- 1Department of Urology, Institute of Urology (Laboratory of Reconstructive Urology), West China Hospital, Sichuan University, Chengdu, China
- 2Department of Oncology, Chengdu Third People’s Hospital, Chengdu, Sichuan, China
Purpose: To evaluate the superior calyceal access’s performance and safety in relation to other calyceal access during percutaneous nephrolithotomy (PCNL).
Methods: The suggested reporting items for systematic reviews and meta-analysis were used to conduct this meta-analysis (PRISMA). To find pertinent studies for this meta-analysis, we searched PubMed, Embase, Web of Science, and China National Knowledge Infrastructure (CNKI). Operation time and hospital stay are two secondary outcomes, whereas failed stone clearance and complication events are the two major outcomes. Utilizing Stata 15.0, RevMan 5.3, and R 4.0.2, relative data were extracted and evaluated.
Results: This meta-analysis was based on 16 studies with 8,541 individuals. Pooled results suggested that superior calyceal access could offer fewer failed stone clearance [odds ratio (OR): 0.64, 95% confidence interval (CI), 0.47–0.88, P = 0.006] and lower additional puncture rate (OR: 0.35, 95% CI, 0.24–0.51, P < 0.001) than other calyceal access. No complication difference was found (OR: 1.10, 95% CI, 0.78–1.56, P = 0.57). Superior calyceal access could offer shorter operation time [standard mean difference (SMD): −0.57, 95% CI, −0.98 to −0.15, P = 0.007]. No hospital stay difference was found (SMD: 0.07, 95% CI, −0.09 to 0.22, P = 0.38). Large heterogeneity was detected in stone clearance comparison (I2 = 71%, P < 0.001) and operation time (I2 = 97%, P < 0.001). The stone clearance comparison also identified significant publication bias (P = 0.026). These defects weaken the credibility of the results.
Conclusion: Superior calyceal access in PCNL may result in a higher stone clearance rate, a lower rate of subsequent punctures, and a faster operation duration with no increase in postoperative complications or hospital stay for kidney stone patients, despite the significant heterogeneity and publication bias. By conducting bigger randomized controlled studies, this discovery still has to be confirmed.
Introduction
Kidney stones are a common disease in the urology department, with prevalence rates of 1%–20% (1). With the development of surgical technology, percutaneous nephrolithotomy (PCNL), a less invasive procedure, has emerged as the preferred method of treating urinary calculi (2). Research on PCNL has always focused on selecting the best renal calyces to create a PCNL channel. This topic was supported by a sizable multicenter prospective study that was published in 2012. Superior calyceal access was found to have a higher potential for problems, longer hospital stays, and a poorer rate of stone clearance than inferior calyceal access (3). It is important to note that the experimental and control groups in this study had significantly different stone locations. A randomized controlled clinical experiment, however, produced findings that diverged from those of earlier research (4). Superior calyceal access had a higher stone clearance rate and a similar postoperative complication rate while treating lower calyx and renal pelvis stones in this randomized controlled trial (RCT) compared to inferior calyceal access. With the exception of the RCT and representative large-sample multicenter prospective cohort study (PCS), many other published studies’ conclusions are inconsistent (5, 6). We conducted this meta-analysis to combine and examine published data in order to produce a greater degree of evidence due to the inconsistency of earlier studies on this subject.
Method
Literature search and inclusion criteria
This meta-analysis was carried out according to preferred reporting items for systematic reviews and meta-analysis (PRISMA). We searched PubMed, Embase, Web of Science, and China National Knowledge Infrastructure (CNKI) to identify relevant studies. The latest search date was December 1, 2021. The searching keywords included percutaneous nephrolithotomy, PCNL, superior calyx, upper calyx, superior calyceal access, and upper calyceal access. Furthermore, the reference part of every candidate literature study was manually screened to find possible data sources.
Detailed inclusion criteria followed PICO principles:
1. Patient: Patients with kidney stones were treated with percutaneous nephrolithotomy.
2. Intervention: Intervention in this analysis was superior calyceal access.
3. Comparison: The comparison was conducted between superior calyceal access and other calyceal access.
4. Outcomes: The primary outcomes were stone clearance and complication events. Other outcomes, such as operation and hospital stay time, were not compulsory.
Two independent authors did all the title screening, abstract screening, and full-text review (YM and LL). Exclusion criteria were as follows: reviews, meta-analysis, letters, comments, case serials, and conference abstracts were excluded. Studies focused on comparing middle and inferior calyceal access or published earlier than 2000 were excluded. Studies that did not offer enough information or data which could be used for meta-analysis were excluded.
Nonrandomized primary articles were evaluated by the Newcastle-Ottawa Scale (NOS) system, and two independent reviewers performed the evaluation procedure. According to the NOS scales, 7–9 score studies were considered high-level quality, 5–6 score studies were considered moderate-level, and <5 score studies were low-level quality. Low-level quality studies should not be involved in the meta-analysis.
Meta-analysis
This study compared the efficacy and safety of superior calyceal access applied in the percutaneous nephrolithotomy. In efficacy comparison, the primary outcome was the postoperative stone clearance for two types of access. However, since some included studies did not offer detailed data about complications in the safety comparison, only the overall complication rate was compared in this analysis. Data on the failed stone clearance event, the number of patients with postoperative complications, and the total number of patients were extracted from the included studies. The operation and hospital stay time were also extracted from included studies to compare superior calyceal access and other calyceal access.
Two authors performed the data extracting procedures and double-checked them independently (YM and LL). The data pooling procedures were performed with RevMan 5.3, Stata 15.0, and R 4.0.2. Statistical significance was defined as P < 0.05. The primary outcomes’ 95% confidential intervals (95% CI) were also provided. Standard mead difference was calculated and synthesized as an estimate for a continuous variable. The odds ratio (OR) was calculated and synthesized as the primary effect size for the discontinuous variable. Heterogeneity was evaluated by I2 and Q tests. When I2 > 50%, heterogeneity was considerable, and a random-effects model should be used. Subgroup analyses were conducted to offer more information to identify potential factors contributing to heterogeneity. Forest plots were produced to display the main results. In addition to funnel plots, Egger’s test was used to detect publication bias. Any detected publication bias was reanalyzed using the trim-and-fill method to evaluate the effect of the publication bias on the meta-analysis results.
Results
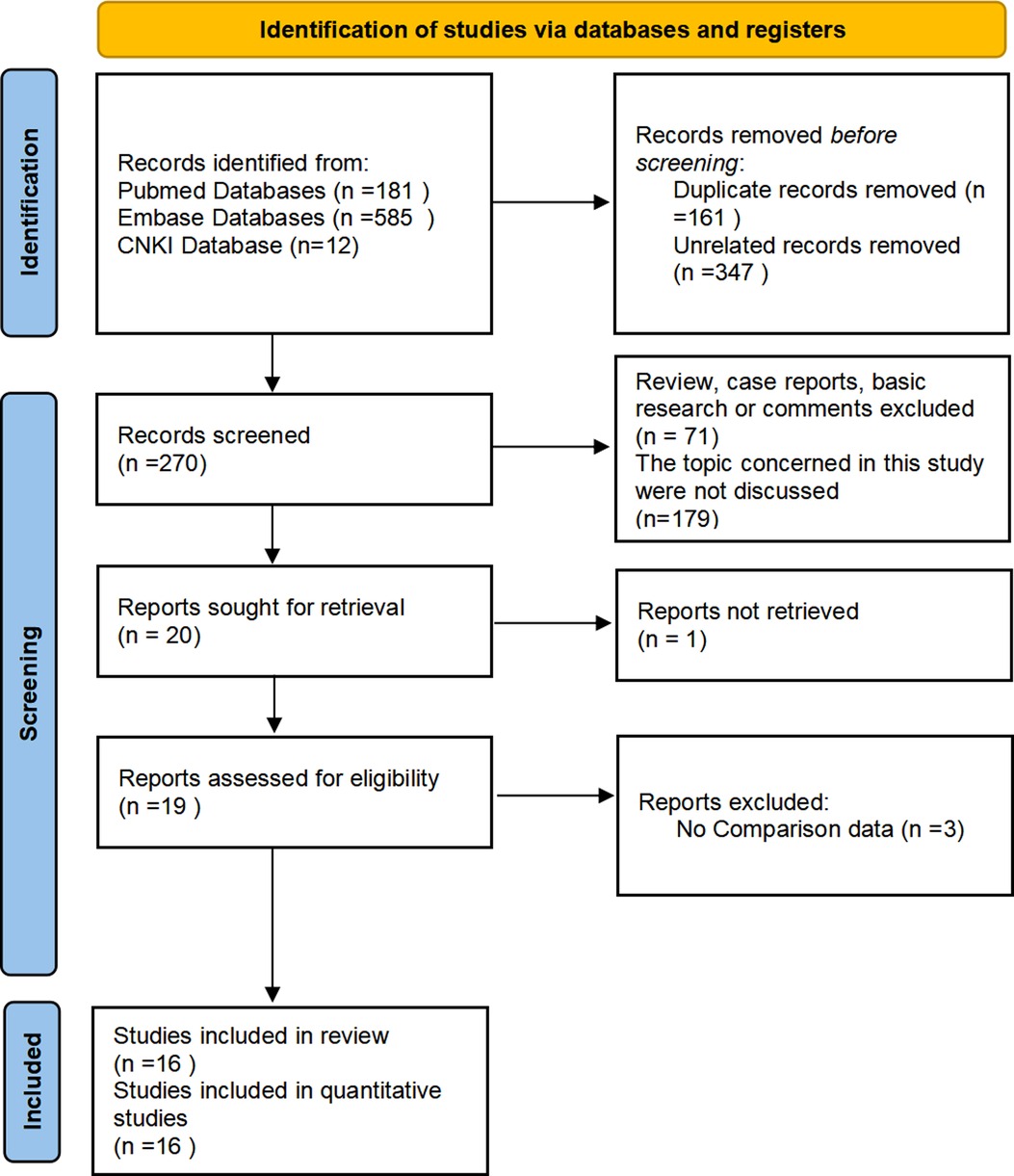
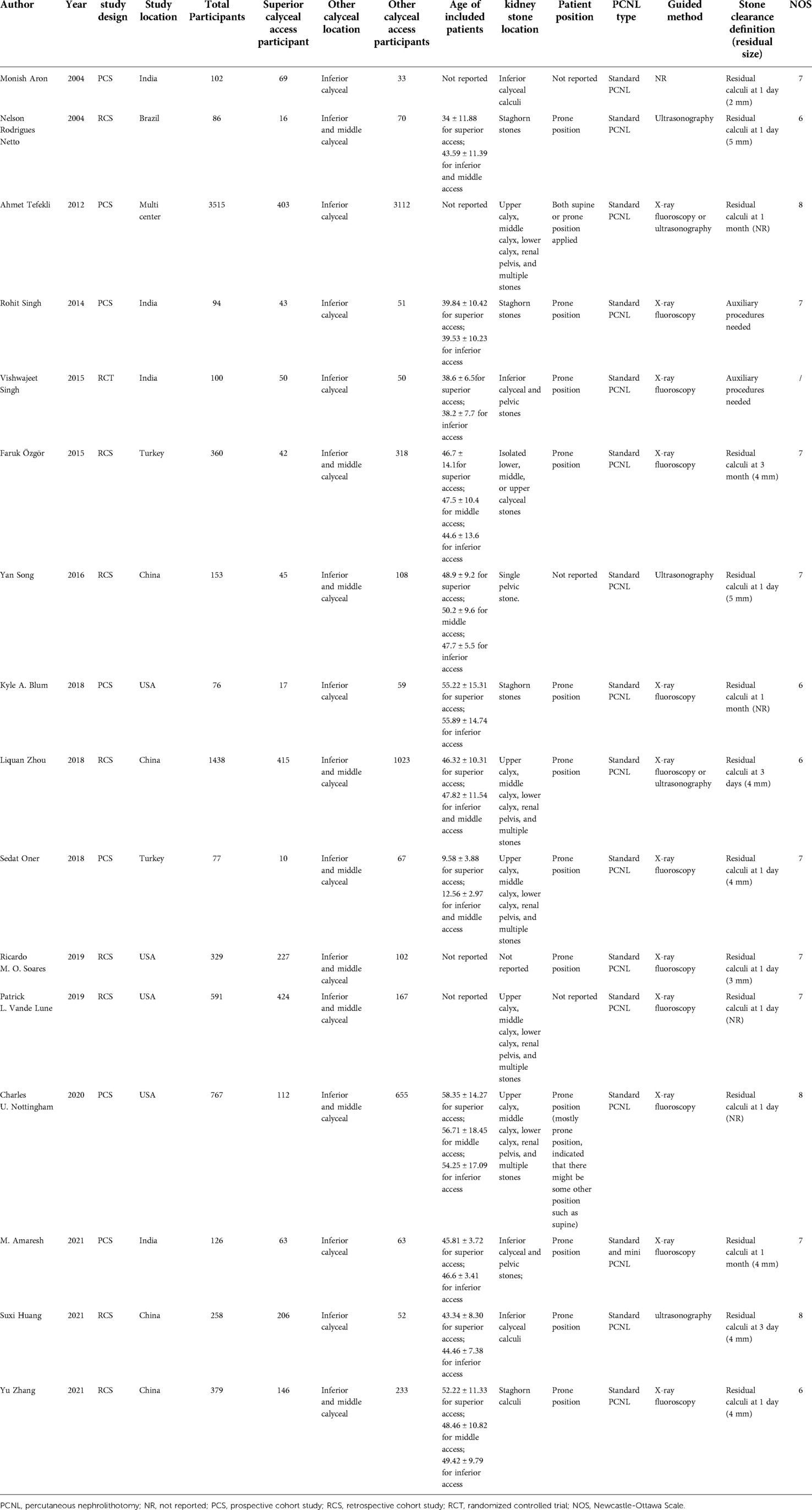
After database search, 778 studies were identified. Original data from 16 research studies were extracted, and after applying screening techniques and quality assessments, they were included in the quantitative analysis (3–18). The flowchart for screening is shown in Figure 1. The efficacy (failed stone clearance) and safety (complication occurrence) of the superior calyceal access against other calyceal access were compared in 16 research studies (a total of 8,451 patients); additional puncture data were examined in 5 studies (987 participants). As secondary outcomes, the comparison of the operation time included 13 studies, and the comparison of the hospital stay included 8 research studies. One RCT, seven prospective studies, and eight retrospective investigations made up the 16 studies. The common PCNL approach served as the foundation for nearly all of the included investigations. Only one employed both conventional and mini PCNL methods (5). Two studies applied for both the prone and supine postures, and 11 research studies applied for the prone position only. Three further studies failed to mention the patient position in the PCNL. The listed studies’ specifics are provided in Table 1. The included papers did not contain any descriptions of flexible nephoscope application.
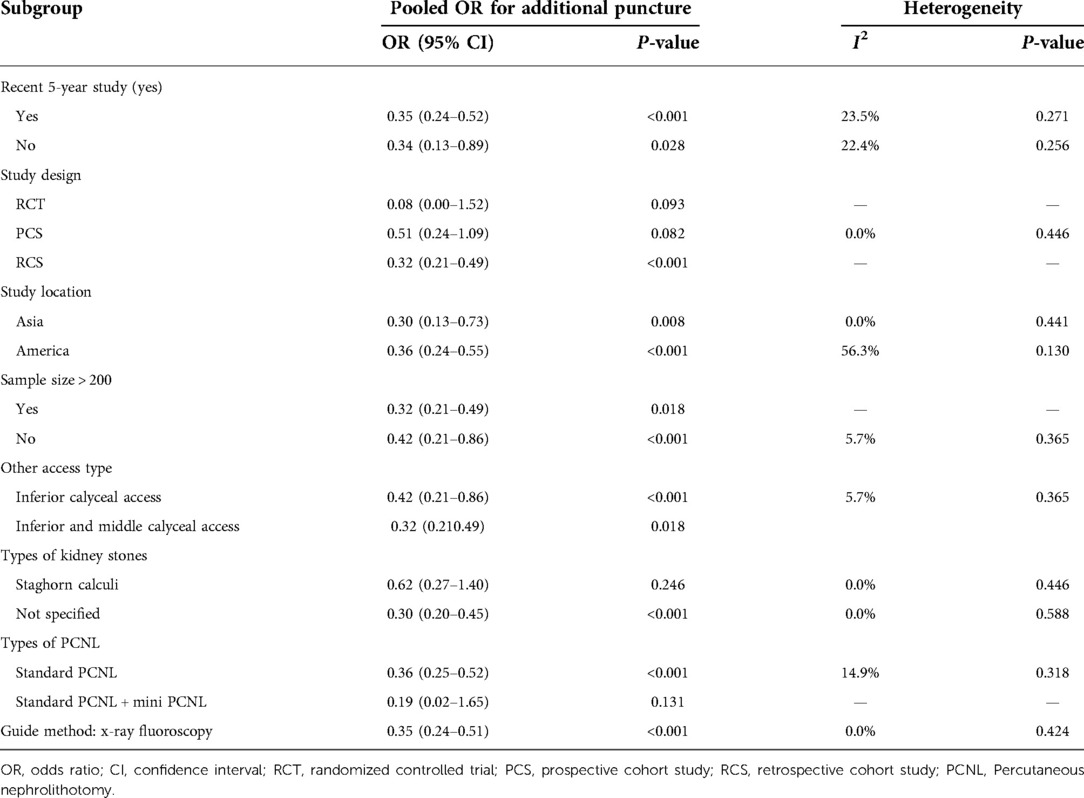
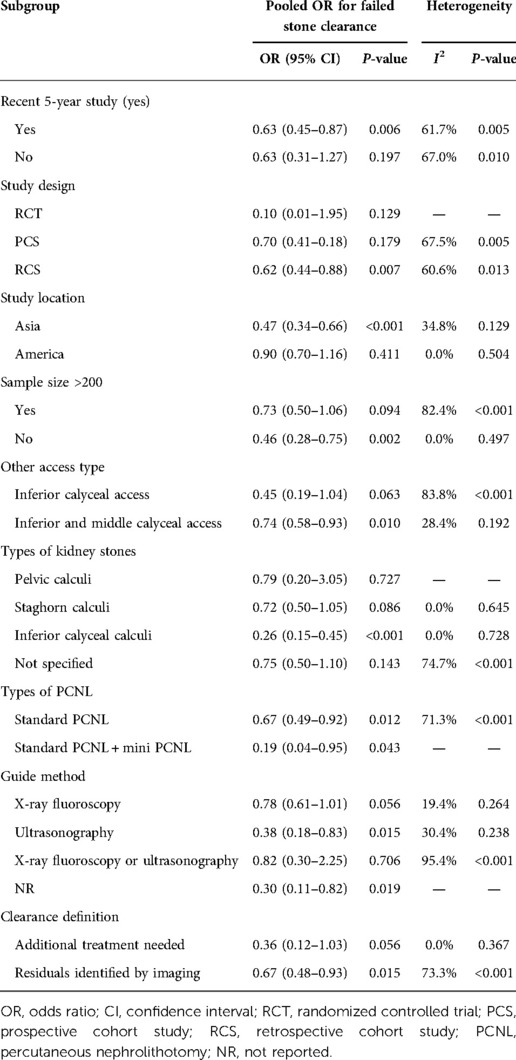
There were 16 studies (comprising 8,451 participants, 2,288 superior calyceal access and 6,163 other calyceal access) included in the comparison of failed stone clearance (3–18). In the overall synthesis, superior calyceal access could offer less failed stone clearance (higher stone-free rate) than other calyceal access [Mantel–Haenszel statistic (M–H) random model, OR: 0.64, 95% CI, 0.47–0.88, P = 0.006, Figure 2A]. The heterogeneity of overall synthesis was significant (I2 = 71%, P < 0.001). The Egger test (P = 0.026) and funnel plot (Figure 3A) detected significant publication bias. The trim-and-fill method was applied to adjust the effect of publication bias on the stability of the results. After adding six additional studies, the pooled result was insignificant (OR: 0.87, 95% CI, 0.60–1.24, P = 0.437, Figure 4). Many interesting things were found in the subgroup analysis (Table 2). Compared with studies in other parts of the world, more positive results have been published in Asia (OR: 0.47, 95% CI, 0.34–0.66, P < 0.001). Unlike prospective studies, retrospectively designed studies support the conclusion that superior calyceal access can provide better stone clearance than other calyceal access (OR: 0.62, 95% CI, 0.44–0.88, P = 0.007).

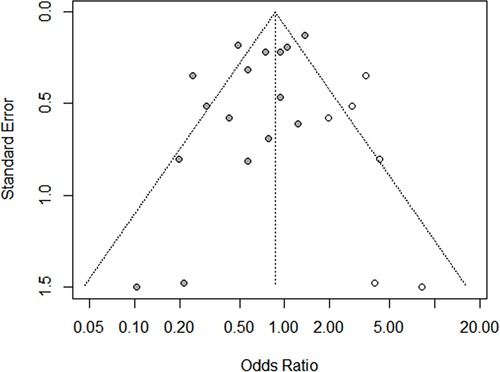
Figure 2. Forest plots of meta-analysis. (A) Stone clearance comparison between superior calyceal access and other calyceal access. (B) Additional puncture rate comparison between superior calyceal access and other calyceal access. (C) Complication comparison between superior calyceal access and other calyceal access.
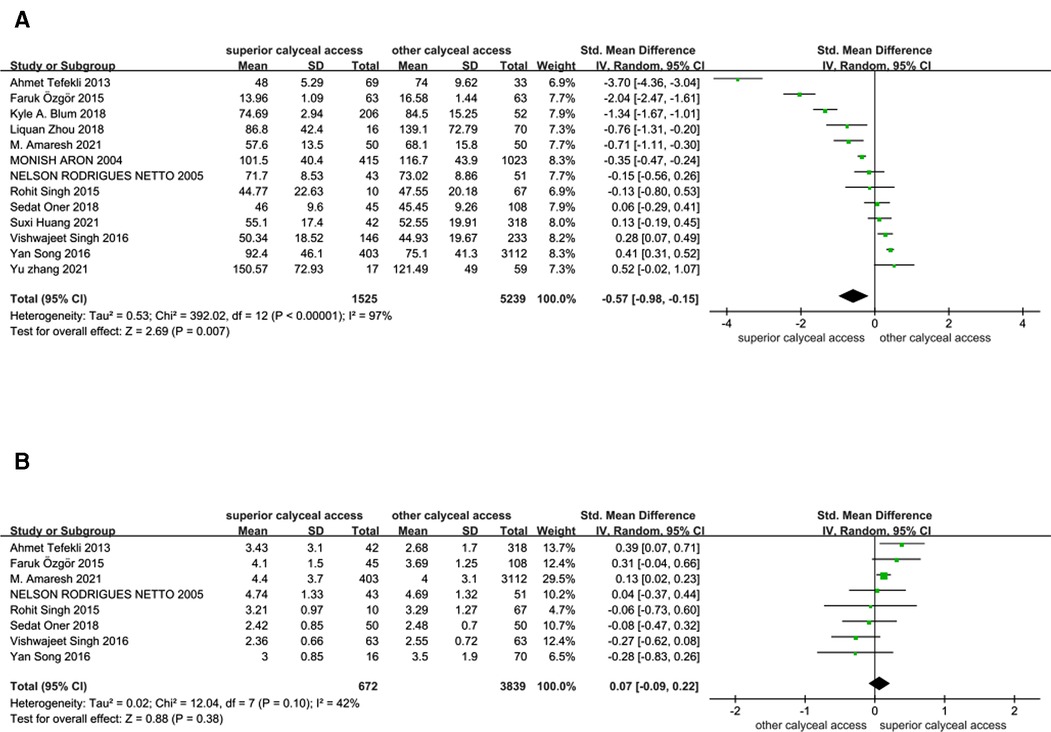
Figure 3. Forest plots of meta-analysis. (A) Operation time comparison between superior calyceal access and other calyceal access. (B) Hospital stays comparison between superior calyceal access and other calyceal access.
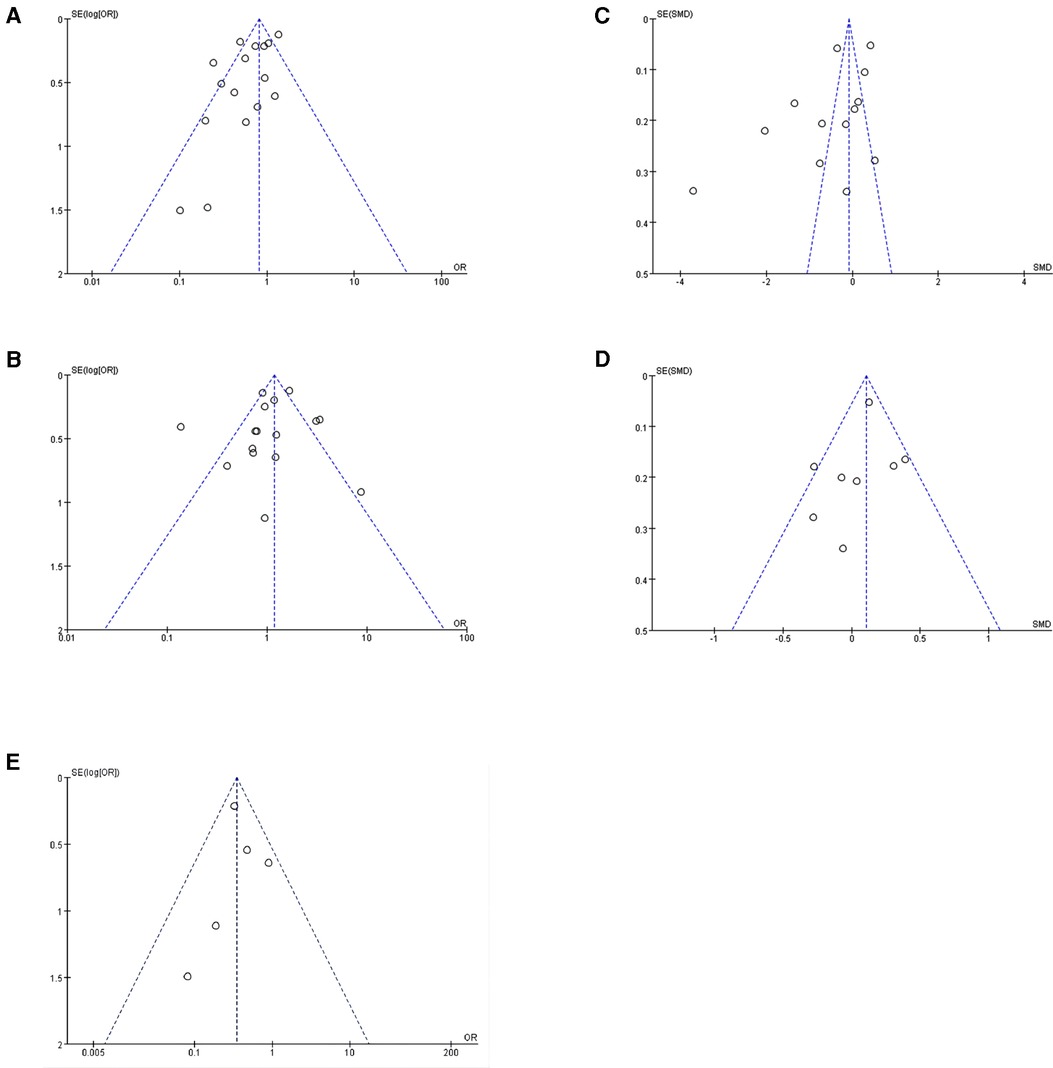
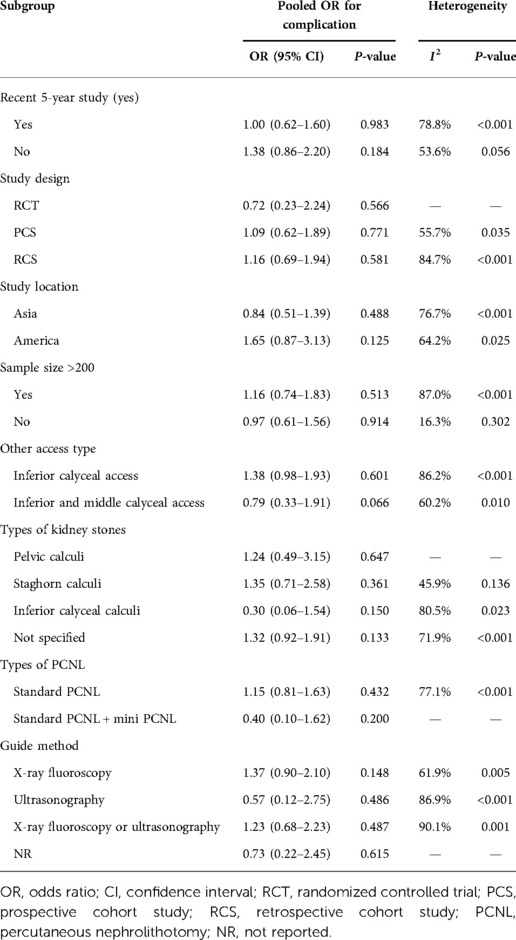
Figure 4. Funnel plots of meta-analysis. (A) Funnel plot for stone clearance comparison. (B) Funnel plot for complication comparison. (C) Funnel plot for operation time comparison. (D) Funnel plot for hospital stay comparison. (E) Funnel plot for additional puncture comparison.
In this meta-analysis, since many included studies did not report the first puncture success rate, we used additional puncture as another efficacy outcome for data pooling. Five studies offered relative information comprising 597 patients who received superior calyceal access and 390 patients who received other calyceal access (4, 5, 7, 8, 16). In the overall comparison, superior calyceal access could offer a lower multiple puncture rate (OR: 0.35, 95% CI, 0.24–0.51, P < 0.001, Figure 2B) without significant heterogeneity detected (I2 = 0%, P = 0.42). No significant publication bias was detected in the funnel plot and Egger test (P = 0.663, Figure 3E). In the PCNL conducted on the patients with staghorn stone, there was no significant difference between superior calyceal access and other calyceal access (OR = 0.62, 95% CI, 0.27–1.40, P = 0.246, Table 3). In the subgroup analysis, we found that in the prospectively designed studies, the comparison is not significant (PCS: OR = 0.51, 95% CI, 0.24–1.09, P = 0.082; RCT: OR = 0.08, 95% CI, 0.00–1.52, P = 0.093, Table 3), this result may indicate possible selecting and reporting bias in the retrospectively designed studies included in this meta-analysis.
There were also 16 studies (comprising 8,451 participants, 2,288 superior calyceal access and 6,163 other calyceal access) included in the complication comparison meta-analysis (3–18). In the overall synthesis, no significant complication difference was detected between superior calyceal access and other calyceal access (M–H random model, OR: 1.10, 95% CI, 0.78–1.56, P = 0.57, Figure 2C). The heterogeneity of synthesis was significant (I2 = 76%, P < 0.001). No publication bias was found by Egger’s test (P = 0.568) and funnel plots (Figure 3B). Detailed subgroup analyses about safety information are shown in Table 4, and there was no significant difference in any subgroup.
In this analysis, operation time and hospital stay were synthesized and compared as secondary outcomes. Since there might be differences in operation time and hospital stay definition among included studies, standard mean difference (SMD) was calculated and pooled to get a proper estimate. There were 13 studies (1,525 superior calyceal access and 5,239 other calyceal access) included in the operation time comparison (3–13, 17, 18). After the data synthesis, we found that superior calyceal access could offer a short operation time compared with other calyceal access [inverse variance weighted method (IVM), SMD: −0.57, 95% CI, −0.98, −0.15, P = 0.007, Figure 5A]. The heterogeneity was substantial (I2 = 97%, P < 0.001). The funnel plot was asymmetric, but Egger’s test detected no publication bias (P = 0.074) (Figure 3C). Hospital stay comparison was conducted among eight studies (672 superior calyceal access, 3,839 other calyceal access) (3–7, 12, 13, 17), and we found that there was no significant difference (IVM, SMD: 0.07, 95% CI, −0.09, 0.22, P = 0.38, Figure 5B) without significant heterogeneity (I2 = 42%, P = 0.10). No publication bias was detected by funnel plot (Figure 3D) and Egger’s test (P = 0.408).
Discussion
The choice of access for PCNL is crucial and has given rise to a heated discussion. Superior calyceal access may provide a higher stone clearance rate than other calyceal access, according the findings of the meta-analysis (M–H random model, OR: 0.64, 95% CI, 0.47–0.88, P = 0.006). This finding is, however, undermined by significant heterogeneity and substantial publication bias. The difference in stone clearance between superior and other calyceal access became minor when publication bias was adjusted using the trim-and-fill technique (six studies included, OR: 0.87, 95% CI, 0.60–1.24, P = 0.437). When comparing additional puncture rates, we discovered that superior calyceal access might provide a lower additional puncture rate than other calyceal access (OR: 0.35, 95% CI, 0.24–0.51, P0.001) without a lot of heterogeneity. There was no discernible difference between superior and inferior calyceal access in the safety comparison (OR: 1.08, 95% CI, 0.76–1.53, P = 0.68). However, significant heterogeneity and possible publication bias continued to have an impact on this conclusion. The combination of operation time and hospital stay was a secondary outcome in this analysis. Superior calyceal access and other calyceal access did not significantly shorten hospital stays (IVM, SMD: 0.07, 95% CI, −0.09, 0.22, P = 0.38, Figure 2D). Similar to stone clearance, despite significant variations in the length of the operation (IVM, SMD: −0.57, 95% CI, −0.98, −0.15, P = 0.007, Figure 2C), the significant heterogeneity has a major impact on the stability of the conclusion (I2 = 97%, P0.001).
Many considerations, including but not limited to the location and size of the stone, additional patient problems like stone burden, location, pelvicalyceal anatomy, history of prior surgery, and the surgeon’s technical preferences, influence the surgeon’s choice of access site (3). A prior study found that with superior calyceal access for patients with superior calyceal and staghorn stones, PCNL might be a preferable option. Its primary benefit is anatomical closeness and instrumentation simplicity (3). Numerous other findings concurred that difficult kidney stones should benefit from greater utilization of superior calyceal access (8, 9). One funnel-shaped calyx that discharges the superior calyx is a distinguishing feature of the superior calyceal access, and the internal space is often bigger than that of the inferior and middle calyces (19). The superior renal calyx has a considerably lower likelihood of developing massive calculi than the middle and inferior renal calyx due to the gravity effect, which is also highly helpful for increasing the operational area and flexibility of the device inside the kidney (20). In addition to facilitating access to the renal pelvis and other calices and achieving a satisfactory stone-free rate with fewer punctures and fewer complications, access through the superior calyx also enables the device to be aligned with the long axis of the kidney in comparison to other access points (8). Although some studies believed that the middle calyceal access could treat both superior and inferior calyx (21), the passage through the middle calyx forms a very small acute angle with the superior calyx and inferior calyx. It was often challenging to perform thorough stone cleaning (20). The advantages of the superior calyx are the main drawbacks of PCNL’s use of the inferior calyx access. The inferior calyx has a more intricate structure, a smaller internal volume, and a larger angle with the kidney’s long axis; all of these characteristics may have an impact on the clearance rate for stones (20). Unless there is clear evidence that superior calyceal access carries a higher risk of perioperative adverse events, such as superior calyceal placement to the 11th and 12th intercostals, the choice of inferior calyceal access and superior calyceal access is more dependent on the doctor’s habits and even the hospital’s tradition (3).
The main difference between superior and inferior calyceal access in terms of problems is that establishing the upper calyx channel frequently necessitates supracostal puncture, which may increase the risk of chest-related complications like pneumothorax and even lung injury (5). The risk of hydrothorax following supracostal puncture was minimal (3.31%), which was within an acceptable range, according to a study that was specifically focused on this procedure (22). Superior calyceal access has been linked to higher difficulties in some research, but this study incorporated more published data and discovered that it does not in overall comparison and subgroup analysis. This may be due to the fact that the researchers in the original studies that made up this meta-analysis excluded obese patients from the superior calyceal access for ethical and medical grounds when the superior calyceal position was too high in such patients. We suspect that selection bias may have a bigger impact on the complication comparison because the majority of the original research in our investigation used unblinded designs, nonrandomized prospective trials, and retrospective studies. Postoperative problems can arise during surgery for various reasons, including stone burden, stone placement, pelvicalyceal anatomy, baseline features, patient posture (prone or supine), tract size, and scope type. Although the results of this study, which included 16 original studies and 8,451 patients’ postoperative data, indicated that statistically superior calyceal access may not increase the risk of complications, it is still necessary to consider the actual patient characteristics when selecting the puncture technique.
An excellent systematic review related to this topic was published in 2019 (23). The authors of that comprehensive review evaluated supracostal and infracostal access for percutaneous nephrolithotomy and came to the conclusion that while supracostal access was safe, infracostal access PCNL was more successful. This conclusion differs from those observed in this study since there was no discernible difference in the rates of complications between superior calyceal access and other calyceal access. This distinction also has an explanation. First of all, unlike the goals of our investigation, the primary objective of the previously published meta-analysis was not to compare supracostal access with infracostal access. Second, there was no discernible difference between infracostal and supracostal access in the entire comparison.
To sum up, we believe that, if safety is completely taken into account prior to surgery, superior calyceal access may be able to result in improved stone free rate (SFR) and a quicker postoperative recovery period in PCNL surgery. A thoroughly planned randomized clinical trial must be conducted to confirm this conclusion.
There were still some limitations of this analysis. First, although the major component studies were prospective designed studies, there was only one RCT included in this meta-analysis. Second, although the pooling result indicated that superior calyceal access could offer a better stone clearance rate, the heterogeneity and publication bias weaken the evidence. Third, although many published research studies included comparisons of data between various PCNL approaches, some did not compare the results primarily based on calyceal access, which inherently creates bias. Notably, when planning a calyx approach in PCNL surgery, urologists must take into account various patient-related aspects. Stone burden, location, pelvic architecture, and history of surgery were among them. Patients with greater suprarenal calyces, especially above the 11th or 12th rib, were likely to experience more perioperative difficulties when they have a superior calyceal access. Only after carefully documenting and examining the aforementioned criteria can meaningful inferences be made. Although the original research included in this analysis attempted to adequately gather the patient’s baseline data, none of the studies were able to produce a thorough report on the pertinent baseline characteristics. Therefore, all conclusions of this study need to be treated with caution. In the future, more large-scale randomized studies should be focused on this topic.
Conclusion
Superior calyceal access in PCNL may result in improved stone clearance rate, lower additional puncture rate, faster operation time, and no increase in postoperative complications or hospital stay for kidney stone patients, despite the significant heterogeneity and publication bias. Larger randomized controlled studies still need to be conducted in order to confirm this finding.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
TJ contributed to the conception and design of the article and provided administrative support. YM and LL contributed to the provision of study materials or patients. YM, LL, and ZL contributed to the collection and assembly of data and data analysis and interpretation. All authors contributed to the writing of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Thongprayoon C, Krambeck AE, Rule AD. Determining the true burden of kidney stone disease. Nat Rev Nephrol. (2020) 16:736–46. doi: 10.1038/s41581-020-0320-7
2. Knoll T, Daels F, Desai J, Hoznek A, Knudsen B, Montanari E, et al. Percutaneous nephrolithotomy: technique. World J Urol. (2017) 35:1361–8. doi: 10.1007/s00345-017-2001-0
3. Tefekli A, Esen T, Olbert PJ, Tolley D, Nadler RB, Sun YH, et al. Isolated upper pole access in percutaneous nephrolithotomy: a large-scale analysis from the CROES percutaneous nephrolithotomy global study. J Urol. (2013) 189:568–73. doi: 10.1016/j.juro.2012.09.035
4. Singh V, Garg Y, Sharma K, Sinha RJ, Gupta S. Prospective randomized comparison between superior calyceal access versus inferior calyceal access in PCNL for inferior calyceal stones with or without pelvic stones. Urolithiasis. (2016) 44:161–5. doi: 10.1007/s00240-015-0805-1
5. Amaresh M, Hegde P, Chawla A, de la Rosette J, Laguna MP, Kriplani A. Safety and efficacy of superior calyceal access versus inferior calyceal access for pelvic and/or lower calyceal renal calculi—a prospective observational comparative study. World J Urol. (2021) 39:2155–61. doi: 10.1007/s00345-020-03409-3
6. Özgör F, Küçüktopcu O, Simsek A, Sarilar Ö, Binbay M, Gürbüz G. Percutaneous nephrolithotomy for isolated calyceal stones: how important is the stone location? Turk J Urol. (2015) 41:171–6. doi: 10.5152/tud.2015.06787
7. Singh R, Kankalia SP, Sabale V, Satav V, Mane D, Mulay A, et al. Comparative evaluation of upper versus lower calyceal approach in percutaneous nephrolithotomy for managing complex renal calculi. Urol Ann. (2015) 7:31–5. doi: 10.1016/j.urology.2015.01.033
8. Blum KA, Parkhomenko E, Thai J, Tran T, Gupta M. A contemporary lower pole approach for complete staghorn calculi: outcomes and efficacy. World J Urol. (2018) 36:1461–7. doi: 10.1007/s00345-018-2284-9
9. Aron M, Goel R, Kesarwani PK, Seth A, Gupta NP. Upper pole access for complex lower pole renal calculi. BJU Int. (2004) 94:849–52, discussion 852. doi: 10.1111/j.1464-410X.2004.05045.x
10. Suxi Huang RY, Chai Y, Hai L, Zhang B. A comparison of two pathways of percutaneous nephrolithotomy in the treatment of complex lower calyceal calculi. Med J Chin PAP. (2021) 32(10):5. doi: 10.14010/j.cnki.wjyx.2021.10.011
11. Yu BY Z, Yin T, Jia W, Wuran W. Effect of different tracts of percutaneous nephrolithotomy on the efficacy of complete staghorn calculus. West China Med J. (2021) 36(8):4. doi: 10.7507/1002-0179.202001005
12. Oner S, Karagozlu Akgul A, Demirbas M, Onen E, Aydos M, Erdogan A. Upper pole access is safe and effective for pediatric percutaneous nephrolithotomy. J Pediatr Urol. (2018) 14:183.e181–e8. doi: 10.1016/j.jpurol.2017.12.013
13. Netto NR Jr, Ikonomidis J, Ikari O, Claro JA. Comparative study of percutaneous access for staghorn calculi. Urology. (2005) 65:659–62, discussion 662–53. doi: 10.1016/j.urology.2004.10.081
14. Soares RMO, Zhu A, Talati VM, Nadler RB. Upper pole access for prone percutaneous nephrolithotomy: advantage or risk? Urology. (2019) 134:66–71. doi: 10.1016/j.urology.2019.08.031
15. Nottingham CU, Large T, Lingeman JE, Krambeck AE. A comparison of perioperative stone-free rates and complications following unilateral, single-access percutaneous nephrolithotomy by access location in 767 patients. Urology. (2020) 142:70–5. doi: 10.1016/j.urology.2020.02.031
16. Vande Lune PL, Thayer D, Mani N, Warren A, Desai AC, Picus DJ, et al. Image-guided access for percutaneous nephrolithotomy: a single-center experience in 591 patients. Curr Urol. (2019) 12:210–5. doi: 10.1159/000499304
17. Song Y, Jin W, Hua S, Fei X. Middle calyx access is better for single renal pelvic stone in ultrasound-guided percutaneous nephrolithotomy. Urolithiasis. (2016) 44:459–63. doi: 10.1007/s00240-016-0866-9
18. Zhou Liquan NZ, Yaoliang D, Guanglong X, Chengyang L, Haipeng H, Xiaofeng G. Comparison of efficacy of PCNL in the treatment of upper urinary calculi in different accesses. J Chongqing Med Univ. (2018) 43(4):4. doi: 10.13406/j.cnki.cyxb.001548
19. Sampaio FJ, Aragao AH. Anatomical relationship between the intrarenal arteries and the kidney collecting system. J Urol. (1990) 143:679–81. doi: 10.1016/S0022-5347(17)40056-5
20. Sampaio FJ. Renal anatomy. Endourologic considerations. Urol Clin North Am. (2000) 27:585–607; vii. doi: 10.1016/S0094-0143(05)70109-9
21. Eryildirim B, Sarica K, Ustun F, Sevinc AH, Simsek B, Sahan A, et al. Comparison of middle and lower calyceal access for renal pelvis stone in percutaneous nephrolithotomy: a prospective randomized study. Urol Int. (2020) 104:758–64. doi: 10.1159/000509330
22. Yadav R, Aron M, Gupta NP, Hemal AK, Seth A, Kolla SB. Safety of supracostal punctures for percutaneous renal surgery. Int J Urol. (2006) 13:1267–70. doi: 10.1111/j.1442-2042.2006.01537.x
Keywords: percutaneous nephrolithotomy, superior calyceal access, meta-analysis, stone clearance, complication
Citation: Ma Y, Lin L, Luo Z and Jin T (2022) Superior calyceal access vs. other calyceal access in percutaneous nephrolithotomy: A systematic review and meta-analysis. Front. Surg. 9:930159. doi: 10.3389/fsurg.2022.930159
Received: 27 April 2022; Accepted: 19 August 2022;
Published: 13 September 2022.
Edited by:
Sajid Sultan, Sindh Institute of Urology and Transplantation, PakistanReviewed by:
Andrey O. Morozov, I.M. Sechenov First Moscow State Medical University, RussiaMahesh R. Desai, Muljibhai Patel Urological Hospital, India
© 2022 Ma, Lin, Luo and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tao Jin amludGFvOTdAc2N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Yucheng Ma
Yucheng Ma Lede Lin1,†
Lede Lin1,† Tao Jin
Tao Jin