
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Surg. , 01 August 2022
Sec. Reconstructive and Plastic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.932164
Objective: This study collected and summarized publications related to craniomaxillofacial distraction osteogenesis(DO) from 2000 to 2021, investigated trends in related research, and compared publications from different countries, institutions and journals. The aim is showcasing hotspots and frontiers in the field and providing a reference for future research.
Background: Craniomaxillofacial DO serves to treat different types of craniomaxillofacial dysplasia and bone defects and deformities. DO can significantly reduce surgical trauma, complications, and recurrence rate compared to conventional surgery. However, there is a lack of bibliometric analyses regarding Craniomaxillofacial DO.
Methods: CiteSpace and VOSviewer were used to analyze and visualize 3,141 articles and reviews searching through the Web of Science Core Collection(WOSCC) to obtain publications on craniomaxillofacial DO from 1 January 2000 to 31 December 2021.
Results: In the last 21 years, there has been a significant increase in the number of publications. The United States, the People's Republic of China, and Italy produce the vast majority of publications. University of Milan and University of Bologna are the most influential in this field. McCarthy JG is the most influential author. Obstructive sleep apnea, TMJ ankylosis and cleft lip and palate are potential research direction in this field.
Conclusion: Future research should focus on the precise indications and optimal timing of craniomaxillofacial DO and the evaluation of the long-term outcomes of various modified procedures. This study provides a relatively objective reference for related researchers, medical practitioners, and global health systems.
Distraction osteogenesis (DO) is a surgical procedure for correcting skeletal deficiencies or repair bone defects by applying a specific amount of traction or expansion force to an incised bone segment to regenerate new bone in the interstitial space to lengthen or widen the bone (1). The principle of DO can be explained by the “law of tension-stress” proposed by Ilizarov, which states that the progressive application of a continuous tension force to living biological tissue stimulates and maintains its tissue regeneration and growth (1). DO was initially applied to the long bones of the limbs and was successfully applied clinically in the craniomaxillofacial treatment by McCarthy in 1992 (2). So far, DO has been a commonly-used approach to treat craniomaxillofacial deformities.
Craniomaxillofacial DO, serves to treat different types of craniomaxillofacial dysplasia and bone defects and deformities. A wide range of indications for the treatment of various types of dysplasia and bone defects and deformities involving the craniomaxillofacial fields and their complications such as Crouzon Syndrome (3), craniosynostosis (4), vertical ridge deficiencies (5, 6), unilateral craniofacial microsomia (7) and so on. DO can significantly reduce surgical trauma, complications, and recurrence rates compared to conventional surgery, advancing the age at which patients can be orthodontically treated (8, 9).
Bibliometrics is a reliable tool for research assessment of publications to explore trends and frontiers on a certain research topic, such as cancer gene therapy (10), neck dissection for oral squamous-cell carcinoma (11) and so on. However, to the best of our knowledge, no one has yet conducted a bibliometric analysis of craniomaxillofacial DO so far. Thus, the current study aims to assess the research trends, country, institution, authors, journals, references and keywords of craniomaxillofacial DO-related publications to reveal the research frontiers and predict future trends for relevant researchers.
We conducted a systematic search of the Web of Science Core Collection for relevant literature to obtain publications on craniomaxillofacial DO from 1 January 2000 to 31 December 2021. We used the following search terms: TS = (distraction osteogenesis) AND TS = (maxillofacial OR craniofacial OR dentofacial OR maxillo-facial OR cranio-facial OR dento-facial OR maxilla* OR mandib* OR alveolar). The total number of publications was 3,515 after initial search. Then the publications were filtered by CiteSpace (Drexel University, Philadelphia, USA). Only articles and reviews were included, and other types of publications(editorial material, meeting abstract, proceedings paper, letter, correction and new item)as well as duplicates were excluded. Detailed information of the corrections were provided in Supplementary Appendix S1. Consequently, a total of 3,141 publications was included in the study (Figure 1).
We used CiteSpace to identify the keywords with burst and the references with burst. CiteSpace is software for analyzing and visualizing publication trends. Burst represents a dramatic increase in interest in the academic field. As a reflection of the academic trends and hot topics in a field at a given time, burst can help predict cutting-edge research directions (12). The visual maps consist of nodes and lines. The nodes represented elements including countries, institutions, authors, journals and keywords. The frequency of occurrence is represented by the size of the nodes. The co-occurrence or co-citation relationship is shown by the lines between the nodes. The nodes and lines' colors correspond to the average year of the relevant publication.
VOSviewer (Leiden University, Leiden, the Netherlands) was used to construct visualization maps of co-citation and co-occurrence analysis. In the clustering maps, different colors represent different clusters. There are differences in the themes represented by the different clusters. In other maps, VOSviewer applies different colors to the keywords based on different average years of occurrence. Elements in blue and green occur earlier, while the yellow and red ones appear later.
A total of 3,141 reviews and articles related to craniomaxillofacial DO were retrieved during the study period. The last two decades can be divided into two phases according to the research trends. The first phase lasted from 2000 to 2012, with a relatively rapid increase in the count of publications, including 208 publications in 2012 The second phase occurred from 2013 to 2021, with a relatively stable number of publications.
From 2000 to 2021, the number of annual citation times showed a clear trend of increase, except for decreases in 2013, 2017 and 2020. Notably, there was a boost increase in annual citation times in 2021 (n = 5,735), compared to 2020(n = 4,572), indicating that craniomaxillofacial DO has recently attracted great academic attention from global researchers (Figure 2).
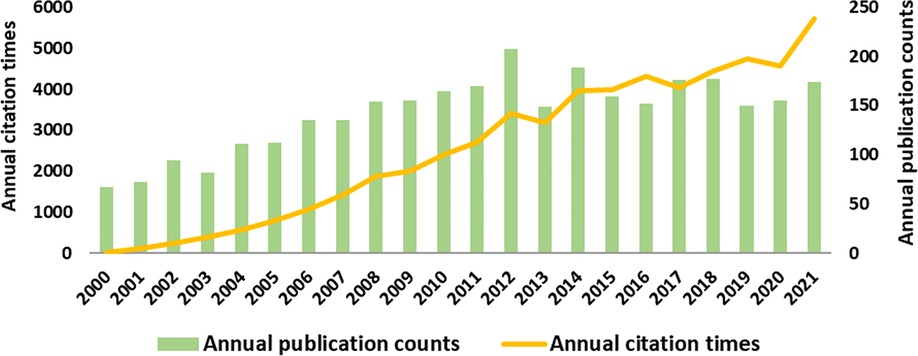
Figure 2. Analysis of global research trend of craniomaxillofacial distraction osteogenesis during 2000–2021.
As shown in Table 1, the United States had the most publications on craniomaxillofacial DO, with 958 publications, followed by People's Republic of China (n = 380), Japan (n = 261), Turkey (n = 218), Italy (n = 216) Germany (n = 157), Netherlands (n = 145), South Korea (n = 138), England(n = 106) and Brazil (n = 96). The co-occurrence analysis (Figure 3A) showed that the United States, People's Republic of China and Japan are the main research forces in craniomaxillofacial DO and a significant amount of cooperation is observed between the United States and other countries such as People's Republic of China, the Netherlands, Italy, Japan, Turkey and Canada. In addition, Germany and Japan have studied craniomaxillofacial DO for an earlier period, while Brazil, Egypt and India are later.
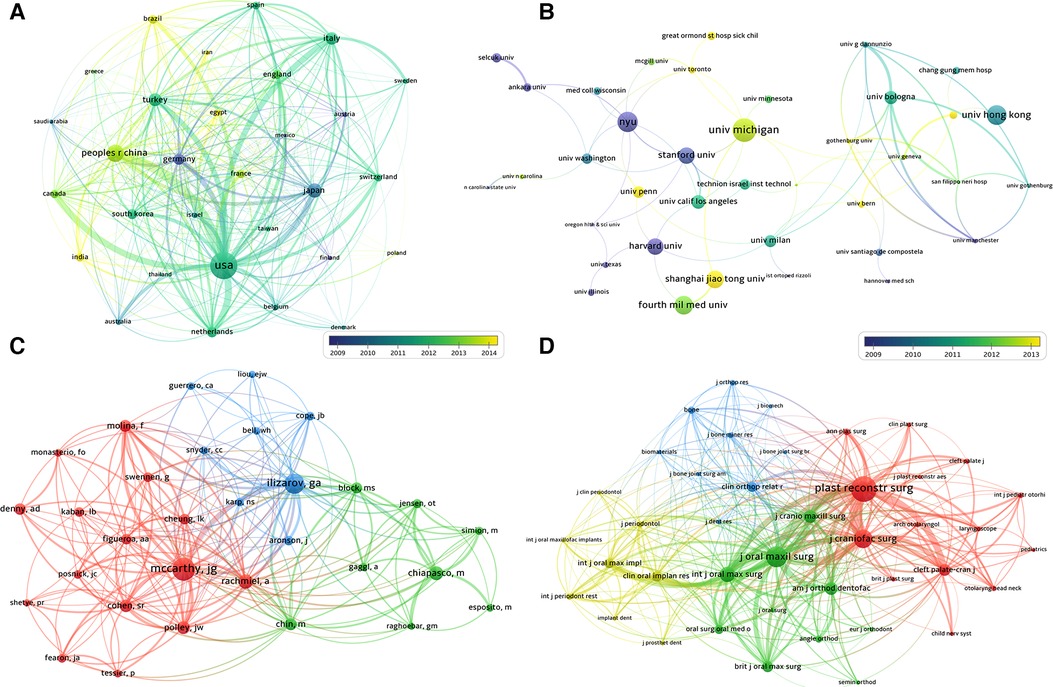
Figure 3. (A) Co-occurrence analysis of countries; (B) Co-occurrence analysis of institution; (C) clustering analysis of cited authors; (D) clustering analysis of cited journals.
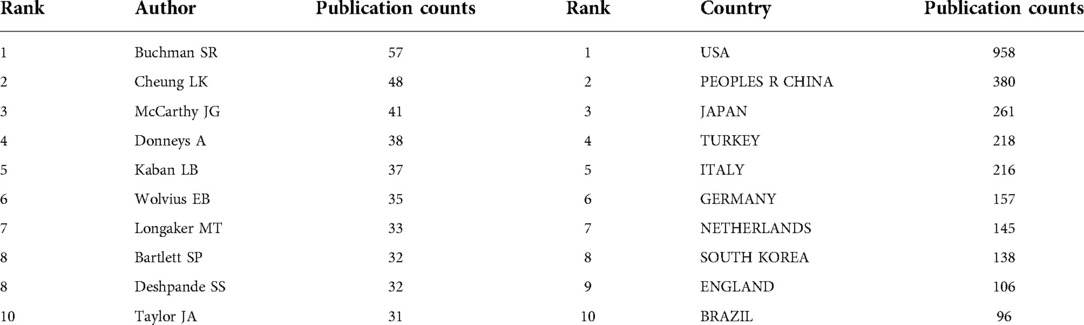
Table 1. The top 10 most productive authors and countries contributing to the research on craniomaxillofacial distraction osteogenesis from 2000 to 2021.
The top 5 institutions in terms of the number of relevant research publications are University of Michigan (with 72 publications), New York University (63), The University of Hong Kong (61), The Fourth Military Medical University (57) and Sichuan University (57). It is worth noting that among the top 5 institutions in terms of citation times, University of Milan (2695) and University of Bologna (1927) are not ranked in the top in terms of the number of publications, which indicates the greater influence of these two institutions in the craniomaxillofacial DO field (Table 2 and Figure 3B).
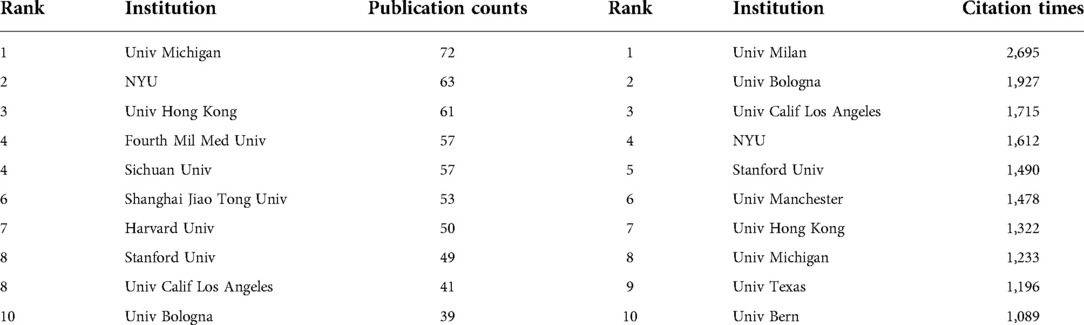
Table 2. The top 10 most productive and most cited institutions contributing to the research on craniomaxillofacial distraction osteogenesis from 2000 to 2021.
Table 1 shows the top 10 most productive authors contributing to the research on craniomaxillofacial DO from 2000 to 2021. The most active author in this field were Buchman SR(with 57 publications), Cheung LK(48) and McCarthy JG(41). McCarthy JG is the most influential author and has worked closely with Molina F and Cohen SR, Polley JW.
The top 10 most productive journals are listed in Table 3. The most productive journals are Journal of Craniofacial Surgery with 531 publications, followed by Journal of Oral and Maxillofacial Surgery(with 314 publications), Journal of Cranio-Maxillofacial Surgery(210), International Journal of Oral and Maxillofacial Surgery(207), Plastic and Reconstructive Surgery(185). Among the top 5 journals, Plastic and Reconstructive Surgery (with 6,343 citations, IF4.73), Journal of Oral and Maxillofacial Surgery (5,482, IF1.895) and Journal of Craniofacial Surgery (5,431, IF1.046) have the most total citations, which indicates that these three journals are the most influential and professional in the field of craniomaxillofacial DO. Scholars conducting research in this field can regard this as a reference to prioritize their articles for publication in these journals. Additionally, the analysis of Figure 3D shows that the most co-cited journals are Craniofacial Surgery, Journal of Oral and Maxillofacial Surgery, Plastic and Reconstructive Surgery and Cleft Palate-craniofacial, which reflects the similarity in publication themes of the three journals.
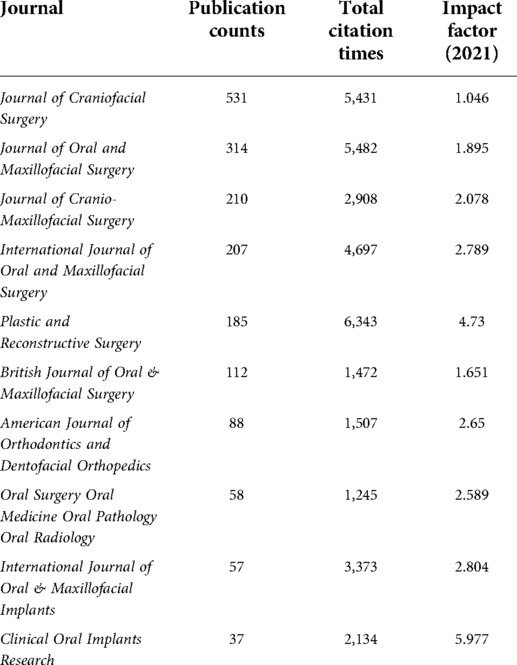
Table 3. The top 10 most productive journals contributing to the research on craniomaxillofacial distraction osteogenesis from 2000 to 2021.
The top 30 cited references with the strongest burst were present in Figure 4. The top 3 among them were as follows. “Distraction osteogenesis of the craniofacial skeleton” by McCarthy et al. (13) in 2001, which reviews the history, biology and clinical applications of DO; “Alveolar distraction osteogenesis vs. vertical guided bone regeneration for the correction of vertically deficient edentulous ridges: a 1–3-year prospective study on humans” by Chiapasco et al. (14) in 2004, which examined the ability of vertical directed bone regeneration with vertical DO to restore vertically deficient alveolar ridges. The results suggested that DO can reduce the incidence of complications and provide a more favorable long-term prognosis (14); “The surgical correction of Pierre Robin sequence(PRS): mandibular distraction osteogenesis vs. tongue-lip adhesion” by Flores et al. (15) in 2014. Flores et al. analyzed the outcomes of mandibular DO vs. tongue-lip adhesion in the surgical treatment of PRS, concluding that DO performs better in terms of improving airway function (15).
Notably, some recent publications were identified as references with burst, indicating that they are gaining much academic attention. Such publications are listed below: “Mandibular distraction osteogenesis for the management of upper airway obstruction in children with micrognathia: a systematic review.” by Breik et al. (16) in 2016; “Best Practices for the Diagnosis and Evaluation of Infants With Robin Sequence: A Clinical Consensus Report.” by Breugem et al. (17) in 2016; “Airway and Feeding Outcomes of Mandibular Distraction, Tongue-Lip Adhesion, and Conservative Management in Pierre Robin Sequence: A Prospective Study.” By Khansa et al. (18) in 2017.
The blue line represents the timeline and the red line represents the period in which a reference had a burst.
The top 20 keywords with the strongest burst were shown in Figure 5. From 2000 to 2010, the keywords with the strongest burst included “gradual distraction”, “deficiency”, “messenger RNA”, “implant”, “alveolar ridge augmentation”, “ridge augmentation”, “vertical distraction”, “device”, “in vitro” and “deficient edentulous ridge”, which reflected the hotspots about the principle, operation of DO and its application in oral implantology and maxillofacial deficiency. Academic attention from 2011 to 2018 turned into the PRS including the efficacy of DO and comparison of DO with other treatment modalities. Since 2018 till now, scholars have gradually embarked on research into the use of DO in the treatment of other craniomaxillofacial disorders such as obstructive sleep apnea, TMJ ankylosis and cleft lip and palate.
The clustering analysis showed that the keywords with high frequency were grouped into three primary clusters (Figure 6A). The green cluster was mainly associated with maxillofacial defect repair and dental implant-related alveolar bone augmentation, including “reconstruction”, “alveolar distraction augmentation”, “bone graft”, “dental implant” and so on. The red cluster focuses on application methods, application sites and the advancement, including “advancement”, “surgery”, “complications”, “gradual distraction”, “osteotomy”, “craniosynostosis” and so on. The blue cluster mainly focused on syndromes resulting from craniomaxillofacial developmental defects, including “mandibular distraction osteoge”, “children”, “management”, “pierre robin sequence”, “upper airway obstruction”, “obstructive sleep apnea” and so on.
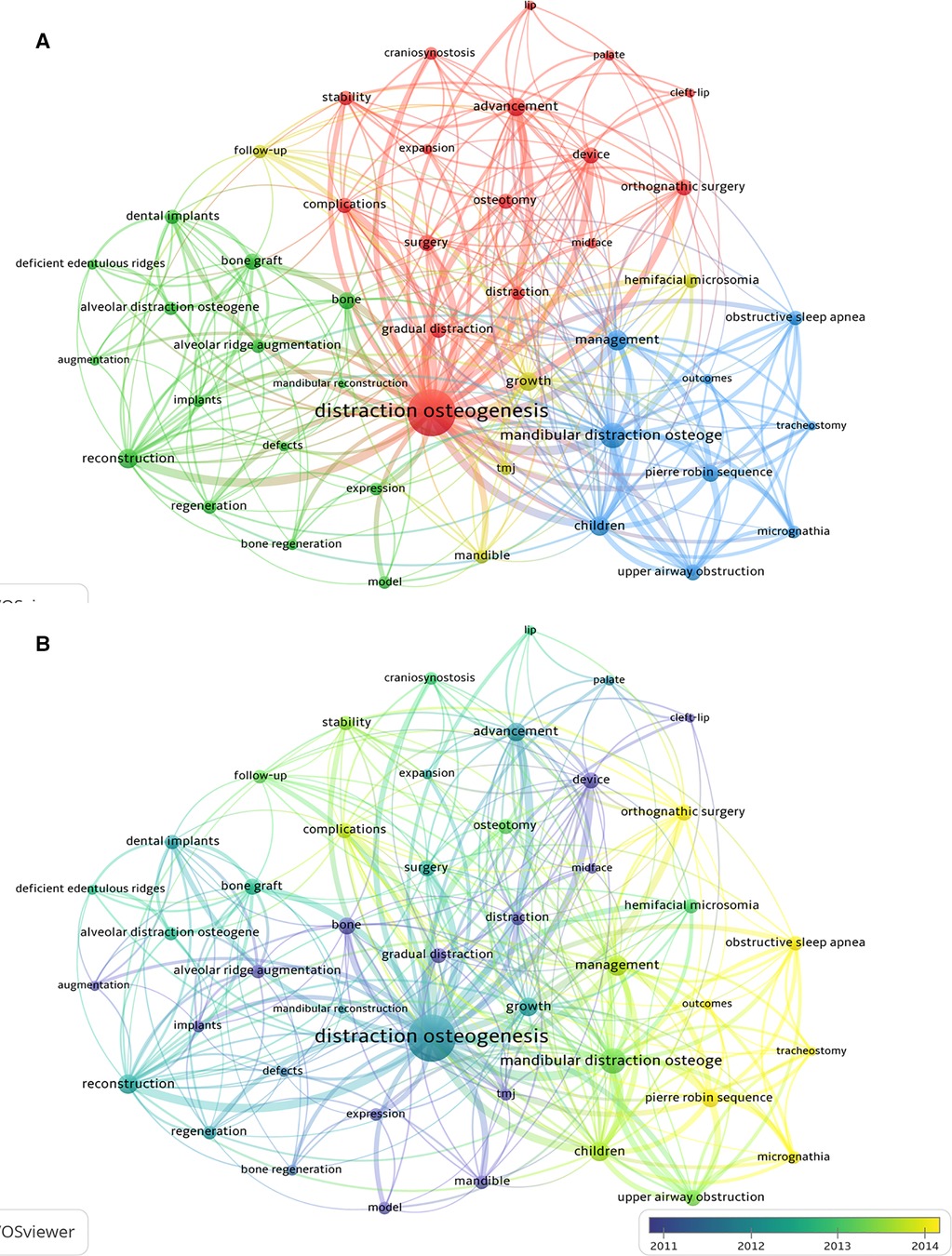
Figure 6. The co-occurrence network of keywords related to research on craniomaxillofacial distraction osteogenesis from 2000 to 2021. (A) Clustering analysis of keywords; (B) Timeline view of keywords with frequency no less than 80.
The timeline view of the keywords with high frequency was provided in Figure 6B. The studies related to the principle of DO and its application in oral implantology and maxillofacial deficiency were carried out earlier, while in the last few years, the research hotspots have focused on its application in orthognathic surgery and the treatment of PRS, obstructive sleep apnea and other craniomaxillofacial disorders.
We conducted a bibliometric analysis of publications on maxillofacial distraction osteogenesis from 2000 to 2021. The number of annual publications and citations increased significantly, according to the results. The United States, the People's Republic of China and Italy are the most dominant forces in research related to this topic. Five of the top ten most productive institutions were located in the United States, four in China, and one in Italy. Although only one institution from Italy is listed, two institutions, University of Milan and University of Bologna, from Italy have the highest number of citations, indicating the high quality of their publications. Buchman SR is the most productive author, while McCarthy JG is the most influential author.
The most influential journal is Plastic and Reconstructive Surgery, whereas the most prolific journal is the Journal of Oral and Maxillofacial Surgery.
The top 3 most recent references with burst are all related to micrognathia, specifically PRS. Breik et al. (16) published “Mandibular distraction osteogenesis for the management of upper airway obstruction in children with micrognathia: a systematic review” in 2016, which found that mandibular distraction osteogenesis (MDO) was highly successful (95.5 percent success rate) in preventing tracheotomies in children with micrognathia who had poor conservative treatment results. MDO had a lower success rate (81 percent) in facilitating decannulation of children depending on tracheotomy. The most common causes of failure are severe preoperative gastro-oesophageal reflux disease, swallowing dysfunction and tracheotomy-related complications. The long-term complications caused by MDO need to be further investigated. Breugem et al. (17) published “Best Practices for the Diagnosis and Evaluation of Infants With Robin Sequence: A Clinical Consensus Report.” in 2016 and provided agreed-on recommendations for clinical features and evaluations of Robin Sequence(RS). The diagnostic points of RS are micrognathia, glossoptosis and airway obstruction. “Airway and Feeding Outcomes of Mandibular Distraction, Tongue-Lip Adhesion, and Conservative Management in Pierre Robin Sequence: A Prospective Study.” by Khansa et al. (18) in 2017 evaluated three approaches to the treatment of PRS in 2017: MDO, tongue-lip adhesion, and conservative management. The results suggested that conservative treatment was best suited to neonates with a stable airway in the side or prone position, who can tolerate oral feeding and gain weight, that tongue-Lip adhesion was best suited to neonates with a less stable airway or poor oral intake and an intermediate apnoea-hypopnoea index, and that MDO was suitable for neonates with a severely compromised airway and a severely underdeveloped mandible with a high apnoea-hypopnoea index.
In recent years, three keywords with burst related to craniomaxillofacial DO have emerged: obstructive sleep apnea, TMJ ankylosis, and cleft lip and palate.
The most cited studies related to obstructive sleep apnea focus on the use of MDO in treatment of pediatric micrognathia such as PRS, bilateral hemifacial microsomia (due to mandibular growth disturbance), Treacher Collins syndrome, Nager syndrome and so on (19). MDO gradually lengthens the mandible allowing the tongue and supraglottis to move forward (20), effectively increasing airway space in pediatric patients with micrognathia and airway obstruction, improving their airway obstruction, preventing tracheotomy and facilitating extubation during tracheotomy (21–23). Failure to extubate after MDO can be attributed to complications of the retraction process or inherent anatomical airway defects that are not detectable beforehand (20), such as the relatively low success rate of MDO-facilitated extubation in tracheotomized patients with complex congenital syndromes (24). However, in these publications with burst, there is no definitive evidence or clear recommendations regarding the osteotomy designs, the determination of whether a latency period is required, or the assessment of long-term stability, and there is no consensus on the precise indications and timing of MDO surgery (20).
There are some articles related to the use of distraction osteogenesis maxillary expansion (DOME) in midfacial dysostosis. Premature closure of the skull sutures, as seen in Crouzon, Apert, and Pfeiffer syndromes, causes midface recession and different sleep-related breathing disorders due to velopharyngeal obstruction in young patients and adults (20). DOME can drive the midface forward, but there is less evidence for the efficacy of this approach in airway obstruction (19).
Recent related research has focused on the specific mechanisms and improved procedures of DO for the treatment of OSA. MDO is widely thought to increase airway space by gradually lengthening the mandible, allowing the tongue and supraglottis to move forward, with studies focusing on the specific mechanism of the change in airway morphology (20). A recent analysis based on computational fluid dynamics has revealed that DO may be effective in treating OSA by widening the upper airway and reducing inspiratory resistance (25). In advancement of midface, the magnitude of horizontal advancement correlates closely with the increase in airway volume and improvement in the apnea hypoventilation index (26). Regarding the modified DO procedure for the treatment of OSA, Counterclockwise craniomaxillofacial distraction osteogenesis (C3DO) is indicated for patients with complex and severe syndromes such as maxillary defects, high occlusal plane, and severe airway obstruction (27). The facial skeletal deformity and expansion of upper airway capacity can be addressed by turning the subcranial complex en bloc around the nasofrontal junction (27). A variation of the previously performed Le Fort III distraction surgery, Le Fort II distraction with zygomatic relocation, allows for a clockwise rotation of the jaws while advancing the midface horizontally (26) to correct the patient's abnormal facial proportions (28, 29). Rare complications following DO, such as retractor breakage, have also received attention (30).
A few successful cases of MDO reconstruction of the TMJ in patients with TMJ ankylosis have been reported in studies. Compared to autologous grafts, MDO allows for shorter hospital admissions and operation times, reduces surgical risks and recurrence rates, and allows the patient to perform jaw movements including opening and closing the mouth and chewing during the process of bone production (31, 32). MDO can be used alone to reconstruct the TMJ or in combination with arthroplasty (33, 34). External distractions are used in most cases, but intraoral distraction osteogenesis followed by arthroplasty, in conjunction with physiotherapy, has been used to successfully treat TMJ ankylosis in combination with endoscopic techniques (35). A recent study performed a finite element analysis of intraoral and extraoral distraction devices and found that an internal device provided better bone protection and reduced stress on the mandible, whereas an external device allowed for greater traction length, making the use of an intraoral device more recommended (36). However, there was no difference in assessing quality of life (QoL) when utilizing an exterior or internal distractor (37). In terms of recently applied modifications, reverse sagittal split can be used when it is not an option for the treatment of dentofacial malocclusion after gap arthroplasty due to poor proximal control, concerns about poor split and financial constraints (38), bidirectional distractors and concomitant neocallous moulding (CM) can be used in high-angle facial types to prevent an anterior open bite (39) and bring about better Qol results (37), and the placement of microimplants in the jaw bones can also help control the direction of distraction (40).
In the most referenced CLP research, the efficacy of DOME in treating severe maxillary hypoplasia in patients with cleft lip and palate (CLP) was assessed (41, 42). In contrast to DO, conventional osteotomy for the treatment of deformities in CLP patients with severe maxillary hypoplasia often require simultaneous mandibular osteotomy, which affects the aesthetics of the lower face (42, 43). The anterior displacement of the upper jaw may also have an adverse effect on pronunciation, and traditional osteotomy has a high recurrence rate (42, 43). DOME using adjustable rigid external distraction (RED) allows predictable control of the distraction process. Greater maxillary advancement is obtained (42) and the technique is relatively simple, requiring no bone graft or rigid fixation hardware and providing better long-term stability (41, 44). The interdental DO technique can effectively reduce alveolar clefts/fistulas and reconstruct alveolar defects in CLP patients with alveolar defects (45). This is performed by distracting and transporting the distal section of the osteotomized dental arch towards the cleft or defect using a toothborne intraoral distraction device (45). However, there is still a lack of studies that evaluate the efficacy of treatment in terms of changes in the soft to hard tissue ratio in 3D imaging.
Recently, researchers have focused on the molecular mechanism of DOME in the treatment of cleft lip and palate, suggesting that fibroblasts in the zygomatic maxillary suture transform into a vascular endothelium-like state in response to mechanical stimulation, promoting angiogenesis under tension, while secreting signal molecules to interact with other cell types and promote osteogenesis (46, 47). Further research is needed, however, on the mechanistic immune status of craniofacial sutures and the interactions between immune cells and other cell types (48). In terms of improved technology, 3D virtual surgical planning (VSP) and CAD/CAM technology can effectively reduce the total treatment time and allow patients to obtain a class I occlusion at the conclusion of the distraction (48) and the The use of a tooth-borne intraoral device in conjunction with the Mid-Maxillary Osteodistraction (MMOD) technique has been shown to be effective (49). However, the long-term stability of these improved techniques remains to be investigated. Furthermore, the importance of presurgical education for patients undergoing RED for maxillary advancement has been highlighted, and it has been discovered that presurgical education can significantly reduce the length of hospital stay and narcotic pain medication use (50).
There are still some limitations to this study. Firstly, all data for this study are solely acquired from WOSCC. Then, due to the lack of technical approach to combine data from different literature databases in CiteSpace and VOSviewer, and language restrictions in the WOSCC database, only English publications were obtained through literature search. Finally, due to technical defects of the CiteSpace and VOSviewer as the bibliometric software, self-citation could not be eliminated, potentially resulting in bias. However, as far as we are aware, this study is the first bibliometric analysis to focus on craniomaxillofacial DO and provides relevant researchers with a comprehensive insight of the trends and current status of craniomaxillofacial DO research.
Based on the bibliometric and visual analysis of the research on craniomaxillofacial DO from 2000 to 2021, the findings can be summarized as follows:
(1) The number of publications on craniomaxillofacial DO has increased significantly since 2000 till now, and there was a boost increase in annual citation times in 2021.
(2) The United States, the People's Republic of China, and Italy produce the great majority of publications. Of all the institutions, University of Milan and University of Bologna are the most influential in this field. McCarthy JG is the most influential author.
(3) The research hotspots have shifted from maxillofacial defect repair and dental implant-related alveolar bone augmentation to syndromes resulting from craniomaxillofacial developmental defects. Obstructive sleep apnea, TMJ ankylosis and cleft lip and palate are potential research direction in this field. Future research should concentrate on the precise indications and timing of craniomaxillofacial DO, as well as the long-term outcomes of various modified procedures.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
EL conceived and designed the structure of this manuscript and revised the paper. ZL, JY, CZ and YL wrote the paper. All authors contributed to the article and approved he submitted version.
This study was supported by Grants from the NSFC 81970917 and Research and Develop Program, West China Hospital of Stomatology Sichuan University, RD-03-202102.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.932164/full#supplementary-material.
1. Ilizarov GA. The tension-stress effect on the genesis and growth of tissues. Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. (1989) 238:249–81. doi: 10.1097/00003086-198901000-00038
2. McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. (1992) 89(1):1–8; discussion 9–10. doi: 10.1097/00006534-199289010-00001
3. Tong H, Liu L, Tang X, Song T, Yin N, Zhang Z, et al. Midface distraction osteogenesis using a modified external device with elastic distraction for crouzon syndrome. J Craniofac Surg. (2017) 28(6):1573–7. doi: 10.1097/SCS.0000000000003377
4. Akizuki T, Komuro Y, Ohmori K. Distraction osteogenesis for craniosynostosis. Neurosurg Focus. (2000) 9(3):e1. doi: 10.3171/foc.2000.9.3.2
5. Urban IA, Montero E, Monje A, Sanz-Sánchez I. Effectiveness of vertical ridge augmentation interventions: a systematic review and meta-analysis. J Clin Periodontol. (2019) 46(Suppl 21):319–39. doi: 10.1111/jcpe.13061
6. Toledano-Serrabona J, Sánchez-Garcés MÁ, Sánchez-Torres A, Gay-Escoda C. Alveolar distraction osteogenesis for dental implant treatments of the vertical bone atrophy: a systematic review. Med Oral Patol Oral Cir Bucal. (2019) 24(1):e70–5. doi: 10.4317/medoral.22750
7. Suh J, Choi TH, Baek SH, Kim JC, Kim S. Mandibular distraction in unilateral craniofacial microsomia: longitudinal results until the completion of growth. Plast Reconstr Surg. (2013) 132(5):1244–52. doi: 10.1097/PRS.0b013e3182a48cf9
8. Saman M, Abramowitz JM, Buchbinder D. Mandibular osteotomies and distraction osteogenesis: evolution and current advances. JAMA Facial Plast Surg. (2013) 15(3):167–73. doi: 10.1001/jamafacial.2013.44
9. Gosain AK. Plastic surgery educational foundation DATA committee. Distraction osteogenesis of the craniofacial skeleton. Plast Reconstr Surg. (2001) 107(1):278–80. doi: 10.1097/00006534-200101000-00050
10. Hu S, Alimire A, Lai Y, Hu H, Chen Z, Li Y. Trends and frontiers of research on cancer gene therapy from 2016 to 2020: a bibliometric analysis. Front Med (Lausanne). (2021) 8:740710. doi: 10.3389/fmed.2021.740710
11. Jiang Z, Wu C, Hu S, Liao N, Huang Y, Ding H, et al. Research on neck dissection for oral squamous-cell carcinoma: a bibliometric analysis. Int J Oral Sci. (2021) 13(1):13. doi: 10.1038/s41368-021-00117-5
12. Chen C. Citespace II: detecting and visualizing emerging trends and transient patterns in scientific literature. J Am Soc Inf Sci Technol. (2006) 57(3):359–77. doi: 10.1002/asi.20317
13. McCarthy JG, Stelnicki EJ, Mehrara BJ, Longaker MT. Distraction osteogenesis of the craniofacial skeleton. Plast Reconstr Surg. (2001) 107(7):1812–27. doi: 10.1097/00006534-200106000-00029
14. Chiapasco M, Romeo E, Casentini P, Rimondini L. Alveolar distraction osteogenesis vs. vertical guided bone regeneration for the correction of vertically deficient edentulous ridges: a 1-3-year prospective study on humans. Clin Oral Implants Res. (2004) 15(1):82–95. doi: 10.1111/j.1600-0501.2004.00999.x
15. Flores RL, Tholpady SS, Sati S, Fairbanks G, Socas J, Choi M, et al. The surgical correction of Pierre Robin sequence: mandibular distraction osteogenesis versus tongue-lip adhesion. Plast Reconstr Surg. (2014) 133(6):1433–9. doi: 10.1097/PRS.0000000000000225
16. Breik O, Tivey D, Umapathysivam K, Anderson P. Mandibular distraction osteogenesis for the management of upper airway obstruction in children with micrognathia: a systematic review. Int J Oral Maxillofac Surg. (2016) 45(6):769–82. doi: 10.1016/j.ijom.2016.01.009
17. Breugem CC, Evans KN, Poets CF, Suri S, Picard A, Filip C, et al. Best practices for the diagnosis and evaluation of infants with robin sequence: a clinical consensus report. JAMA Pediatr. (2016) 170(9):894–902. doi: 10.1001/jamapediatrics.2016.0796
18. Khansa I, Hall C, Madhoun LL, Splaingard M, Baylis A, Kirschner RE, et al. Airway and feeding outcomes of mandibular distraction, tongue-lip adhesion, and conservative management in pierre robin sequence: a prospective study. Plast Reconstr Surg. (2017) 139(4):975e–83e. doi: 10.1097/PRS.0000000000003167
19. Randerath WJ, Verbraecken J, Andreas S, Bettega G, Boudewyns A, Hamans E, et al. Non-CPAP therapies in obstructive sleep apnoea. Eur Resp J. (2011) 37(5):1000–28. doi: 10.1183/09031936.00099710
20. Ow ATC, Cheung LK. Meta-analysis of mandibular distraction osteogenesis: clinical applications and functional outcomes. Plast Reconstr Surg. (2008) 121(3):54E–69E. doi: 10.1097/01.prs.0000299285.97379.35
21. Denny AD, Talisman R, Hanson PR, Recinos RF. Mandibular distraction osteogenesis in very young patients to correct airway obstruction. Plast Reconstr Surg. (2001) 108(2):302–11. doi: 10.1097/00006534-200108000-00004
22. Cohen SR, Simms C, Burstein FD. Mandibular distraction osteogenesis in the treatment of upper airway obstruction in children with craniofacial deformities. Plast Reconstr Surg. (1998) 101(2):312–8. doi: 10.1097/00006534-199802000-00008
23. Monasterio FO, Drucker M, Molina F, Ysunza A. Distraction osteogenesis in Pierre Robin sequence and related respiratory problems in children. J Craniofac Surg. (2002) 13(1):79–83. doi: 10.1097/00001665-200201000-00018
24. Mandell DL, Yellon RF, Bradley JP, Izadi K, Gordon CB. Mandibular distraction for micrognathia and severe upper airway obstruction. Arch Otolaryngol Head Neck Surg. (2004) 130(3):344–8. doi: 10.1001/archotol.130.3.344
25. Wang R, Xu S, Yang R. What is the impact of distraction osteogenesis on the upper airway of hemifacial microsomia patient with obstructive sleep apnea: a case report. Eur J Med Res. (2021) 26:76. doi: 10.1186/s40001-021-00547-1
26. Liu MT, Kurnik NM, Mercan E, Susarla SM, Purnell CA, Hopper RA. Magnitude of horizontal advancement is associated with apnea hypopnea index improvement and counter-clockwise maxillary rotation after subcranial distraction for syndromic synostosis. J Oral Maxillofac Surg. (2021) 79(5):1133.e1–e16. doi: 10.1016/j.joms.2020.12.037
27. Hopper RA, Wang HD, Mercan E, Kapadia H. Counterclockwise craniofacial distraction osteogenesis. Clin Plast Surg. (2021) 48(3):445–54. doi: 10.1016/j.cps.2021.02.006
28. Hopper RA, Wang HD, Mercan E. Le fort II distraction with simultaneous zygomatic repositioning. Clin Plast Surg. (2021) 48(3):487–96. doi: 10.1016/j.cps.2021.02.007
29. Purnell CA, Evans M, Massenburg BB, Kim S, Preston K, Kapadia H, et al. Lefort II distraction with zygomatic repositioning versus Lefort III distraction: a comparison of surgical outcomes and complications. J Cranio-Maxillofac Surg. (2021) 49(10):905–13. doi: 10.1016/j.jcms.2021.03.003
30. Dasukil S, Verma S, Boyina KK, Jena AK. Unpredicted bilateral device breakage during active phase of mandibular distraction: a case report and literature review. J Stomatol Oral Maxillofac Surg. (2021) 122(3):319–24. doi: 10.1016/j.jormas.2020.08.011
31. Khadka A, Hu J. Autogenous grafts for condylar reconstruction in treatment of TMJ ankylosis: current concepts and considerations for the future. Int J Oral Maxillofac Surg. (2012) 41(1):94–102. doi: 10.1016/j.ijom.2011.10.018
32. Lopez EN, Dogliotti PL. Treatment of temporomandibular joint ankylosis in children: is it necessary to perform mandibular distraction simultaneously? J Craniofac Surg. (2004) 15(5):879–84. doi: 10.1097/00001665-200409000-00037
33. StuckiMcCormick SU. Reconstruction of the mandibular condyle using transport distraction osteogenesis. J Craniofac Surg. (1997) 8(1):48–52. doi: 10.1097/00001665-199701000-00016
34. Dean A, Alamillos F. Mandibular distraction in temporomandibular joint ankylosis. Plast Reconstr Surg. (1999) 104(7):2021–31. doi: 10.1097/00006534-199912000-00012
35. Elgazzar RF, Abdelhady AI, Saad KA, Elshaal MA, Hussain MM, Abdelal SE, et al. Treatment modalities of TMJ ankylosis: experience in Delta Nile, Egypt. Int J Oral Maxillofac Surg. (2010) 39(4):333–42. doi: 10.1016/j.ijom.2010.01.005
36. Elhadidi YN, Askar MG, El Sayed AGA. The stress concentration and biomechanical properties of the intra-oral distractors and the extra-oral distractors used in treatment of post ankylosis facial asymmetric patients: a finite element analysis study. J Craniofac Surg. (2021) 32(6):1977–80. doi: 10.1097/SCS.0000000000007320
37. Vignesh U, Mehrotra D, Bhave SM, Singh PK. Quality of life after distraction osteogenesis in TMJ ankylosis patients. Oral Surg Oral Med Oral Pathol Oral Radiol. (2021) 131(3):295–303. doi: 10.1016/j.oooo.2020.09.005
38. Bansal V, Mowar A, Gupta S, Amit K. A clinical re-evaluation of an unexplored technique for post gap arthroplasty retrognathic mandible. J Maxillofac Oral Surg. (2021). [cited 2022 Apr 11].doi: 10.1007/s12663-021-01539-8.
39. Garg N, Anchlia S, Dhuvad J, Gosai H, Chaudhari P. Bilateral biplanar distraction osteogenesis in facial deformity secondary to temporomandibular ankylosis. J Maxillofac Oral Surg. (2021). [cited 2022 Apr 11]. doi: 10.1007/s12663-020-01502-z
40. Kim HJ, Park HS. Treatment of severe mandibular deficiency following TMJ ankyloses by distraction osteogenesis and orthodontic treatment with microimplants. J Orthod. (2021). 14653125211059840. doi: 10.1177/14653125211059839
41. Figueroa AA, Polley JW, Friede H, Ko EW. Long-term skeletal stability after maxillary advancement with distraction osteogenesis using a rigid external distraction device in cleft maxillary deformities. Plast Reconstr Surg. (2004) 114(6):1382–92. doi: 10.1097/01.PRS.0000138593.89303.1B
42. Figueroa AA, Polley JW. Management of severe cleft maxillary deficiency with distraction osteogenesis: procedure and results. Am J Orthod Dentofac Orthop. (1999) 115(1):1–12. doi: 10.1016/S0889-5406(99)70310-0
43. Cheung LK, Chua HDP. A meta-analysis of cleft maxillary osteotomy and distraction osteogenesis. Int J Oral Maxillofac Surg. (2006) 35(1):14–24. doi: 10.1016/j.ijom.2005.06.008
44. Cheung LK, Chua HDP, Hagg MB. Cleft maxillary distraction versus orthognathic surgery: clinical morbidities and surgical relapse. Plast Reconstr Surg. (2006) 118(4):996–1008. doi: 10.1097/01.prs.0000232358.31321.ea
45. Liou EJW, Chen PKT, Huang CS, Chen YR. Interdental distraction osteogenesis and rapid orthodontic tooth movement: a novel approach to approximate a wide alveolar cleft or bony defect. Plast Reconstr Surg. (2000) 105(4):1262–72. doi: 10.1097/00006534-200004040-00002
46. Li G, Liang W, Ding P, Zhao Z. Sutural fibroblasts exhibit the function of vascular endothelial cells upon mechanical strain. Arch Biochem Biophys. (2021) 712:109046. doi: 10.1016/j.abb.2021.109046
47. Liang W, Zhao E, Li G, Bi H, Zhao Z. Suture cells in a mechanical stretching niche: critical contributors to trans-sutural distraction osteogenesis. Calcif Tissue Int. (2022) 110(3):285–93. doi: 10.1007/s00223-021-00927-z
48. Gerbino G, Autorino U, Giaccone E, Novaresio A, Ramieri G. Virtual planning and CAD/CAM-assisted distraction for maxillary hypoplasia in cleft lip and palate patients: accuracy evaluation and clinical outcome. J Cranio-MaxilloFac Surg. (2021) 49(9):799–808. doi: 10.1016/j.jcms.2021.03.004
49. Perera WKL, Jayawardana RADTM, Pathirage SL, Dias DK, Dasanayaka DARK. Occlusal and functional improvement of patients with midfacial hypoplasia corrected using intraoral tooth-borne mid-maxillary osteodistractors at teaching hospital-karapitiya, Sri Lanka. Cleft Palate-Craniofac J. (2021) 58(9):1160–8. doi: 10.1177/1055665620980220
50. Kim EN, Moss WD, Rosales MN, Lyon N, Lotz A, Yamashiro DK, et al. Multidisciplinary presurgical education: clinical impact on children with orofacial clefts undergoing maxillary distraction via rigid external distraction. Cleft Palate-Craniofac J. 10556656211055412. doi: 10.1177/10556656211055411
Keywords: bibliometrics, CiteSpace, distraction osteogenesis, craniomaxillofacial dysplasia, bone defects, orthognathic surgery
Citation: Liu Z, Yang J, Zhou C, Liu Y and Luo E (2022) A bibliometric analysis of research on craniomaxillofacial distraction osteogenesis from 2000 to 2021. Front. Surg. 9:932164. doi: 10.3389/fsurg.2022.932164
Received: 29 April 2022; Accepted: 18 July 2022;
Published: 1 August 2022.
Edited by:
Alexander Hemprich, University of Leipzig, GermanyReviewed by:
Peter Anderson, University of Adelaide, Australia© 2022 Liu, Yang, Zhou, Liu and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: En Luo bHVvZW41MjExMjVAc2luYS5jb20=
†These authors have contributed equally to this work
Specialty Section: This article was submitted to Reconstructive and Plastic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.