- 1Department of Anorectal Surgery, The Affiliated Hospital of Nanjing University of Chinese Medicine, Nanjing, China
- 2Department of Anorectal Surgery, The Affiliated Xing Tai People Hospital of Hebei Medical University, Xingtai, China
- 3Department of Colorectal Surgery, The Sixth Affiliated Hospital (Gastrointestinal & Anal Hospital), Sun Yat-sen University, Guangzhou, China
Background: The relationship between hemorrhoid recurrence and poor defecation habits is poorly understood. This study aimed to analyze the effects of poor defecation habits on postoperative hemorrhoid recurrence.
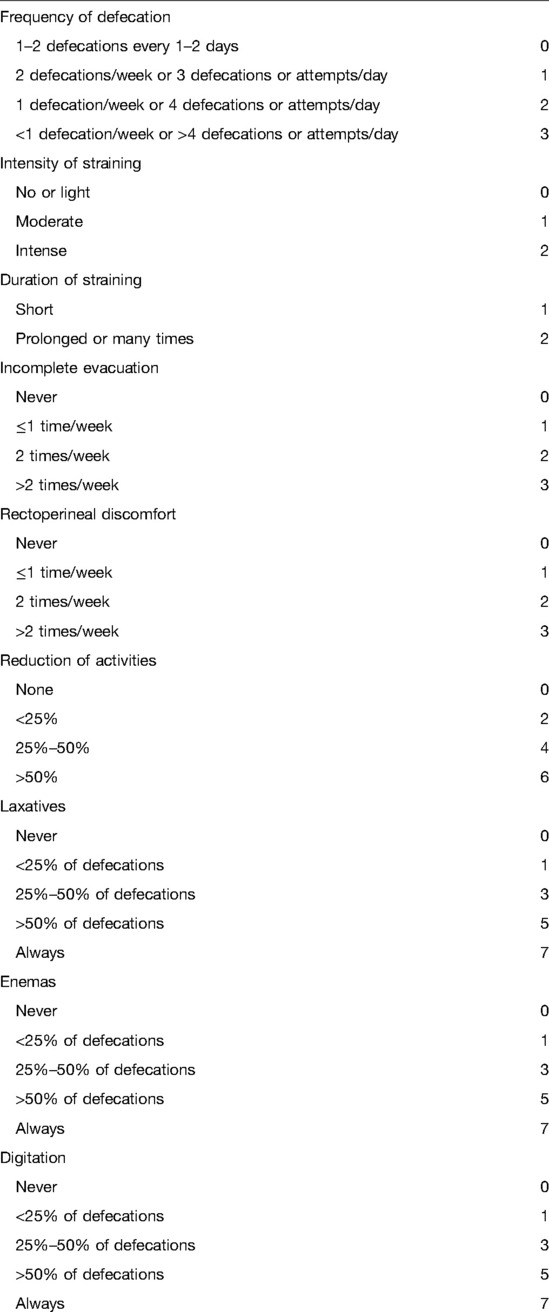
Materials and Method: We performed a retrospective study on 1,162 consecutive patients who underwent a surgical procedure for hemorrhoids at the Sixth Affiliated Hospital of Sun Yat-Sen University from December 2016 to May 2020. All patients were followed for 12 months post-operatively. Patients were monitored for disease recurrence. Patient defecation habits were assessed using an obstructive defecation syndrome (ODS) score.
Results: Patients with a score of 0–4 had a mild defecation disorder, 5–8 a moderate defecation disorder, and 9 or more ODS. Of the 1,162 patients, 1,144 (98.45%) had a mild defecation disorder, 13 (1.12%) had a moderate defecation disorder, and 9 (0.43%) had ODS. Older patients were significantly more likely to have worse defecation habits (P < 0.001). A higher ODS score correlated with a higher maximum anal squeeze pressure (P = 0.07) and a more severe inability for the anus to relax during simulated evacuation (P = 0.002). The maximum rectum threshold was also found to be the highest in ODS patients (P = 0.010). The proportion of Procedure for prolapsing hemorrhoids (PPH) was the highest in the moderate defecation disorder group (53.85), followed by the ODS group (40.00) and the mild defecation disorder group (P = 0.023). Recurrence occurred in 5.51% of patients in the mild defecation disorder group, 38.46% of the moderate defecation disorder group, and 60% of the ODS group (P < 0.001). Multivariate analysis confirmed a higher ODS score (P < 0.001) was an independent predictor of recurrence. Furthermore, patients who occasionally exercised (P = 0.01) and patients who exercised regularly (P = 0.021) were less likely to have a recurrence.
Conclusion: Patients with unresolved defecation disorders are more likely to have their hemorrhoids recur and are unlikely to be satisfied with surgical management.
Introduction
Hemorrhoids are the most common anorectal disease and have a considerable impact on health care expenditure (1). The prevalence of hemorrhoids in the general population is as high as 50% (2), affecting a considerable proportion of adults of all ages and genders (3). Current causes of hemorrhoids include chronic straining during defecation, lack of physical exercise, diarrhea, pregnancy, and inadequate fiber intake (4). There is a close link between hemorrhoids and constipation (5, 6). Hard or large stools and exertion during defecation are associated with an increased prevalence of hemorrhoids. Bowel habit regulation is essential to managing hemorrhoids (7–9). For instance, oral fiber is adjusted for constipation symptoms (5, 10) and flavonoids decrease the risk and recurrence rate of hemorrhoids (11).
Patients diagnosed with obstructive defecation syndrome (ODS) usually have long-standing constipation. The surgical treatment of defecation disorders is still very controversial, with unacceptable effects on patient quality of life (12). Hemorrhoid management is usually conservative, and only 20% of patients require surgical management (13). Similarly, before developing hemorrhoidal symptoms patients usually suffer from difficulty defecating (14). Many patients undergo surgery for this, often without treating the underlying cause of their symptoms. Unsurprisingly, the postoperative recurrence rate of hemorrhoids is still high (15, 16), with multiple studies attributing recurrence to surgical technique (17, 18).
Although surgical technique is widely accepted as the main reason for hemorrhoid treatment failure, the relationship between poor defecation habits and hemorrhoid recurrence is poorly understood. This study aimed to analyze the effects of poor defecation habits on postoperative hemorrhoid recurrence. We hypothesized that patients with more severe defecation disorders would be more likely to see their hemorrhoids recur following surgery. Patients with a severe defecation disorder are less likely to be satisfied with their surgical outcome regardless of the method used to perform the surgery.
Materials and Methods
Study Design and Participant Selection
The unit protocol and study format were approved by the Sixth Affiliated Hospital of Sun Yat-Sen University (Approval code: 2022ZSLYEC-096). This retrospective study was performed on 1,162 consecutive patients who underwent a surgical procedure for hemorrhoids from December 2016 to May 2020 (Figure 1). All patients were followed for 12 months post-operatively. Inclusion criteria were age > 18 and ≤80 years old, a clinical diagnosis of hemorrhoids, and surgery performed by a surgeon with at least 5 years of experience with all three common surgical techniques. Exclusion criteria were previous hemorrhoidal surgical management, malignancies, fecal incontinence, pregnancy, and severe psychiatric disorders.
Preoperative Preparation, Surgical Methods
All patients underwent routine pre-operative bloodwork, electrocardiograms, and chest X-rays to rule out surgical contraindications. They also underwent a pre-operative colonoscopy to exclude more serious diseases such as inflammatory bowel disease, proliferative polyps, and colorectal cancer. All patients underwent pre-operative anorectal manometry, which was preceded by a phosphate enema. Anorectal manometry was performed with patients in the left lateral position with their hips flexed. Anorectal manometric parameters such as anorectal pressure, rectal sensation, and neural reflexes were recorded. All patients received a pre-operative bowel enema the night before surgery, and a prophylactic antibiotic was injected 30 min before the surgical procedure was started. Most patients had spinal anesthesia and were placed in the jackknife or left lateral position. Tape was attached to both sides of the buttocks to expose the anus.Some other patients underwent local anesthesia, because these patients were able to tolerate the relatively simple procedure under local anesthesia. General anesthesia was performed in some patients because of lumbar lesions, coagulopathy, or psychosomatic disorders.
Surgical Modalities
Many patients had a combination of surgical therapies. The Goligher classification is the most widely used classification for HD. Surgical management was performed based on the Goligher Classification of hemorrhoids (19), the type of health insurance patient’s choice. Patients with bleeding hemorrhoids underwent either Hemorrhoid injection sclerotherapy (IS)or rubber band ligation (RBL), which was performed either in the treatment room using 1% lidocaine as a local anesthetic or in the operation theater under spinal anesthesia. IS and RBL were used for the treatment of I, II, and III-degree HD. A recent multicentre study showed that Sclerotherapy with 3% polidocanol foam is a safe, effective, painless, repeatable and low-cost procedure in patients with bleeding hemorrhoids, especially in the treatment of 2nd-degree hemorrhoids (20). After a thorough digital rectal examination (DRE), an anoscope was inserted to fully expose the hemorrhoids. Sclerotherapy was mainly performed if the patient suffered from hemorrhoidal bleeding. It was done using “Shaobei” (Taifeng, Henan, China) and lidocaine in a 1:1 ratio. The mixture was injected into the submucosa of each hemorrhoid tissue, paying attention to avoid any blood vessels. The total injection volume was generally less than 20 mL. Rubber band ligation was used on patients with bleeding hemorrhoids. It was performed using a ligation device to ligate the hemorrhoid, bleeding point, or tissue superior to the hemorrhoid. There were generally less than four ligation sites. Procedure for prolapsing hemorrhoids (PPH) and the Milligan-Morgan hemorrhoidectomy (MMH) was indication for symptomatic III- and IV-degree HD. Preoperative clinical evaluation is essential for HD patient treatment and outcome and classification systems are useful for the therapeutic choice (21). Our patients with obvious protrusions underwent PPH or MMH, which were usually performed under spinal anesthesia. Endotracheal anesthesia was used in patients who had any contraindications to spinal anesthesia, such as a coagulopathy. The patient was usually in the prone jackknife position or the lithotomy position during surgery. After a thorough DRE and insertion of an anal speculum, the surgeon identified the hemorrhoids that were to be excised. PPH was performed as previously described (22). For MMH, tissue forceps were used to grasp and lift the external hemorrhoid towards the surgeon at the mucocutaneous junction. Monopolar electrocautery or a pair of scissors were used to make a V-shaped incision in the skin around the base of hemorrhoid. The dissection continued into the submucosal space to peel the entire hemorrhoid from its bed. The pedicle was ligated, and the distal part of the hemorrhoid was excised. All of the other hemorrhoids were similarly treated, leaving a skin bridge in-between to avoid stenosis. Large wounds were closed and sutured with 3-0 absorbable thread for aesthetic reasons. An absorbable sponge dressing was placed in the anal canal when the procedure was completed. Post-operatively, the patient was advised to take an adequate amount of dietary fiber and water.
Follow-Up
All cases were followed for at least 12 months from the date of surgery for any disease recurrence. Recurrence was defined as unresolved bleeding or prolapse at the site where surgical management was performed. It is difficult for patients to accurately describe their defecation habits. Given the anatomic, functional, and sometimes psychological factors involved in defecation there may be a variety of clinical presentations of ODS. We therefore used the ODS severity index to evaluate patients’ defecation habits (12). The ODS score (23, 24) was chosen to assess these patients’ defecation habits (Table 1). A score of 0–4 was classified as a mild defecation disorder, 5–8 as a moderate defecation disorder, and 9 or more as ODS.
Statistical Methods
The statistical analyses were performed using SPSS 26.0 (Armonk, NY, USA). All tests were two-way, and P < 0.05 was considered statistically significant. Mean ± standard deviation was used to describe continuous variables, frequency and frequency were used to describe categorical variables, and the analysis of variance or chi-square tests were used to identify statistically significant differences between groups. Univariate logistic regressions were used to identify correlations between various factors and hemorrhoid recurrence. The univariate results were included in a multivariate logistic regression model for further analysis, and stepwise regression was used to screen variables.
Results
Patient Demographics
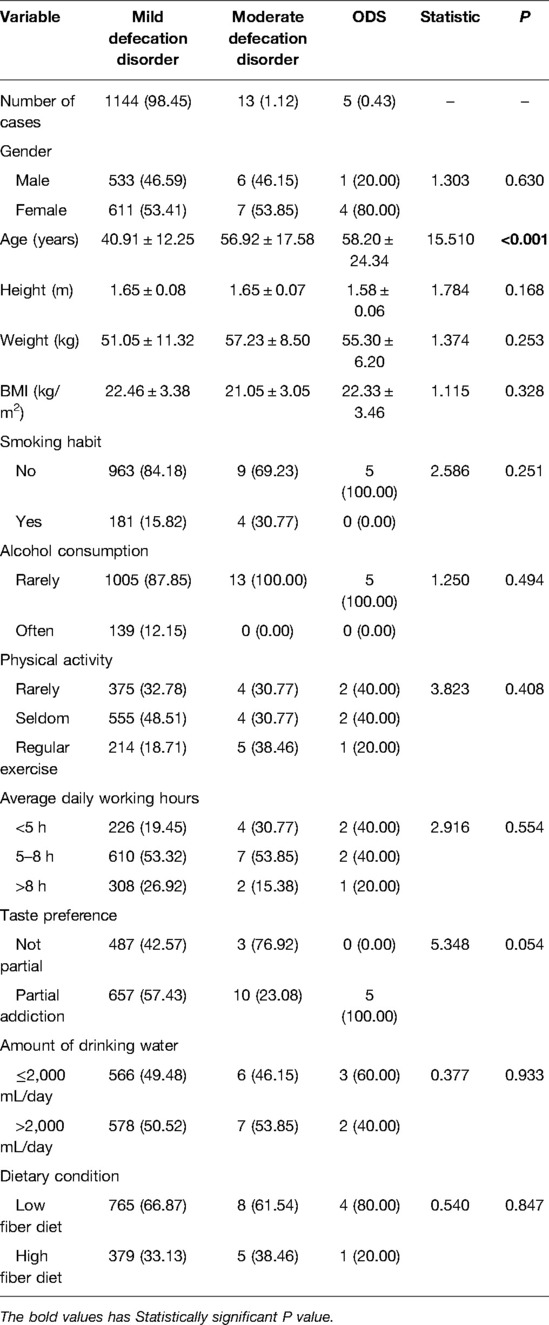
A total of 1,162 consecutive patients underwent a hemorrhoidectomy at our institution and followed up for at least 12 months. Of the 1,162 patients, 1,144 (98.45%) had a mild defecation disorder, 13 (1.12%) had a moderate defecation disorder and 9 (0.43%) had ODS. Older age was significantly correlated with worsen defecation habits (P < 0.001) (Table 2).
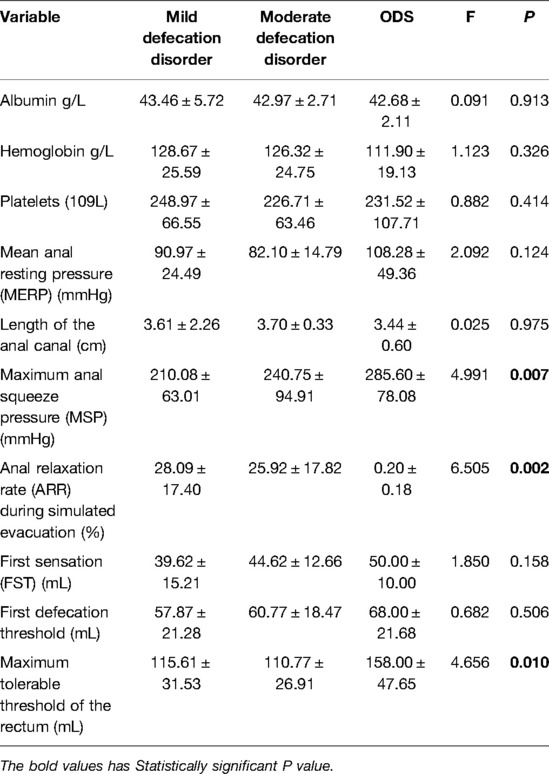
Pre-Operative Anorectal Manometry
We aimed to understand the effects of poor defecation habits on pre-operative anorectal function (Table 3). A higher ODS score correlated with a higher maximum anal squeeze pressure (P = 0.07) and a more severe inability for the anus to relax during simulated evacuation (P = 0.002). ODS patients also had the highest maximum rectum threshold (P = 0.010).
Goligher Classification and Surgical treatment
1 RBL procedure and 11 IS procedures were done spinal anesthesia due to lumbar lesions, coagulopathy, or psychosomatic disorders. 5 MMH procedures were performed under local anesthesia because these patients were able to tolerate the relatively simple procedure under local anesthesia. Endotracheal intubation was performed in 12 combined PPH and MMH procedures, 9 combined MMH and RBL procedures, and 5 MMH procedure because of lumbar lesions, coagulopathy, or psychosomatic disorders. The other 1,119 patients routinely received spinal anesthesia.
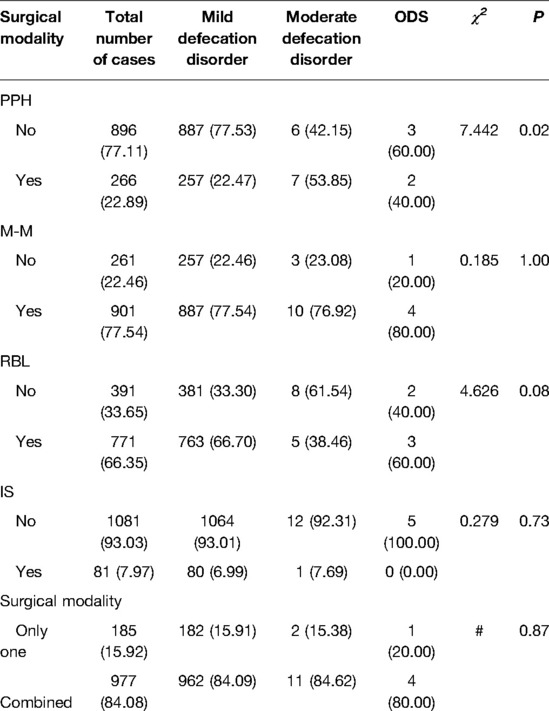
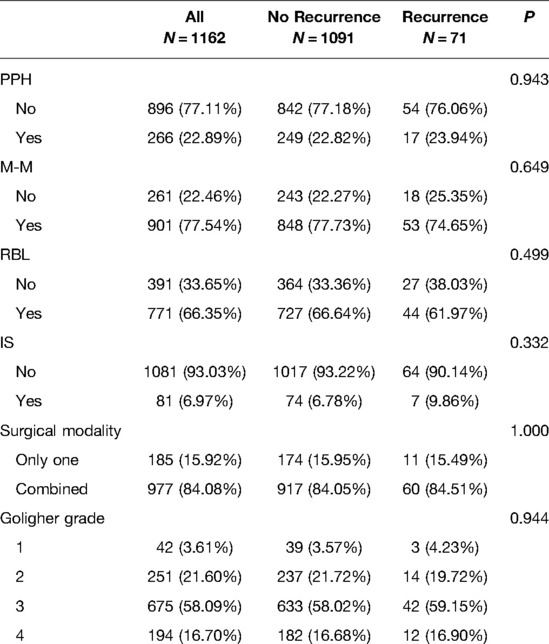
Most of the low defecation disorder patients underwent an MMH procedure (77.54%) while sclerotherapy was least utilized (7.97%). Only the use of PPH was statistically significant between groups. The proportion of PPH was the highest in the moderate defecation disorder group (53.85%), followed by the ODS group (40.00%) and the mild defecation disorder group (P = 0.023). The proportion of single operation and combined operation was 185 (15.92%) and 977 (84.08%) respectively. The proportion of single operation and compound operation in each group of defecation disorder was almost the same. (P = 0.876). Results are shown in Table 4. There was no statistical significance observed on the use of single or combined surgeries (P = 1.000). No statistical significance was observed among the four surgical methods _ PPH (P = 0.943), MMH (P = 0.649), RBL (P = 0.499), IS (P = 0.332). There was also no statistical significance observed between Goligher grade and recurrence rates (P = 0.944) (Table 5).
Unresolved Poor Defecation Habits and Hemorrhoids Recurrence
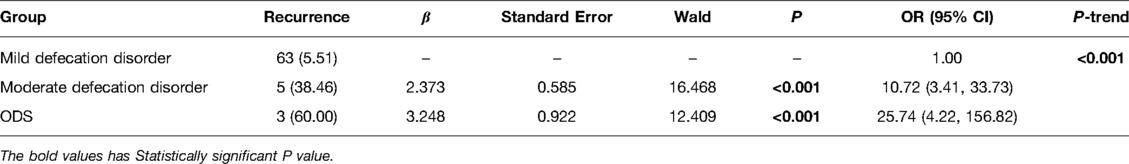
We assessed the impact of an unresolved defecation habit on hemorrhoidal recurrence using linear regression (Table 6). Recurrence occurred in 5.51% of the mild defecation disorder group, 38.46% of the moderate defecation disorder group, and 60% of the ODS group (P < 0.001).
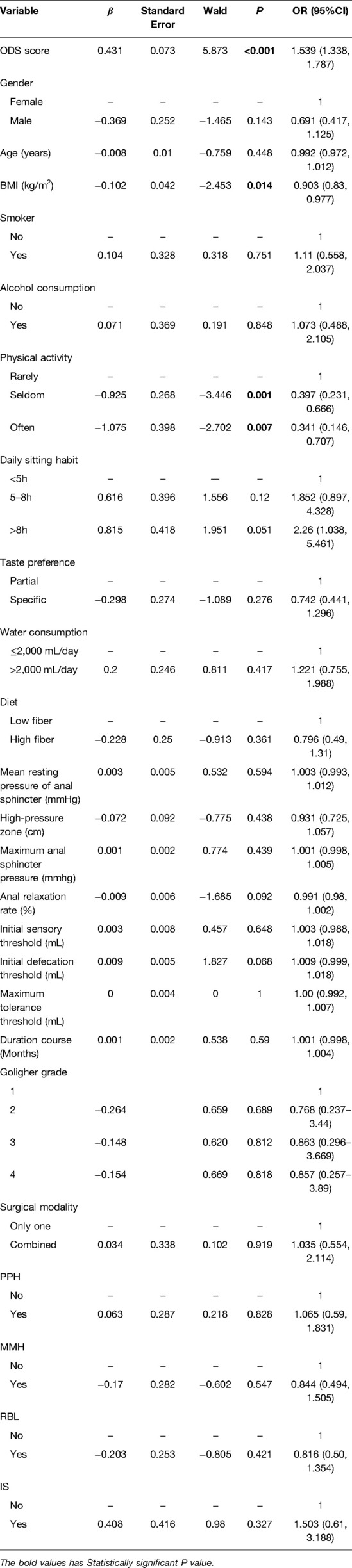
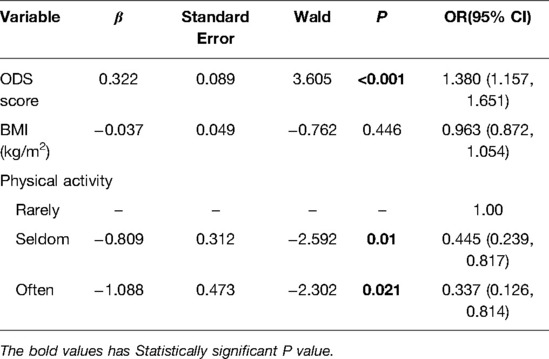
Analysis of Factors Influencing Hemorrhoids Recurrence
We aimed to identify factors associated with hemorrhoid recurrence. In a univariate analysis (Table 7), ODS score (P < 0.001), physical activity (P = 0.001), and BMI (P = 0.014)) were significantly associated with hemorrhoid recurrence. There was no statistical significance observed between recurrence and surgical modality (P = 0.919). Multivariate analysis (Table 8) confirmed that ODS score (OR = 1.380, P < 0.001) was independent risk factor for hemorrhoid recurrence. Every increment in the ODS score resulted in an increased risk of hemorrhoid recurrence of 1.38 times. Interestingly, the recurrence risk of patients who exercised occasionally was 0.445 and that of for those who exercised regularly was 0.337, implying that physical activity has a protective effect against hemorrhoid recurrence.
Discussion
The primary aim of this study was to understand if patients with unresolved poor defecation habits are at a higher risk of recurrence following hemorrhoidectomy. Our results show 1,144 (98.45%) had a mild defecation disorder, 13 (1.12%) had a moderate defecation disorder, and 9 (0.43%) had ODS. Older patients were significantly more likely to have worse defecation habits (P < 0.001). A higher ODS score correlated with a higher maximum anal squeeze pressure (P = 0.07) and a more severe inability for the anus to relax during simulated evacuation (P = 0.002). The maximum rectum threshold was also found to be the highest in ODS patients (P = 0.010). The proportion of (PPH) was the highest in the moderate defecation disorder group (53.85), followed by the ODS group (40.00) and the mild defecation disorder group (P = 0.023). Recurrence occurred in 5.51% of patients in the mild defecation disorder group, 38.46% of the moderate defecation disorder group, and 60% of the ODS group (P < 0.001). Multivariate analysis confirmed a higher ODS score (P < 0.001) was an independent predictor of recurrence. Furthermore, patients who occasionally exercised (P = 0.01) and patients who exercised regularly (P = 0.021) were less likely to have a recurrence.
The pathophysiology of hemorrhoids is not fully understood. A recent genome-wide association study (GWAS) analysis of 944,133 individuals found that hemorrhoids, which is a partially inherited disease, could be affected by functional gastrointestinal diseases (FGID) through genotype-driven modulation of Caja interstitial cell (ICC) function (25). ICCs are present throughout the human gastrointestinal tract and help in normal intestinal function and peristalsis. Few studies have shown differences in ICC distribution between ODS and non-ODS patients (26, 27), implying that patients with FGID are more likely to suffer from hemorrhoids.
It is difficult for patients to accurately describe their defecation habits. Given the anatomic, functional, and sometimes psychological factors involved in defecation there may be a variety of clinical presentations of ODS. It is therefore recommended that the ODS severity index is used evaluate patient defecation habits (12). ODS score describes a series of complex symptoms such as repeated straining, difficulty evacuating, using laxatives or an enema to defecate, using digital means, spending an excessive amount of time on the toilet during defecation, feelings of incomplete evacuation, perineal pain, and rectal discomfort (23, 24). Our results show that the defecation disorder score is an independent predictor for hemorrhoidal recurrence. Every one-point increment increased the risk of hemorrhoid recurrence by 1.38 times (P = <0.001). Furthermore, risk of hemorrhoid recurrence in the moderate defecation disorder group was 10.72 times higher, and 25.74 higher in the ODS group (P < 0.001). According to previous literature reports, key components of the pathogenesis and aggravation of hemorrhoids are rectal mucosal prolapse and increased anal pressure (28). Defecation disorder and pelvic floor disease cause the disintegration of the muscle fibers of Treitz (29). Straining during defecation may lead to excessive intra-abdominal pressure, rendering defecation ineffective and therefore multiple evacuations are required. Straining also impairs venous drainage of the hemorrhoids (30). Avoiding forced defecation has been shown to limit the prolapse of hemorrhoids (31).
We also found that physical activity has a protective effect against hemorrhoidal recurrence. Patients who exercised occasionally (P = 0.01) or regularly (P = 0.021) were less likely to have a recurrence. Mild physical activity can accelerate gastrointestinal transit and increase the stimulation of abdominal muscles, therefore aiding in the movement of stool into the rectum (32). However, high-intensity exercises can often lead to gastrointestinal distress when associated with either dehydration or increased intra-abdominal pressure (33). As noted by Marco et al. (5), we recommend that hemorrhoidal patients abandon a sedentary lifestyle and practice mild exercises such as walking, swimming, and yoga. This approach can result in improved circulation, strengthen the pelvic floor muscles, improve anorectal function, and prevent a defecation disorder.
We also found that older patients were more likely to have worse defecation habits (P < 0.001). The physiologic changes that result from poor defecation habits are not fully understood (34). Aging is associated with a higher prevalence of constipation (35) and impaired collagen quality. The ratio of connective tissue to muscle tissue increases with age and may play a role in the development of rectal mucosal or rectal prolapse in the elderly (36). This imbalance would result in the inability of the muscles to adequately contract to support the internal hemorrhoidal plexus (37). These factors would lead to sliding of the anal cushion, relaxation of the cushion’s connective tissue, and reduced venous return to the middle rectal vein and the superior rectal vein (38). A recent study (39) by Stanford Medical School showed that elderly patients had more severe prolapse symptoms than younger patients. With respect to anorectal function, we found that a higher ODS score was associated with a higher maximum anal squeeze pressure (P = 0.07), a more severe inability for the anus to relax during simulated evacuation (P = 0.002), and a higher maximum rectum threshold (P = 0.010). Increased maximum anal resting pressure, (40) increased internal anal sphincter activity, and a higher maximum rectum threshold (41) are common in patients with hemorrhoids and ODS.
Our results show a hemorrhoid recurrence rate of 6.11% following surgery, which is consistent with recurrence rates of 2% to 8% cited by previous clinical studies (42–44). There was no significant difference in recurrence rate based on the surgical procedure performed, which is consistent with the review by Naldini et al. (45). Patients with a moderate defecation disorder or ODS were more likely to undergo PPH. This is because these patients were more likely to have a higher degree of protrusion compared with mild defecation disorder patients.
Our findings are in line with those of a recent systematic review that reported that functional evacuation disorder, dyssynergic defecation, and abnormal balloon expulsion were more frequent in patients with hemorrhoids compared with healthy subjects (P < 0.0001) (46). The review concluded that it would be more effective to treat functional constipation instead of repeating RBL procedures. Pelvic floor physiotherapy was also deemed necessary to improving the long-term results of hemorrhoid treatment (14). We believe that it is necessary to evaluate the bowel habits of hemorrhoidal patients prior to surgery. We recommend performing preoperative anorectal manometry if the ODS score is 5 or more. Patients with defective anorectal function should be treated preoperatively conservatively or through biofeedback (47, 48). Patients should also be regularly followed for their symptoms. If poor defecation habits persist, defecation habit scores should be re-evaluated. Once these habits are improved, surgical management can be considered.
This study has several limitations. First, this is a retrospective study that has a small sample size of patients with a moderate defecation disorder or ODS. Prospective randomized controlled clinical trials need to be performed in the future. Secondly, we did not investigate whether there is a causal relationship or co-disease mechanism between ODS and hemorrhoids. Neural pathways and the role of the anal sphincter and pelvic floor muscles during defecation needs to be further studied. Further basic research projects on genetic and molecular mechanisms will be considered in future work.
Conclusion
The defecation habits of patients with hemorrhoids should be scored both perioperatively and postoperatively. They should be encouraged to normalize their defecation habit and pick the right exercise routine. A scoring system will help guide the preoperative conversation, analyze the patient’s prognosis, managing the patient’s post-operative expectations, and reduce hemorrhoid recurrence.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by The Sixth Affiliated Hospital of Sun Yat-Sen University (Approval code: 2022ZSLYEC-096). The patients/participants provided their written informed consent to participate in this study.
Author Contributions
QL: Conception, data analysis, drafting the manuscript, review of the literature. RG: Conception, data acquisition, interpretation of data, drafting the manuscript. LL: Conception, data acquisition, interpretation of data. HZ: Conception, data collection, revision. DZ: Critical revision of the manuscript and factual content. HQ: Interpretation of manuscript revision, critical revision of the statistical analysis. DR: critical revision of the manuscript and factual content. DS: Conception and design, data acquisition, critical manuscript review. All authors have agreed to the final revision of the manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Foundation of the Hebei Province 2020 Annual Medical Science Research Project (20201578).
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Cosman BC. Piles of money: “Hemorrhoids” are a billion-dollar industry. Am J Gastroenterol. (2019) 114(5):716–7. doi: 10.14309/ajg.0000000000000234
2. Sandler RS, Peery AF. Rethinking what we know about hemorrhoids. Clin Gastroenterol Hepatol. (2019) 17(1):8–15. doi: 10.1016/j.cgh.2018.03.020
3. Sugerman DT. JAMA patient page. Hemorrhoids. JAMA. (2014) 312(24):2698. doi: 10.1001/jama.2014.281
4. Qureshi WA. Office management of hemorrhoids. Am J Gastroenterol. (2018) 113(6):795–8. doi: 10.1038/s41395-018-0020-0
5. De Marco S, Tiso D. Lifestyle and risk factors in hemorrhoidal disease. Front Surg. (2021) 8:729166. doi: 10.3389/fsurg.2021.729166
6. Parés D, Molinet Coll C, Troya J, Altimira Queral L, Lopez-Negre JL, Martinez-Franco E. Influence of bowel habit and hormonal changes on the development of hemorrhoidal disease during pregnancy and the postdelivery period: a prospective cohort study. Dis Colon Rectum. (2021) 64(6):724–34. doi: 10.1097/DCR.0000000000001822
7. Altomare DF, Giuratrabocchetta S. Conservative and surgical treatment of hemorrhoids. Nat Rev Gastroenterol Hepatol. (2013) 10(9):513–21. doi: 10.1038/nrgastro.2013.91
8. Jacobs D. Clinical practice. Hemorrhoids. N Engl J Med. (2014) 371(10):944–51. doi: 10.1056/NEJMcp1204188
9. Muldoon R. Review of american society of colon and rectal surgeons clinical practice guidelines for the management of hemorrhoids. JAMA Surg. (2020) 155(8):773–4. doi: 10.1001/jamasurg.2020.0788
10. Alonso-Coello P, Mills E, Heels-Ansdell D, López-Yarto M, Zhou Q, Johanson JF, et al. Fiber for the treatment of hemorrhoids complications: a systematic review and meta-analysis. Am J Gastroenterol. (2006) 101(1):181–8. doi: 10.1111/j.1572-0241.2005.00359.x
11. Gravina AG, Pellegrino R, Facchiano A, Palladino G, Loguercio C, Federico A. Evaluation of the efficacy and safety of a compound of micronized flavonoids in combination with vitamin C and extracts of centella asiatica, vaccinium myrtillus, and vitis vinifera for the reduction of hemorrhoidal symptoms in patients with grade II and III hemorrhoidal disease: a retrospective real-life study. Front Pharmacol. (2021) 12:773320. doi: 10.3389/fphar.2021.773320
12. Picciariello A, O’Connell PR, Hahnloser D, Gallo G, Munoz-Duyos A, Schwandner O, et al. Obstructed defaecation syndrome: European consensus guidelines on the surgical management. Br J Surg. (2021) 108(10):1149–53. doi: 10.1093/bjs/znab123
13. Podzemny V, Pescatori LC, Pescatori M. Management of obstructed defecation. World J Gastroenterol. (2015) 21(4):1053–60. doi: 10.3748/wjg.v21.i4.1053
14. Kalkdijk J, Broens P, Ten Broek R, van der Heijden J, Trzpis M, Pierie JP, et al. Functional constipation in patients with hemorrhoids: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. (2022) 10–1097. doi: 10.1097/MEG.0000000000002361. [Epub ahead of print]35412490
15. Aibuedefe B, Kling SM, Philp MM, Ross HM, Poggio JL. An update on surgical treatment of hemorrhoidal disease: a systematic review and meta-analysis. Int J Colorectal Dis. (2021) 36(9):2041–9. doi: 10.1007/s00384-021-03953-3
16. Jayaraman S, Colquhoun PH, Malthaner RA. Stapled hemorrhoidopexy is associated with a higher long-term recurrence rate of internal hemorrhoids compared with conventional excisional hemorrhoid surgery. Dis Colon Rectum. (2007) 50(9):1297–305. doi: 10.1007/s10350-007-0308-4
17. Pata F, Gallo G, Pellino G, Vigorita V, Podda M, Di Saverio S, et al. Evolution of surgical management of hemorrhoidal disease: an historical overview. Front Surg. (2021) 8:727059. doi: 10.3389/fsurg.2021.727059
18. Giamundo P, Braini A, Calabrò G, Crea N, De Nardi P, Fabiano F, et al. Doppler-guided hemorrhoidal dearterialization with laser (HeLP): indications and clinical outcome in the long-term. Results of a multicenter trial. Surg Endosc. (2022) 36(1):143–8. doi: 10.1007/s00464-020-08248-2
19. Dekker L, Han-Geurts IJM, Grossi U, Gallo G, Veldkamp R. Is the Goligher classification a valid tool in clinical practice and research for hemorrhoidal disease? Tech Coloproctol. (2022) 26(5):387–92. doi: 10.1007/s10151-022-02591-3
20. Gallo G, Pietroletti R, Novelli E, Sturiale A, Tutino R, Lobascio P, et al. A multicentre, open-label, single-arm phase II trial of the efficacy and safety of sclerotherapy using 3% polidocanol foam to treat second-degree haemorrhoids (SCLEROFOAM) [published online ahead of print, 2022 Mar 25]. Tech Coloproctol. (2022) 1–10. doi: 10.1007/s10151-022-02609-w.34767095
21. Picciariello A, Tsarkov PV, Papagni V, Efetov S, Markaryan DR, Tulina I, et al. Classifications and clinical assessment of haemorrhoids: the proctologist’s corner. Rev Recent Clin Trials. (2021) 16(1):10–6. doi: 10.2174/1574887115666200312163940
22. Lin HC, He QL, Shao WJ, Chen XL, Peng H, Xie SK, et al. Partial stapled hemorrhoidopexy versus circumferential stapled hemorrhoidopexy for grade III to IV prolapsing hemorrhoids: a randomized, noninferiority trial. Dis Colon Rectum. (2019) 62(2):223–33. doi: 10.1097/DCR.0000000000001261
23. Jayne DG, Schwandner O, Stuto A. Stapled transanal rectal resection for obstructed defecation syndrome: one-year results of the European STARR Registry. Dis Colon Rectum. (2009) 52(7):1205–12; discussion 1212–4. doi: 10.1007/DCR.0b013e3181a9120f
24. Altomare DF, Spazzafumo L, Rinaldi M, Dodi G, Ghiselli R, Piloni V. Set-up and statistical validation of a new scoring system for obstructed defaecation syndrome. Colorectal Dis. (2008) 10(1):84–8. doi: 10.1111/j.1463-1318.2007.01262.x
25. Zheng T, Ellinghaus D, Juzenas S, Cossais F, Burmeister G, Mayr G, et al. Genome-wide analysis of 944 133 individuals provides insights into the etiology of haemorrhoidal disease. Gut. (2021) 70(8):1538–49. doi: 10.1136/gutjnl-2020-323868.
26. Bassotti G, Villanacci V, Bellomi A, Fante R, Cadei M, Vicenzi L, et al. An assessment of enteric nervous system and estroprogestinic receptors in obstructed defecation associated with rectal intussusception. Neurogastroenterol Motil. (2012) 24(3):e155–61. doi: 10.1111/j.1365-2982.2011.01850.x
27. Brunenieks I, Pekarska K, Kasyanov V, Groma V. Biomechanical and morphological peculiarities of the rectum in patients with obstructed defecation syndrome. Rom J Morphol Embryol. (2017) 58(4):1193–200.29556608
28. Pata F, Sgró A, Ferrara F, Vigorita V, Gallo G, Anatomy PG. Physiology and pathophysiology of haemorrhoids. Rev Recent Clin Trials. (2021) 16(1):75–80. doi: 10.2174/1574887115666200406115150
29. Yang HK. The pathophysiology of hemorrhoids[M]//Hemorrhoids. Berlin, Heidelberg: Springer (2014). 15–24.
30. Kepenekci I, Keskinkilic B, Akinsu F, Cakir P, Elhan AH, Erkek AB, et al. Prevalence of pelvic floor disorders in the female population and the impact of age, mode of delivery, and parity. Dis Colon Rectum. (2011) 54(1):85–94. doi: 10.1007/DCR.0b013e3181fd2356
31. Garg P. Conservative treatment of hemorrhoids deserves more attention in guidelines and clinical practice. Dis Colon Rectum. (2018) 61(7):e348. doi: 10.1097/DCR.0000000000001127
32. Gao R, Tao Y, Zhou C, Li J, Wang X, Chen L, et al. Exercise therapy in patients with constipation: a systematic review and meta-analysis of randomized controlled trials. Scand J Gastroenterol. (2019) 54(2):169–77. doi: 10.1080/00365521.2019.1568544
33. de Oliveira EP, Burini RC. The impact of physical exercise on the gastrointestinal tract. Curr Opin Clin Nutr Metab Care. (2009) 12(5):533–8. doi: 10.1097/MCO.0b013e32832e6776
34. Heitmann PT, Vollebregt PF, Knowles CH, Lunniss PJ, Dinning PG, Scott SM. Understanding the physiology of human defaecation and disorders of continence and evacuation. Nat Rev Gastroenterol Hepatol. (2021) 18(11):751–69. doi: 10.1038/s41575-021-00487-5
35. Johanson JF, Sonnenberg A. The prevalence of hemorrhoids and chronic constipation. An epidemiologic study. Gastroenterology. (1990) 98(2):380–6. doi: 10.1016/0016-5085(90)90828-o
36. Haas PA, Fox TA Jr. Age-related changes, and scar formations of perianal connective tissue. Dis Colon Rectum. (1980) 23(3):160–9. doi: 10.1007/BF02587619
37. Haas PA, Fox TA Jr, Haas GP. The pathogenesis of hemorrhoids. Dis Colon Rectum. (1984) 27(7):442–50. doi: 10.1007/BF02555533
38. Margetis N. Pathophysiology of internal hemorrhoids. Ann Gastroenterol. (2019) 32(3):264–72. doi: 10.20524/aog.2019.0355
39. Neshatian L, Lee A, Trickey AW, Arnow KD, Gurland BH. Rectal prolapse: age-related differences in clinical presentation and what bothers women most. Dis Colon Rectum. (2021) 64(5):609–16. doi: 10.1097/DCR.0000000000001843
40. Sun WM, Read NW, Shorthouse AJ. Hypertensive anal cushions as a cause of the high anal canal pressures in patients with haemorrhoids. Br J Surg. (1990) 77(4):458–62. doi: 10.1002/bjs.1800770430
41. Hancock BD. Internal sphincter and the nature of haemorrhoids. Gut. (1977) 18(8):651–5. doi: 10.1136/gut.18.8.651
42. Gallo G, Martellucci J, Sturiale A, Clerico G, Milito G, Marino F, et al. Consensus statement of the Italian society of colorectal surgery (SICCR): management and treatment of hemorrhoidal disease. Tech Coloproctol. (2020) 24(2):145–64. doi: 10.1007/s10151-020-02149-1
43. Mehigan BJ, Monson JR, Hartley JE. Stapling procedure for haemorrhoids versus Milligan-Morgan haemorrhoidectomy: randomised controlled trial. Lancet. (2000) 355(9206):782–5. doi: 10.1016/S0140-6736(99)08362-2
44. Watson AJ, Cook J, Hudson J, Kilonzo M, Wood J, Bruhn H, et al. A pragmatic multicentre randomised controlled trial comparing stapled haemorrhoidopexy with traditional excisional surgery for haemorrhoidal disease: the eTHoS study. Health Technol Assess. (2017) 21(70):1–224. doi: 10.3310/hta21700
45. Naldini G, Sturiale A. Comments on a systematic review assessing the outcomes of stapled hemorrhoidopexy versus open hemorrhoidectomy. Tech Coloproctol. (2021) 25(8):991–2. doi: 10.1007/s10151-021-02424-9
46. Jain M, Baijal R, Srinivas M, Venkataraman J. Fecal evacuation disorders in anal fissure, hemorrhoids, and solitary rectal ulcer syndrome. Indian J Gastroenterol. (2019) 38(2):173–7. doi: 10.1007/s12664-018-0927-9
47. Murad-Regadas SM, Regadas FS, Bezerra CC, de Oliveira MT, Regadas Filho FS, Rodrigues LV, Almeida SS, et al. Use of biofeedback combined with diet for treatment of obstructed defecation associated with paradoxical puborectalis contraction (Anismus): predictive factors and short-term outcome. Dis Colon Rectum. (2016) 59(2):115–21. doi: 10.1097/DCR.0000000000000519
Keywords: defecation habit, obstructive defecation syndrome, hemorrhoid, recurrence, risk factors
Citation: Li Q, Ghoorun RA, Li L, Zhang H, Zhang D, Qian H, Ren D and Su D (2022) Correlation Between Poor Defecation Habits and Postoperative Hemorrhoid Recurrence. Front. Surg. 9:930215. doi: 10.3389/fsurg.2022.930215
Received: 27 April 2022; Accepted: 31 May 2022;
Published: 17 June 2022.
Edited by:
Alberto Realis Luc, Clinica Santa Rita, ItalyReviewed by:
Audrius Dulskas, National Cancer Institute (Lithuania), LithuaniaGiovanni Tomasicchio, Università degli Studi di Bari, Italy
Copyright © 2022 Li, Ghoorun, Li, Zhang, Zhang, Qian, Ren and Su. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Su c3VkYW4zQG1haWwuc3lzdS5lZHUuY24= Haihua Qian aGFpaHVhcWlhbkAxMjYuY29t Dong-Lin Ren cmVuZGwxMTFAMTYzLmNvbQ==
†These authors have equally contributed to this work
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Qing Li
Qing Li Roshan Ara Ghoorun3†
Roshan Ara Ghoorun3† Dan Zhang
Dan Zhang