
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg. , 05 September 2022
Sec. Otorhinolaryngology - Head and Neck Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.925824
 Bruno Popić1
Bruno Popić1 Andrijana Kopić2,3*
Andrijana Kopić2,3* Dubravka Holik4
Dubravka Holik4 Kristijan Dinjar1,3
Kristijan Dinjar1,3 Vlatko Kopić1,3
Vlatko Kopić1,3 Marko Matijević5
Marko Matijević5 Fran Popić5
Fran Popić5
Advanced periorbital basal cell carcinomas may necessitate orbital exenteration and consequent vision loss, which significantly reduces patients’ life quality. Orbital reconstruction is a demanding surgical procedure due to the complex orbital anatomy and vital structures located in the orbit. In this report, we presented an 83-year-old patient with advanced basal cell carcinoma that had expanded into the orbit. An orbitotomy was performed to remove the tumor completely while preserving the eye function. Orbital reconstruction was performed by a standard surgical method using a titanium mesh modeled according to a natural phantom skull. This maintained the eye function and achieved satisfactory facial esthetics.
Basal cell carcinoma (BCC) is the most common malignant skin tumor and accounts for approximately 90% skin cancers (1, 2). The incidence of skin malignancy with orbital invasion is 2%–4% (3, 4). BCC most commonly occurs in the lower eyelid and medial canthus (5). Initially, BCC shows no signs of orbital penetration, although tumor mass is always palpable (6). With disease progression, BCC erodes the bone. Penetration of the periorbita and the involvement of extraocular muscles can restrict eye movement and lead to eyeball dislocation (7). Computed tomography (CT) is a suitable imaging technique for bone destruction diagnosis, and magnetic resonance imaging is reliable for detecting soft tissue orbital invasion (8). In the case of diagnostically confirmed invasion of the malignancy into the orbit, therapy planning requires the collaboration of a multidisciplinary team (2). When planning the surgical procedure, it is necessary to take into the account biological behavior of the tumor, histological findings, and the possibility of perineural invasion, which requires extended edges for surgical excision (1, 2). After orbital exenteration, recurrences occur in about 5% of cases. Inadequate BCC treatment leads to orbital invasion and, consequently, a greater number of orbital exenterations (9), which was confirmed by Bartley et al. in 80% of cases with failed first treatment (surgery or/and radiotherapy) (10).
In this case report, we present a case where we performed lateral orbital wall reconstruction with a titanium mesh previously adapted and modeled using a natural phantom skull and avoided orbital exenteration. Reconstruction of orbital wall defects after tumor resection due to complex anatomy is also a challenge even for experienced maxillofacial surgeons.
An 83-year-old patient was admitted in 2018 to our Department of Maxillofacial and Oral Surgery, University Hospital Center Osijek, because of a tumor in the frontozygomatic region on the right side. In 2010, the patient was treated in the surgical department of another institution. According to the pathohistological findings, it was a skin basal cell carcinoma. Due to the irregularity of the preparation, it was not possible to assess the status of the edges of the preparation, so the patient was referred to our department. He neglected that recommendation for next eight years and did not perform the examination in our department. In October 2018, the patient was examined by an ophthalmologist, who performed lower eyelid ectropion correction twice and referred the patient to our department now due to suspected recurrence of the tumor frontotemporally in the right side.
Examination revealed a serious impaired general condition of the patient (Parkinson's disease, moving difficulties, prostate hyperplasia, and poorly regulated hypertension). In the local status, we found a tumorous change of 3 cm × 3 cm in the frontozygomatic region fixed to the right on the base, right eye lower eyelid ectropion, while the regional lymph nodes were not palpable.
During the preoperative preparation, a native and postcontrast orbital CT was performed and a lobulated solid expansive formation of the zygomatic region on the right (2.5 cm × 2.3 cm × 2.1 cm) was determined, which infiltrated and eroded the frontozygomatic extension on the right side 1.8 cm × 1.7 cm long (Figures 1A,B).
In the infratemporal space on the right, a solid formation size 1.5 cm × 1.0 cm was differentiated without right eye bulbus infiltration. Tumor had two lobes, one lobe that affected the skin and was fixed to the eroded bone and the other part that was in the infratemporal cavity and penetrated into the orbit through the lateral wall of the orbit, so the tumor was folded over the lateral edge of the orbit.
Based on the CT findings, we decided to operate the tumor with resection of the lateral orbital wall while preserving the eyeball. With written informed consent of the patient, under general anesthesia, an incision was made in the skin and subcutaneous tissue around the tumor, with adequate surgical margins (Figure 2A). During the operation, the tumor was removed completely with the resection of the lateral orbital wall, part of the body and the beginning of the arch of the zygomatic bone, the associated periosteum, orbital fat, and the lateral canthal ligament. Right eyeball and ocular muscles remained preserved (Figure 2B).
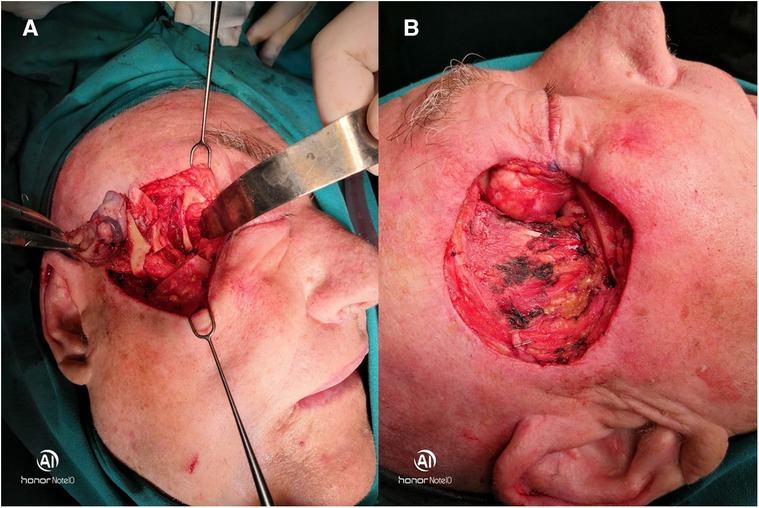
Figure 2. (A,B) Surgical approach with the resection of the lateral orbital wall and completely removed tumor with a preserved eyeball.
Bone defect of the lateral orbital wall was reconstructed using a titanium mesh previously adapted and modeled using a natural phantom skull (Figure 3).
Once the mesh was fixed in a satisfactory position, a portion of the temporalis muscle and temporal fascia was pulled over it. The entire defect was then covered with a Thiersch skin graft taken from the right thigh. The skin graft was fixed with sutures to the surrounding skin with compression with a cotton ball with Vaseline gauze. The site of Thiersch transplant on the right thigh was covered with a Kaltostat, which was removed after three weeks. Compression of the skin graft and sutures were removed after one week. It should be emphasized that the patient did not agree to local skin flaps, which was good because a thin skin graft allowed more adequate control of the occurrence of possible tumor recurrence. The patient was controlled regularly for two years by a maxillofacial surgeon and an ophthalmologist. A control CT scan was performed without recurrence of the tumor, eye motility was in order, as was the function of eyelids closing (Figure 4). Mild asymmetry of the right side of the face was left behind.
Malignant primary or secondary tumors that penetrate the orbit from the surrounding skin, maxillary sinus, or neurocranium require surgical treatment. The incidence of malignant tumors of the skin of the periorbital region is constantly increasing, and accordingly, an increased number of indications for orbital exenteration are expected. Kesting et al. in their study reported that 99.3% of patients underwent orbital exenteration due to a malignant tumor, and in 23.8% of cases, the cause was the progression of skin cancer into the orbit (11). Usually, orbital exenteration is performed when the malignant process affects the periorbital tissue, external eye muscles, orbital apex, and in case of vision loss. Orbital reconstruction is the most challenging part of midface surgery, especially in preserved eyeballs, and aims to restore the contours, volume of the orbit, and position of the eyeball. The decision on reconstruction is made taking into account the available materials and techniques of reconstruction and always in agreement with the patient (12). In the case of a preserved eyeball, functional and esthetic defects are common, and they include enophthalmos, hypophthalmus, eyelid malposition, epiphora, and diplopia. Subsequent surgical corrections of structural disorders are often unsuccessful, so it is necessary to choose the optimal primary method of orbital reconstruction whenever it is possible. During orbital reconstruction, it is important to keep the eyelids in a normal position to protect the eye from external influences (13). A review of the literature suggests various approaches to midface reconstruction and the focus is on midface reconstruction as a whole, but a structural approach to the orbit is a bit lacking. Thus, there is no consensus on the classification of orbital defects and consequently no standardized reconstructions (14). Titanium mesh implants, bone grafts, or polyether-ether-ketone implants can be used to reconstruct the orbit. The success of the reconstruction depends not only on the type of material used for the orbital reconstruction but also on the possibility of visualizing the bone defect (15). Kim et al., like Ellis and Messo, reported that titanium mesh is an excellent alloplastic material for orbital reconstruction (16, 17). The low rejection rate, extrusion and infection, is attributed to the characteristic of titanium to cause an inflammatory and fibrous response of the surrounding tissue (18). The use of individual titanium meshes shortens the duration of the operation because it is possible to position the mesh better without unnecessary multiple removal and placement of implants, which further traumatizes the soft tissue and sensitive structures of the orbit (18). Computer-assisted design/computer-aided fabrication (CAD/CAM) reconstruction of individual implants is an effective procedure that allows for very precise reconstruction of the complex orbital anatomy. CAD/CAM 3D planning and customized implants are now considered the gold standard in most centers (19–21).
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
BP contributed to data gathering and drafting. AK contributed to revision and drafting. DH, VK, MM, and KD contributed to data gathering and final revision. All authors contributed to the article and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Furdova A, Lukacko P. Periocular basal cell carcinoma predictors for recurrence and infiltration of the orbit. J Craniofac Surg. (2017) 1:e84–7. doi: 10.1097/SCS.0000000000003242
2. Tyers AG. Orbital exenteration for invasive skin tumours. Eye. (2006) 20(10):1165–70. doi: 10.1038/sj.eye.6702380
3. Perlman GS, Hornblass A. Basal cell carcinoma of the eyelids: a review of patients treated by surgical excision. Ophthal Surg. (1976) 7:23–7. PMID: 1004805
4. Howard GR, Nerad JA, Carter KD, Whitaker DC. Clinical characteristics associated with orbital invasion of cutaneous basal cell and squamous cell tumours of the eyelid. Am J Ophthalmol. (1992) 113:123–33. doi: 10.1016/S0002-9394(14)71523-5
5. Wang JK, Liao SL, Jou JR, Lai PC, Kao SCS, Hou PK, et al. Malignant eyelid tumours in Taiwan. Eye. (2003) 17(2):216–20. doi: 10.1038/sj.eye.6700231
6. Leibovitch I, McNab A, Sullivan T, Davis G, Selva D. Orbital invasion by periocular basal cell carcinoma. Ophthalmology. (2005) 112:717–23. doi: 10.1016/j.ophtha.2004.11.036
7. McNab AA, Francis IC, Benger R, Crompton JL. Perineural spread of cutaneous squamous cell carcinoma via the orbit, clinical features and outcome in 21 cases. Ophthalmology. (1997) 104(9):1457–62. doi: 10.1016/S0161-6420(97)30116-X
8. Williams LS, Mancuso AA, Mendenhall WM. Perineural spread of cutaneous squamous and basal cell carcinoma: CT and MR detection and its impact on patient management and prognosis. Int J Radiol Oncol Biol Phys. (2001) 49(4):1061–9. doi: 10.1016/S0360-3016(00)01407-3
9. Rahman I, Cook AE, Leatherbarrow B. Orbital exenteration: a 13 year Manchester experience. Br J Ophthalmol. (2005) 89(10):1335–40. doi: 10.1136/bjo.2004.062471
10. Bartley GB, Garrity JA, Waller RR, Henderson JW, Ilstrup DM. Orbital exenteration at the Mayo Clinic: 1967–1986. Ophthalmology. (1989) 96(4):468–73. doi: 10.1016/s0161-6420(89)32872-7
11. Kesting MR, Koerdt S, Rommel N, Mücke T, Wolff KD, Nobis CP, et al. Classification of orbital exenteration and reconstruction. J Craniomaxillofac Surg. (2017) 45(4):467–73. doi: 10.1016/j.jcms.2017.01.003
12. Legocki AT, Miles BA. Considerations in orbital reconstruction for the oncologic surgeon: critical versus optimal objectives. Indian J Plast Surg. (2019) 52(2):231–7. doi: 10.1055/s-0039-1696624
13. Imola MJ, Schramm VL Jr. Orbital preservation in surgical management of sinonasal malignancy. Laryngoscope. (2002) 112(08 Pt 1):1357–65. doi: 10.1097/00005537-200208000-00007
14. Cordeiro PG, Chen CM. A 15-year review of midface reconstruction after total and subtotal maxillectomy: part I. Algorithm and outcomes. Plast Reconstr Surg. (2012) 129(01):124–36. doi: 10.1097/PRS.0b013e318221dca4
15. Saqr OM, Kotb AR, EL-Mahallawy AS, El Dibany RM, Mahmoud H. Moursy reconstruction of the orbital skeleton using computer-aided individualized titanium mesh compared to conventional titanium mesh. Alex Dent J. (2020) 45:50–5. doi: 10.21608/adjalexu.2020.79933
16. Kim YC, Jeong WS, Park T-K, Choi JW, Koh KS, Oh TS. The accuracy of patient specific implant prebented with 3D printed rapid prototype model for orbital wall reconstruction. J Craniomaxillofac Surg. (2017) 45:928–36. doi: 10.1016/j.jcms.2017.03.010
17. Ellis E 3rd, Messo E. Use of nonresorbable alloplastic implants for internal orbital reconstruction. J Oral Maxillofac Surg. (2004) 62:873–81. doi: 10.1016/j.joms.2003.12.025
18. Mwenifumbo S, Li M, Chen J, Beye A, Soboyejo W. Cell/surface interactions on laser micro-textured titanium-coated silicon surfaces. J Mater Sci Mater Med. (2007) 18:9–23. doi: 10.1007/s10856-006-0658-9
19. Chepurnyi Y, Chernogorskyi D, Petrenko O, Kopchak A. Reconstruction of post-traumatic orbital defects and deformities with custom-made patient-specific implants: evaluation of the efficacy and clinical outcome. Craniomaxillofac Trauma Reconstr Open. (2019) 3:e9–17. doi: 10.1055/s-0039-1685505
20. Baumann A, Sinko K, Dorner G. Late reconstruction of the orbit with patient-specific implants using computer-aided planning and navigation. J Oral Maxillofac Surg. (2015) 73(Suppl 12):S101–6. doi: 10.1016/j.joms.2015.06.149
Keywords: lateral orbital wall, basal cell carcinoma, penetration, reconstruction, titanium mesh
Citation: Popić B, Kopić A, Holik D, Dinjar K, Kopić V, Matijević M and Popić F (2022) Lateral orbital wall reconstruction after basal cell carcinoma penetration—Case report. Front. Surg. 9:925824. doi: 10.3389/fsurg.2022.925824
Received: 21 April 2022; Accepted: 8 August 2022;
Published: 5 September 2022.
Edited by:
Ingo Todt, Bielefeld University, GermanyReviewed by:
Merima Kasumovic, University of Zenica, Bosnia and Herzegovina© 2022 Popić, Kopić, Holik, Dinjar, Kopić, Matijević and Popić. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrijana Kopić YW5kcmlqYW5ha29waWNAZ21haWwuY29t
Specialty Section: This article was submitted to Otorhinolaryngology—Head and Neck Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.