- Department of Hepatobiliary Surgery, Aerospace Center Hospital, Beijing, China
Background: Cholecystitis with incarcerated gallstones (CIG) is a type of acute abdomen in the field of hepatobiliary surgery. Whether gallbladder-preserving surgery (GPS) can be performed to treat it, however, depends on the improvement of gallbladder contractile function. The present study aimed to investigate the changes in gallbladder contractile function and its influencing factors after minimally invasive GPS for CIG.
Methods: A total of 95 patients with CIG treated in the Aerospace Center Hospital between May 2017 and May 2019 were enrolled as the study subjects. All patients received minimally invasive GPS. The patients' operation-related conditions (including stone removal success rate, duration of surgery, intraoperative blood loss, etc.), changes in gallbladder contractile function, and influencing factors of GPS were analyzed.
Results: Among the 95 patients included in the study, the success rate of stone removal was 100%, the duration of surgery was 76.0 ± 26.5 min, and the intraoperative blood loss was 10.17 ± 4.43 ml. The rate of good gallbladder contractile function at one and two years after surgery was significantly higher than before surgery (P < 0.05). Age, duration of surgery, stone recurrence, and diabetes were the independent risk factors for postoperative gallbladder contractile function (P < 0.05).
Conclusion: Minimally invasive GPS for patients with CIG has a good curative effect. The changes in gallbladder contractile function after the surgery are influenced by many factors.
Introduction
Cholecystitis with incarcerated gallstones (CIG), a type of acute abdomen in the field of hepatobiliary surgery, is a common form of cholecystitis. The main treatment for the disease is laparoscopic cholecystectomy. With the growth in understanding of the physiological function of the gallbladder and the development of choledochoscopy technology, the concept of gallbladder-preserving surgery (GPS) has been gradually accepted by physicians and patients, and the indications for GPS have slowly relaxed. However, the question of how to avoid recurrence has become the most important research direction for minimally invasive GPS. To date, a number of studies have confirmed that stone recurrence is related to dynamic gallbladder injury or gallbladder contractile dysfunction (1–3). As such, the present study enrolled 95 patients with CIG and treated them with minimally invasive GPS, after which any changes in gallbladder contractile function were observed and the factors affecting the recovery of gallbladder contractile function analyzed.
Methods
General Information
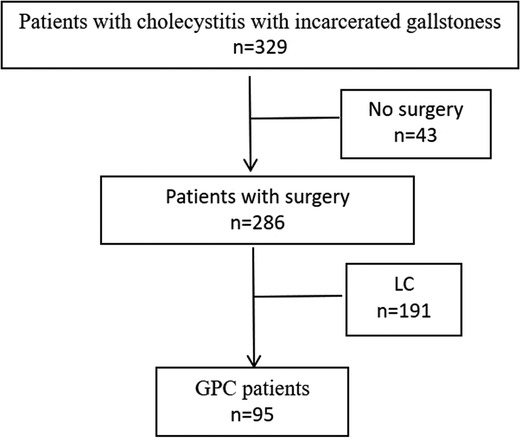
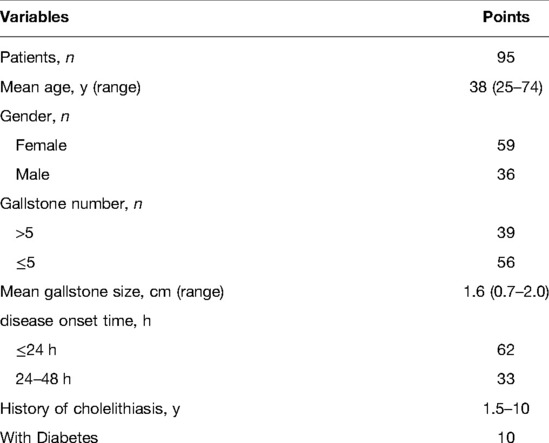
A total of 329 patients with CIG and a disease onset time of <48 h who were treated at the Aerospace Center Hospital from May 2017 to May 2019 were selected, 43 patients who did not undergo surgical treatment and 191 patients who underwent laparoscopic cholecystectomy for laparoscopic cholecystectomy were excluded. The remaining 95 CIG patients were included, including 36 males and 59 females, aged 25–74 years (Figure 1). All patients were definitively diagnosed with stone incarceration of the gallbladder neck or duct by imaging examination (B-ultrasound, computed tomography, etc.). The patient has the willingness and needs of gallbladder preservation. After treatment, the symptoms were relieved and the body temperature was normal. The gallbladder function test was performed to evaluate the preoperative gallbladder contractile function, which showed that there was no obvious edema of the gallbladder wall, and the plasma cholecystokinin level of each patient was normal. Patients with liver and kidney dysfunction, a history of upper abdominal surgery, acute attack of non-gallbladder inflammation, mental disorders, blood system diseases, etc., were excluded. The study was conducted with the informed consent of all patients.
Surgical Procedure
Minimally invasive GPS was conducted as follows: (1) The patient was placed in a supine position under general anesthesia, routine disinfection was performed, and surgical drapes were put in place. (2) An incision of 1.0 cm was made at the umbilicus, a 10-mm trocar was placed to establish pneumoperitoneum, and pressure was controlled within 10–12 mmHg. (3) A laparoscope was placed through the trocar, and the abdominal cavity was observed to determine the volume, location, appearance, and surrounding organs of the gallbladder. (4) A 5-mm trocar was placed under the xiphoid process, a 12-mm disposable trocar was placed under the costal margin of the right midclavicular line, and the bottom of the gallbladder was suspended on the abdominal wall. (5) The bottom of the gallbladder was incised with an electrocoagulation hook, a choledochoscope was placed via the 12-mm disposable trocar hole to explore the gallbladder and determine the location of the incarcerated stones in the gallbladder neck or duct, and corresponding methods were adopted to remove stones of different diameters (see Figures 2A–C). (6) The gallbladder exploration was continued, and 2–3 spiral valves in the gallbladder duct were observed to ensure that the stones were removed completely and that the bile reflux could be seen (see Figure 2D). (7) The gallbladder incision was sutured with 4/0 absorbable sutures, and the mucosal layer and seromuscular layer were sutured continuously (see Figure 2E), ensuring that there was no bile fistula or bleeding. (8) After surgery, the patients were treated with antibiotics, Danning tablets, ursodeoxycholic acid, and other drug therapies according to the doctor's advice. The patients were advised to take medication regularly for 6 months after surgery, and they were followed up regularly for two years.
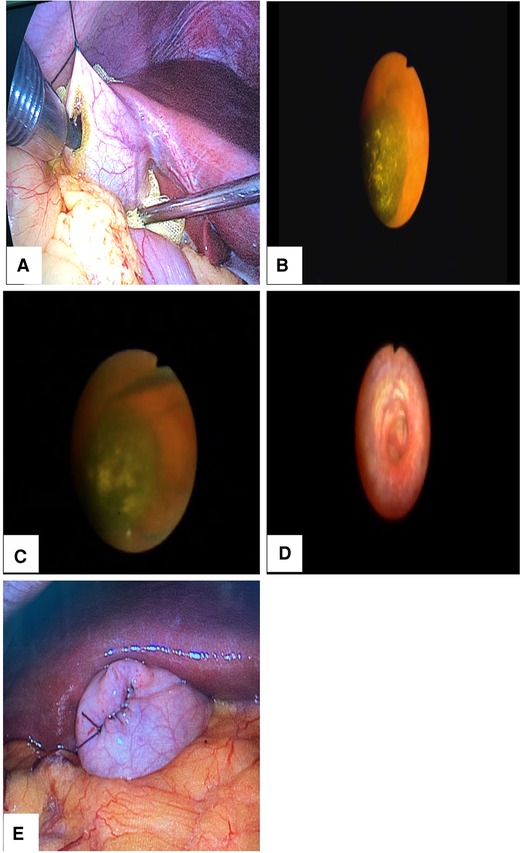
Figure 2. Intraoperative illustration. (A) The bottom of the gallbladder was suspended from the abdominal wall, and the choledochoscope was inserted into the gallbladder through a 12-mm disposable trocar. (B) Exploration found incarcerated gallbladder neck stones. (C) A stone extraction basket was used to remove the stone. (D) Exploration was undertaken to at least two spiral valves of the cystic duct after stone extraction to ensure that no stones remained and that the bile reflux was good. (E) The gallbladder incision was sutured with 4/0 absorbable sutures.
Observation Indexes
The patients' operation-related conditions, including stone removal success rate, duration of surgery, intraoperative blood loss, etc., were analyzed, and the gallbladder contractile function before and after surgery were compared. On this basis, the influencing factors for gallbladder contractile function were analyzed. To calculate maximum contractile rate of the gallbladder before and after surgery (i.e., the proportion of the difference between the fasting gallbladder volume and the minimum residual volume of the gallbladder to the fasting gallbladder volume). Three-dimensional ultrasound was used to measure the size of the gallbladder: after 6 h of fasting, the long, transverse and anterior-posterior diameters of the gallbladder were measured. After eating a standard fat meal (4), the measurement was repeated. The ellipsoid method was used, that is, gallbladder volume = 0.52 × long diameter * front and rear diameter * transverse diameter (5). Using this method, the recovery of gallbladder function was determined, with good function being indicated by a maximum gallbladder contractile rate of ≥50% and poor function being indicated by a maximum gallbladder contractile rate of <50%.
Statistical Analysis
The SPSS 24.0 software was used for statistical analysis. Measurement data were expressed as mean ± standard deviation and compared using a t-test. Count data were expressed as a percentage (n[%]) and compared using a χ2 test. Univariate and multivariate logistic regression analyses were also carried out, with good gallbladder contractile function as the dependent variable and gender, age, and other factors as the independent variables. P < 0.05 was considered statistically significant.
Results
Analysis of Operation-Related Conditions
Among the 95 patients, there were 39 with more than five gallstones and 56 with five or fewer gallstones. The average gallstone size was 1.6 cm, with a range of 0.7–2.0 cm. There were 10 patients with diabetes (see Table 1). The success rate of stone removal was 100% (95/95), and none of the patients required conversion to laparotomy. The duration of surgery was 76.0 ± 26.5 min, and the intraoperative blood loss was 10.17 ± 4.43 ml. None of the patients experienced special discomfort after surgery. All patients undertook gentle exercise and ate liquid food on the first day after surgery, and they were hospitalized for two to four days, with an average of three days.
Comparison of Good Gallbladder Contractile Function Before Surgery and One and Two Years After Surgery
The rate of good gallbladder contractile function was higher at one and two years after surgery than before surgery (P < 0.05; see Table 2).

Table 2. Comparison of good rate of gallbladder contractile function before operation and 1 and 2 years after operation (n [%]).
Analysis of Factors Affecting Changes in Gallbladder Contractile Function
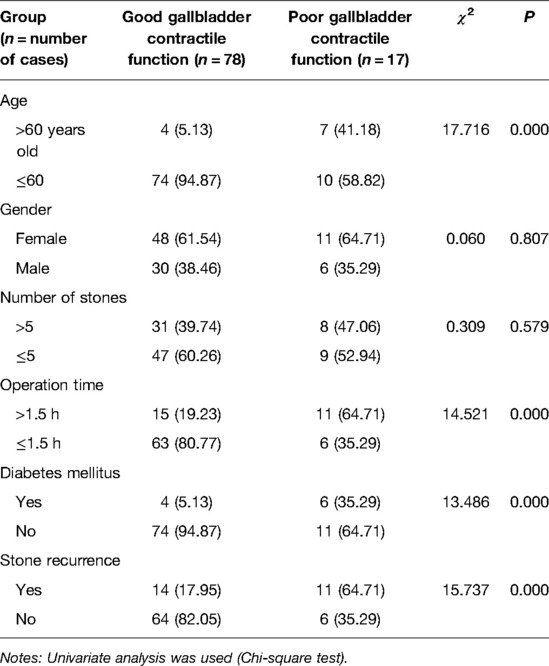
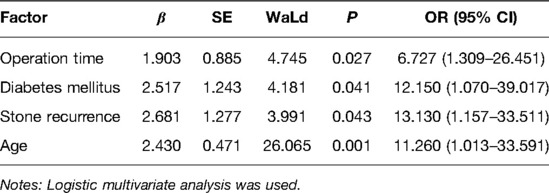
In the univariate analysis, duration of surgery, age, and diabetes mellitus were associated with postoperative gallbladder contractile function (see Table 3), and the differences were statistically significant (P < 0.05). In the logistic multivariate analysis, stone recurrence, age, diabetes mellitus, and duration of surgery were independent risk factors for the postoperative recovery of gallbladder contractile function (P < 0.05; see Table 4).
Discussion
Gallstones can cause abdominal pain, fever, nausea, vomiting, and other symptoms; stones can stimulate the gallbladder wall for a long time and even carry the risk of canceration (6).
In the past, laparoscopic cholecystectomy was the gold standard for the treatment of gallstones. With the improvement of minimally invasive technology, however, choledochoscopy combined with laparoscopic minimally invasive GPS was proposed and widely applied. Furthermore, a study reported its advantages from multiple angles (7). Despite these advantages, the recurrence of gallstones is a significant problem related to minimally invasive GPS, causing patients a lot of worry. To solve this problem, many researchers have sought preventive measures for stone recurrence (8).
To date, several studies have reported a low recurrence rate of gallstones during long-term follow-up after minimally invasive GPS: Gao et al. conducted a long-term follow-up of 508 patients who underwent minimally invasive GPS, finding a gallstone recurrence rate of only 1.2% (9); Zha et al. reported 12-month, 36-month, and 60-month follow-up gallstone recurrence rates of 0%, 3.32%, and 5.64%, respectively, in 316 cases (10); and the Qu et al. found that most instances of recurrence occurred within two years of gallbladder-preserving cholecystolithotomy, with recurrence rates of 2.3%, 3.7%, and 7.6% at 6, 12, and 24 months, respectively(11). Regarding longer-term follow-up, the Liu et al. team reported that the five-year recurrence rate of minimally invasive GPS for stones in the neck of gallbladder was only 2.3% (12).
In the past, the gallbladder was not preserved during the removal of stones in the treatment of incarcerated stones in the neck or duct of the gallbladder; however, the incarceration of stones affects gallbladder contractile function, making it impossible to correctly evaluate the function of the gallbladder. This means that blind cholecystectomy requires the removal of the gallbladder in some patients with normal gallbladder function.
Patients whose stone incarceration time was <48 h and whose gallbladder wall had no obvious congestion or edema were enrolled in the present study, and minimally invasive choledochoscopic GPS was adopted to improve the stone clearance rate, alleviate symptoms, preserve gallbladder function, and improve quality of life. The results revealed that the success rate of stone removal in all patients was 100%, and the rate of good gallbladder contractile function was higher one and two years after surgery than before surgery (P < 0.05). These results suggest that minimally invasive GPS has good short-term and long-term outcomes.
There are many factors leading to gallbladder dysfunction (13). Combined with an in-depth analysis of relevant research, the results of the present study revealed that the recovery degree of gallbladder contractile function after surgery differs to a certain extent in different patients with cholecystitis. The altered gallbladder contractility may not only result from the inflammatory response within the gallbladder secondary to the stones but may also contribute to stone formation and cholecystitis (14). Actively mastering the factors affecting the recovery of postoperative gallbladder contractile function is therefore of great significance to its prognosis.
The results of the present study revealed that duration of surgery, age, diabetes mellitus, and stone recurrence are associated with postoperative gallbladder contractile function. On this basis, logistic multivariate analysis was carried out, and the results revealed that these factors were independent risk factors affecting the recovery of gallbladder contractile function after surgery (P < 0.05). There are several reasons for each of these independent risk factors:
Duration of surgery: Surgery that continues for too long not only increases the degree of trauma but also induces aseptic inflammation and edema of the gallbladder wall, which affects the recovery of gallbladder contractile function.
Age: Organ function gradually declines with age, resulting in low immunity. This prolongs the healing time of the gallbladder wall and increases the risk of cholecystitis recurrence after surgery, directly affecting the normal recovery of gallbladder contractile function.
Diabetes mellitus: The existence of an abnormal lipid metabolism, metabolic disorders, and other problems easily induces hyperlipidemia, which is a risk factor affecting gallstone formation. Furthermore, autonomic nerve injury, weakened gallbladder emptying function, gallbladder artery vascular disease, and other problems affect gallbladder emptying function (15).
Stone recurrence: Postoperative stone recurrence directly delays the recovery of gallbladder contractile function.
These results indicate that actively mastering the indications for minimally invasive GPS is the key to ensuring a good surgical effect and maintaining normal gallbladder contractile function in patients with CIG.
Conclusion
Minimally invasive gallbladder-preserving surgery was performed on patients with stone-incarcerated cholecystitis, and the curative effect was definite. The changes of gallbladder contractile function after operation were related to the patient's age, diabetes mellitus, operation time and postoperative stone recurrence. Close attention to the above factors can improve the level of patient prognosis and recovery.
Data Availability Statement
The original contributions presented in the study are included in the article/Suplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethic Committe of Aerospace Center Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
Conception and design of the research: XNA, ZYW, CGO; Acquisition of data: XNA, TFW, QZ; Analysis and interpretation of the data: XNA, TFW, QZ; Statistical analysis: XNA, ZYW; Writing of the manuscript: XNA; Critical revision of the manuscript for intellectual content: ZYW. All authors contributed to the article and approved the submitted version.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li Q-F, Xu X, Ge X. Gallstone recurrence after minimally-invasive cholecystolithotomy with gallbladder reservation: a follow-up of 720 cases. Eur Rev Med Pharmacol Sci. (2015) 19(8):1403–6. PMID: 25967715
2. Lyu ZH, Yu L, Han EH, Hong W, Hu XJ, Pei F. Ultrasonographic signs as factors for recurrence of gallstones and polypoid lesion of the gallbladder after gallbladder—preserving surgery. J Clin Hepatol. (2016) 32(4):746–9 (in Chinese). doi: 10.3969/j.issn.1001-5256.2016.04.029
3. Portincasa P, Di Ciaula A, vanBerge-Henegouwen GP. Smooth muscle function and dysfunction in gallbladder disease. Curr Gastroenterol Rep. (2004) 6:151–62. doi: 10.1007/s11894-004-0043-0
4. Dodds WJ, Groh WJ, Darweesh RM, Lawson TL, Kishk SM, Kern MK. Sonographic measurement of gallbladder volume. AJR Am J Roentgenol. (1985) 145(5):1009–11. doi: 10.2214/ajr.145.5.1009
5. Wedmann B, Schmidt G, Wegener M, Coenen C, Ricken D, Dröge C. Sonographic evaluation of gallbladder kinetics: in vitro and vivo comparison of different method to assess gallbladder emptying. J Clin Ultrasound. (1991) 19(6):341–9. doi: 10.1002/jcu.1870190604
6. Shabanzadeh DM, Sorensen LT, Jorensen T. Association between screen-detected gallstone disease and cancer in a cohort study. Gastroenterology. (2017) 152(8):1965–74. doi: 10.1053/j.gastro.2017.02.013
7. Tan YY, Zhao G, Wang D, Wang JM, Tang JR, Ji ZL. A new strategy of minimally invasive surgery for cholecystolithiasis: calculi removal and gallbladder preservation. Dig Surg. (2013) 30(4-6):466–71. doi: 10.1159/000357823
8. Du QC, Wang YY, Hu CL, Zhou Y. Reconsideration of indications for choledochoscopic gallbladder-preserving surgery and preventive measures for postoperative recurrence of gallstones. Wideochir Inne Tech Maloinwazyjne. (2020) 15(1):87–96. doi: 10.5114/WIITM.2019.88647
9. Gao D-K, Wei S-H, Li W, Ren J, Ma XM, Gu CW, et al. Totally laparoscopic gallbladder-preserving surgery: a minimally invasive and favorable approach for cholelithiasis. Exp Ther Med. (2015) 9(2):395–8. doi: 10.3892/etm.2014.2107
10. Zha Y, Zhou ZZ, Chen XR, Gan P, Tan J. Gallbladder-preserving cholelithotomy in laparoscopic and flexible choledochoscopic era: a report of 316 cases. Surg Laparosc Endosc Percutan Tech. (2013) 23(2):167–70. doi: 10.1097/SLE.0b013e31828a0b5f
11. Qu Q, Chen WJ, Liu X, Wang WD, Hong T, Liu W, et al. Role of gallbladder-preserving surgery in the treatment of gallstone diseases in young and middle-aged patients in China: results of a 10-year prospective study. Surgery. (2020) 167(2):283–9. doi: 10.1016/j.surg.2019.09.001
12. Liu JS, Zhao QK, Chen JF, Zhang HL. (in Chinese) Analysis of the factors of gallbladder stone recurrence after minimal invasive gallbladder preserved choledochoscopy. China J Endosc. (2015) 21(5):525–7.
13. Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder dysfunction: cholecystitis, choledocholithiasis, cholangitis, and biliary dyskinesia. Prim Care. (2017) 44(4):575–97. doi: 10.1016/j.pop.2017.07.002
14. Lavoie B, Nausch B, Zane EA, Leonard MR, Balemba OB, Bartoo AC, et al. Disruption of gallbladder smooth muscle function is an early feature in the development of cholesterol gallstone disease. Neurogastroenterol Motil. (2012) 24:e313–24. doi: 10.1111/j.1365-2982.2012.01935.x
15. Gustafsson U, Sahlin S, Einarsson C. Biliary lipid composition in patients with cholesterol and pigment gallstones and gallstone-free subjects: deoxycholic acid does not contribute to formation of cholesterol gallstones. Eur J Clin Invest. (2000) 30(12):1099–106. doi: 10.1046/j.1365-2362.2000.00740.x
Keywords: minimally invasive gallbladder-preserving surgery, cholecystitis with incarcerated gallstones, gallbladder contractile function, influence factor, gallbladder
Citation: Ai X, Wang T, Zhang Q, Ouyang C and Wu Z (2022) Changes in Gallbladder Contractile Function and its Influencing Factors After Minimally Invasive Gallbladder-Preserving Surgery for Cholecystitis With Incarcerated Gallstones. Front. Surg. 9:926141. doi: 10.3389/fsurg.2022.926141
Received: 22 April 2022; Accepted: 21 June 2022;
Published: 14 July 2022.
Edited by:
Pasquale Cianci, Azienda Sanitaria Localedella Provincia di Barletta Andri Trani (ASL BT), ItalyReviewed by:
Vincenzo Lizzi, Azienda Ospedaliero-Universitaria Ospedali Riuniti di Foggia, ItalyDimitri Krizzuk, Aurelia Hospital, Italy
Copyright © 2022 Ai, Wang, Zhang, Ouyang and Wu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhen-Yu Wu eTE4Mzc1MTAwNXlAMTI2LmNvbQ==
Specialty section: This article was submitted to Visceral Surgery, a section of the journal Frontiers in Surgery
 Xiang-Nan Ai
Xiang-Nan Ai Zhen-Yu Wu
Zhen-Yu Wu