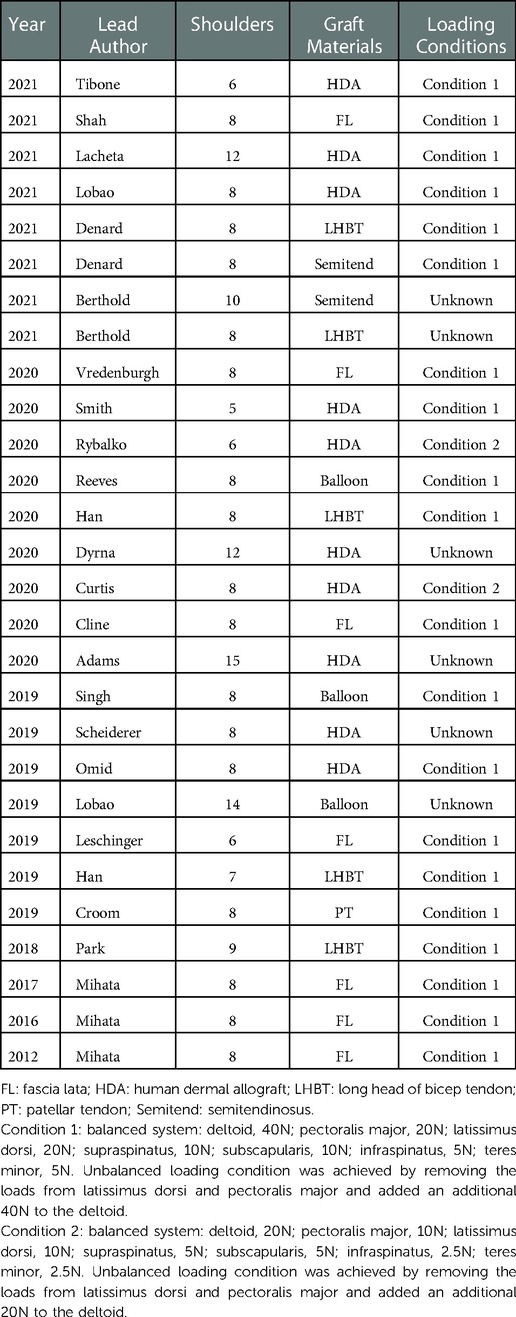
Superior translation of humeral head
Superior translation of humeral head was reported in 15 studies (15, 17, 21, 27, 38, 40, 41, 43–45, 50, 55, 58–60). In 14 studies, a significant increase was found in superior translation of the humeral head after establishing an irreparable rotator cuff tear, except in the Han study (27). In addition, 13 studies—all except the Denard study (45)— found a significant improvement in the superior translation of the humeral head following SCR. Of these, 10 studies reported that superior translation could be restored to intact rotator cuff by SCR (15, 17, 21, 27, 40, 41, 44, 55, 58, 60). One study reported lower superior translation after SCR, compared to intact rotator cuff (59). The standard mean difference between intact rotator cuff and IRCT was −4.49 (95% CI [−5.27;-3.71], I2 = 95%, p < 0.01). For SCR vs. intact and IRCT vs. SCR, the standard mean difference was −1.14 (SCR vs. intact, 95% CI [−2.07;−0.22], I2 = 99%, p < 0.01) and 3.33 (IRCT vs. SCR, 95% CI [2.434;4.33], I2 = 98%, p < 0.01), respectively (Figures 2A–C).
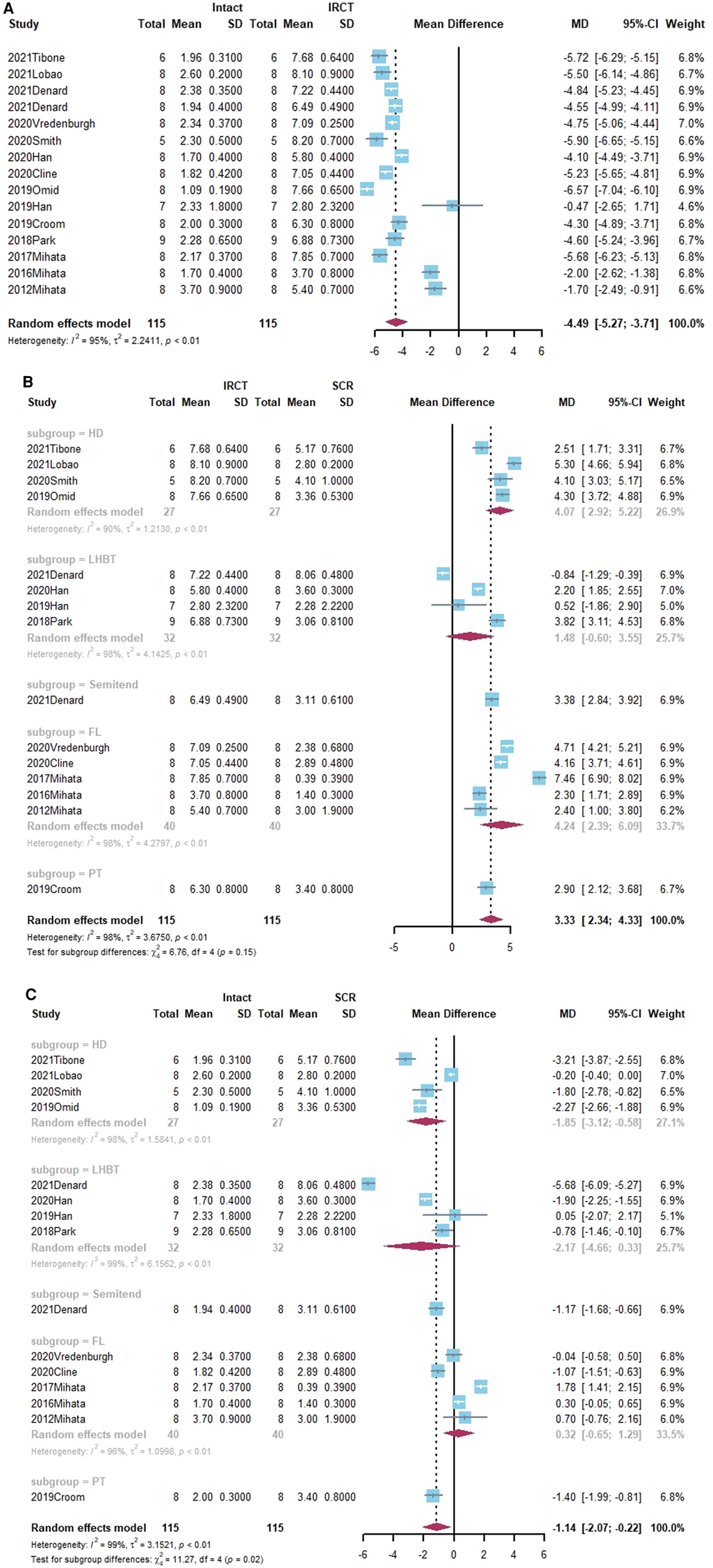
Figure 2. (A) forest plot comparing the mean difference (MD) of superior translation of humeral head between intact cuff and IRCT. (B) Forest plot comparing the mean difference (MD) of superior translation of humeral head between IRCT and SCR. (C) Forest plot comparing the mean difference (MD) of superior translation of humeral head between Intact cuff and SCR.
In a subgroup analysis, SCR with FL achieved superior translation more closed to Intact cuff (MD = 0.32, 95% CI [-0.65;1.29]). The superior translation after SCR with HDA or LHBT was slightly greater than Intact cuff (HD: MD = −1.85, 95% CI [−3.12;−0.58]; LHBT: MD = −2.17, 95% CI [−4.66;0.33]). Meanwhile, the difference between FL and other grafts was statistically significant (X2 = 11.27, p = 0.02).
Subacromial peak contact pressure
Subacromial peak contact pressure was reported in 12 studies (21, 27, 38–41, 44, 45, 55, 58–60). Of these, six studies noted a marked increase in subacromial peak contact pressure following the appearance of the irreparable rotator cuff tear (21, 39–41, 59, 60). All studies restored subacromial peak contact after SCR. The standard mean difference among intact rotator cuff, IRCT, and SCR was −483.98 (Intact vs. IRCT, 95% CI [−656.46;−311.5], I2 = 96%, p < 0.01), 37.15 (Intact vs. SCR, 95% CI [-145.56; 219.85], I2 = 98%, p < 0.01) and 519.28 (IRCRT vs. SCR, 95% CI [298.83;739.73], I2 = 98%, p < 0.01) respectively (Figures 3A–C).
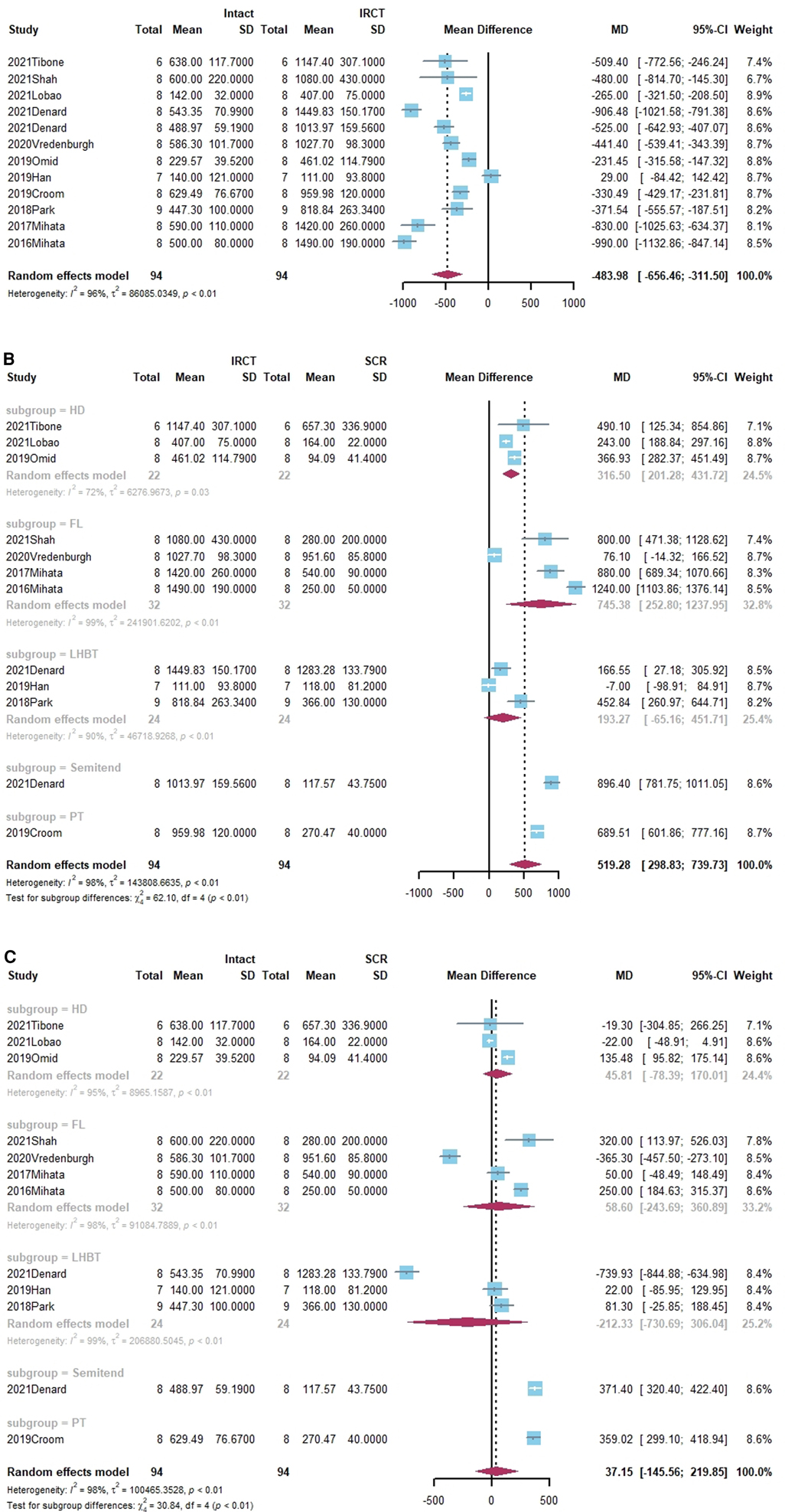
Figure 3. (A) Forest plot comparing the mean difference (MD) of subacromial peak contact pressure between Intact cuff and IRCT. (B) Forest plot comparing the mean difference (MD) of subacromial peak contact pressure between IRCT and SCR. (C) Forest plot comparing the mean difference (MD) of subacromial peak contact pressure between Intact cuff and SCR.
According to a subgroup analysis, the subacromial peak contact pressure may be brought back to the same level as the intact cuff regardless of the type of grafts utilized for SCR.
The size of grafts
Four studies reported on the size of grafts (38, 39, 43, 59). Of these, three studies presented both grafts thickness and lengths (39, 43, 59). In a subgroup analysis, there was no statistically significant difference between HDA and FL in terms of the change in graft thickness. (x2 = 0.83, p = 0.36). While the change in length of FL was substantially smaller than that of HD in terms of grafts (x2 = 17.87, p < 0.01). Shown in Figures 4A,B.
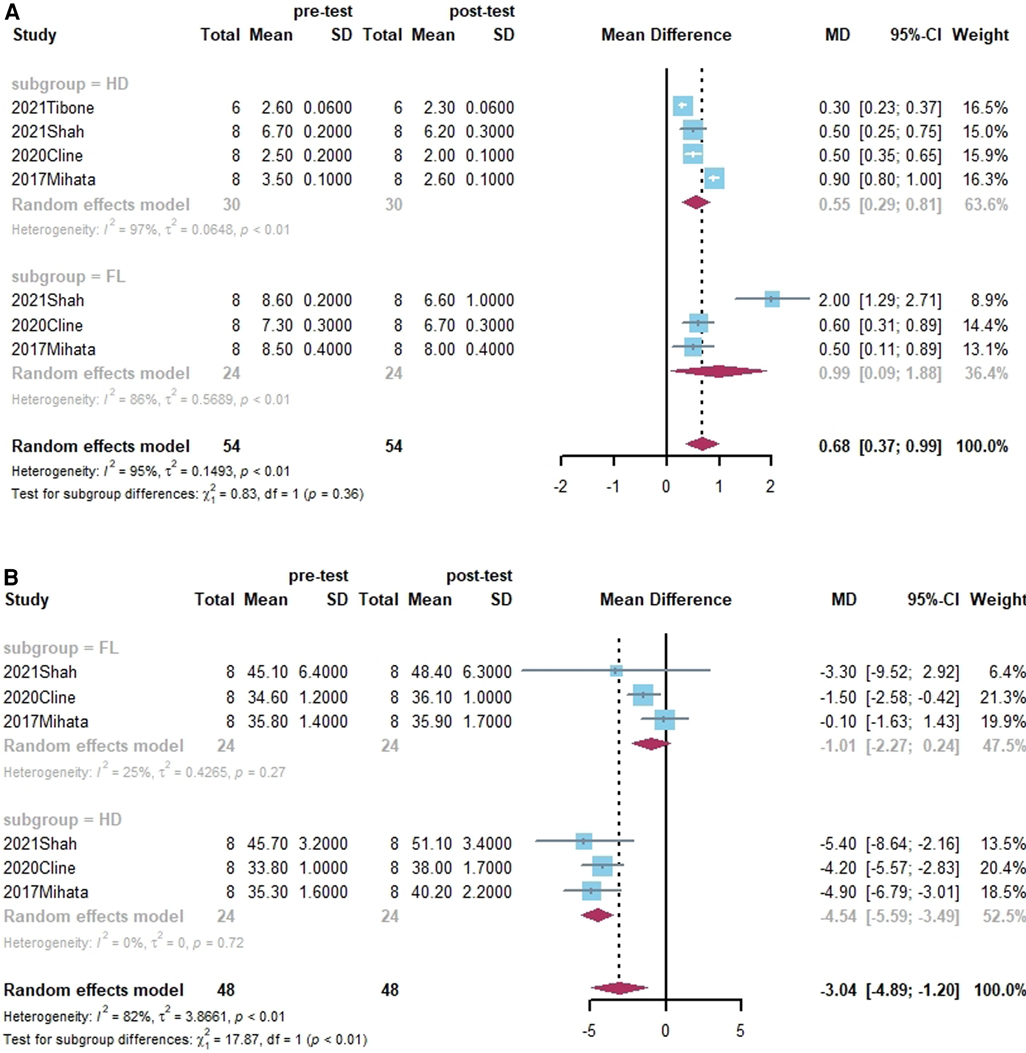
Figure 4. (A) Forest plot comparing the mean difference (MD) of thickness of graft materials in pre- and post-test. (B) Forest plot comparing the mean difference (MD) of length of graft materials in pre- and post-test.
Anteroposterior translation of humeral head
Anteroposterior translation of the humeral head was described in four studies overall (38, 40, 41, 55). Of these, three studies found that, following the occurrence of the irreparable rotator cuff tear, the posterior translation of humeral head was significantly increased, and could be returned to the level of Intact cuff after SCR (38, 41, 55). Shown in Figures 5A–C.
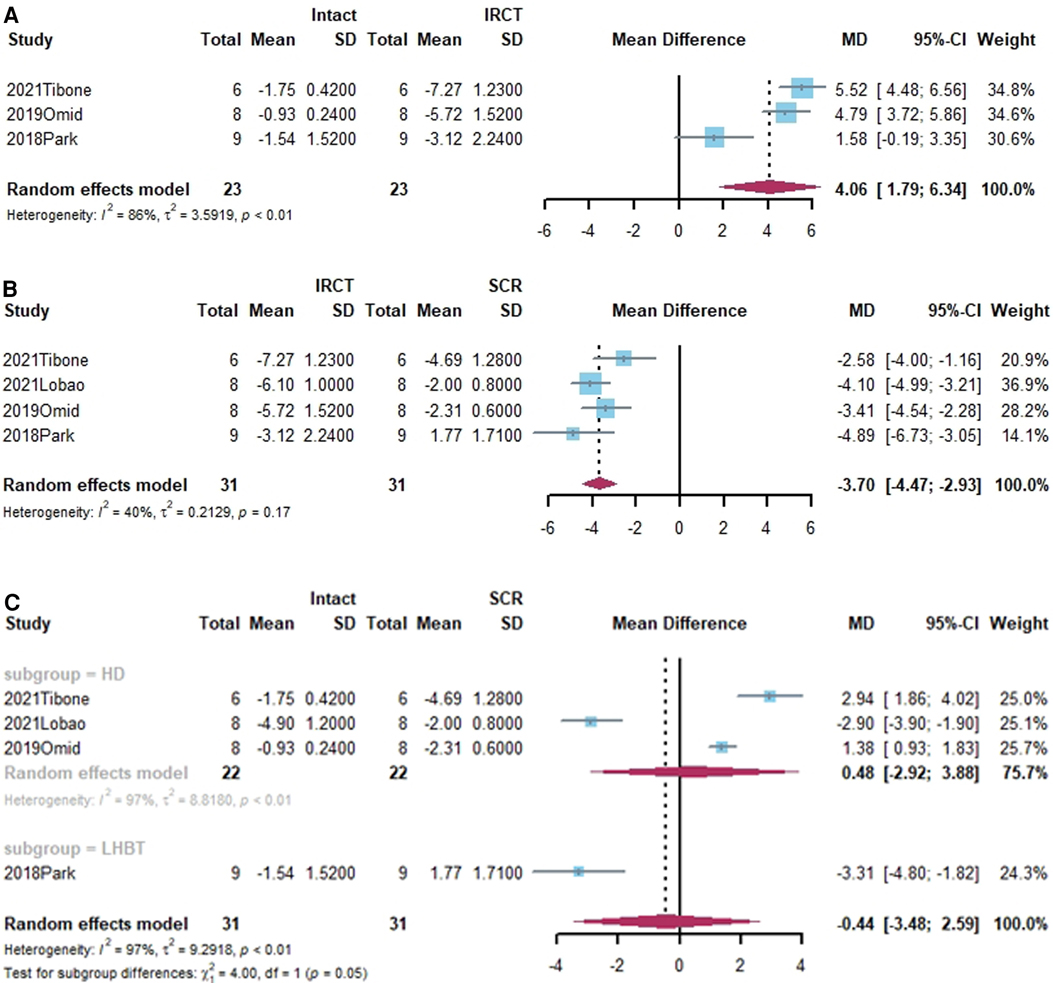
Figure 5. (A) Forest plot comparing the mean difference (MD) of antero-posterior translation of humeral head between Intact cuff and IRCT. (B) Forest plot comparing the mean difference (MD) of antero-posterior translation of humeral head between IRCT and SCR. (C) Forest plot comparing the mean difference (MD) of antero-posterior translation of humeral head between Intact cuff and SCR.
Deltoid force
Five studies reported on deltoid force (46–48, 51, 53). Because the loading circumstances were not disclosed in any of the five studies, a qualitative analysis was done. In all five studies, the establishment of the IRCT resulted in a considerable increase in deltoid force relative to the intact cuff. Only one study found that deltoid force had considerably improved following SCR (46). Meanwhile, all studies reported that deltoid force after SCR was not as low as that of intact cuff (Figures 6A–C).
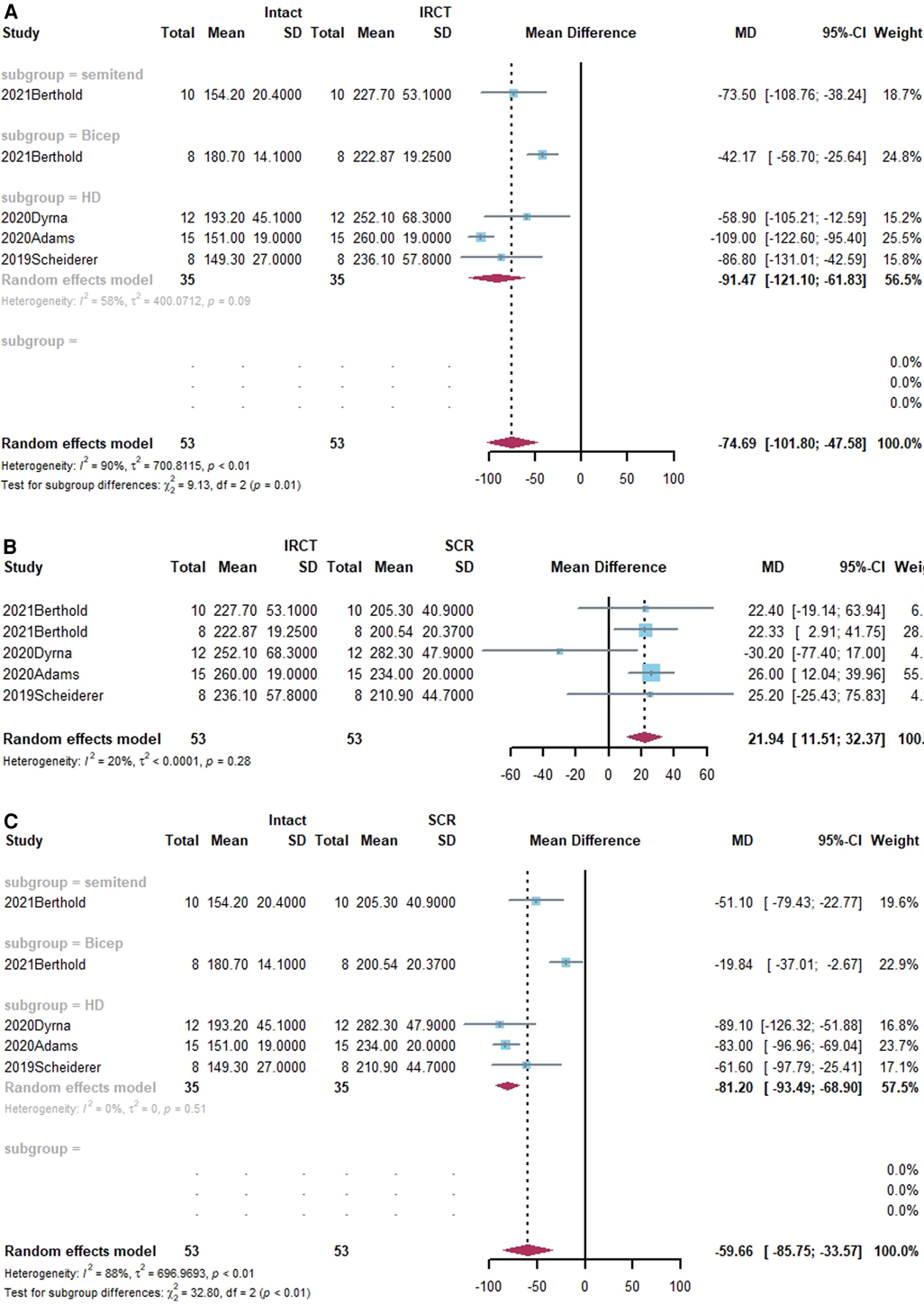
Figure 6. (A) Forest plot comparing the mean difference (MD) of deltoid force between Intact cuff and IRCT. (B) Forest plot comparing the mean difference (MD) of deltoid force between IRCT and SCR. (C) Forest plot comparing the mean difference (MD) of deltoid force between Intact cuff and SCR.
Risk of publication bias
Egger's regression test demonstrated no evidence of publication bias for superior translation of humeral head (t = 1.01, p = 0.329), and subacromial peak contact pressure (t = −1.53, p = 0.157). The funnel plots demonstrated no evidence of publication bias for the size of grafts, anteroposterior translation of humeral head, and deltoid force. The funnel plots are shown in Figure 7.
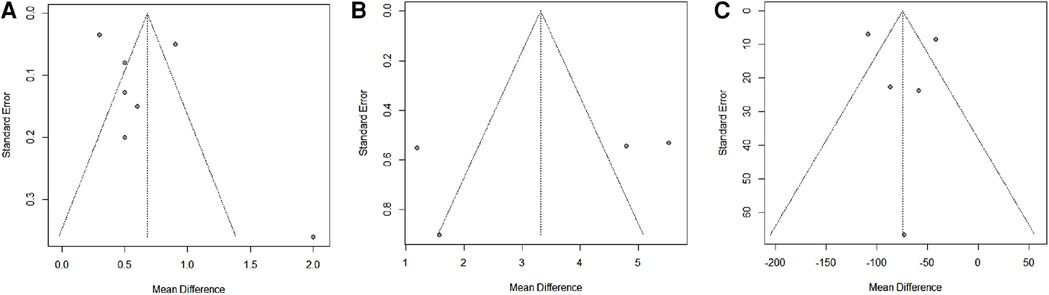
Figure 7. The funnel plots for the size of grafts (A), anteroposterior translation of humeral head (B), and deltoid force (C).
Risk of methodological bias
Out of a possible maximum of 26 points, the mean risk of bias score across studies was 12.03, SD = 1.68 (range = 9 to 14). Lack of blind procedure was common in these studies.
Discussion
In this systematic review and meta-analysis, we discovered that SCR with FL, in comparison to HDA and LHBT, achieved better results in terms of restricting superior translation of humeral head and graft deformation. However, all of the studies included in this meta-analysis used cadavers, which is the IV-level of evidence-based medicine.
The large majority of studies showed that IRCT increased the superior translation of the humeral head, which suggests that the superior capsule, along with dynamic strengthening of the rotator cuff, is an essential static stabilizer that prevents superior translation of the humeral head (10, 62). SCR with FL, however, was able to achieve a level of humeral head translation that was closer to that of an intact cuff when compared to SCR with HDA and LHBT, and this may be due to the different graft thickness (43, 48, 60, 63). It is crucial to remember that the improved translation was not restored to its original state regardless of the graft materials employed for SCR.
In line with our findings, IRCT may also cause subacromial impingement by raising the subacromial contact pressure. Subacromial contact pressure was significantly reduced after SCR and nearly returned to its original level. With these two enhancements, SCR for IRCT could improve the functional outcomes and restore the biomechanical outcomes, as seen in the clinical studies (39, 45, 58, 59).
The stability of the glenohumeral joint, which is crucial for shoulder function and elevation, is indicated by the humeral head's anteroposterior location within the glenoid (64, 65). In our study, the humeral head was seen to move posteriorly following IRCT. SCR was able to center the humeral head in the glenoid and successfully restore the integrity of the capsule. Therefore, by recreating concavity compression, the humeral head might be fixed to the glenoid.
One of the most crucial elements affecting SCR is graft. Since SCR was used, numerous grafts have been developed for greater biomechanical properties and lower prices. The most frequent are LHBT, HDA, and FL grafts. According to our research, HDA is less effective than FL at limiting the superior translation of the humeral head at the same graft fixation angle. Additionally, SCR with LHBT had less effect on limiting humeral head superior translation as compared to FL and HDA, which may be related to the LHBT's insufficient thickness and flatness, which, in turn, may be a factor in the “spacer” effects. Additionally, during the same mechanical test cycles, HDA deformed more than FL, which explains why SCR will eventually fail.
Makovicka et al. (20) conducted a systematic review of biomechanical outcomes by graft type. However, this study only included eight studies, and five of these were conducted by the same author. Besides, only comparison between fascia lata allograft and dermal allograft was analyzed. Our study is the first systematic evaluation and meta-analysis of several grafts for SCR that we are aware of. Biomechanical studies illustrated that FL has the highest biomechanical efficiency when compared to HDA and LHBT, which serves as a reminder that new graft materials need to be investigated since they need to be less expensive, more robust, and more biocompatible. Following the biomechanical outcomes, LHBT was shown not to be a suitable graft for SCR, although there are various surgical procedures that use LHBT. The limitations of this review relate to: (1) In our study, the effectiveness of each graft material was examined only from the perspective of biomechanics; clinical results were not taken into account. However, we thought that strong graft biomechanics was a prerequisite for good clinical outcomes; (2) The studies that were involved used various measuring techniques, which might have impacted the baseline of the measured data. However, the comparison of the data before and after the experiments was unaffected by this difference; (3) The surgical method is another element that affects SCR in addition to the graft. We did not group the various operations in our study according to the surgical methods. However, the surgical procedure had no impact on the graft's biomechanical effectiveness.
Conclusion
In conclusion, SCR combined with IRCT could greatly increase the superior and anteroposterior stability of the glenohumeral joint. However, it should be highlighted that SCR, particularly SCR with LHBT or HDA, might not restore the glenohumeral joint's original biomechanical condition. Despite the potential for donor-site morbidity and the longer recovery time, FL is still the best current option for SCRe. The goal of future research should be to discover new grafts that are less expensive, more effective from a biomechanical standpoint, and have good biocompatibility for SCR.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author contributions
XZ: conception and design of study, drafting and revising article, final approval of version to be submitted and statistics. JJ: conception and design of study, drafting and revising article, final approval of version to be submitted and statistics. LW: acquisition of data, review of article and final approval of the version to be submitted. BZ: conception and design of study, revising article, analysis and interpretation of data, final approval of version to be submitted and supervision. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to acknowledge the support of professor YL, who worked at Beijing Chao-yang Hospital, as our academic leader.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Pashuck TD, Hirahara AM, Cook JL, Cook CR, Andersen WJ, Smith MJ. Superior capsular reconstruction using dermal allograft is a safe and effective treatment for massive irreparable rotator cuff tears: 2-year clinical outcomes. Arthrosc. (2021) 37(2):489–96 e1. doi: 10.1016/j.arthro.2020.10.014
2. Ishigaki N, Hata Y, Matsuba T, Hino M, Murakami N, Kobayashi H. Long-term results of partial repair for irreparable rotator cuff tear. JSES Int. (2021) 5(4):642–8. doi: 10.1016/j.jseint.2021.02.010
3. Oh JH, Park MS, Rhee SM. Treatment strategy for irreparable rotator cuff tears. Clin Orthop Surg. (2018) 10(2):119–34. doi: 10.4055/cios.2018.10.2.119
4. Elhassan BT, Wagner ER, Werthel JD. Outcome of lower trapezius transfer to reconstruct massive irreparable posterior-superior rotator cuff tear. J Shoulder Elbow Surg. (2016) 25(8):1346–53. doi: 10.1016/j.jse.2015.12.006
5. Kovacevic D, Suriani RJ Jr., Grawe BM, Yian EH, Gilotra MN, Hasan SA, et al. Management of irreparable massive rotator cuff tears: a systematic review and meta-analysis of patient-reported outcomes, reoperation rates, and treatment response. J Shoulder Elbow Surg. (2020) 29(12):2459–75. doi: 10.1016/j.jse.2020.07.030
6. Liu F, Dong J, Kang Q, Zhou D, Xiong F. Subacromial balloon spacer implantation for patients with massive irreparable rotator cuff tears achieves satisfactory clinical outcomes in the short and middle of follow-up period: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. (2021) 29(1):143–53. doi: 10.1007/s00167-019-05834-3
7. Sevivas N, Ferreira N, Andrade R, Moreira P, Portugal R, Alves D, et al. Reverse shoulder arthroplasty for irreparable massive rotator cuff tears: a systematic review with meta-analysis and meta-regression. J Shoulder Elbow Surg. (2017) 26(9):e265–e77. doi: 10.1016/j.jse.2017.03.039
8. Reeves JM, Singh S, Langohr GDG, Athwal GS, Johnson JA. An in-vitro biomechanical assessment of humeral head migration following irreparable rotator cuff tear and subacromial balloon reconstruction. Shoulder Elbow. (2020) 12(4):265–71. doi: 10.1177/1758573219865479
9. Mirzaee F, Aslani MA, Zafarani Z, Aslani H. Treatment of massive irreparable rotator cuff tear with arthroscopic subacromial bursectomy, Biceps tenotomy, and tuberoplasty. Arch Bone Jt Surg. (2019) 7(3):263–8.31312685
10. Gervasi E, Cautero E, Dekel A. Fluoroscopy-guided implantation of subacromial “biodegradable spacer” using local anesthesia in patients with irreparable rotator cuff tear. Arthrosc Tech. (2014) 3(4):e455–8. doi: 10.1016/j.eats.2014.05.010
11. Cvetanovich GL, Waterman BR, Verma NN, Romeo AA. Management of the irreparable rotator cuff tear. J Am Acad Orthop Surg. (2019) 27(24):909–17. doi: 10.5435/JAAOS-D-18-00199
12. Garofalo R, Flanagin B, Castagna A, Calvisi V, Krishnan SG. Massive irreparable rotator cuff tear and associated deltoid tear. Does the reverse shoulder arthroplasty and deltoid repair be a possible option of treatment? J Orthop Sci. (2016) 21(6):753–8. doi: 10.1016/j.jos.2016.06.016
13. Matsen FA 3rd, Whitson A, Jackins SE, Hsu JE. Significant improvement in patient self-assessed comfort and function at six weeks after the smooth and move procedure for shoulders with irreparable rotator cuff tears and retained active elevation. Int Orthop. (2019) 43(7):1659–67. doi: 10.1007/s00264-019-04310-4
14. Sanchez G, Rossy WH, Lavery KP, McHale KJ, Ferrari MB, Sanchez A, et al. Arthroscopic superior capsule reconstruction technique in the setting of a massive, irreparable rotator cuff tear. Arthrosc Tech. (2017) 6(4):e1399–e404. doi: 10.1016/j.eats.2017.05.020
15. Mihata T, McGarry MH, Pirolo JM, Kinoshita M, Lee TQ. Superior capsule reconstruction to restore superior stability in irreparable rotator cuff tears: a biomechanical cadaveric study. Am J Sports Med. (2012) 40(10):2248–55. doi: 10.1177/0363546512456195
16. Li H, Zhou B, Tang K. Advancement in arthroscopic superior capsular reconstruction for irreparable massive rotator cuff tear. Orthop Surg. (2021) 13(7):1951–9. doi: 10.1111/os.12976
17. Smith GC, Im HY, Lam PH. Effect of human dermal allograft thickness on glenohumeral stability for superior capsular reconstruction in irreparable supraspinatus tears: a biomechanical analysis of the superior capsular reconstruction - A cadaveric study. Shoulder Elbow. (2022) 14(1):31–7. doi: 10.1177/1758573220925086
18. Lee A, Farooqi AS, Novikov D, Li X, Kelly JDT, Parisien RL. Clinical and functional outcomes by graft type in superior capsular reconstruction: a systematic review and meta-analysis. Am J Sports Med. (2021) 50(14):3998–4007. doi: 10.1177/03635465211040440
19. Baek S, Shin MH, Kim TM, Im JM, Oh KS, Chung SW. Clinical outcomes of interposition graft versus superior capsular reconstruction in patients with irreparable rotator cuff tears: a systematic review and meta-analysis. Orthop J Sports Med. (2021) 9(9):23259671211022241. doi: 10.1177/23259671211022241
20. Makovicka JL, Chung AS, Patel KA, Deckey DG, Hassebrock JD, Tokish JM. Superior capsule reconstruction for irreparable rotator cuff tears: a systematic review of biomechanical and clinical outcomes by graft type. J Shoulder Elbow Surg. (2020) 29(2):392–401. doi: 10.1016/j.jse.2019.07.005
21. Vredenburgh ZD, Prodromo JP, Tibone JE, Dunphy TR, Weber J, McGarry MH, et al. Biomechanics of tensor fascia lata allograft for superior capsular reconstruction. J Shoulder Elbow Surg. (2021) 30(1):178–87. doi: 10.1016/j.jse.2020.04.025
22. Alarcon JF, Uribe-Echevarria B, Clares C, Apablaza D, Vargas JC, Benavente S, et al. Superior capsular reconstruction with autologous fascia Lata using a single lateral-row technique is an effective option in massive irreparable rotator cuff tears: minimum 2-year follow-up. Arthrosc. (2021) 37(9):2783–96. doi: 10.1016/j.arthro.2021.04.009
23. Gracitelli MEC, Beraldo RA, Malavolta EA, Assuncao JH, Oliveira DRO, Ferreira Neto AA. Superior capsular reconstruction with fascia Lata allograft for irreparable supraspinatus tendon tears. Rev Bras Ortop (Sao Paulo). (2019) 54(5):591–6. doi: 10.1016/j.rbo.2017.11.011
24. Polacek M, Nyegaard CP. Superior capsular reconstruction using 3-layered fascia Lata autograft reinforced with a nonresorbable suture mesh. Arthrosc Sports Med Rehabil. (2020) 2(5):e489–e97. doi: 10.1016/j.asmr.2020.05.011
25. Angelo A, de Campos Azevedo CI. Minimally invasive fascia lata harvesting in ASCR does not produce significant donor site morbidity. Knee Surg Sports Traumatol Arthrosc. (2019) 27(1):245–50. doi: 10.1007/s00167-018-5085-1
26. Angelo A, de Campos Azevedo CI. Donor-Site morbidity after autologous fascia Lata harvest for arthroscopic superior capsular reconstruction: a midterm follow-up evaluation. Orthop J Sports Med. (2022) 10(2):23259671211073133. doi: 10.1177/23259671211073133
27. Han F, Kong CH, Hasan MY, Ramruttun AK, Kumar VP. Superior capsular reconstruction for irreparable supraspinatus tendon tears using the long head of biceps: a biomechanical study on cadavers. Orthop Traumatol Surg Res. (2019) 105(2):257–63. doi: 10.1016/j.otsr.2018.10.023
28. Lubowitz JH, Brand JC, Rossi MJ. Shoulder superior capsular reconstruction using acellular human dermal allograft. Arthrosc. (2019) 35(10):2769–70. doi: 10.1016/j.arthro.2019.07.014
29. de Campos Azevedo CI, Andrade R, Leiria Pires Gago Angelo AC, Espregueira-Mendes J, Ferreira N, Sevivas N. Fascia Lata autograft versus human dermal allograft in arthroscopic superior capsular reconstruction for irreparable rotator cuff tears: a systematic review of clinical outcomes. Arthrosc. (2020) 36(2):579–91 e2. doi: 10.1016/j.arthro.2019.08.033
30. Ferrando A, Kingston R, Delaney RA. Superior capsular reconstruction using a porcine dermal xenograft for irreparable rotator cuff tears: outcomes at minimum two-year follow-up. J Shoulder Elbow Surg. (2021) 30(5):1053–9. doi: 10.1016/j.jse.2020.08.020
31. Polacek M. Arthroscopic superior capsular reconstruction with acellular porcine dermal Xenograft for the treatment of massive irreparable rotator cuff tears. Arthrosc Sports Med Rehabil. (2019) 1(1):e75–84. doi: 10.1016/j.asmr.2019.08.001
32. Cromheecke M, Garret J, Deranlot J, Bonnevialle N, Gaudin S, Ladermann A, et al. Low healing rates and moderate functional outcome after arthroscopic superior capsular reconstruction using a porcine xenograft. Knee Surg Sports Traumatol Arthrosc. (2022) 30(7):2528–34. doi: 10.1007/s00167-022-06916-5
33. Singh S, Reeves J, Langohr GDG, Johnson JA, Athwal GS. The subacromial balloon spacer versus superior capsular reconstruction in the treatment of irreparable rotator cuff tears: a biomechanical assessment. Arthrosc. (2019) 35(2):382–9. doi: 10.1016/j.arthro.2018.09.016
34. Osti L, Milani L, Ferrari S, Maffulli N. Subacromial spacer implantation: an alternative to arthroscopic superior capsular reconstruction. A systematic review. Br Med Bull. (2021) 139(1):59–72. doi: 10.1093/bmb/ldab014
35. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Br Med J. (2021) 372:n71. doi: 10.1136/bmj.n71
36. Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev. (2019) 10:ED000142. doi: 10.1002/14651858.ED000142
37. Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. (1998) 52(6):377–84. doi: 10.1136/jech.52.6.377
38. Tibone JE, Mansfield C, Kantor A, Giordano J, Lin CC, Itami Y, et al. Human dermal allograft superior capsule reconstruction with graft length determined at glenohumeral abduction angles of 20° and 40° decreases joint translation and subacromial pressure without compromising range of motion: a cadaveric biomechanical study. Arthrosc - J Arthrosc and Relat Surg. (2021) 38(5):1398–407. doi: 10.1016/j.arthro.2021.11.007
39. Shah SS, Kontaxis A, Jahandar A, Bachner E, Gulotta LV, Dines DM, et al. Superior capsule reconstruction using a single 6-mm-thick acellular dermal allograft for massive rotator cuff tears: a biomechanical cadaveric comparison to fascia lata allograft. J Shoulder Elbow Surg. (2021) 30(9):2166–76. doi: 10.1016/j.jse.2020.11.015
40. Park MC, Hung VT, DeGiacomo AF, McGarry MH, Adamson GJ, Lee TQ. Anterior cable reconstruction of the superior capsule using semitendinosus allograft for large rotator cuff defects limits superior migration and subacromial contact without inhibiting range of motion: a biomechanical analysis. Arthrosc. (2021) 37(5):1400–10. doi: 10.1016/j.arthro.2020.12.183
41. Lobao MH, Melvani RT, Abbasi P, Parks BG, Murthi AM. Dermal allograft superior capsule reconstruction biomechanics and kinematics. J Shoulder Elbow Surg. (2021) 30(9):2156–65. doi: 10.1016/j.jse.2020.11.024
42. Lacheta L, Brady A, Rosenberg SI, Dekker TJ, Kashyap R, Zandiyeh P, et al. Superior capsule reconstruction with a 3 mm-thick dermal allograft partially restores glenohumeral stability in massive posterosuperior rotator cuff deficiency: a dynamic robotic shoulder model. Am J Sports Med. (2021) 49(8):2056–63. doi: 10.1177/03635465211013364
43. EC K, Tibone JE, Ihn H, Akeda M, Kim BS, McGarry MH, et al. Superior capsule reconstruction using fascia Lata allograft compared with double- and single-layer dermal allograft: a biomechanical study. Arthrosc. (2021) 37(4):1117–25. doi: 10.1016/j.arthro.2020.11.054
44. Denard PJ, Park MC, McGarry MH, Adamson G, Lee TQ. Biomechanical assessment of a V-shaped semitendinosus allograft anterior cable reconstruction for irreparable rotator cuff tears. Arthrosc. (2021) 38(3):719–28. doi: 10.1016/j.arthro.2021.07.031
45. Denard PJ, Chae S, Chalmers C, Choi JH, McGarry MH, Adamson G, et al. Biceps box configuration for superior capsule reconstruction of the glenohumeral joint decreases superior translation but not to native levels in a biomechanical study. Arthrosc Sports Med Rehabil. (2021) 3(2):e343–e50. doi: 10.1016/j.asmr.2020.09.024
46. Berthold DP, Muench LN, Dyrna F, Scheiderer B, Obopilwe E, Cote MP, et al. Comparison of different fixation techniques of the long head of the Biceps tendon in superior capsule reconstruction for irreparable posterosuperior rotator cuff tears: a dynamic biomechanical evaluation. Am J Sports Med. (2021) 49(2):305–13. doi: 10.1177/0363546520981559
47. Berthold DP, Bell R, Muench LN, Jimenez AE, Cote MP, Obopilwe E, et al. A new approach to superior capsular reconstruction with hamstring allograft for irreparable posterosuperior rotator cuff tears: a dynamic biomechanical evaluation. J Shoulder Elbow Surg. (2021) 30(7S):S38–47. doi: 10.1016/j.jse.2021.04.002
48. Scheiderer B, Kia C, Obopilwe E, Johnson JD, Cote MP, Imhoff FB, et al. Biomechanical effect of superior capsule reconstruction using a 3-mm and 6-mm thick acellular dermal allograft in a dynamic shoulder model. Arthrosc. (2020) 36(2):355–64. doi: 10.1016/j.arthro.2019.08.026
49. Rybalko D, Bobko A, Amirouche F, Peresada D, Hussain A, Patetta M, et al. Biomechanical effects of superior capsular reconstruction in a rotator cuff–deficient shoulder: a cadaveric study. J Shoulder and Elbow Surg. (2020) 29(10):1959–66. doi: 10.1016/j.jse.2020.03.007
50. Han SY, Lee TQ, Wright DJ, Park IJ, Mauro M, McGarry MH, et al. Effect of biceps rerouting technique to restore glenohumeral joint stability for large irreparable rotator cuff tears: a cadaveric biomechanical study. J Shoulder Elbow Surg. (2020) 29(7):1425–34. doi: 10.1016/j.jse.2019.11.015
51. Dyrna F, Berthold DP, Muench LN, Beitzel K, Kia C, Obopilwe E, et al. Graft tensioning in superior capsular reconstruction improves glenohumeral joint kinematics in massive irreparable rotator cuff tears: a biomechanical study of the influence of superior capsular reconstruction on dynamic shoulder abduction. Orthop J Sports Med. (2020) 8(10):2325967120957424. doi: 10.1177/2325967120957424
52. Curtis DM, Lee CS, Qin C, Edgington J, Parekh A, Miller J, et al. Superior capsule reconstruction with subacromial allograft spacer: biomechanical cadaveric study of subacromial contact pressure and superior humeral head translation. Arthrosc. (2020) 36(3):680–6. doi: 10.1016/j.arthro.2019.09.047
53. Adams CR, Comer B, Scheiderer B, Imhoff FB, Morikawa D, Kia C, et al. The effect of glenohumeral fixation angle on deltoid function during superior capsule reconstruction: a biomechanical investigation. Arthrosc. (2020) 36(2):400–8. doi: 10.1016/j.arthro.2019.09.011
54. Singh S, Reeves J, Langohr GDG, Johnson JA, Athwal GS. The effect of the subacromial balloon spacer on humeral head translation in the treatment of massive, irreparable rotator cuff tears: a biomechanical assessment. J Shoulder Elbow Surg. (2019) 28(10):1841–7. doi: 10.1016/j.jse.2019.03.036
55. Omid R, Stone MA, Lin CC, Patel NA, Itami Y, McGarry MH, et al. Biomechanical analysis of latissimus dorsi tendon transfer with and without superior capsule reconstruction using dermal allograft. J Shoulder Elbow Surg. (2019) 28(8):1523–30. doi: 10.1016/j.jse.2019.01.016
56. Lobao MH, Canham RB, Melvani RT, Abboud JA, Parks BG, Murthi AM. Biomechanics of biodegradable subacromial balloon spacer for irreparable superior rotator cuff tears: study of a cadaveric model. J Bone Joint Surg Am. (2019) 101(11):e49. doi: 10.2106/JBJS.18.00850
57. Leschinger T, Besch K, Aydin C, Staat M, Scaal M, Muller LP, et al. Irreparable rotator cuff tears: a biomechanical comparison of superior capsuloligamentous Complex reconstruction techniques and an interpositional graft technique. Orthop J Sports Med. (2019) 7(8):2325967119864590. doi: 10.1177/2325967119864590
58. Croom WP, Adamson GJ, Lin CC, Patel NA, Kantor A, McGarry MH, et al. A biomechanical cadaveric study of patellar tendon allograft as an alternative graft material for superior capsule reconstruction. J Shoulder Elbow Surg. (2019) 28(7):1241–8. doi: 10.1016/j.jse.2018.12.015
59. Mihata T, Bui CNH, Akeda M, Cavagnaro MA, Kuenzler M, Peterson AB, et al. A biomechanical cadaveric study comparing superior capsule reconstruction using fascia lata allograft with human dermal allograft for irreparable rotator cuff tear. J Shoulder Elbow Surg. (2017) 26(12):2158–66. doi: 10.1016/j.jse.2017.07.019
60. Mihata T, McGarry MH, Kahn T, Goldberg I, Neo M, Lee TQ. Biomechanical effect of thickness and tension of fascia Lata graft on glenohumeral stability for superior capsule reconstruction in irreparable supraspinatus tears. Arthrosc. (2016) 32(3):418–26. doi: 10.1016/j.arthro.2015.08.024
61. Altintas B, Storaci HW, Lacheta L, Dornan GJ, Krob JJ, Aman ZS, et al. Superior capsule reconstruction using acellular dermal allograft secured at 45° of glenohumeral abduction improves the superior stability of the glenohumeral joint in irreparable massive posterosuperior rotator cuff tears. Arthrosc. (2022) S0749-8063(22):695–8. doi: 10.1016/j.arthro.2022.10.037
62. Senekovic V, Poberaj B, Kovacic L, Mikek M, Adar E, Dekel A. Prospective clinical study of a novel biodegradable sub-acromial spacer in treatment of massive irreparable rotator cuff tears. Eur J Orthop Surg Traumatol. (2013) 23(3):311–6. doi: 10.1007/s00590-012-0981-4
63. de Campos Azevedo CI, Leiria Pires Gago Angelo AC, Quental C, Goncalves S, Folgado J, Ferreira N, et al. Proximal and mid-thigh fascia lata graft constructs used for arthroscopic superior capsule reconstruction show equivalent biomechanical properties: an in vitro human cadaver study. JSES Int. (2021) 5(3):439–46. doi: 10.1016/j.jseint.2021.01.016
64. Eppler MB, Bolia IK, Tibone JE, Gamradt SC, Hatch GF, Omid R, et al. Superior capsular reconstruction of the shoulder. Arthrosc. (2021) 37(6):1708–10. doi: 10.1016/j.arthro.2021.04.001
Keywords: rotator cuff, superior capsular reconstruction, graft, material, biomechanics
Citation: Zhao X, Wen L, Zhang B and Jia J (2023) Biomechanical outcomes of superior capsular reconstruction for irreparable rotator cuff tears by different graft materials-a systematic review and meta-analysis. Front. Surg. 9:939096. doi: 10.3389/fsurg.2022.939096
Received: 8 May 2022; Accepted: 14 December 2022;
Published: 9 January 2023.
Edited by:
Jaimo Ahn, Michigan Medicine, University of Michigan, United StatesReviewed by:
Yansong Qi, Inner Mongolia People's Hospital, ChinaAlideertu Dong, Inner Mongolia University, China
© 2023 Zhao, Wen, Zhang and Jia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoxiong Zhao emhhb3hpYW94aW9uZ0BjY211LmVkdS5jbg==
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Xiaoxiong Zhao
Xiaoxiong Zhao Liang Wen
Liang Wen Bo Zhang
Bo Zhang