- 1Graduate School, Beijing University of Chinese Medicine, Beijing, China
- 2Department of Orthopaedic Surgery, China-Japan Friendship Hospital, Beijing, China
- 3Department of Orthopaedic Surgery, Peking University of China-Japan Friendship School of Clinical Medicine, Beijing, China
- 4Department of Adult Joint Reconstruction, Henan Luoyang Orthopedic Hospital (Henan Provincial Orthopedic Hospital), Zhengzhou, China
Introduction: Many studies have reported the clinical outcomes of a jumbo cup in revision total hip arthroplasty (rTHA) with acetabular bone defect. We conducted a systematic review to access the survivorship and clinical and radiological outcomes of a jumbo cup in rTHA.
Methods: A systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines. A comprehensive literature search from PubMed, MEDLINE, EMBASE, and the Cochrane Database of Systematic Reviews was performed with the keywords (“revision” OR “revision surgery” OR “revision arthroplasty”) AND (“total hip arthroplasty” OR “total hip replacement” OR “THA” OR “THR”) AND (“jumbo cup” OR “jumbo component” OR “extra-large cup” OR “extra-large component”). Studies reporting the clinical or radiological outcomes were included. The basic information and radiological and clinical results of these studies were extracted and summarized for analysis.
Results: A total of 19 articles were included in the systematic review. The analysis of clinical results included 953 hips in 14 studies. The re-revision-free survivorship of the jumbo cup was 95.0% at a mean follow-up of 9.3 years. Dislocation, aseptic loosening, and periprosthetic joint infection were the top three complications with an incidence of 5.9%, 3.0%, and 2.1%, respectively. The postrevision hip center was relatively elevated 10.3 mm on average; the mean postoperative leg-length discrepancy was 5.4 mm.
Conclusion: A jumbo cup is a favorable option for acetabular bone defect reconstruction in rTHA with satisfying survivorship and acceptable complication rates.
Introduction
Reconstruction of an acetabular bone defect is a difficult procedure in revision total hip arthroplasty (rTHA) (1). In rTHA, the primary goal of acetabular reconstruction is creating sufficient mechanical support and bone contact for the acetabular cup, thereby achieving bone ingrowth or ongrowth and attaining stability of the acetabular cup (2). In addition, the position of the rotation hip center is also an important factor to consider. Due to the complexity and variety of the acetabular bone defect, it is highly possible for unexpected challenges to occur beyond the preoperative plan. Moreover, many patients who accept revision arthroplasty are at an advanced age with underlying diseases; therefore, there is need for enhancing surgical efficiency and limiting damage control. These factors all bring significant challenges to surgeons.
Before performing rTHA, an evaluation of the acetabular bone defect is necessary. The Paprosky classification, American Academy of Orthopaedic Surgeons (AAOS) classification, and Gross system are the most commonly used in preoperative planning (3, 4). Many new methods of evaluation have also been developed to help surgeons make better surgical strategy (5–9). Currently, the Paprosky type IIIA and IIIB and AAOS type III and IV are regarded as the most challenging conditions, which involve extensive bone loss of the acetabular rim and columns, and even pelvic discontinuity (10, 11). Several methods of reconstruction have been developed for severe acetabular bone loss in rTHA, such as structural allografts, impaction bone grafting, the jumbo cup, the highly porous metallic augments and hemispherical cup, the cup-cage system, custom monoflanged acetabular components, and the cup-on-cup technique (12–20). Many studies as well as systematic reviews have reported the clinical results of these reconstruction techniques (21–24), but the most effective solution remains controversial.
Using a jumbo cup is one of the most commonly recommended reconstruction methods for severe acetabular bone defect in rTHA. It was first reported by Jasty in 1998 (25). There is no strict definition for the jumbo cup. Most papers define the jumbo cup as a diameter of over 66 or 64 mm for males and over 62 or 60 mm for females. The advantages of the jumbo cup include the obvious simplified surgical procedure, more contact area with the host bone, and less requirement for bone graft (26). However, there are also some limitations in using the jumbo cup for reconstruction. For example, it may result in further bone loss (27), which may delay the full weight-bearing time and even cause a protrusion of the jumbo cup into the pelvic cavity. Therefore, the jumbo cup is usually applied in Paprosky type I–III acetabular bone defect and rarely used alone for pelvic discontinuity (11). In many cases, jumbo cups have to be set in a high position to provide sufficient contact with the host bone and mechanical support, which may lead to rotation center elevation, leg-length discrepancy (LLD), and soft tissue imbalance (28). Although many studies have reported the clinical results of the jumbo cup in rTHA, no systematic review has been conducted to date. In this context, the aim of this study is to systematically summarize the current evidence of the jumbo cup in rTHA, including survivorship and failure, radiological outcome, hip function, and complications.
Materials and methods
Literature search strategy
We conducted a comprehensive literature search from the electronic databases PubMed, EMBASE, Web of Science, and Cochrane Library. The last literature search was on 15 April 2022. The search project was based on the following keywords: (“revision” OR “revision surgery” OR “revision arthroplasty”) AND (“total hip arthroplasty” OR “total hip replacement” OR “THA” OR “THR”) AND (“jumbo cup” OR “jumbo component” OR “extra-large cup” OR “extra-large component”). The language was limited to English. If the abstract was not sufficient for us to include or exclude a study, we would download the full text. The literature search process was carried out on the basis of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (29).
Inclusion and exclusion criteria
Only those clinical studies that met the following criteria were included in this systematic review: (1) rTHA with acetabular bone defect; (2) using a jumbo cup for acetabular reconstruction; and (3) reporting clinical results or radiological data. Reviews, conference abstracts, non-English written articles, letters, case reports, experiment studies, and simulation studies were excluded from this systematic review.
Data extraction
Two researchers separately extracted all data according to the rules described above. We developed an extraction table for data extraction including the following: (1) basic information of each study; (2) radiological results evaluating the implant position; and (3) clinical results including studying the accuracy of the preoperative plan, intraoperative details, and postoperative function complications. All data were extracted by two investigators; any disagreement was solved by an expert surgeon and a third researcher to make a final decision.
Quality assessment
We used the Methodological Index for Non-Randomized Studies (MINORS) for quality assessment (30). This evaluation system involves 12 items for comparative studies and 8 items for noncomparative studies, with total scores of 24 and 16, respectively. The item was separately scored with 0, 1, and 2 corresponding to nonreported information, inadequate information, and adequate information, respectively. Two authors independently filled the evaluation system. Studies that scored >75% of the total score were considered to have a low risk of bias.
Results
Literature selection
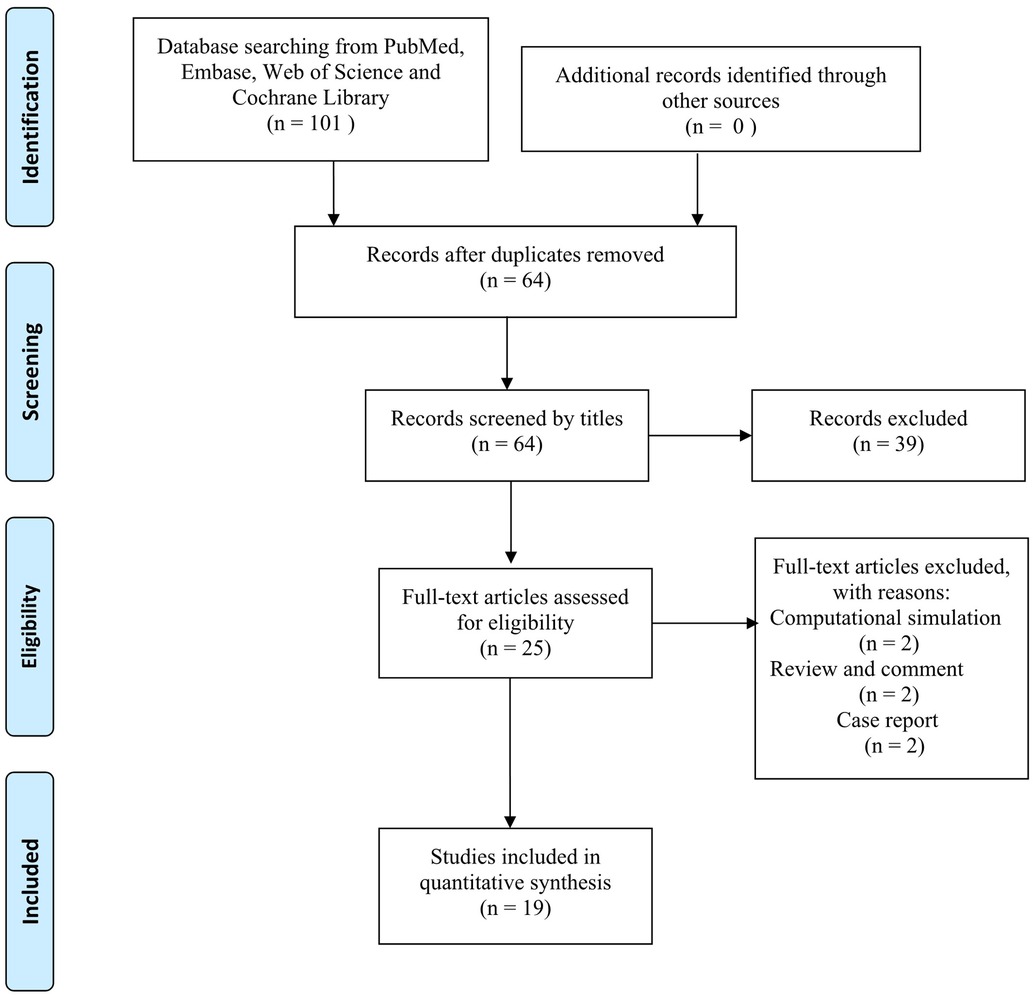
The literature search initially identified 101 articles and finally included 19 articles in this systematic review according to the inclusion and exclusion criteria (31–49) (Figure 1). Among the 19 articles, 2 articles were pure radiological studies (31, 40). There were three pairs of cognate articles (six articles) that were published in different years (38, 39, 41, 45, 48, 49). For these coupled cognate articles, the results of the more recent articles were adopted.
Quality assessment
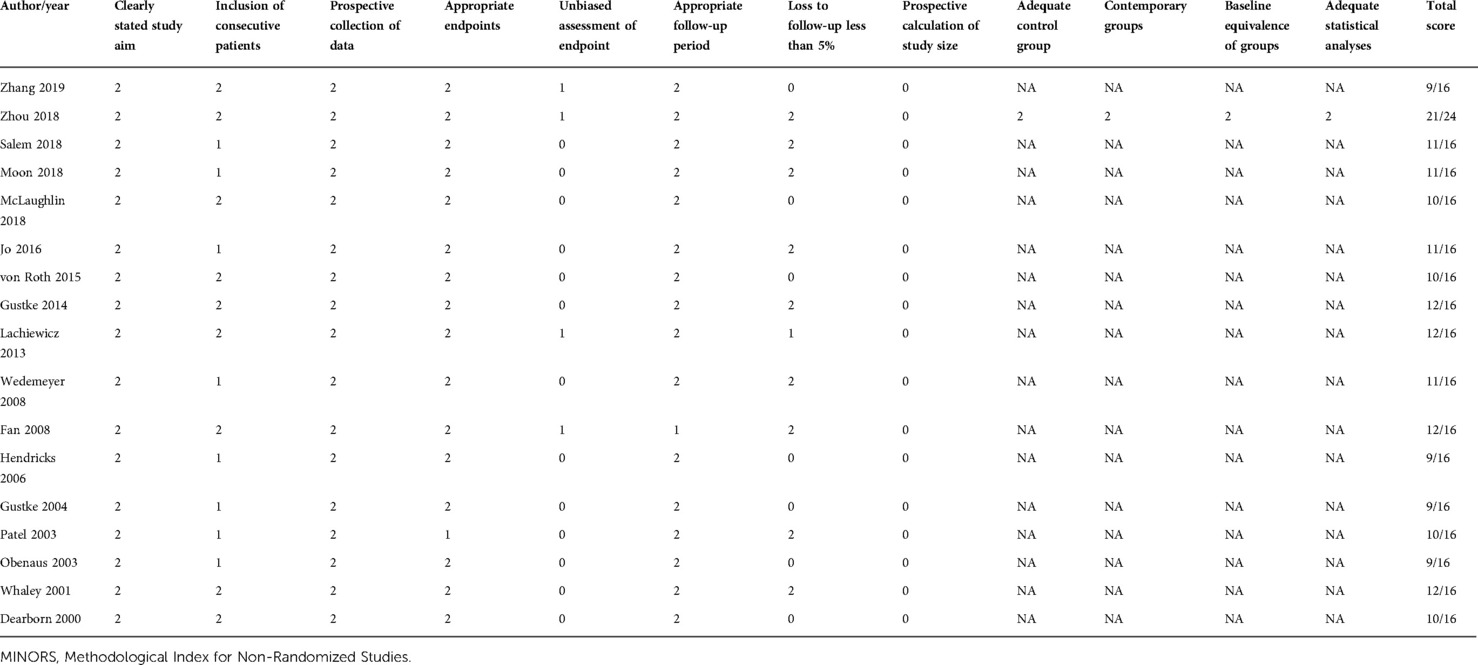
Except for the two pure radiological studies, the remaining 17 clinical studies were included in the quality assessment (32–39, 41–49) (Table 1). Only one study was a comparative study and its quality was high (21/24) (33). The other 16 studies were noncomparative studies, with a mean MINORS score of 10.5, which indicated that the general quality of these studies was relatively low. Therefore, a further meta-analysis was not conducted.
Demographics and characteristics
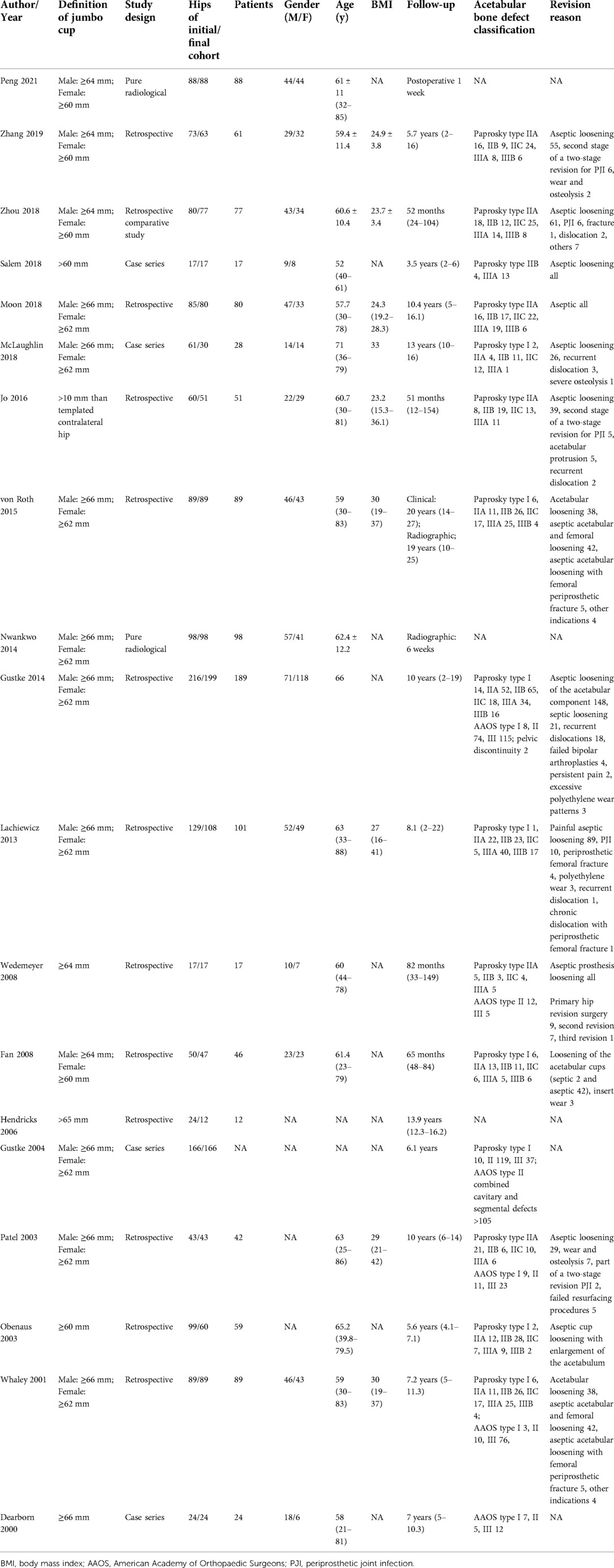
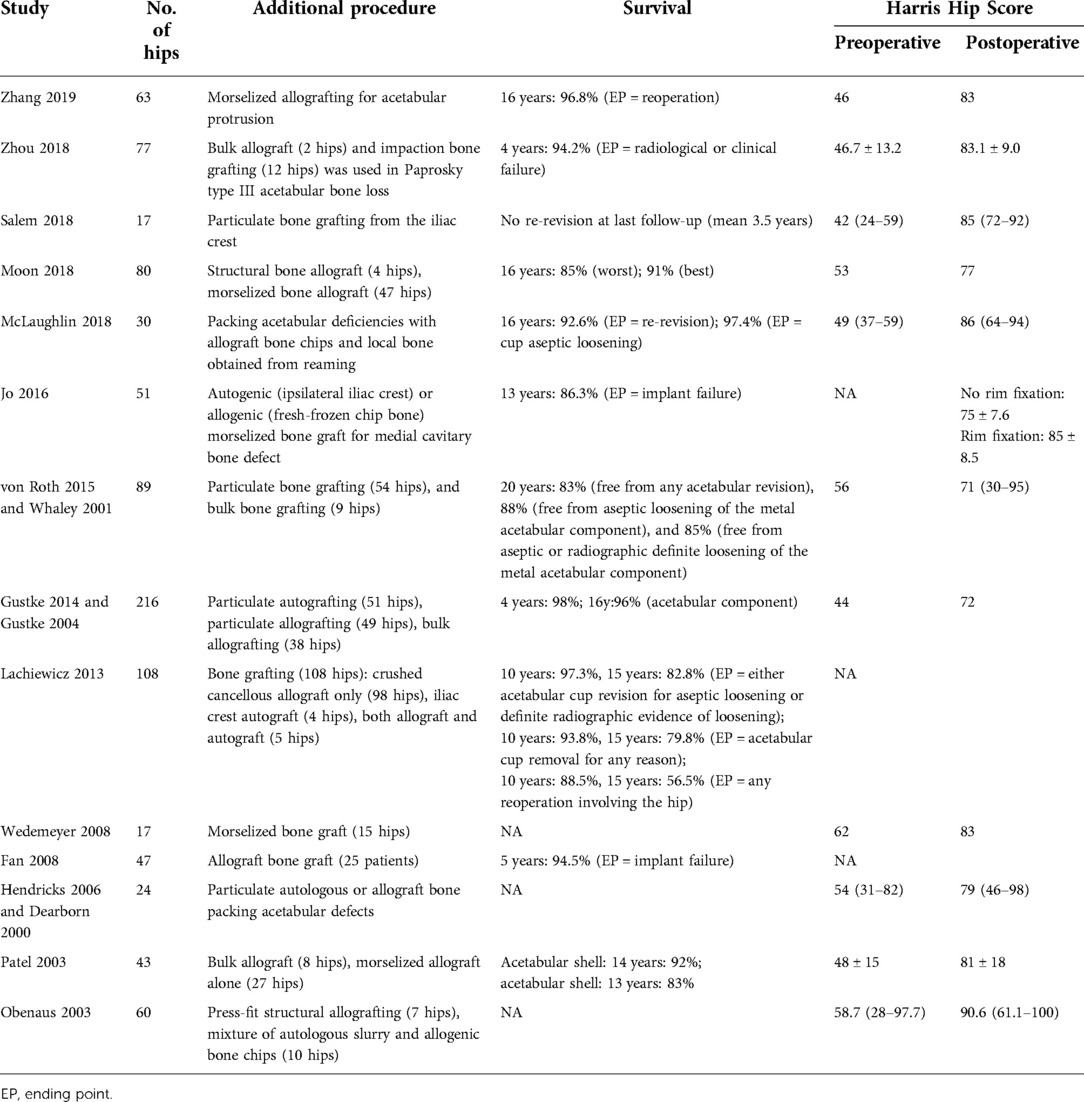
A total of 1,406 hips were initially included in the review (Table 2). To analyze the clinical results, the two pure radiological studies were removed and the results of the cognate articles were merged and adjusted. As a result, 953 hips in 14 studies were included in the analysis of clinical results (32–39, 41–44, 46, 47) (Tables 3–5). The patients who underwent rTHA had a mean age of 62.5 years. The mean follow-up was 9.3 years. In the radiological result analysis part, 631 hips in 11 studies were included (31–34, 37, 40, 43, 44, 47–49). The data of the hip center position and leg-length discrepancy were extracted and analyzed (Table 6).
Definition of the jumbo cup
There were two main definitions of the jumbo cup among the studies. One was a diameter >66 mm for males and >62 mm for females and was usually adopted in European and American studies (35, 36, 39–42, 45, 46, 48). The other was a diameter >64 mm for males and >60 mm for females and was usually adopted in Asian studies (31–33, 44). Other definitions included diameter >60 mm (34, 47), >64 mm (43), >65 mm (38), >66 mm (49), and diameter >10 mm than templated contralateral hip (37).
Clinical analysis
Bone defect evaluation
All 14 studies reported the severity of acetabular bone defect. The Paprosky classification was adopted in 13 studies of 881 hips (32–37, 39, 41–44, 46, 47). Paprosky type IIB accounted for the largest proportion (26.6%, 234/881), followed by type IIA (22.5%, 198/881), type IIIA (21.6%, 190/881), type IIC (18.5%, 163/881), type IIIB (7.4%, 65/881), and type I (3.5%, 31/881). The AAOS classification was utilized in five studies with 372 hips (41, 43, 46, 48, 49). AAOS type III occupied the most (62.1%, 231/372), followed by type II (30.1%, 112/372), type I (7.3%, 27/372), and type IV (0.5%, 2/372). In most studies, additional procedures such as structural bone grafting and press-fit bone grafting were also performed to fill the severe acetabular bone defect.
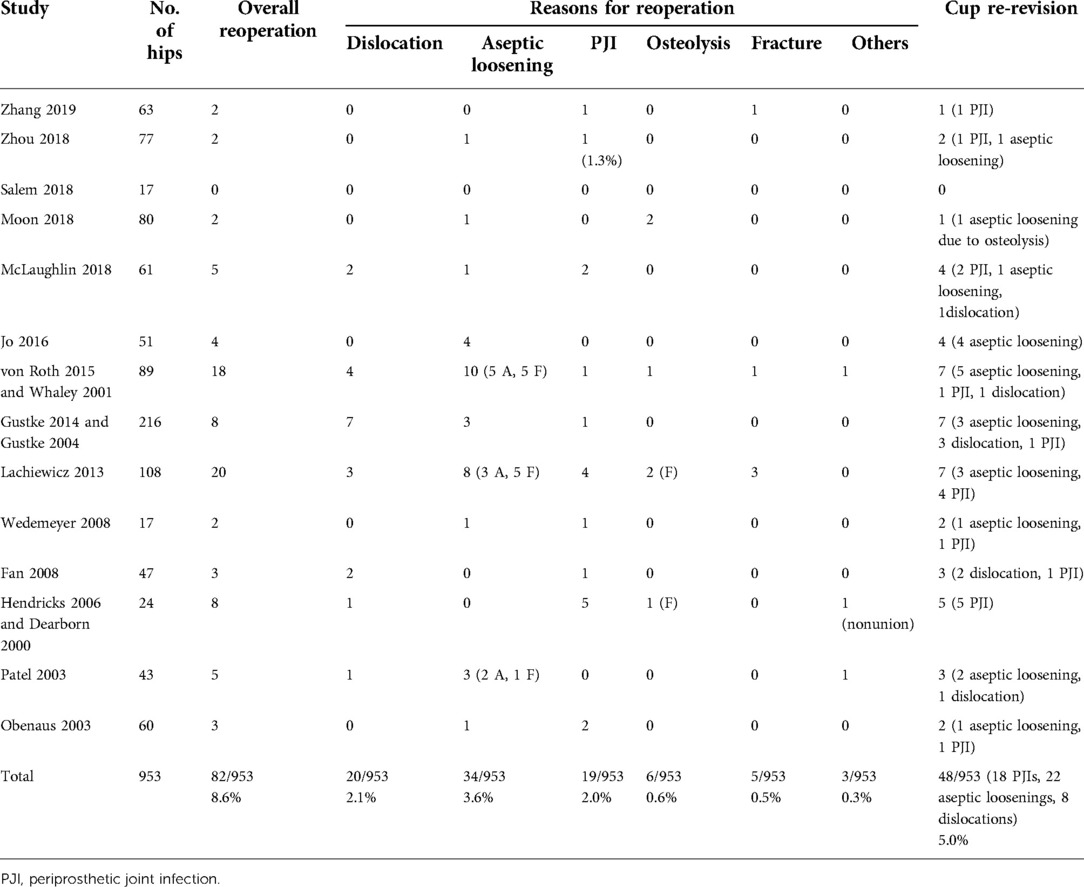
Reoperation
All 14 clinical studies reported the rate of reoperation. The overall reoperation rate was 8.6% (82/953). The most common reasons for reoperation were aseptic loosening and dislocation with an incidence of 3.6% and 2.1%, respectively. Removal of the jumbo cup was defined as failure. The failure rate of the jumbo cups was 5.0% (48/953). Among the 48 failed jumbo cups, 22 were removed for aseptic loosening, 18 were removed for periprosthetic joint infection (PJI), and 8 were removed for dislocation. The survivorship of the jumbo cups was 95.0% in the mean follow-up of 9.3 years.
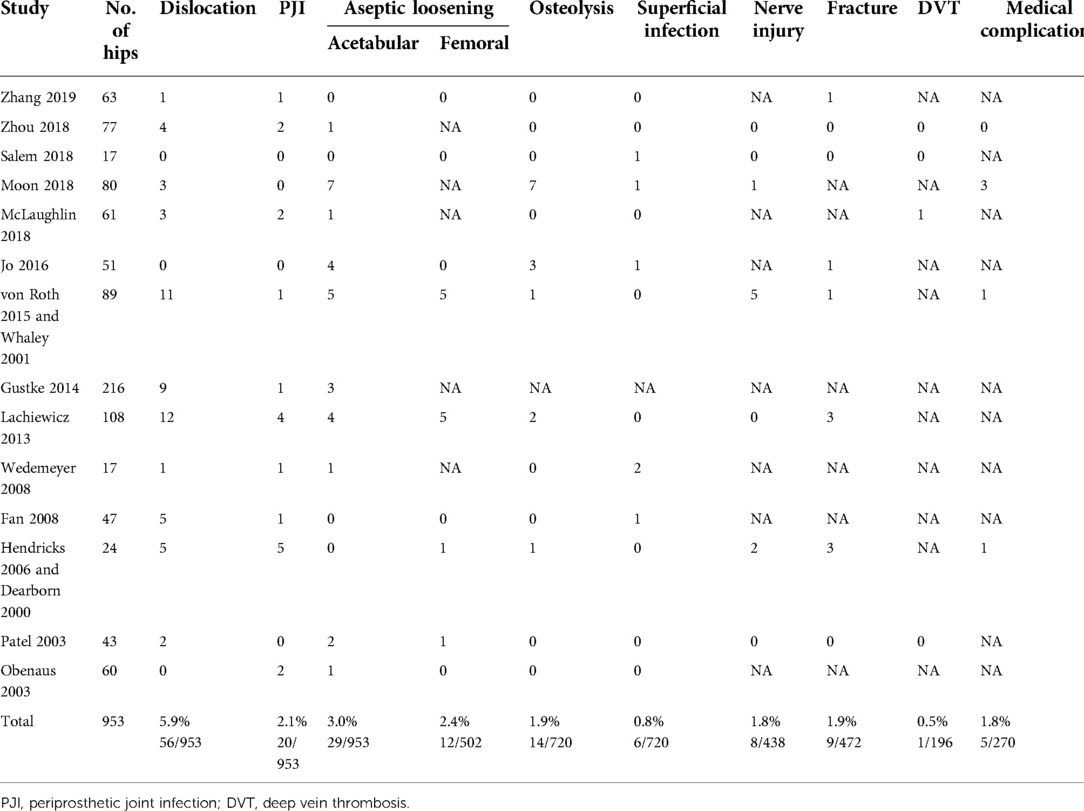
Complications
All 14 clinical studies reported complications. Due to the lack of a clear definition of complication, the overall complication rate was not calculated. Dislocation was the most common complication with a rate of 5.9%, followed by aseptic loosening (3.0% in acetabular and 2.4% in femoral) and PJI (2.1%).
Dislocation
Dislocation was the most frequent complication with a prevalence of 5.9% (56/953). Of the 56 dislocations, 20 (35.7%) accepted reoperation, with 7 re-revisions of the acetabular cup [five studies (36, 39, 41, 44, 46)], 7 femoral and liner re-revisions [three studies (39, 41, 42)], 4 femoral head and/or liners exchange [four studies (36, 39, 41, 42)], one femoral re-revision [one study (39)], and 1 resection arthroplasty [one study (41)].
Aseptic loosening
The incidence of jumbo cup aseptic loosening was 3.0% [29 of 953 hips, 10 studies (33, 35–37, 39, 41–43, 46, 47)]. Among these cases, 22 were managed with acetabular re-revision, 5 refused reoperation, and 2 could not receive re-revision for medical problems.
Periprosthetic joint infection
PJI was the third most common complication after dislocation and aseptic loosening, with a rate of 2.1% [20 of 953 hips, 10 studies (32, 33, 36, 38, 39, 41–44, 47)]. Only one patient was treated with antibiotics only for his poor physical condition as he could not tolerate re-revision. The remaining 19 cases of PJI were treated with re-revision and the jumbo cups were removed.
Harris Hip Score
Eleven studies (687 hips) reported the pre- and postoperative Harris Hip Score (HHS) (32–36, 38, 39, 41, 43, 46, 47). The mean preoperative HHS was 49.4 (poor) and improved to 78.2 (fair) at the latest follow-up.
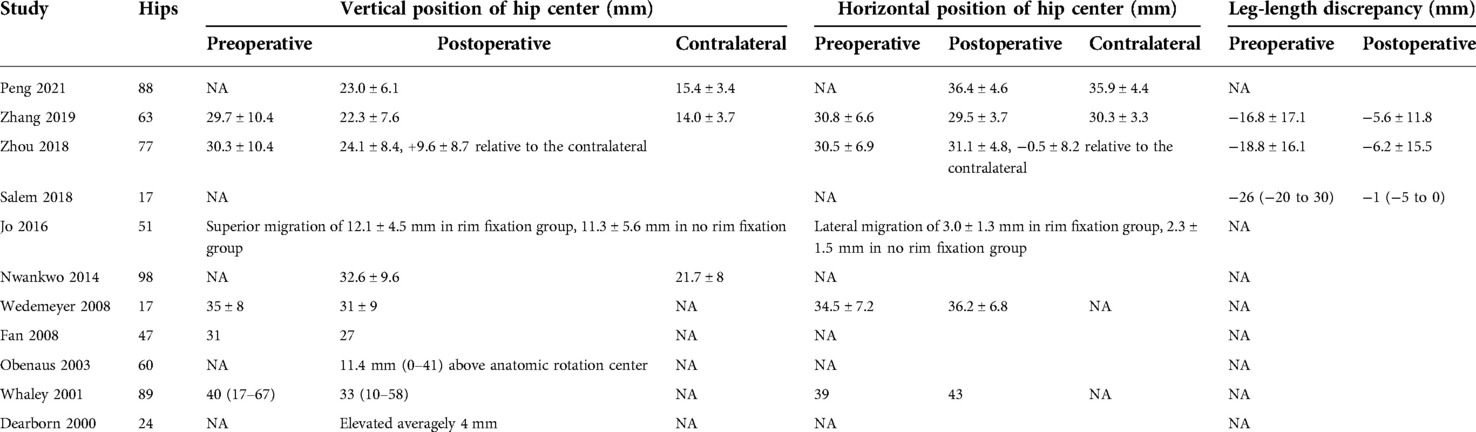
Radiological measurements
Vertical position of the hip center
Seven studies (461 hips) reported the postoperative vertical distance of hip center elevation relative to the contralateral hip center (31–33, 37, 40, 47, 49). The postrevision hip center was elevated 10.3 mm on average. Five studies (293 hips) compared the pre- and postoperative vertical positions of the hip center (32, 33, 43, 44, 48). Compared with the preoperative condition, the postrevision hip center dropped 6.2 mm on average in the vertical position.
Horizontal position of the hip center
Four studies (279 hips) reported the postoperative lateral migration of the hip center relative to the contralateral hip center (31–33, 37). The revision hip center moved 0.4 mm laterally on average. Four studies compared the pre- and postoperative horizontal positions of the hip center (32, 33, 43, 48). The postoperative hip center migrated 1.4 mm laterally on average compared with the preoperative position.
Leg-length discrepancy
Three studies reported an improvement of LLD (32–34). The mean LLD was corrected from a preoperative 18.8 mm to a postoperative 5.4 mm.
Discussion
The jumbo cup has been used for acetabular bone defect reconstruction in rTHA for a long time. To the best of our knowledge, this is the first systematic review to evaluate the evidence of a jumbo cup in rTHA. In general, the results indicated that the jumbo cup was a favorable option for acetabular reconstruction in rTHA for satisfying survivorship and acceptable complication rates.
As was summarized previously, there was no unified definition for the jumbo cup. The definition differed between the studies and could be influenced by the factors of time, race, and surgeon preference. Therefore, to a greater extent, the jumbo cup represents a special idea for acetabular reconstruction. By using a “very large” cup in this study, the contact area with the host bone increased; thereby, the goal of three-point stability and bone ingrowth was achieved.
With respect to postoperative complications, dislocation occupied the first position, with the highest rate of 5.9%. Therefore, we should lay emphasis on this complication and try to place the large diameter femoral head component to reduce the rate of dislocation. We should also identify the patients with high risk of dislocation in advance according to the reported risk factors related to dislocation after rTHA, such as advanced age, history of instability, and prior revision history (50). However, this rate of dislocation (5.9%) is also acceptable because the rate of dislocation is naturally high after rTHA, with 5%–35% in various studies (51–54). In a meta-analysis by Guo et al. that included 4,656 rTHAs, the accumulated incidence of postoperative dislocation was 9.04% (55). Many factors contribute to the high rate of dislocation after rTHA. Due to the extensive exposure in revision arthroplasty, the soft tissue deconstruction process is more severe, especially in revision for PJI because of the thorough debridement procedure. In addition, the posterolateral approach is commonly applied in rTHA, which also leads to injuries of the abduction muscles and an increased risk of dislocation (56, 57). Moreover, the rotation center may not restore in its original position and the offset may also be unsatisfying after rTHA. All these factors may lead to soft tissue imbalance and further postoperative dislocation. However, most dislocations can be addressed by conservative therapy; dislocation is just the second cause for reoperation. Therefore, it is also unnecessary to harbor too much fear for dislocation.
The rate of reoperation was 8.6% and the re-revision of the jumbo cups was 5.0%. Aseptic loosening was the primary mode of failure leading to reoperation and re-revision of the jumbo cups. This may be related to the fixation mechanism of the jumbo cup, which increases the contact area with the host bone to achieve bone ingrowth. Nevertheless, the local host bone may become severely ossified and the bioactivity of the implanted bone is also unreliable. In addition, there is some bone loss in the filing process. These elements can impede bone ingrowth and further lead to a failure of fixation. Hence, if the intraoperative findings indicate that the condition of the local host bone is poor for bone ingrowth, the rotation center elevation technique should be adopted to provide more contact area as well as better bioactivity of the host bone, which is beneficial for bone ingrowth and biomechanical instability.
The radiological outcome indicated that the rotation center position was elevated postoperatively compared with the original anatomical position. This is quite understandable for the combination of the rotation center elevation technique to achieve successful bone ingrowth as mentioned before. Another finding is that the elevation of the rotation center position has already existed preoperatively due to the acetabular bone defect, which also attained a certain degree of correction through the rTHA. The mean postoperative LLD was only 5.4 mm, which is quite acceptable and has no adverse influence on the patient's feeling and limb function. The Harris Hip Score also improved significantly, which indicated that the general condition (pain, activity, deformity, and range of motion) of the hip improved after rTHA. The revised hip could be regarded as meeting the need for daily life, as the mean postoperative HHS was up to the fair level. Thus, although in situ reconstruction of the rotation center is the gold standard in rTHA, good clinical results can also be received in the condition of rotation center elevation.
PJI is a disastrous complication that keeps troubling arthroplasty surgeons. For rTHA, the risk of PJI is higher than in primary THA. The rate of PJI in postrevision THA was in the range of 1.3%–17.3% from different registers (58–60). Fröschen et al. retrospectively analyzed 68 rTHAs using custom-made acetabular implants for Paprosky IIIA or IIIB acetabular bone defect reconstruction; the rate of postoperative PJI was unexpectedly up to 22% (61). In systematic reviews of other reconstruction methods for acetabular bone defect, the PJI rates of the custom triflange acetabular component and cup-cage technique were 6.2% and 3.3%, respectively (21, 22). In our systematic review of the jumbo cup for rTHA, the rate of PJI was only 2.1%, which can be regarded as relatively low. We speculate that this reduced rate of PJI may be due to the simplified procedure in acetabular reconstruction of jumbo cups, which may save surgical time and lower the risk of PJI. Another reason is that the jumbo cup method requires a smaller amount of implant compared with other methods, such as porous metallic augments, cup-cage, and monoflanged acetabular component. However, many factors can affect the rate of PJI, such as femoral revision or no revision, use of antibiotics, type of material, and implant coating design. Therefore, we still recommend that this relatively low rate of PJI should be treated with caution because of some existing bias and the relatively simple statistical method.
There are also some controversies on using the jumbo cup for rTHA. In 2016, Lachiewicz and Watters pointed out that although the jumbo cup had shown excellent 10-year survivorship, the late loosening of “first-generation” porous surfaces and wear with periprosthetic osteolysis of traditional polyethylene liners had also been reported and needed more attention (27). They also recommended the use of enhanced porous coatings, highly cross-linked polyethylene liners, and large femoral heads in jumbo cup reconstruction. Zhou et al. retrospectively compared 74 consecutive rTHAs using metal augments with a cementless hemispherical cup and 77 consecutive rTHAs using the jumbo cup (33). The biomechanical parameters of the metal augment group, such as rotator center position, leg-length discrepancy, head-cup difference, and femoral offset, are all superior to those of the jumbo cup group. In recent years, many advanced reconstruction techniques such as 3D printing, custom prosthesis, and robot-assisted arthroplasty have been developed and seem to stand for the future direction of rTHA (62–64). Even so, the results of our systematic review have already supported the jumbo cup as a successful method for acetabular reconstruction in rTHA. The development of advanced biomaterials will further improve the performance of the jumbo cup.
Our study also has several limitations, some of which are listed here. First, the quality of the included studies is relatively low, and most of these are of a single-arm design. Second, the sample size is also relatively limited. In addition, the acetabular bone defects of many included cases are mild-to-moderate and relatively easy to reconstruct. In fact, the reconstruction for severe acetabular bone defect is the real hot spot and core problem in rTHA. Therefore, if only the performance of the jumbo cup for severe acetabular defect is discussed, the results may not be presented as well as those in our study. Unfortunately, most papers report the overall survivorship and failure and do not report the relation with the extent of bone defect. Therefore, this relation was not explored in this systematic review. Certainly, on the other hand, the results can also indicate that the jumbo cup is a good option for mild-to-moderate acetabular bone defect at least.
Conclusion
In summary, according to this systematic review, the jumbo cup is a recommended method for acetabular reconstruction in rTHA. The clinical outcomes and survivorship of the jumbo cup are satisfying. However, in most cases, the acetabular bone defects are mild to moderate. Further research is still required to review its performance for severe or extreme acetabular bone defect reconstruction.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding authors.
Author contributions
WG and WW set the topic and designed the protocol. QZ and JG conducted the literature search and quality assessment. QyW, QW, and PL extracted and analyzed the data and wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by Beijing Natural Science Foundation (7202183) and National Natural Science Foundation of China (81972107).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Volpin A, Konan S, Biz C, Tansey RJ, Haddad FS. Reconstruction of failed acetabular component in the presence of severe acetabular bone loss: a systematic review. Musculoskelet Surg. (2019) 103:1–13. doi: 10.1007/s12306-018-0539-7
2. Sheth NP, Nelson CL, Springer BD, Fehring TK, Paprosky WG. Acetabular bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. (2013) 21:128–39. doi: 10.5435/JAAOS-21-03-128
3. D’Antonio JA, Capello WN, Borden LS, Bargar WL, Bierbaum BF, Boettcher WG, et al. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. (1989) 243:126–37. doi: 10.1097/00003086-198906000-00019
4. Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. (1994) 9:33–44. doi: 10.1016/0883-5403(94)90135-x
5. Jaenisch M, Wirtz DC, Kohlhof H, Gathen M, Kabir K, Koob S, et al. APP-guided assessment of acetabular defects in hip revision arthroplasty: a structured approach to a complex situation. Arch Orthop Trauma Surg. (2021):1–10. doi: 10.1007/s00402-021-04270-8
6. Wirtz DC, Jaenisch M, Osterhaus TA, Gathen M, Wimmer M, Randau TM, et al. Acetabular defects in revision hip arthroplasty: a therapy-oriented classification. Arch Orthop Trauma Surg. (2020) 140:815–25. doi: 10.1007/s00402-020-03379-6
7. Walter SG, Thomas TS, Kenndoff D, Thomas W. Mid-term follow-up after all-size acetabular revision and proposal for a stability classification system. Hip Int. (2020) 30:431–7. doi: 10.1177/1120700019839698
8. Zhang JW, Liu XL, Zeng YM, Zhai ZJ, Mao YQ, Yu DG, et al. Comparison of 3D printing rapid prototyping technology with traditional radiographs in evaluating acetabular defects in revision hip arthroplasty: a prospective and consecutive study. Orthop Surg. (2021) 13:1773–80. doi: 10.1111/os.13108
9. Meynen A, Vles G, Zadpoor AA, Mulier M, Scheys L. The morphological variation of acetabular defects in revision total hip arthroplasty—a statistical shape modeling approach. J Orthop Res. (2021) 39:2419–27. doi: 10.1002/jor.24995
10. Hasenauer MD, Paprosky WG, Sheth NP. Treatment options for chronic pelvic discontinuity. J Clin Orthop Trauma. (2018) 9:58–62. doi: 10.1016/j.jcot.2017.09.009
11. Babis GC, Nikolaou VS. Pelvic discontinuity: a challenge to overcome. EFORT Open Rev. (2021) 6:459–71. doi: 10.1302/2058-5241.6.210022
12. Cassar-Gheiti AJ, Mei XY, Afenu EA, Safir OA, Gross AE, Kuzyk P. Midterm outcomes after reconstruction of superolateral acetabular defects using flying buttress porous tantalum augments during revision total hip arthroplasty. J Arthroplasty. (2021) 36:2936–41. doi: 10.1016/j.arth.2021.03.040
13. Li GY, Zhang XQ, Chen M, Luo ZL, Ji XF, Shang XF. Modular revision strategy with bispherical augments in severe acetabular deficiency reconstruction. Int Orthop. (2022) 46:215–22. doi: 10.1007/s00264-021-05195-y
14. Loppini M, Schiavi P, Rocca AD, Traverso F, Rocca FD, Mazziotta G, et al. Double-trabecular metal cup technique for the management of Paprosky type III defects without pelvic discontinuity. Hip Int. (2018) 28:66–72. doi: 10.1177/1120700018813208
15. Chang CH, Hu CC, Chen CC, Mahajan J, Chang Y, Shih HN, et al. Revision total hip arthroplasty for Paprosky type III acetabular defect with structural allograft and tantalum trabecular metal acetabular cup. Orthopedics. (2018) 41:e861–7. doi: 10.3928/01477447-20181023-02
16. Brown NM, Morrison J, Sporer SM, Paprosky WG. The use of structural distal femoral allograft for acetabular reconstruction of Paprosky type IIIA defects at a mean 21 years of follow-up. J Arthroplasty. (2016) 31:680–3. doi: 10.1016/j.arth.2015.10.020
17. Hipfl C, Janz V, Löchel J, Perka C, Wassilew GI. Cup-cage reconstruction for severe acetabular bone loss and pelvic discontinuity: mid-term results of a consecutive series of 35 cases. Bone Joint J. (2018) 100-B:1442–8. doi: 10.1302/0301-620X.100B11.BJJ-2018-0481.R1
18. Webb JE, McGill RJ, Palumbo BT, Moschetti WE, Estok DM. The double-cup construct: a novel treatment strategy for the management of Paprosky IIIA and IIIB acetabular defects. J Arthroplasty. (2017) 32:S225–31. doi: 10.1016/j.arth.2017.04.017
19. Barlow BT, Oi KK, Lee YY, Carli AV, Choi DS, Bostrom MP. Outcomes of custom flange acetabular components in revision total hip arthroplasty and predictors of failure. J Arthroplasty. (2016) 31:1057–64. doi: 10.1016/j.arth.2015.11.016
20. Li H, Qu X, Mao Y, Dai K, Zhu Z. Custom acetabular cages offer stable fixation and improved hip scores for revision THA with severe bone defects. Clin Orthop Relat Res. (2016) 474:731–40. doi: 10.1007/s11999-015-4587-0
21. De Martino I, Strigelli V, Cacciola G, Gu A, Bostrom MP, Sculco PK. Survivorship and clinical outcomes of custom triflange acetabular components in revision total hip arthroplasty: a systematic review. J Arthroplasty. (2019) 34:2511–8. doi: 10.1016/j.arth.2019.05.032
22. Changjun C, Xin Z, Mohammed A, Liyile C, Yue L, Pengde K. Survivorship and clinical outcomes of “cup-cage” reconstruction in revision of hip arthroplasty for chronic pelvic discontinuity: a systematic review. Surgeon. (2021) 19:e475–84. doi: 10.1016/j.surge.2020.11.007
23. Wang CX, Huang ZD, Wu BJ, Li WB, Fang XY, Zhang WM. Cup-cage solution for massive acetabular defects: a systematic review and meta-analysis. Orthop Surg. (2020) 12:701–7. doi: 10.1111/os.12710
24. Walter SG, Randau TM, Gravius N, Gravius S, Fröschen FS. Monoflanged custom-made acetabular components promote biomechanical restoration of severe acetabular bone defects by metallic defect reconstruction. J Arthroplasty. (2020) 35:831–5. doi: 10.1016/j.arth.2019.10.040
25. Jasty M. Jumbo cups and morsalized graft. Orthop Clin North Am. (1998) 29:249–54. doi: 10.1016/s0030-5898(05)70323-0
26. Emerson RH Jr, Head WC. Dealing with the deficient acetabulum in revision hip arthroplasty: the importance of implant migration and use of the jumbo cup. Semin Arthroplasty. (1993) 4:2–8.10148091
27. Lachiewicz PF, Watters TS. The jumbo acetabular component for acetabular revision: curtain calls and caveats. Bone Joint J. (2016) 98-B:64–7. doi: 10.1302/0301-620X.98B1.36139
28. Nwankwo C, Dong NN, Heffernan CD, Ries MD. Do jumbo cups cause hip center elevation in revision THA? A computer simulation. Clin Orthop Relat Res. (2014) 472:572–6. doi: 10.1007/s11999-013-3169-2
29. Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Br Med J. (2009) 339:b2535. doi: 10.1136/bmj.b2535
30. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. (2003) 73:712–6. doi: 10.1046/j.1445-2197.2003.02748.x
31. Peng YW, Shen JM, Zhang YC, Sun JY, Du YQ, Zhou YG. Jumbo cup in hip joint renovation may cause the center of rotation to increase. World J Clin Cases. (2021) 9:6300–7. doi: 10.12998/wjcc.v9.i22.6300
32. Zhang J, Huang Y, Zhou B, Zhou Y. Mid-term follow-up of acetabular revision arthroplasty using jumbo cups. Orthop Surg. (2019) 11:811–8. doi: 10.1111/os.12522
33. Zhou B, Zhou Y, Yang D, Tang H, Shao H, Huang Y. The utilization of metal augments allows better biomechanical reconstruction of the hip in revision total hip arthroplasty with severe acetabular defects: a comparative study. J Arthroplasty. (2018) 33:3724–33. doi: 10.1016/j.arth.2018.08.027
34. Salem Eid A, Kotb A, Elshabrawy W. Cementless jumbo cups for revision of failed Furlong prosthesis. A case series. J Clin Orthop Trauma. (2020) 11:56–61. doi: 10.1016/j.jcot.2018.08.009
35. Moon JK, Ryu J, Kim Y, Yang JH, Hwang KT, Kim YH. Acetabular revision arthroplasty using press-fitted jumbo cups: an average 10-year follow-up study. Arch Orthop Trauma Surg. (2019) 139:1149–60. doi: 10.1007/s00402-019-03214-7
36. McLaughlin JR, Lee KR. Acetabular revision arthroplasty using an uncemented deep profile jumbo component: a ten to sixteen year follow-up study. J Arthroplasty. (2018) 33:496–9. doi: 10.1016/j.arth.2017.09.002
37. Jo WL, Lim YW, Im JH, Kim SC, Kwon SY, Kim YS. Comparative study of peripheral rim fixation using jumbo cup in revisional hip arthroplasty. Hip Pelvis. (2017) 29:24–9. doi: 10.5371/hp.2017.29.1.24
38. Hendricks KJ, Harris WH. Revision of failed acetabular components with use of so-called jumbo noncemented components. A concise follow-up of a previous report. J Bone Joint Surg Am. (2006) 88:559–63. doi: 10.2106/JBJS.E.00389
39. von Roth P, Abdel MP, Harmsen WS, Berry DJ. Uncemented jumbo cups for revision total hip arthroplasty: a concise follow-up, at a mean of twenty years, of a previous report. J Bone Joint Surg Am. (2015) 97:284–7. doi: 10.2106/JBJS.N.00798
40. Nwankwo CD, Ries MD. Do jumbo cups cause hip center elevation in revision THA? A radiographic evaluation. Clin Orthop Relat Res. (2014) 472:2793–8. doi: 10.1007/s11999-014-3632-8
41. Gustke KA, Levering MF, Miranda MA. Use of jumbo cups for revision of acetabulae with large bony defects. J Arthroplasty. (2014) 29:199–203. doi: 10.1016/j.arth.2012.11.010
42. Lachiewicz PF, Soileau ES. Fixation, survival, and dislocation of jumbo acetabular components in revision hip arthroplasty. J Bone Joint Surg Am. (2013) 95:543–8. doi: 10.2106/JBJS.L.00758
43. Wedemeyer C, Neuerburg C, Heep H, von Knoch F, von Knoch M, Löer F, et al. Jumbo cups for revision of acetabular defects after total hip arthroplasty: a retrospective review of a case series. Arch Orthop Trauma Surg. (2008) 128:545–50. doi: 10.1007/s00402-007-0501-x
44. Fan CY, Chen WM, Lee OK, Huang CK, Chiang CC, Chen TH. Acetabular revision arthroplasty using jumbo cups: an experience in Asia. Arch Orthop Trauma Surg. (2008) 128:809–13. doi: 10.1007/s00402-007-0492-7
45. Gustke KA. Jumbo cup or high hip center: is bigger better. J Arthroplasty. (2004) 19:120–3. doi: 10.1016/j.arth.2004.02.012
46. Patel JV, Masonis JL, Bourne RB, Rorabeck CH. The fate of cementless jumbo cups in revision hip arthroplasty. J Arthroplasty. (2003) 18:129–33. doi: 10.1054/arth.2003.50038
47. Obenaus C, Winkler H, Girtler R, Huber M, Schwägerl W. Extra-large press-fit cups without screws for acetabular revision. J Arthroplasty. (2003) 18:271–7. doi: 10.1054/arth.2003.50049
48. Whaley AL, Berry DJ, Harmsen WS. Extra-large uncemented hemispherical acetabular components for revision total hip arthroplasty. J Bone Joint Surg Am. (2001) 83:1352–7. doi: 10.2106/00004623-200109000-00010
49. Dearborn JT, Harris WH. Acetabular revision arthroplasty using so-called jumbo cementless components: an average 7-year follow-up study. J Arthroplasty. (2000) 15:8–15. doi: 10.1016/s0883-5403(00)90999-9
50. Faldini C, Stefanini N, Fenga D, Neonakis EM, Perna F, Mazzotti A, et al. How to prevent dislocation after revision total hip arthroplasty: a systematic review of the risk factors and a focus on treatment options. J Orthop Traumatol. (2018) 19:17. doi: 10.1186/s10195-018-0510-2
51. Khatod M, Barber T, Paxton E, Namba R, Fithian D. An analysis of the risk of hip dislocation with a contemporary total joint registry. Clin Orthop Relat Res. (2006) 447:19–23. doi: 10.1097/01.blo.0000218752.22613.78
52. Wetters NG, Murray TG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ. Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res. (2013) 471:410–6. doi: 10.1007/s11999-012-2561-7
53. Jo S, Jimenez Almonte JH, Sierra RJ. The cumulative risk of re-dislocation after revision THA performed for instability increases close to 35% at 15years. J Arthroplasty. (2015) 30:1177–82. doi: 10.1016/j.arth.2015.02.001
54. Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. (2002) 84:1788–92. doi: 10.2106/00004623-200210000-00008
55. Guo L, Yang Y, An B, Yang Y, Shi L, Han X, et al. Risk factors for dislocation after revision total hip arthroplasty: a systematic review and meta-analysis. Int J Surg. (2017) 38:123–9. doi: 10.1016/j.ijsu.2016.12.122
56. Kurkis GM, Chihab S, Farley KX, Anastasio AT, Bradbury TL, Guild GN. Anterior revision hip arthroplasty is associated with higher wound complications but fewer dislocations compared to posterior revision hip surgery. J Arthroplasty. (2021) 36:250–4. doi: 10.1016/j.arth.2020.07.030
57. Robertson RN, Parks NL, Ho H, Hopper RH Jr, Hamilton WG. Does approach influence the dislocation rate following head and liner exchange in revision hip arthroplasty. J Arthroplasty. (2022) 37:336–41. doi: 10.1016/j.arth.2021.10.005
58. Badarudeen S, Shu AC, Ong KL, Baykal D, Lau E, Malkani AL. Complications after revision total hip arthroplasty in the Medicare population. J Arthroplasty. (2017) 32:1954–8. doi: 10.1016/j.arth.2017.01.037
59. Gold PA, Garbarino LJ, Sodhi N, Anis HK, Ehiorobo JO, Kurtz SM, et al. A 6-year trends analysis of infections after revision total hip arthroplasty. Ann Transl Med. (2019) 7:76. doi: 10.21037/atm.2019.01.48
60. Goldman AH, Sierra RJ, Trousdale RT, Lewallen DG, Berry DJ, Abdel MP. The Lawrence D. Dorr surgical techniques / technologies award: why are contemporary revision total hip arthroplasties failing? An analysis of 2500 cases. J Arthroplasty. (2019) 34:S11–11S16. doi: 10.1016/j.arth.2019.01.031
61. Fröschen FS, Randau TM, Hischebeth G, Gravius N, Gravius S, Walter SG. Mid-term results after revision total hip arthroplasty with custom-made acetabular implants in patients with Paprosky III acetabular bone loss. Arch Orthop Trauma Surg. (2020) 140:263–73. doi: 10.1007/s00402-019-03318-0
62. Hao Y, Luo D, Wu J, Wang L, Xie K, Yan M, et al. A novel revision system for complex pelvic defects utilizing 3D-printed custom prosthesis. J Orthop Translat. (2021) 31:102–9. doi: 10.1016/j.jot.2021.09.006
63. von Hertzberg-Boelch SP, Wagenbrenner M, Arnholdt J, Frenzel S, Holzapfel BM, Rudert M. Custom made monoflange acetabular components for the treatment of Paprosky type III defects. J Pers Med. (2021) 11(4):283. doi: 10.3390/jpm11040283
Keywords: jumbo cup, acetabular bone defect, revision total hip arthroplasty, survivorship, rotation hip center
Citation: Wang Q, Wang Q, Liu P, Ge J, Zhang Q, Guo W and Wang W (2022) Clinical and radiological outcomes of jumbo cup in revision total hip arthroplasty: A systematic review. Front. Surg. 9:929103. doi: 10.3389/fsurg.2022.929103
Received: 26 April 2022; Accepted: 24 August 2022;
Published: 4 October 2022.
Edited by:
Carlos Suarez-Ahedo, Hospital Médica Sur, MexicoReviewed by:
Dejin Yang, Beijing Jishuitan Hospital, ChinaSebastian Walter, University Hospital of Cologne, Germany
Paul Simon Unwin, Independent Researcher, United Kingdom
© 2022 Wang, Wang, Liu, Ge, Zhang, Guo and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Weiguo Wang am9pbnR3d2dAMTYzLmNvbQ== Wanshou Guo enJnd3NidWNtQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
 Qiuyuan Wang
Qiuyuan Wang Qi Wang2,3,†
Qi Wang2,3,† Pei Liu
Pei Liu Juncheng Ge
Juncheng Ge Weiguo Wang
Weiguo Wang