
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Surg. , 04 July 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.922637
This article is part of the Research Topic Surgical Innovation and Advancement in Orthopedics View all 57 articles
Background: The clinical efficacy of platelet-rich plasma (PRP) in the treatment of total joint replacement (TJR) remains inconclusive. In this paper, systematic review and meta-analysis was adopted to assess the efficacy of using PRP for the treatment of TJR.
Methods: A comprehensive search of Medline, Embase, and Cochrane library databases for randomized controlled trial (RCT) articles recording data of PRP for TJR was conducted from inception to February 2022. Outcomes concerned were pain, range of motion (ROM), WOMAC score, length of hospital stay (LOS), hemoglobin (Hb) drop, total blood loss, wound healing rate, and wound infection. The methodological quality of the included RCTs was evaluated by using the Cochrane Risk of Bias Tool 2.0 (RoB 2.0). The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) was utilized to assess the level of evidence for the outcomes. Subgroup analysis was conducted according to the type of TJR.
Results: Ten RCTs were included in the meta-analysis. In the TKA subgroup, the available data demonstrated that there were significant differences in the outcomes of pain and Hb drop, while it was the opposite of ROM, WOMAC score, LOS, total blood loss, wound healing rate, and wound infection. In the THA subgroup, no significant differences could be seen between two groups in the outcomes of LOS and wound infection. However, the PRP group gained a higher wound healing rate in the THA subgroup.
Conclusion: The application of PRP did not reduce blood loss but improved the wound healing rate. However, more prospective and multicenter studies are warranted to confirm these results.
Total joint replacement (TJR) is a common surgical procedure in which the weight-bearing surface of a joint is replaced to restore its capacity and function (1–5). During the operation, TJR can cause many complications, including blood loss, deep vein thrombosis, and wound complications (5). These disorders have a poor prognosis and can cause severe pain, which increases the length of hospital stay (LOS), medical costs, and even the risk of deep vein thrombosis (DVT) (6). Nowadays, multiple approaches have been used to manage complications arising after TJR, including fibrin tissue adhesive, epidural infusion, and oral opioids (3, 7, 8). However, the treatment outcome is not satisfactory and is accompanied by side effects (9).
Platelet-rich plasma (PRP) has been increasingly used in the field of sports injuries and has attracted extensive attention due to its high safety, simple preparation, and ease of extraction (10). PRP is a highly concentrated platelet solution extracted from autologous whole blood by centrifugation. PRP can release high concentrations of autogenous growth factors, including transforming growth factor β1 (TGF-β1), platelet-derived growth factor, insulin-like growth factor (IGF), and epidermal growth factor (EGF), which can promote chondrocyte proliferation and vascular growth to accelerate wound site repair (11). A large amount of fibrin also contributes to wound repair, which facilitates wound contraction and provides scaffolding (12, 13). Previous meta-analysis demonstrated that PRP does accelerate wound healing for diabetic foot ulcers and venous ulcers (14). However, the clinical evidence for TJR was lacking.
In recent years, an increasing number of studies on the use of PRP in TJR have been conducted, but many clinical studies have not drawn definitive conclusions on the efficacy and safety of PRP. A previous meta-analysis (15) concluded that there was no significant difference in pain at 24 h and 48 h, which is contradictory to a recent study (16). Ma J et al (17) performed a meta-analysis including six randomized controlled trials (RCTs), demonstrating that PRP reduced blood loss after total knee arthroplasty (TKA). However, data from subsequent studies on this topic revealed that there was no statistical difference between the PRP group and the control group (18–20). RCTs published in recent years may alter previous conclusions on the effect of PRP. Hence, this systematic review and meta-analysis related to the use of topical PRP for TJR was performed to explore the potential clinical values of PRP.
This systematic review was conducted by following Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (21). Because it was a review of the existing literature, and there was no registered protocol, ethical approval was not necessary.
Relevant randomized controlled trials (RCTs) were identified from databases Medline, the Cochrane library, and Embase. The search strategy for Medline was as follows: ((“Platelet-rich plasma” or “PRP”) and (“Arthroplasty, Replacement, Hip” or “THA” or “THA” or “Total Joint Arthroplasty” or “Arthroplasty, Replacement, Knee” or “TKA”)). The last search date was February 2, 2022. We manually searched for eligible references by reading the title and abstract. In addition, we manually screened previous reviews and reference lists of relevant studies to broaden the search.
After downloading all citations, RCTs were reviewed by two independent investigators (HS, ZH), and any disagreements were resolved by a third investigator (BZ). All RCTs meeting the following inclusion criteria were considered: patients (age>18 years) who underwent primary TJR; and PRP intervention in the experiment group. There were no restrictions on the year of publication, and language was limited to English. The following types were excluded: letter, case report, case series, review, non-RCT, and Quasi-RCT.
The following items were extracted from eligible studies by two independent investigators (HS, ZH): name of first author, year of publication, country of origin, the number of patients in each group, the number of males in each group, mean (± standard deviation) age of patients per group, type of operation, type of prosthesis, type of PRP, preparation of PRP, and the dose of PRP. A standardized Microsoft Excel file was used to record the data and a third investigator (BZ) verified the collected data.
Based on Cochrane Collaboration's tool, risk of bias 2.0 (RoB 2.0) (22) was assessed by two independent investigators (HS, ZH), and any disputes were resolved by another investigator (BZ). The overall level of evidence for each endpoint was evaluated by Grading of Recommendations dations Assessment, Development, and Evaluation (GRADE) (23).
The outcomes of interest were pain, range of motion (ROM), Western Ontario and McMaster Osteoarthritis Index (WOMAC) score, length of hospital stay (LOS), hemoglobin (Hb) drop, total blood loss, wound healing rate, and wound infection. Visual analogue scale (VAS) was used to measure pain, which consisted of a scale of 1 to 10. All calculations were performed using STATA 17.0 software (StataCorp, College Station, TX). For continuous outcomes, mean difference (MD) was calculated, and the risk ratio (RR) was calculated for dichotomous outcomes. Heterogeneity was calculated using the I2 statistical and Chi-square test, indicating high heterogeneity when I2 was greater than 50%. In this case, a random-effects model was used; otherwise, we conducted the fixed-effects model. The p-value of less than 0.05 was defined as a significant difference. Summary effect measures were presented along with their corresponding 95% confidence intervals (CIs). Sensitivity analyses were conducted by omitting one study at a time, and subgroup analyses were performed to explore the source of bias according to the type of TJR. Egger’s test and Begg’s test were performed to assess publication bias (24, 25).
The literature search resulted in 456 hits, of which 101 were duplicates and were excluded. After screening based on titles and abstracts, the full text of 21 relevant studies was eligible. Three case reports, four non-English, three reviews, and one letter were excluded. Subsequently, a total of 10 origin RCTs (16, 18, 26–33) were included in the current systematic review (Figure 1).
The studies are summarized in Table 1. A total of 772 patients who underwent TKA or total hip arthroplasty (THA) were included, of which 332 were in the PRP group. Eight studies reported the effect of PRP on TKA, one study reported that on THA, and one study reported that on TKA and THA. The studies were published between 2009 and 2021. The risk of bias is presented in Figure 2. One study (31) was defined as high bias and two studies (18, 27) were defined as low bias.
A total of 3 studies (16, 18, 30) accessed pain following total knee arthroplasty by using VAS, which included 161 cases. As shown in Figure 3, the PRP group had a similar VAS score to the control group at postoperative day (POD) 1 (MD = −0.47, 95%CI: −1.31 to 0.38), POD 2 (MD = −0.63, 95%CI: −1.38 to 0.13), but 3-week (MD = −0.92, 95%CI: −1.25 to −0.60) and 2-month (MD = −0.93, 95%CI: −1.24 to −0.63) scores were significantly lower than those of the control group.
Five studies (18, 26, 28, 30, 31) reported ROM following total knee arthroplasty in a total of 529 cases. Between the PRP group and the control group, the ROM was similar at POD 2 (MD = 1.90, 95%CI: −1.08 to 4.87), POD 5 (MD = 3.16, 95%CI: −0.73 to 7.06), 1-week (MD = −1.06, 95%CI: −4.62 to 1.42), 2-week (MD = −0.88, 95%CI: −3.70 to 1.94), and 6-week (MD = 3.88, 95%CI: −5.23 to 12.98) (Figure 4)
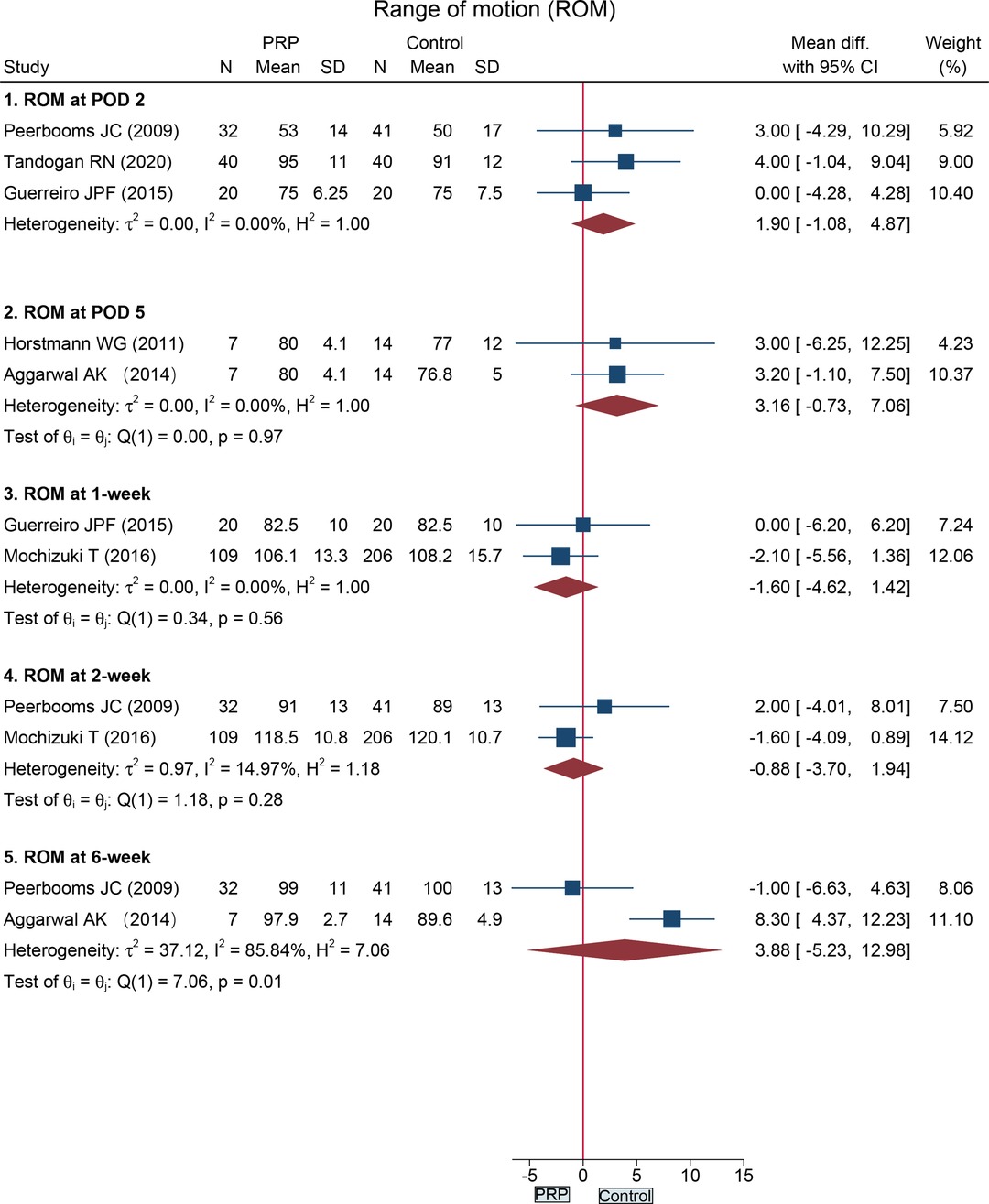
Figure 4. Forest plot presents the pooled results for the range of motion in the total knee arthroplasty subgroup.
The data on WOMAC score at 6-week, 2-month, 3-month, and 6-months following total knee arthroplasty were recorded in four RCTs (16, 26, 28, 30). The WOMAC score did not significantly differ between the two groups at 6-week (MD = −2.37, 95%CI: −9.78 to 5.04), 2-month (MD = 2.90, 95%CI: −3.97 to 9.76), 3-month (MD = −0.71, 95%CI: −8.51 to 7.08), and 6-month (MD = −0.69, 95%CI: −1.65 to 0.28) (Figure 5).
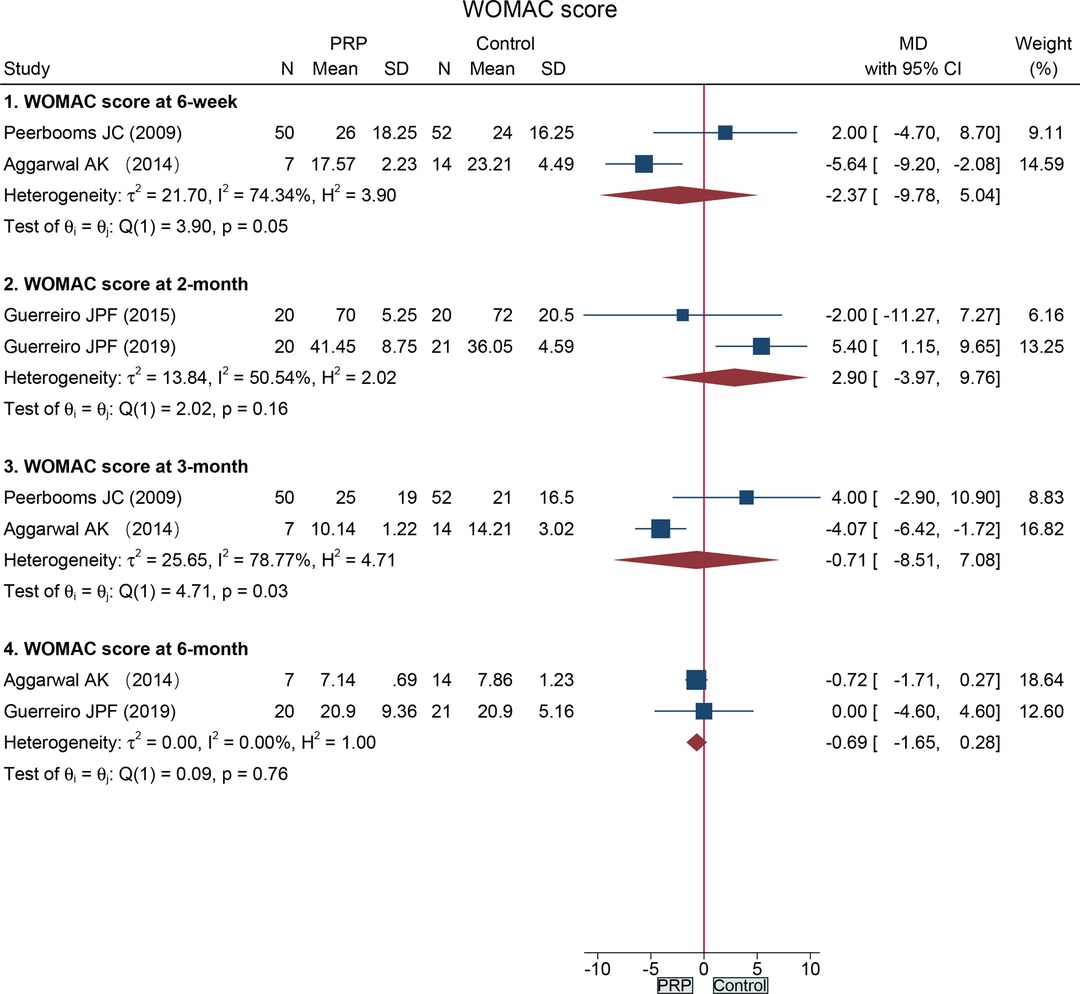
Figure 5. Forest plot presents the pooled results for WOMAC score in the total knee arthroplasty subgroup.
Three RCTs (18, 27, 28) reported the length of hospital stay following total knee arthroplasty, and one RCT (33) provided data on total hip arthroplasty. Compared with the control group, no significant difference was found in the THA subgroup (MD = 0.00, 95%CI: −0.86 to 0.86) and TKA subgroup (MD = −1.27, 95%CI: −2.90 to 0.35) (Figure 6A).
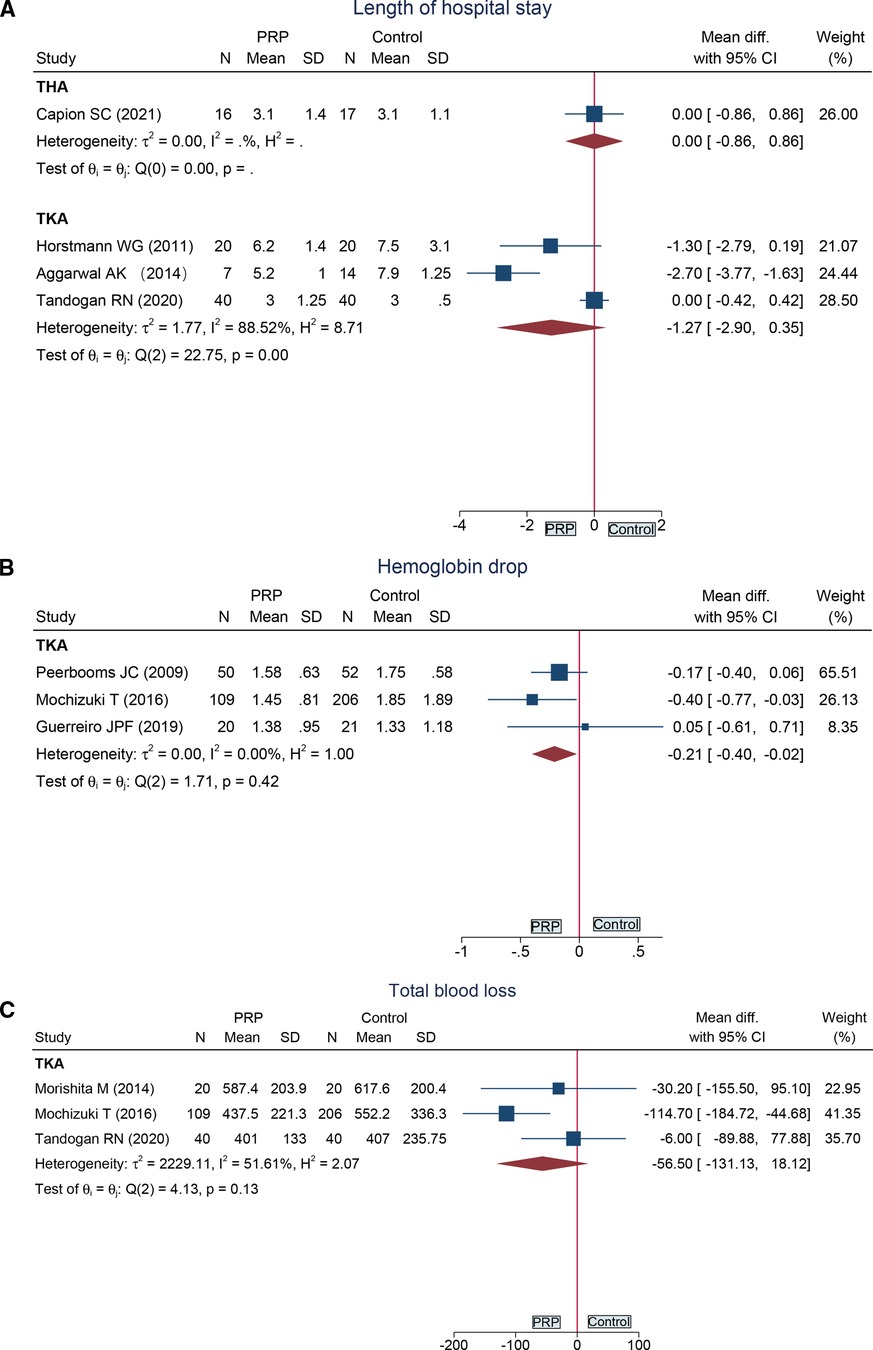
Figure 6. Forest plot presents the pooled results for: (A) length of hospital stay; (B) hemoglobin drop; (C) total blood loss.
Hemoglobin drop following total knee arthroplasty at POD 1 was reported in three RCTs (16, 26, 31) in 458 cases. Compared with the control group, hemoglobin drop was lower in the PRP group (MD = −0.21, 95%CI: −0.40 to −0.02) (Figure 6B).
Data from three RCTs (18, 29, 31) demonstrated that total blood loss in the PRP group was similar to that of the control group following total knee arthroplasty (MD = −56.50, 95%CI: −131.13 to 18.12) (Figure 6C).
One study (29) provided total knee arthroplasty data and one (33) provided total hip arthroplasty data on wound healing rates within 4 weeks. There was no significant difference in the TKA subgroup (MD = 1.12, 95%CI: 0.91 to 1.38), while there was a significant difference in the THA subgroup (MD = 2.13, 95%CI: 1.05 to 4.29) (Figure 7A).
Four original studies reported the data of TKA, one study (33) reported the data of THA, and one study (32) reported the data of TKA and THA. However, there was no significant difference in all subgroups (Figure 7B).
Table 2 shows the quality of evidence for each outcome. The certainty of pain at 2 months, ROM at POD 5, and WOMAC score at 6 months was high. The level of evidence for ROM at 2 weeks, ROM at 6 weeks, WOMAC score at 6 weeks, and hemoglobin drop was low. The rest of the outcomes were regarded as moderate-level evidence.
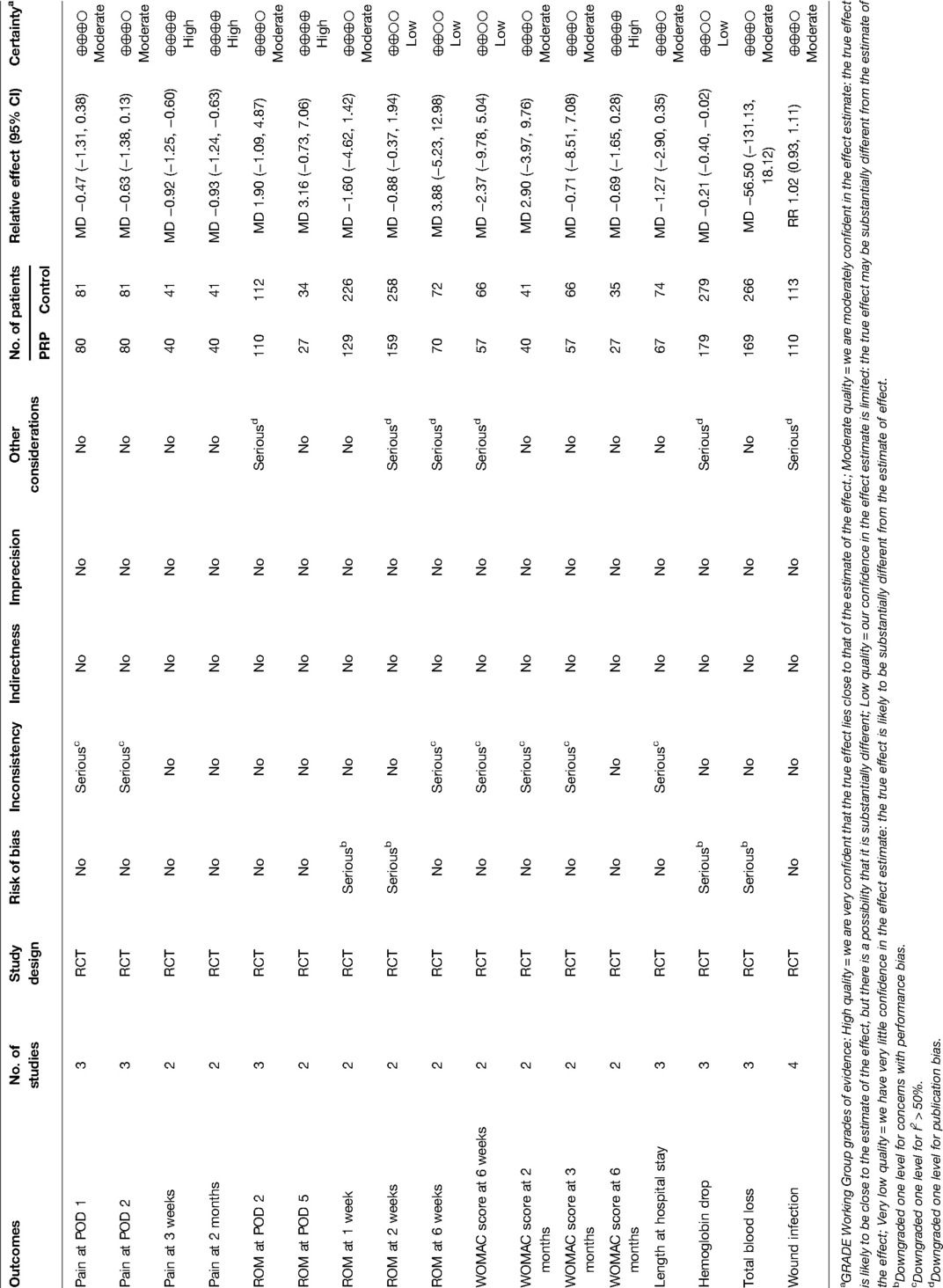
Table 2. GRADE assessment for outcomes reported in randomized controlled trials (RCTs) on PRP vs control for total knee arthroplasty.
Due to the limitations in the number of origin studies, Egger’s test and Begg’s test could not be conducted to assess publication bias. After sensitivity analysis, the results of the current study did not change and were considered stable.
The current systematic review provided the latest evidence involving 772 cases on PRP for TJR. In the TKA subgroup, the available data demonstrated that there was a significant difference in the outcomes of pain and Hb drop, while there was no significant difference in the outcomes for ROM, WOMAC score, LOS, total blood loss, wound healing rate, and wound infection. Moreover, the pooled results found that the PRP group and the control group had similar outcomes of LOS and wound infection in the THA subgroup. Interestingly, data from the included studies revealed that the application of PRP had a positive effect on wound healing rates.
Previous systematic review and meta-analysis including both RCTs and non-RCTs held different points with the current study (15). In this study, Li FX et al included 11 origin studies (7 RCTs, and 4 non-RCTs) to investigate the effect of PRP for TKA, and the pooled results demonstrated that ROM at 3 days and 3 months were significantly higher than in the control group, whereas statistical difference was found in our study. It is noteworthy that non-RCTs included by Li FX et al contributed to bias, which may explain a different point of view from the current study. In another meta-analysis conducted by Ma J et al, which contained 6 RCTs and enrolled 529 patients, it was demonstrated that the application of PRP did decrease the length of hospital stay after TKA (17). However, recently, Capion SC et al (33) found no significant difference in terms of length of hospital stay following TKA between two groups (P = .223). Combining the data from Capion SC et al, we found that there was no significant difference in terms of length of hospital stay in the TKA subgroup. For the outcome of hemoglobin drop, a significant difference was found in the study of Ma J et al (17), while Guerreiro JPF et al (16) found no distinction. After pooling the data of Guerreiro JPF et al, the synthesized result of the current meta-analysis remained significant.
Many technologies and drugs have emerged to reduce blood loss during and after total joint replacement (34). It was reported that platelet-rich plasma contributes to reducing blood loss for TJR (17, 28, 31, 35). However, Tingstad EM et al (19) analyzed the data from 93 patients who underwent TKA and discovered that PRP injections did not reduce blood loss (P = .686). In a systematic review, Muchedzi TA et al (20) included ten studies to assess average blood loss for patients during TKA, and they also did not find statistical differences between the PRP group and the control group (P = .07). Tranexamic acid (TA) administration during TKA had been demonstrated to reduce blood loss (36). Tandogan RN et al (18) evaluated the effect of platelet-rich fibrin (PRF) on blood loss by comparing the combined utilization of PRF and TA with TA alone, and the data showed no significant difference between two groups (P = .722). In this meta-analysis, we synthesized the latest evidence and revealed that PRP did not reduce total blood loss in patients following TKA.
Platelet-rich plasma has a strong effect on wound repair (37, 38). A meta-analysis of 15 RCTs by Xia Y et al (14) concluded that additional application of PRP enhanced chronic wound closure. Analogously, the current study provided evidence that PRP accelerates wound healing in total hip arthroplasty. However, there was no significant difference in the total knee arthroplasty subgroup. The reason for the different results may be the differences in cavity between the knee and the hip. A systematic review conducted by Muchedzi TA et al's also found no benefit of PRP application on wound score after TKA (P = .33) (20). To the best of our knowledge, this is the first meta-analysis to demonstrate a positive effect of PRP on improving wound rates for patients following THA. Additionally, increased skin healing may be associated with a reduced economic burden. A cost-effectiveness analysis (CEA) conducted by Russo S et al (39) implied that additional PRP was a cost-effective or even a cost-saving alternative treatment for diabetic foot ulcers (incremental cost-effectiveness ratio [ICER] −€613/ QALY). For knee osteoarthritis, however, Rajan PV et al (40) conducted a Markov decision analysis and demonstrated that PRP injections were not cost-effective due to the lack of clinical evidence for pain relief, improved function, and delayed TKA. Here, our study provided the latest data on pain relief for TKA, although the pooled results of postoperative function were not statistically different. Furthermore, the events of wound infection were pooled in the current study, but no difference was found, demonstrating that intraoperative PRP was safe.
Several limitations should be noted. First, only 10 RCTs were extracted in the current meta-analysis. More high-quality RCTs, in the future, are needed to investigate these results. Second, the high heterogeneity should not be ignored. Third, publication bias is a concern, because non-English studies were excluded. Fourth, there is a lack of available data on THA, and only one eligible study was included in this meta-analysis. Therefore, future work should focus on the effect of PRP on THA.
The application of platelet-rich plasma to patients following total keen arthroplasty is associated with pain relief and decreased Hb drop. In addition, available data reveal that platelet-rich plasma accelerates wound healing rates in patients undergoing total hip arthroplasty. Intra-operative PRP is active; however, more prospective and multicenter studies are warranted to confirm these results.
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found in the article/Supplementary Material.
HS and ZH designed the study; XB, ZX, and NW performed the data collection; HS, XF, and XC did the data analysis; HS and BZ wrote the article. All authors contributed to the article and approved the submitted version.
This work was supported by the Science and Technology Plan of Jiangxi Provincial Health and Family Planning Commission (No. 20195226).
There is no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Sax OC, Chen Z, Bains SS, Salib CG, Pervaiz SS, Mont MA, et al. Timing and type of bariatric surgery preceding total knee arthroplasty leads to similar complications and outcomes. J Arthroplasty. (2022) 2022:S0883-5403(22)00093-6. doi: 10.1016/j.arth.2022.01.076
2. Werner A, Jäger M, Schmitz H, Krauspe R. Joint preserving surgery for osteonecrosis and osteochondral defects after chemotherapy in childhood. Klin Padiatr. (2003) 215(6):332–7. doi: 10.1055/s-2003-45495
3. Sun XL, Zhao ZH, Ma JX, Li FB, Li YJ, Meng XM, et al. Continuous local infiltration analgesia for pain control after total knee arthroplasty: a meta-analysis of randomized controlled trials. Medicine (Baltimore). (2015) 94(45):e2005. doi: 10.1097/MD.0000000000002005
4. Tay HP, Wang X, Narayan SW, Penm J, Patanwala AE. Persistent postoperative opioid use after total hip or knee arthroplasty: a systematic review and meta-analysis. Am J Health Syst Pharm. (2022) 79(3):147–64. doi: 10.1093/ajhp/zxab367
5. Xiao PL, Hsu CJ, Ma YG, Liu D, Peng R, Xu XH, et al. Prevalence and treatment rate of osteoporosis in patients undergoing total knee and hip arthroplasty: a systematic review and meta-analysis. Arch Osteoporos. (2022) 17(1):16. doi: 10.1007/s11657-021-01055-9
6. Januel JM, Chen G, Ruffieux C, Quan H, Douketis JD, Crowther MA, et al. Symptomatic in-hospital deep vein thrombosis and pulmonary embolism following hip and knee arthroplasty among patients receiving recommended prophylaxis: a systematic review. Jama. (2012) 307(3):294–303. doi: 10.1001/jama.2011.2029
7. Moghtadaei M, Farahini H, Faiz SH, Mokarami F, Safari S. Pain management for total knee arthroplasty: single-injection femoral nerve block versus local infiltration analgesia. Iran Red Crescent Med J. (2014) 16(1):e13247. doi: 10.5812/ircmj.13247
8. Lee DH, Padhy D, Lee SH, Kim TK, Choi J, Han SB. Shed blood re-transfusion provides no benefit in computer-assisted primary total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. (2011) 19(6):926–31. doi: 10.1007/s00167-010-1228-8
9. Tang JZ, Nie MJ, Zhao JZ, Zhang GC, Zhang Q, Wang B. Platelet-rich plasma versus hyaluronic acid in the treatment of knee osteoarthritis: a meta-analysis. J Orthop Surg Res. (2020) 15(1):403. doi: 10.1186/s13018-020-01919-9
10. Nguyen RT, Borg-Stein J, McInnis K. Applications of platelet-rich plasma in musculoskeletal and sports medicine: an evidence-based approach. Pm r. (2011) 3(3):226–50. doi: 10.1016/j.pmrj.2010.11.007
11. Zhu Y, Yuan M, Meng HY, Wang AY, Guo QY, Wang Y, et al. Basic science and clinical application of platelet-rich plasma for cartilage defects and osteoarthritis: a review. Osteoarthritis Cartilage. (2013) 21(11):1627–37. doi: 10.1016/j.joca.2013.07.017
12. Houdek MT, Wyles CC, Stalboerger PG, Terzic A, Behfar A, Moran SL. Collagen and fractionated platelet-rich plasma scaffold for dermal regeneration. Plast Reconstr Surg. (2016) 137(5):1498–506. doi: 10.1097/PRS.0000000000002094
13. Romano F, Paolino FM, Rizzo BA, Russo A, Southworth S, Serra R, et al. The use of growth factors, CD34(+) cells and fibrin for the management of chronic venous ulcers. Int Wound J. (2016) 13(5):1011–3. doi: 10.1111/iwj.12500
14. Xia Y, Zhao J, Xie J, Lv Y, Cao DS. The efficacy of platelet-rich plasma dressing for chronic nonhealing ulcers: a meta-analysis of 15 randomized controlled trials. Plast Reconstr Surg. (2019) 144(6):1463–74. doi: 10.1097/PRS.0000000000006281
15. Li FX, Li Y, Qiao CW, Zhu J, Chen J, Zhang PY. Topical use of platelet-rich plasma can improve the clinical outcomes after total knee arthroplasty: a systematic review and meta-analysis of 1316 patients. Int J Surg. (2017) 38:109–16. doi: 10.1016/j.ijsu.2016.12.013
16. Guerreiro JPF, Lima DR, Bordignon G, Danieli MV, Queiroz AO, Cataneo DC. Platelet-rich plasma (prp) and tranexamic acid (txa) applied in total knee arthroplasty. Acta Ortop Bras. (2019) 27(5):248–51. doi: 10.1590/1413-785220192705214417
17. Ma J, Sun J, Guo W, Li Z, Wang B, Wang W. The effect of platelet-rich plasma on reducing blood loss after total knee arthroplasty: a systematic review and meta-analysis. Medicine (Baltimore). (2017) 96(26):e7262. doi: 10.1097/MD.0000000000007262
18. Tandogan RN, Polat M, Beyzadeoglu T, Karabulut E, Yildirim K, Kayaalp A. Topical co-delivery of platelet rich fibrin and tranexamic acid does not decrease blood loss in primary total knee arthroplasty compared to the standard of care: a prospective, randomized, controlled trial. Knee Surg Sports Traumatol Arthrosc. (2021) 29(2):519–28. doi: 10.1007/s00167-020-05938-1
19. Tingstad EM, Bratt SN, Hildenbrand KJ, O'Malley BA, Mitchell ER, Gaddis CE, et al. Platelet-rich plasma does not decrease blood loss in total knee arthroplasty. Orthopedics. (2015) 38(5):e434–6. doi: 10.3928/01477447-20150504-63
20. Muchedzi TA, Roberts SB. A systematic review of the effects of platelet rich plasma on outcomes for patients with knee osteoarthritis and following total knee arthroplasty. Surgeon. (2018) 16(4):250–8. doi: 10.1016/j.surge.2017.08.004
21. Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 Explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. Br Med J. (2021) 372:n160. doi: 10.1136/bmj.n160
22. Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. Rob 2: a revised tool for assessing risk of bias in randomised trials. Br Med J. (2019) 366:l4898. doi: 10.1136/bmj.l4898
23. Guyatt GH, Oxman AD, Schünemann HJ, Tugwell P, Knottnerus A. GRADE guidelines: a new series of articles in the journal of clinical epidemiology. J Clin Epidemiol. (2011) 64(4):380–2. doi: 10.1016/j.jclinepi.2010.09.011
24. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315(7109):629–34. doi: 10.1136/bmj.315.7109.629
25. Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. (1994) 50(4):1088–101. doi: 10.2307/2533446
26. Peerbooms JC, de Wolf GS, Colaris JW, Bruijn DJ, Verhaar JA. No positive effect of autologous platelet gel after total knee arthroplasty. Acta Orthop. (2009) 80(5):557–62. doi: 10.3109/17453670903350081
27. Horstmann WG, Slappendel R, van Hellemondt GG, Wymenga AW, Jack N, Everts PA. Autologous platelet gel in total knee arthroplasty: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc. (2011) 19(1):115–21. doi: 10.1007/s00167-010-1207-0
28. Aggarwal AK, Shashikanth VS, Marwaha N. Platelet-rich plasma prevents blood loss and pain and enhances early functional outcome after total knee arthroplasty: a prospective randomised controlled study. Int Orthop. (2014) 38(2):387–95. doi: 10.1007/s00264-013-2136-6
29. Morishita M, Ishida K, Matsumoto T, Kuroda R, Kurosaka M, Tsumura N. Intraoperative platelet-rich plasma does not improve outcomes of total knee arthroplasty. J Arthroplasty. (2014) 29(12):2337–41. doi: 10.1016/j.arth.2014.04.007
30. Guerreiro JP, Danieli MV, Queiroz AO, Deffune E, Ferreira RR. Platelet-rich plasma (PRP) applied during total knee arthroplasty. Rev Bras Ortop. (2015) 50(2):186–94. doi: 10.1016/j.rbo.2014.05.005
31. Mochizuki T, Yano K, Ikari K, Hiroshima R, Kawakami K, Koenuma N, et al. Platelet-rich plasma for the reduction of blood loss after total knee arthroplasty: a clinical trial. Eur J Orthop Surg Traumatol. (2016) 26(8):901–5. doi: 10.1007/s00590-016-1821-8
32. Evans DC, Evans BG. The effects of platelet-rich plasma and activated collagen on wound healing in primary total joint arthroplasty. Orthopedics. (2018) 41(2):e262–e7. doi: 10.3928/01477447-20180213-05
33. Capion SC, Jørgensen HBL, Ågren MS, Daugaard H, Ribel-Madsen S, Marando D, et al. The wound healing effect of local leukocyte platelet-rich plasma after total hip arthroplasty: a randomized controlled trial. Wound Repair Regen. (2021) 29(6):988–95. doi: 10.1111/wrr.12967
34. Lu Q, Peng H, Zhou GJ, Yin D. Perioperative blood management strategies for total knee arthroplasty. Orthop Surg. (2018) 10(1):8–16. doi: 10.1111/os.12361
35. Gardner MJ, Demetrakopoulos D, Klepchick PR, Mooar PA. The efficacy of autologous platelet gel in pain control and blood loss in total knee arthroplasty. an analysis of the haemoglobin, narcotic requirement and range of motion. Int Orthop. (2007) 31(3):309–13. doi: 10.1007/s00264-006-0174-z
36. Wang F, Zhao KC, Zhao MM, Zhao DX. The efficacy of oral versus intravenous tranexamic acid in reducing blood loss after primary total knee and hip arthroplasty: a meta-analysis. Medicine (Baltimore). (2018) 97(36):e12270. doi: 10.1097/MD.0000000000012270
37. Sclafani AP, Azzi J. Platelet preparations for use in facial rejuvenation and wound healing: a critical review of current literature. Aesthetic Plast Surg. (2015) 39(4):495–505. doi: 10.1007/s00266-015-0504-x
38. Jee CH, Eom NY, Jang HM, Jung HW, Choi ES, Won JH, et al. Effect of autologous platelet-rich plasma application on cutaneous wound healing in dogs. J Vet Sci. (2016) 17(1):79–87. doi: 10.4142/jvs.2016.17.1.79
39. Russo S, Landi S, Courric S. Cost-Effectiveness analysis for the treatment of diabetic foot ulcer in France: platelet-rich plasma vs standard of care. Clinicoecon Outcomes Res. (2022) 14:1–10. doi: 10.2147/CEOR.S327191
Keywords: meta-analysis, randomized controlled trial, total joint replacement, total knee arthroplasty, total hip arthroplasty, platelet-rich plasma
Citation: Shu H, Huang Z, Bai X, Xia Z, Wang N, Fu X, Cheng X and Zhou B (2022) The Application of Platelet-Rich Plasma for Patients Following Total Joint Replacement: A Meta-Analysis of Randomized Controlled Trials and Systematic Review. Front. Surg. 9:922637. doi: 10.3389/fsurg.2022.922637
Received: 18 April 2022; Accepted: 13 June 2022;
Published: 4 July 2022.
Edited by:
Paphon Sa-ngasoongsong, Ramathibodi Hospital, Mahidol University, ThailandReviewed by:
Tulyapruek Tawonsawatruk, Mahidol University, ThailandCopyright © 2022 Shu, Huang, Bai, Xia, Wang, Fu, Cheng and Zhou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Zhou emhvdWJpbm5kZWZ5QDE2My5jb20=
Specialty section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.