- Outpatient Operating Room, Wenzhou Hospital of Integrated Traditional Chinese and Western Medicine, Wenzhou, China
Objective: The current study aimed to assess the efficacy and safety of percutaneous nephrolithotomy (PCNL) in obese and overweight individuals based on body mass index (BMI).
Methods: We electronically explored the databases of PubMed, CENTRAL, ScienceDirect, Embase, and Google Scholar databases for all types of comparative studies investigating the role of BMI on PCNL outcomes. Only studies defining obesity as >30 kg/m2 were included. Efficacy outcomes were stone-free rates and operating time while safety outcomes were complications and length of hospital stay (LOS).
Results: Eighteen studies with 101,363 patients were included. We noted no difference in the stone-free rates after PCNL for morbid obese vs normal BMI patients (OR: 0.78 95% CI, 0.57, 1.08 I2 = 7% p = 0.13), overweight vs normal (OR: 1.01 95% CI, 0.89, 1.15 I2 = 1% p = 0.83) and obese vs normal patients (OR: 1.00 95% CI, 0.87, 1.16 I2 = 0% p = 0.95). PCNL operative time was significantly increased in morbid obese (MD: 9.36 95% CI, 2.85, 15.88 I2 = 76% p = 0.005) and obese patients as compared with normal patients (MD: 2.15 95% CI, 1.20, 3.10 I2 = 0% p < 0.00001), but not for overweight patients. There was no difference in the odds of complications between morbid obese vs normal (OR: 1.26 95% CI, 0.93, 1.72 I2 = 0% p = 0.13), overweight vs normal (OR: 1.11 95% CI, 0.96, 1.28 I2 = 0% p = 0.15), and obese vs normal patients (OR: 1.07 95% CI, 0.91, 1.27 I2 = 0% p = 0.40). LOS was significantly reduced in obese patients (MD: −0.12 95% CI, −0.20, −0.04 I2 = 0% p = 0.004) as compared to normal patients, but not for morbid obese or overweight patients.
Conclusion: PCNL has similar efficacy and safety in morbidly obese, obese, and overweight patients as compared to normal BMI patients with no difference in the stone-free and complication rates. Evidence suggests that operating time is increased in morbidly obese and obese patients and the latter may have shorter LOS.
Systematic Review Registration: https://www.crd.york.ac.uk/prospero/, identifier: CRD42022313599.
Introduction
Renal stones are a very common urological disease that has a significant impact on the health and quality of life of affected patients (1). The prevalence of the disease varies from 0.1 to 14.8% amongst Western populations to as high as 10.6% in the Asian population (1, 2). Indeed, renal stones can lead to significant patient morbidity causing symptoms like abdominal pain, infections, hydronephrosis, and decreased renal function (1). It is well known that colicky pain due to renal stones is one of the most common presenting symptoms in the emergency department (3). Management protocols for renal stones include observation and pharmacotherapy or invasive procedures like shockwave lithotripsy, percutaneous nephrolithotomy (PCNL), ureterorenoscopy, and even laparoscopic/open renal surgeries for severe cases (4).
As with the high prevalence of renal stones, the world is also witnessing an obesity epidemic. The worldwide prevalence of obesity has exponentially increased from <1% in 1975 to 6%–8% in 2016 (5). The prevalence, however, varies significantly across countries ranging from 0.2% in Vietnamese women to as high as 65.3% in American Samoan women (6). With such growing incidence, a large number of obese patients are being seen by a urologist for managing renal stone disease. Management of such patients is challenging not only due to the change in body habitus but also due to the presence of other comorbidities like diabetes, hypertension, coronary heart disease, atrial fibrillation, and heart failure (7). Obesity restricts the application of shockwave lithotripsy due to the increased patient weight, problems with stone localization, and increased skin to stone distance (8). Delekas et al. (9) in a cohort study of 502 patients have shown that obesity is an independent predictor of failure after shockwave lithotripsy. Ureterorenoscopy is considered to be a safe and efficacious procedure for obese patients but has disadvantages of increased operating time based on the size, location, and the number of calculi (10). Its success rate also depends on the experience of the operating surgeon (11). On the other hand, PCNL is highly efficacious in treating patients with stones of >2cms in size, multiple calculi, and staghorn calculi (12). PCNL can achieve high stone-free rates as compared to shockwave lithotripsy and has significantly lower morbidity as opposed to open surgery (13). However, it is unclear if PCNL has similar efficacy and safety in obese patients as compared to normal body mass index (BMI) patients. In the past, Zhou et al. (14) in their systematic review have attempted to compare outcomes of obese and normal BMI patients undergoing PCNL. Using the WHO based definitions of normal (<25 kg/m2), overweight (25–29.9 kg/m2), obese (30–39.9 kg/m2), and morbid obese (≥40 kg/m2), the authors concluded that obesity had no impact on the outcomes of PCNL except for longer operating times in morbid obese and shorter hospital stay in obese patients. However, their review could include just seven studies. With the publication of several new studies in the recent past, there is a need for high-quality updated evidence to guide urologists on the clinical efficacy of PCNL for obese patients. We therefore conducted the current study to investigate the role of BMI on the efficacy and safety of PCNL by means of a systematic review and meta-analysis.
Material and Methods
Search Strategy
The online systematic review database of PROSPERO was used to register our meta-analysis (CRD42022313599). We carried out a systematic and comprehensive electronic database search of the PubMed, CENTRAL, ScienceDirect, Embase, and Google Scholar databases. Since Google Scholar has a large number of search records, we restricted the search to only the initial 100 results of each query. The last day of the search was 1st March 2022. Results were limited to English-language studies. The search terms used were: “percutaneous nephrolithotomy”, “nephrolithiasis”, “urolithiasis”, “renal stones”, “body mass index”, “BMI”, “obese”, “obesity”, “overweight”, and “treatment” (Supplementary Table S1). The search results were imported in a reference manager and deduplicated. The reviewers carried out an initial screening using the title and abstracts of the search results. Only relevant publications were downloaded. The two reviewers then independently cross-checked each study against the eligibility criteria for final inclusion in our review. Any disagreements were cleared by consensus. The bibliography of studies included were then hand-searched to find any other possible inclusions. We also adhered to the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-analyses) during the reporting of the review (15).
Inclusion/Exclusion
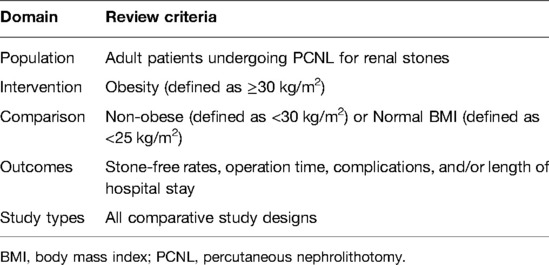
The following studies were included (Table 1): (1) All types of comparative studies conducted on adult patients undergoing PCNL for renal stones with no restriction on study design. (2) Studies comparing data of patients based on BMI. (3) Studies were to define obese patients as BMI of >30 kg/m2. (4) Studies were to report any of the following outcomes: stone-free rates, operation time, complications, and/or length of hospital stay (LOS).
Exclusion criteria were: (1) Studies reporting the combined effect of PCNL with any other surgical treatment modality (2) Not defining obese patients as BMI of ≥30 kg/m2 (3) Studies reporting duplicate data from the same database. If there was a partial overlap of data from two studies, the article with a greater sample size was to be included.
Data Management and Risk of Bias
Data extraction was carried out by two reviewers independent of each other using a standardized data collection form. Data extracted included author details, publication year, study type, study location, the database used, study groups, BMI definition, sample size, demographic details, stone size, the definition of stone-free status, patient position, sheath and nephroscope used, type of lithotripsy, diagnostic modality for stone-free status, follow-up period and outcomes. We did not define stone-free rates a priori and accepted all definitions used by the included studies. The outcomes of interest were: stone-free rates, operating times, complications, and LOS.
Two reviewers examined the quality of studies using the Newcastle-Ottawa scale (NOS) (16). Any disagreements between the reviewers were cleared by consensus. The NOS tool has the following domains: selection of study population, comparability, and outcomes. A maximum of four, two, and three points are allocated to each domain in this respective order. The highest score for a study can be nine.
Statistical Analysis
Dichotomous data were combined using odds ratios (OR) and continuous data were combined using mean difference (MD) with 95% confidence intervals (CI) in a random-effects model. We performed separate comparisons for morbid obese (BMI ≥40 kg/m2) vs normal (BMI <25 kg/m2), obese (BMI ≥30 kg/m2) vs normal, overweight (BMI 25–29.9 kg/m2) vs normal, and obese vs non-obese patients (BMI ≥30 kg/m2 vs <30 kg/m2).
Inter-study heterogeneity was examined by the I2 statistic. I2 values were classified as 25–50% = low, 50–75% = medium, and >75% = substantial heterogeneity. p values of <0.05 were considered statistically significant. We used “Review Manager” (RevMan, version 5.3; Nordic Cochrane Centre [Cochrane Collaboration], Copenhagen, Denmark; 2014) for the meta-analysis. Publication bias was examined by means of funnel plots. A leave-one-out sensitivity analysis was done by excluding one study at a time and assessing the results again. However, this was done only for analyses including more than three studies.
Results
Search Results
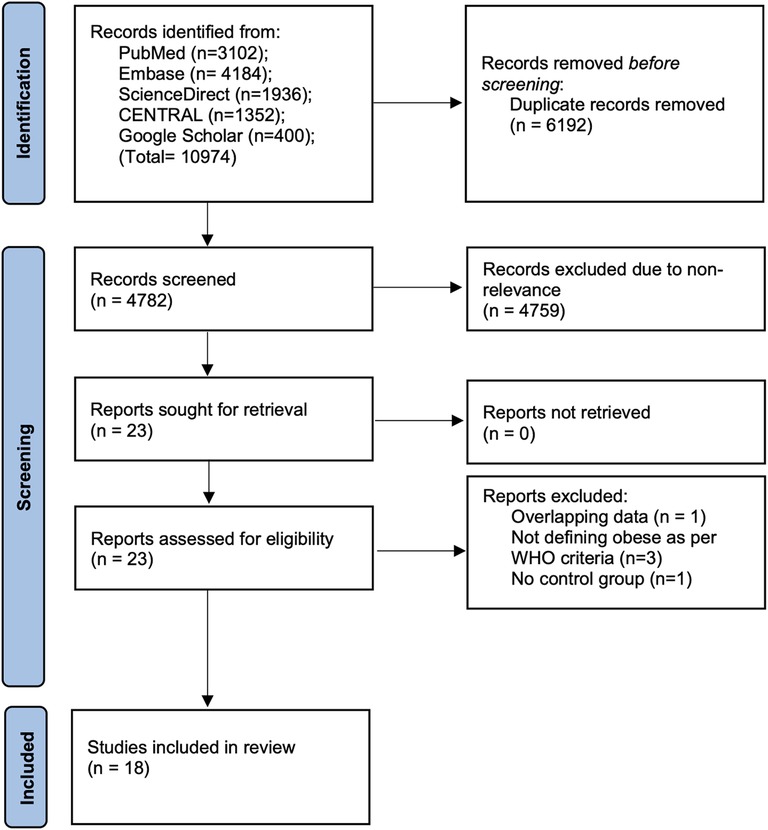
We identified a total of 4,782 unique articles (Figure 1). On initial titles and abstract screening, 4,759 articles were excluded due to non-relevance. The authors selected 23 articles for full-text analysis. Of these, 5 were excluded due to various reasons. A total of 18 studies were then included in the current review (17–34).
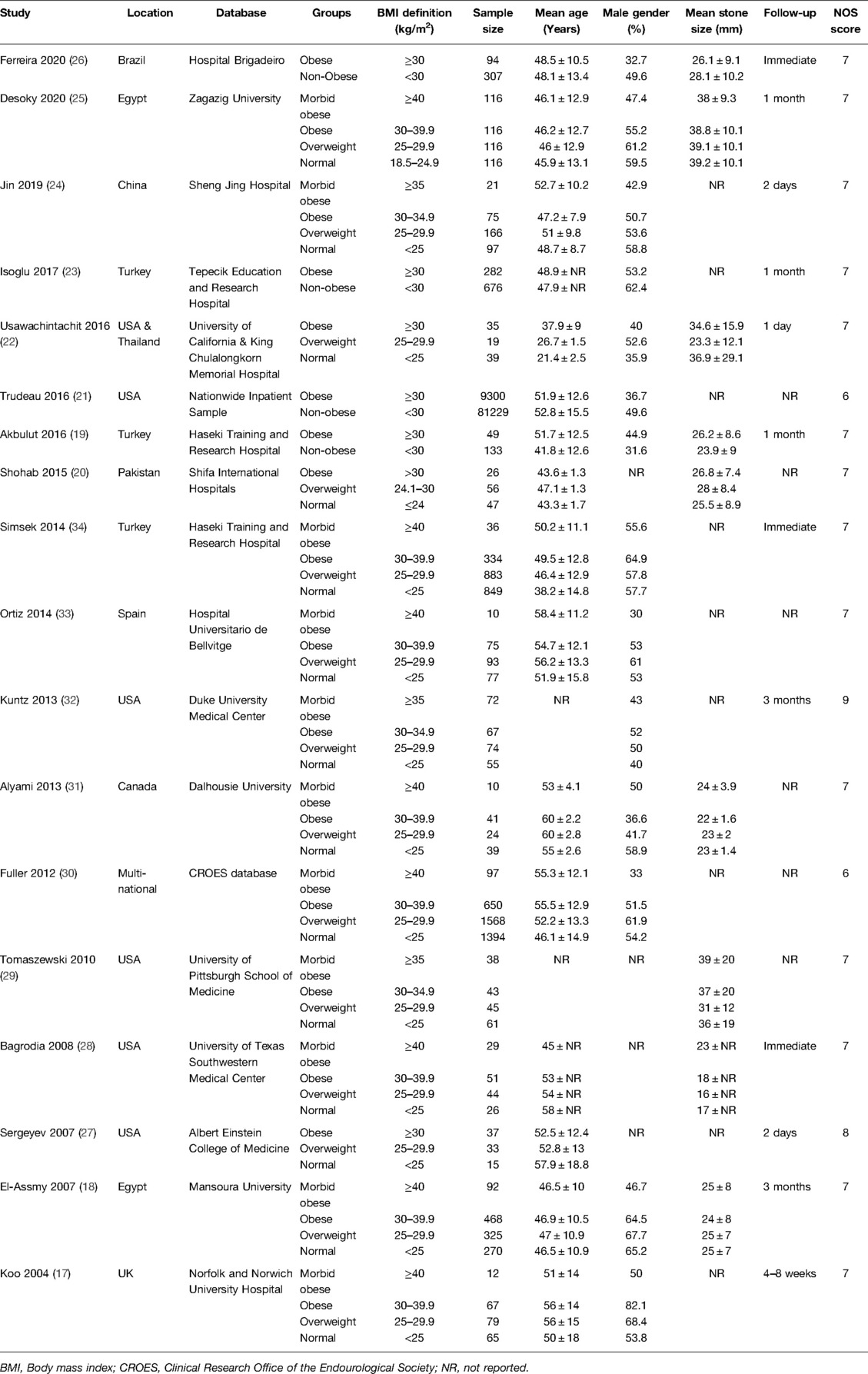
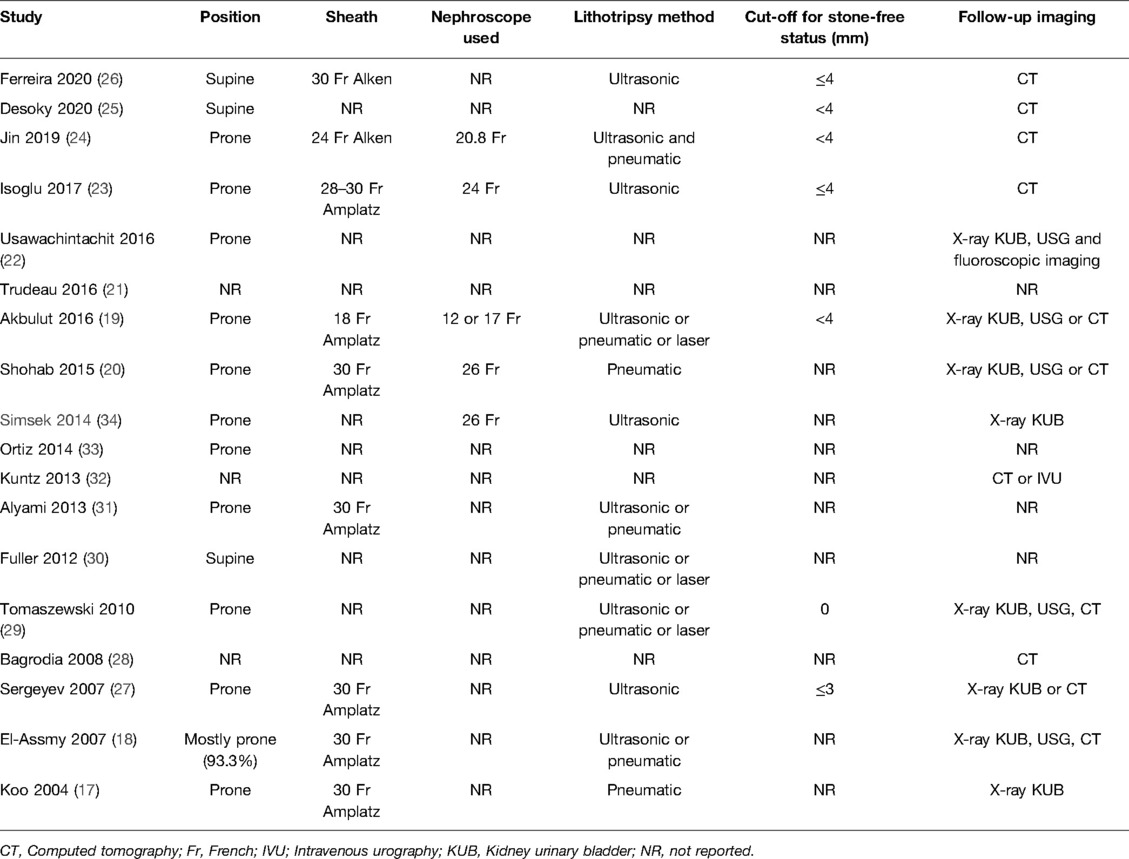
All studies were prospective or retrospective observational studies published between 2004 to 2020 (Table 2). Four studies compared data between obese and non-obese patients only. The remaining studies divided the cohort into multiple groups of morbidly obese, obese, overweight, and normal. The study of Shohab et al. (20) defined obesity based on WHO classification but used the cut-off of 24 kg/m2 to separate overweight and normal BMI patients. Since this was a minor change, the study was included in the meta-analysis. A few studies (24, 29, 32) also deviated from the WHO definition of morbidly obese and defined it as ≥35 kg/m2. However, since the definition of obese and overweight was based on WHO criteria these studies were included in the analysis but not in the subgroup analysis of morbid obese vs normal. The included studies examined a data of 101,363 patients. The NOS score ranged from 6 to 9. PCNL was performed in the prone position in most of the studies (Table 3). Only two studies reported the use of supine position. The majority of the studies did not define the cut-off for stone-free status. The definition was provided by just six studies that used <4 mm, ≤4 mm, or ≤3 mm as the cut-off for stone-free status.
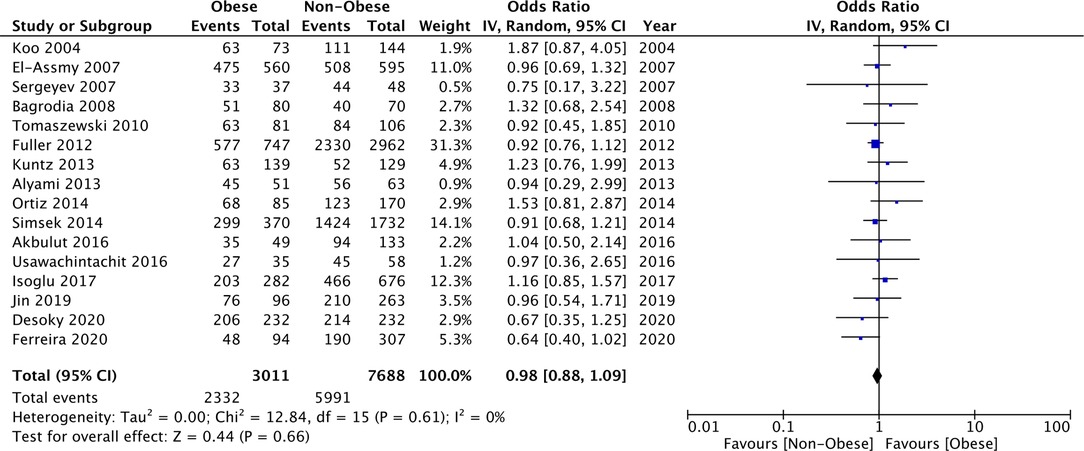
Stone-free Rates
Comparing data of morbid obese vs normal BMI patients, our meta-analysis failed to demonstrate any statistically significant difference in stone-free rates between the two groups (OR: 0.78 95% CI, 0.57, 1.08 I2 = 7% p = 0.13) (Figure 2). Similarly, we also noted no difference in the stone-free rates after PCNL for overweight vs normal (OR: 1.01 95% CI, 0.89, 1.15 I2 = 1% p = 0.83) and obese vs normal patients (OR: 1.00 95% CI, 0.87, 1.16 I2 = 0% p = 0.95) as well (Figure 2). On comparison of data of obese vs non-obese patients with the cut-off of 30 kg/m2, we noted no difference in the stone-free rates after PCNL (OR: 0.98 95% CI, 0.88, 1.09 I2 = 0% p = 0.66) (Figure 3). There was no evidence of publication bias (Supplementary Figure S1).
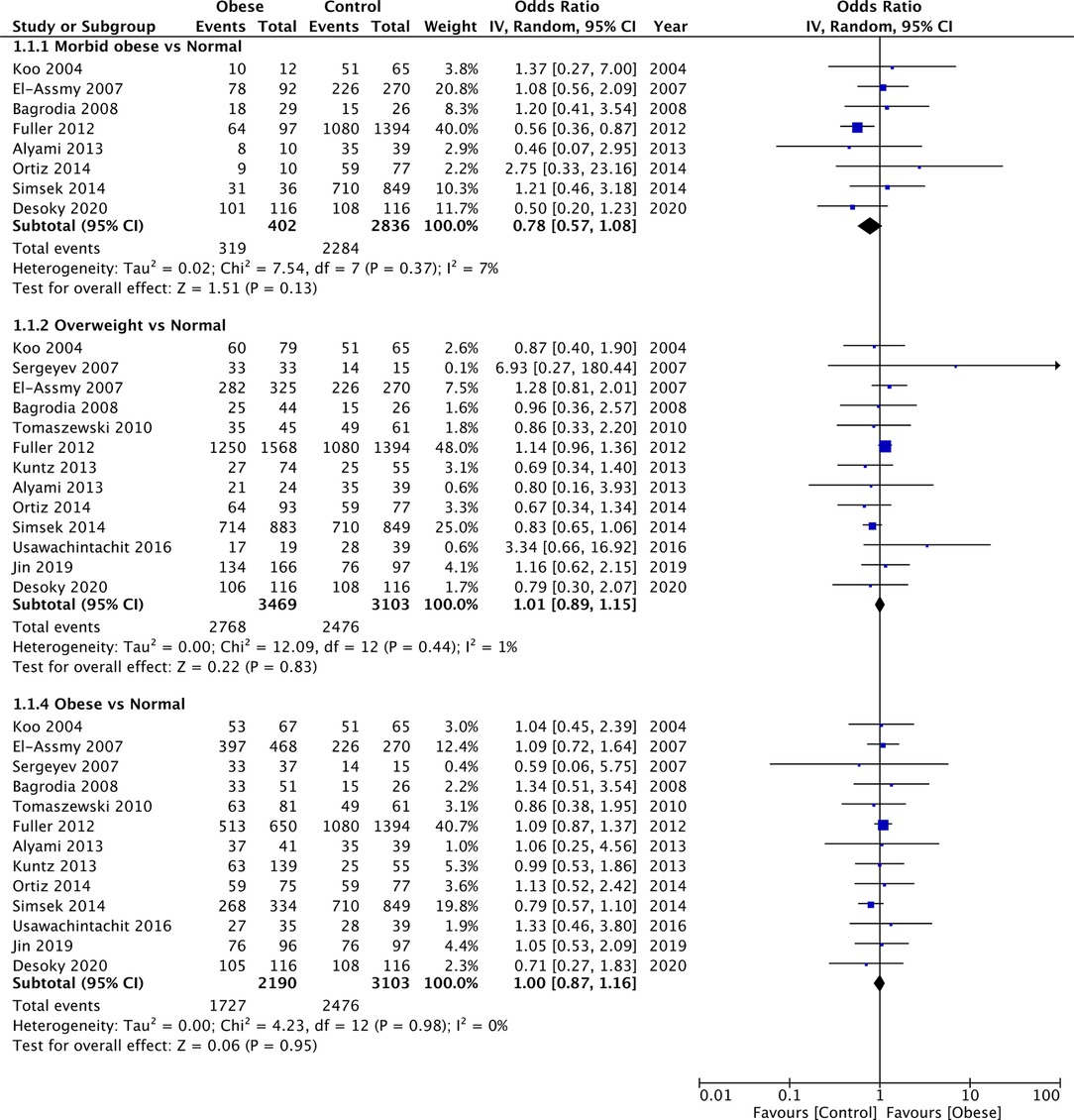
Figure 2. Meta-analysis of stone-free rates between morbid obese, overweight and obese vs normal BMI patients.
The results of all comparisons were stable on sensitivity analysis with no change in the significance, except for the comparison of morbid obese vs normal. On the exclusion of the study of El-Assmy et al. (18), the results indicated lower stone-free rates in morbid obese vs normal BMI patients (OR: 0.70 95% CI, 0.50, 0.99 I2 = 2% p = 0.04).
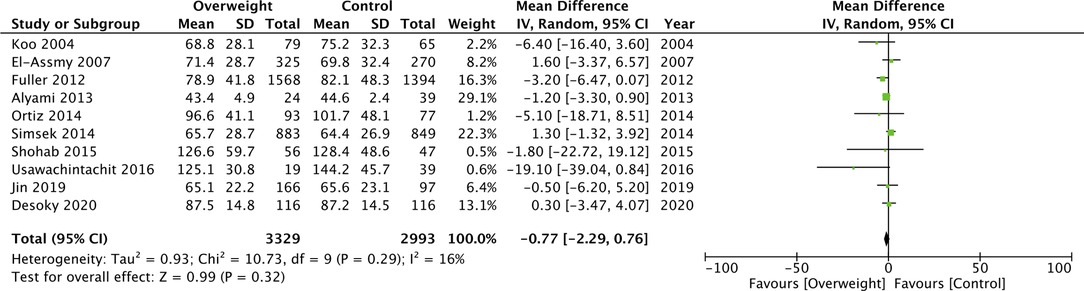
Operation Time
Our meta-analysis demonstrated that PCNL operative time was significantly increased in morbidly obese patients as compared to normal patients (MD: 9.36 95% CI, 2.85, 15.88 I2 = 76% p = 0.005) (Figure 4). A similar difference was noted when obese patients were compared with normal patients (MD: 2.15 95% CI, 1.20, 3.10 I2 = 0% p < 0.00001) (Figure 4). However, on a pooled analysis of three studies, comparing data of obese vs non-obese patients, we noted no difference in PCNL operating time between the two groups (MD: −4.46 95% CI, −10.37, 1.45 I2 = 38% p = 0.14) (Figure 4). We also noted no statistically significant difference in the operating time between overweight vs normal patients (MD: −0.77 95% CI, −2.29, 0.76 I2 = 16% p = 0.32) (Figure 5).
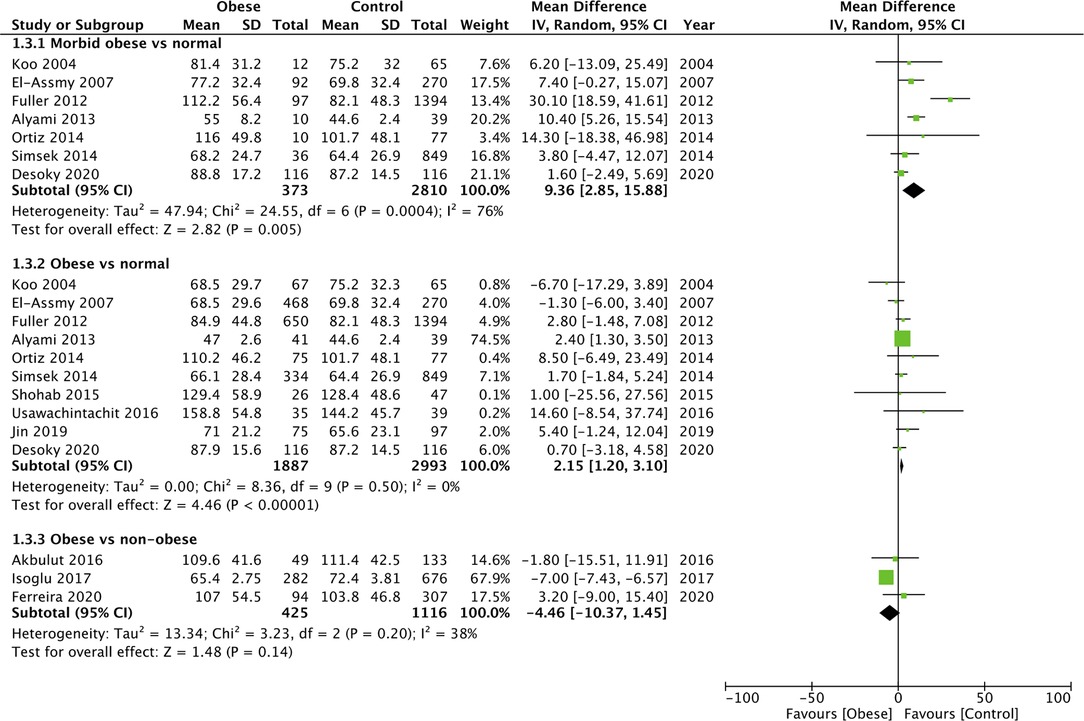
Figure 4. Meta-analysis of operation time between morbid obese vs normal, Obese vs normal, and obese vs non-obese patients.
For the comparison of obese vs normal patients, the results turned non-significant on the exclusion of the study of Alyami et al. (31) (MD: 1.42 95% CI, −0.45, 3.29 I2 = 0% p = 0.14). However, the results of the analysis of morbid obese vs normal patients and overweight vs normal patients were stable on sensitivity analysis.
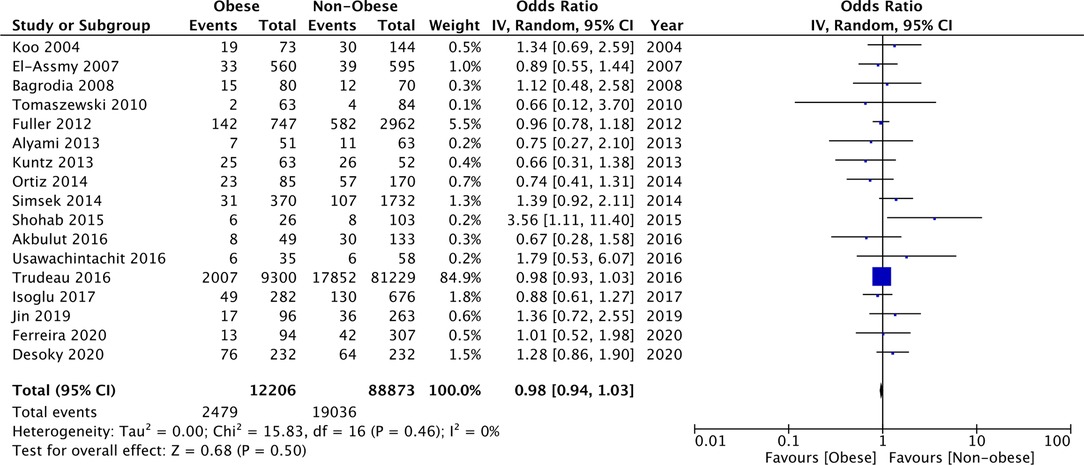
Complications
Since several different complications were described in the studies, separate analyses for the same could not be conducted. Our meta-analysis indicated no difference in the odds of complications between morbid obese vs normal (OR: 1.26 95% CI, 0.93, 1.72 I2 = 0% p = 0.13), overweight vs normal (OR: 1.11 95% CI, 0.96, 1.28 I2 = 0% p = 0.15), and obese vs normal patients (OR: 1.07 95% CI, 0.91, 1.27 I2 = 0% p = 0.40) (Figure 6). Similarly, on comparing data of obese vs non-obese patients, we noted no difference in complication rates between the two groups (OR: 0.98 95% CI, 0.94, 1.03 I2 = 0% p = 0.50) (Figure 7). We noted no evidence of publication bias on the funnel plot (Supplementary Figure S2). There was no change in the significance of the results on sensitivity analyses.
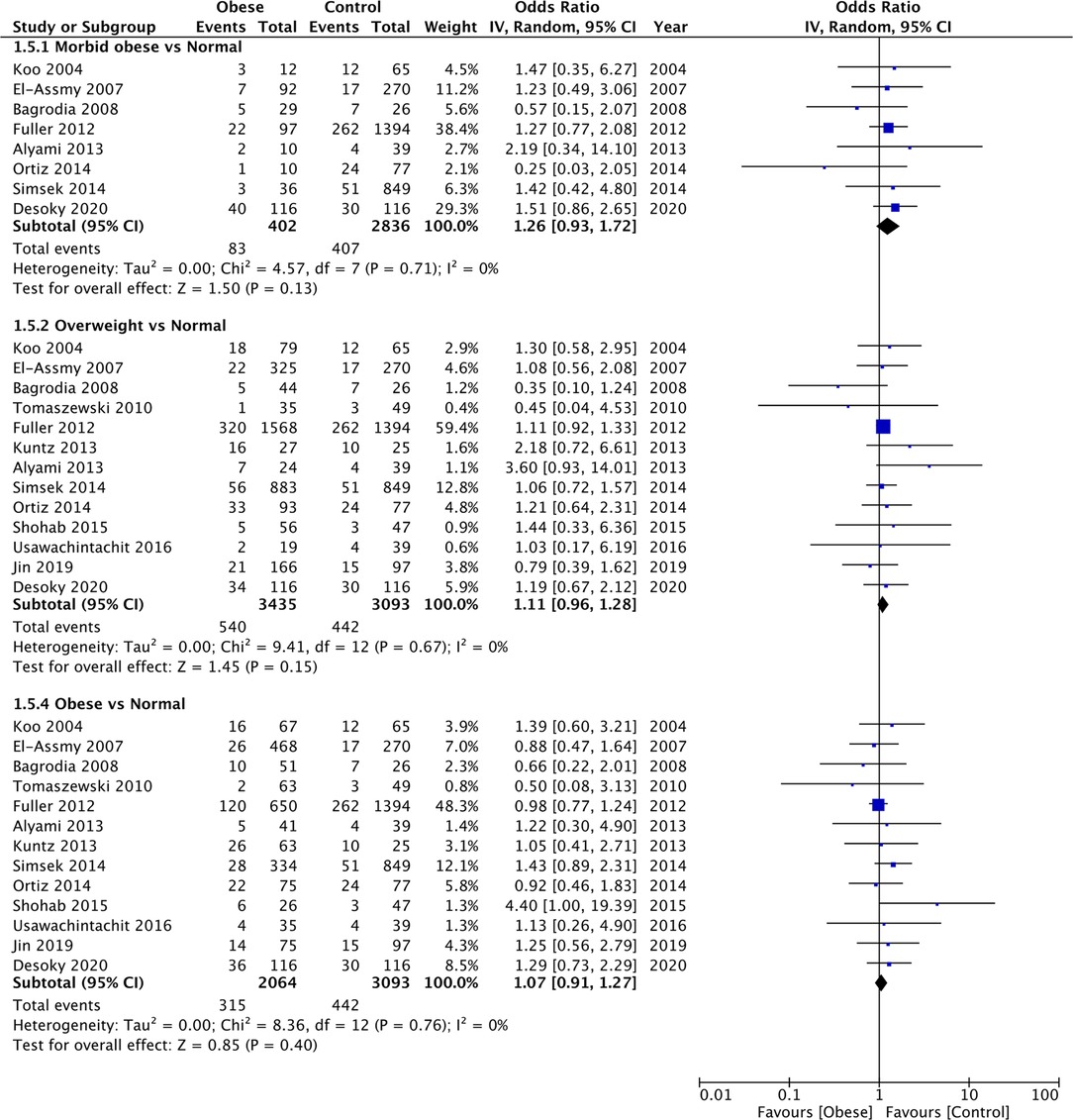
Figure 6. Meta-analysis of complication rates between morbid obese, overweight and obese vs normal BMI patients.
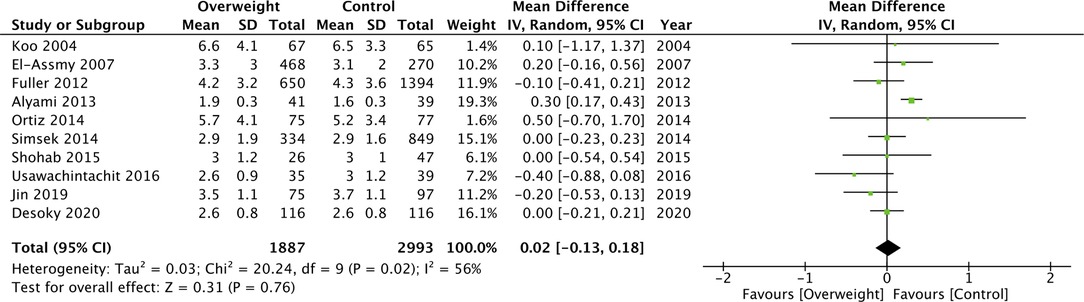
LOS
On pooled analysis, we noted no statistically significant difference in the LOS between morbidly obese and normal BML patients undergoing PCNL (MD: −0.01 95% CI, −0.14, 0.12 I2 = 0% p = 0.85) (Figure 8). However, the meta-analysis revealed that obese patients had significantly shorter LOS as compared to normal patients (MD: −0.12 95% CI, −0.20, −0.04 I2 = 0% p = 0.004) (Figure 8). Combining data from two studies comparing obese vs non-obese patients, we noted no difference in the LOS between the two groups (MD: −0.13 95% CI, −0.70, −0.44 I2 = 76% p = 0.65) (Figure 8). Similarly, we noted no difference in the LOS when analyzing data of overweight vs normal BMI patients (MD: 0.02 95% CI, −0.13, 0.18 I2 = 56% p = 0.76) (Figure 9). All results were found to be stable on sensitivity analysis.
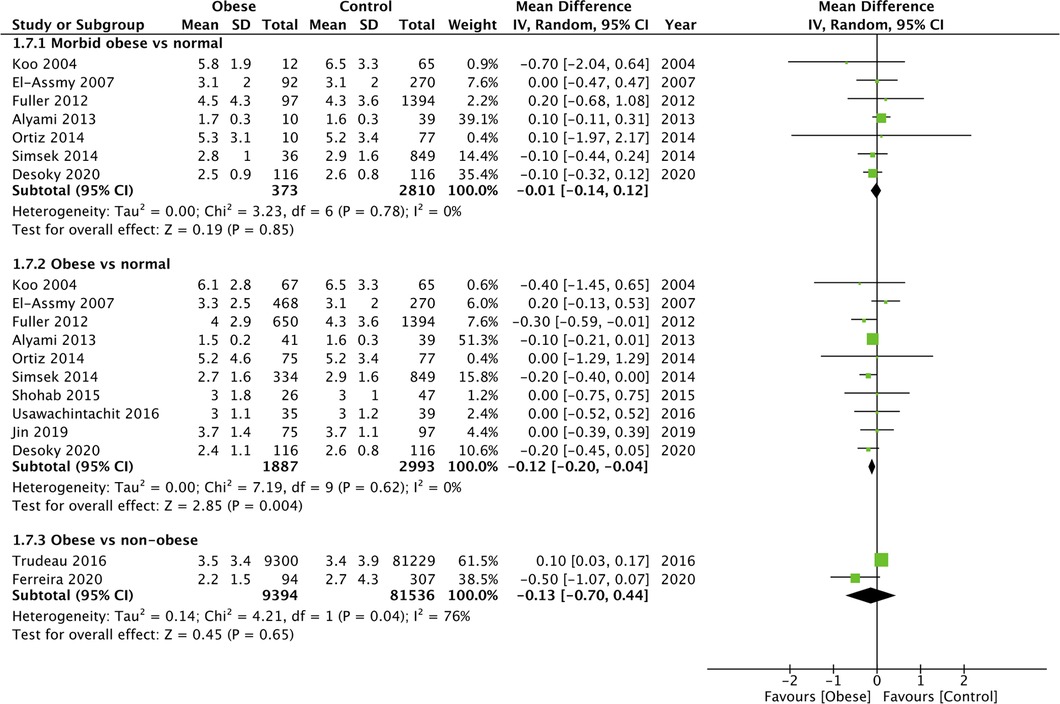
Figure 8. Meta-analysis of LOS between morbid obese vs normal, Obese vs normal and obese vs non-obese patients.
Discussion
Overweight, obese, and morbidly obese patients represent a unique cohort of individuals who are difficult to manage by both physicians and surgeons (35). Indeed, these patients have several medical comorbidities which include cardiovascular, metabolic, and respiratory illnesses which can complicate the management of any other disease (36). Surgical procedures in these patients are frequently complicated and associated with an increased risk of complications with less than satisfactory outcomes (37, 38). Furthermore, research indicates that morbid obesity is an independent risk factor for mortality after surgery (36). Since obesity has become a major global healthcare problem, it is necessary to assess the impact of this comorbidity on every surgical procedure to enable risk stratification and informed clinical decisions. In this context, the current study comprehensively assessed the impact of morbid obesity, obesity, and overweight on outcomes of PCNL.
The success of any procedure performed for renal stones is measured by the stone-free status. Amongst the included studies, there was a wide variation in the stone-free rates after PCNL amongst obese and morbidly obese patients ranging from 62% to 90%. This is partly because of the non-standard definitions used by the included studies in assessing stone-free rates. Also, the majority of the studies did not report the cut-off used to assess residual fragments. Another difference was the imaging modality used by the studies to assess residual stones. While the recent studies used computed tomography (CT), older studies used either plain radiographs, ultrasonography, CT, or intravenous urography. It is well-known that different imaging modalities have different sensitivities and specificities to detect residual stones, with CT being the most efficient tool (39). However, since both obese and non-obese patients were assessed by the same criteria and imaging modality in each study, such differences may not have affected the overall outcomes of our review. Our meta-analysis demonstrated that morbidly obese, obese, and overweight individuals do not have worse stone-free rates as compared to normal BMI patients. Additionally, using the WHO-defined cut-off of 30 kg/m2, we also compared all obese patients (including morbid obese) vs non-obese patients (overweight and normal BMI) only to find no difference in the stone-free rates between the two groups. Despite the data being derived from observational studies, the lack of heterogeneity in the meta-analysis and lack of publication bias provides credibility to the results. Furthermore, most of the outcomes were stable on sensitivity analysis, and no study had a disproportionate effect on the results.
In the analysis of stone-free rates between morbid obese vs normal BMI patients, we noted that on the exclusion of one study, the results indicated inferior outcomes in morbidly obese patients. Importantly, this outcome was largely influenced by the results of Fuller et al. (30) which carried the maximum weight in the analysis (40%). Except for this study, all others reported no difference in stone-free rates between morbidly obese and normal BMI patients. In the study of Fuller et al. (30), the authors noted a significantly high rate of staghorn stones in morbid obese vs normal patients (40.2% vs 26%) which could have led to inferior outcomes in the obese cohort. Such disparity also points out another important factor in the interpretation of our results, which is, baseline differences between obese and normal BMI patients. It has been noted that diabetes, metabolic syndrome, and hypertension which are commonly seen with obesity are predisposing factors for renal stones (40). Obesity also leads to increased excretion of lithogenic substances, including calcium, oxalate, sodium, and uric acid thereby affecting urinary composition (41). Indeed, obese patients also have a higher incidence of uric acid stones (42). Insulin resistance associated with obesity may interfere with renal ammonium production and decrease urine pH (43). Thus, several factors can predispose an obese patient to renal stones and there could have been baseline differences between obese and normal BMI patients. In this context, the lack of propensity score matching for baseline variables is an important limitation of the included studies. However, even if it is assumed that obese patients had worse stone characteristics, the lack of difference in stone-free rates is indeed encouraging and PCNL should be routinely offered to such patients.
One of the difficulties in performing PNCL in an obese patient includes difficulty in the visualization of the stone under fluoroscopic or ultrasonographic guidance. The excess abdominal fat can hinder the identification of anatomical landmarks and stone positions making the procedure difficult. Standard instruments may also not be feasible for use in obese patients. Morbid obese patients require longer sheaths which can be difficult to handle and manipulate during the procedure. Indeed, we noted longer significantly longer operating times in morbidly obese and obese patients as compared to normal BMI patients. Our analysis demonstrated that operating time was increased by around 9 min for morbidly obese patients and 2 min for obese patients. The clinical significance of such a minor difference in operating times is indeed debatable.
Patient position is another important factor of consideration for obese patients. The majority of the included studies used the standard prone position for PCNL even for obese patients. Some studies have reported that obese patients in the prone position are vulnerable to abdominal compression due to intra-operative muscle relaxation which decreases total lung capacity and functional residual capacity. Furthermore, inferior vena cava compression can reduce preload and impair oxygenation leading to cardiopulmonary complications (30, 44). However, effect of patient position on cardiopulmonary complications during PCNL is conflicting and these is no clear evidence on what constitutes the best clinical practice. Nevertheless, to overcome such problems, researchers have advocated supine or lateral decubitus positioning, use of conscious sedation, and awake endotracheal intubation with prone patient self-positioning (45). Mazzucchi et al. (46) have compared outcomes of supine and prone PCNL in obese patients only to find no difference in clinical outcomes. Abouelleil et al. (47) have noted that the distance between skin to renal collecting system is significantly increased with supine as compared to the prone position and this difference increases with the patient’s BMI. The increased distance corresponds to increased nephrostomy tract length which reduces maneuverability and increases the difficulty of the procedure. There is also a possibility of higher surgical complications like bowel injury or bleeding from trauma to the kidney because of torquing of the renal parenchyma due to the larger distance (47). Further comparative studies are needed to provide clarity on what is the best position for obese patients undergoing PCNL.
Despite the majority of studies using the prone position, our meta-analysis failed to demonstrate any increased risk of complications in the overweight, obese, or morbid obese group. Even comparing obese vs non-obese patients, there was no difference in the risk of complications. It must be noted that all different complications reported by the studies were pooled in the meta-analysis. Only a limited number of studies classified the complication rates based on the Calvien-Dindo classification system, precluding a thorough analysis. We also noted no difference in the LOS in morbidly obese and overweight patients as compared to normal BMI patients. A small reduction in the LOS was noted in obese patients as compared to normal patients but with a MD of just 0.1 days. A difference of a few hours of hospital stay may not be clinically relevant.
There are certain limitations to our review. Firstly, all data was observational and therefore is prone to bias. Secondly, we were unable to assess the impact of important variables like patient positioning, stone size, stone composition, and stone location on the outcomes due to a lack of reporting of data by the included studies. Thirdly, we could not assess the risk of specific complications in the two groups. Incidence of specific complications would have produced better evidence. Fourthly, while all studies used the WHO criteria for defining obesity, the study of Shohab et al. (20) did not define overweight as per the WHO criteria. The small variation in definition could have resulted in bias in the analysis. However, we did not find any difference in outcomes on the exclusion of this study during sensitivity analysis. Lastly, the WHO cut-off for obesity is different for Asian and Non-Asian subjects. For Asian subjects, the WHO cut-off for obesity is 27 kg/m2. Therefore, our results may not be generalized for these patients till future studies report specific data on Asian population.
Nevertheless, our review has certain strengths. As compared to the previous review (14), we were able to add 11 more studies thereby significantly increasing the statistical power of the analyses. Unlike the previous review, we also compared outcomes of overweight and normal patients and obese vs non-obese patients.
Conclusions
Our updated systematic review and meta-analysis of 18 observational studies including 101,363 participants have demonstrated that PCNL has similar efficacy and safety in morbidly obese, obese, and overweight patients as compared to normal BMI patients with no difference in the stone-free and complication rates. Evidence suggests that operating time is increased in morbidly obese and obese patients and the latter may have shorter LOS. Future studies should use propensity-score matching for baseline characteristics to increase the quality of evidence.
Data Availability Statement
Publicly available datasets were analyzed in this study. This data can be found here: The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
YX and XH conceived and designed the study. YX and XH collected the data and performed the analysis. YX was involved in the writing of the manuscript and is responsible for the integrity of the study. All authors contributed to the article and approved the submitted version.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2022.922451/full#supplementary-material.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Wang W, Fan J, Huang G, Li J, Zhu X, Tian Y, et al. Prevalence of kidney stones in mainland China: a systematic review. Sci Rep. (2017) 7:41630. doi: 10.1038/SREP41630
2. Romero V, Akpinar H, Assimos DG. Kidney stones: a global picture of prevalence, incidence, and associated risk factors. Rev Urol. (2010) 12:e86–e96. https://pubmed.ncbi.nlm.nih.gov/20811557/. Accessed 4 Dec 2021.20811557
3. Leveridge M, D’Arcy FT, O’Kane D, Ischia JJ, Webb DR, Bolton DM, et al. Renal colic: current protocols for emergency presentations. Eur J Emerg Med. (2016) 23:2–7. doi: 10.1097/MEJ.0000000000000324
4. Zisman AL. Effectiveness of treatment modalities on kidney stone recurrence. Clin J Am Soc Nephrol. (2017) 12:1699–708. doi: 10.2215/CJN.11201016
5. Jaacks LM, Vandevijvere S, Pan A, McGowan CJ, Wallace C, Imamura F, et al. The obesity transition: stages of the global epidemic. lancet Diabetes Endocrinol. (2019) 7:231–40. doi: 10.1016/S2213-8587(19)30026-9
6. Bentham J, Di Cesare M, Bilano V, Bixby H, Zhou B, Stevens GA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet (London. England). (2017) 390:2627–42. doi: 10.1016/S0140-6736(17)32129-3
7. Apovian CM. Obesity: definition, comorbidities, causes, and burden. Am J Manag Care. (2016) 22:s176–85. https://pubmed.ncbi.nlm.nih.gov/27356115/. Accessed 9 Oct 2021.27356115
8. Javanmard B, Razaghi MR, Jafari AA, Mazloomfard MM. Flexible ureterorenoscopy versus extracorporeal shock wave lithotripsy for the treatment of renal pelvis stones of 10-20 mm in obese patients. J lasers Med Sci. (2015) 6:162–6. doi: 10.15171/JLMS.2015.12
9. Delakas D, Karyotis I, Daskalopoulos G, Lianos E, Mavromanolakis E. Independent predictors of failure of shockwave lithotripsy for ureteral stones employing a second-generation lithotripter. J Endourol. (2003) 17:201–5. doi: 10.1089/089277903765444302
10. Doizi S, Letendre J, Bonneau C, Gil Diez De Medina S, Traxer O. Comparative study of the treatment of renal stones with flexible ureterorenoscopy in normal weight, obese, and morbidly obese patients. Urology. (2015) 85:38–44. doi: 10.1016/J.UROLOGY.2014.08.028
11. Sfoungaristos S, Lorber A, Gofrit ON, Yutkin V, Landau EH, Pode D, et al. Surgical experience gained during an endourology fellowship program may affect fluoroscopy time during ureterorenoscopy. Urolithiasis. (2015) 43:369–74. doi: 10.1007/S00240-015-0774-4
12. Ferakis N, Stavropoulos M. Mini percutaneous nephrolithotomy in the treatment of renal and upper ureteral stones: lessons learned from a review of the literature. Urology Annals. (2015) 7:141–8. doi: 10.4103/0974-7796.152927
13. Weiland D, Pedro RN, Anderson JK, Best SL, Lee C, Hendlin K, et al. Randomized prospective evaluation of nephrostomy tube configuration: Impact on postoperative pain. Int Braz J Urol. (2007) 33:313–22. doi: 10.1590/S1677-55382007000300003
14. Zhou X, Sun X, Chen X, Gong X, Yang Y, Chen C, et al. Effect of obesity on outcomes of percutaneous nephrolithotomy in renal stone management: a systematic review and meta-analysis. Urol Int. (2017) 98:382–90. doi: 10.1159/000455162
15. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021:88. doi: 10.1016/j.ijsu.2021.105906
16. Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 22. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 30 Oct 2020. doi: 10.1186/s40064-016-2830-0
17. Koo BC, Burtt G, Burgess NA. Percutaneous stone surgery in the obese: outcome stratified according to body mass index. BJU Int. (2004) 93:1296–9. doi: 10.1111/J.1464-410X.2004.04862.X
18. El-Assmy AM, Shokeir AA, El-Nahas AR, Shoma AM, Eraky I, El-Kenawy MR, et al. Outcome of percutaneous nephrolithotomy: effect of body mass index. Eur Urol. (2007) 52:199–205. doi: 10.1016/J.EURURO.2006.11.049
19. Akbulut F, Kucuktopcu O, Kandemir E, Ucpinar B, Ozgor F, Simsek A, et al. Efficacy and safety of mini percutaneous nephrolithotomy in obese patients. Springerplus. (2016) 5:19–1148. doi: 10.1186/S40064-016-2830-0
20. Shohab D, Ayub R, Alam MU, Butt A, Sheikh S, Assad S, et al. Effect of body mass index on operative time, hospital stay, stone clearance, postoperative complications, and postoperative analgesic requirement in patients undergoing percutaneous nephrolithotomy. Turkish J Urol. (2015) 41:177–80. doi: 10.5152/TUD.2015.61482
21. Trudeau V, Karakiewicz PI, Boehm K, Dell’Oglio P, Tian Z, Briganti A, et al. The effect of obesity on perioperative outcomes following percutaneous nephrolithotomy. J Endourol. (2016) 30:864–70. doi: 10.1089/END.2015.0789
22. Usawachintachit M, Masic S, Chang HC, Allen IE, Chi T. Ultrasound guidance to assist percutaneous nephrolithotomy reduces radiation exposure in obese patients. Urology. (2016) 98:32–8. doi: 10.1016/J.UROLOGY.2016.04.012
23. Isoglu CS, Suelozgen T, Boyacioglu H, Koc G. Effects of body mass index on the outcomes of percutaneous nephrolithotomy. Int Braz J Urol. (2017) 43:698–703. doi: 10.1590/S1677-5538.IBJU.2016.0678
24. Jin W, Song Y, Fei X. Does body mass index impact the outcomes of ultrasound-guided percutaneous nephrolithotomy? Urol Int. (2019) 103:149–55. doi: 10.1159/000501809
25. Desoky E, Abd Elwahab KM, El-Babouly IM, Seleem MM. Outcomes of flank-free modified supine percutaneous nephrolithotomy based on BMI. Urol Int. (2021) 105:77–82. doi: 10.1159/000511292
26. Ferreira TAC, Dutra MMG, Vicentini FC, Szwarc M, Mota PKV, Eisner B, et al. Impact of obesity on outcomes of supine percutaneous nephrolithotomy. J Endourol. (2020) 34:1219–22. doi: 10.1089/END.2020.0576
27. Sergeyev I, Koi PT, Jacobs SL, Godelman A, Hoenig DM. Outcome of percutaneous surgery stratified according to body mass index and kidney stone size. Surg Laparosc Endosc Percutan Tech. (2007) 17:179–83. doi: 10.1097/SLE.0B013E318051543D
28. Bagrodia A, Gupta A, Raman JD, Bensalah K, Pearle MS, Lotan Y. Impact of body mass index on cost and clinical outcomes after percutaneous nephrostolithotomy. Urology. (2008) 72:756–60. doi: 10.1016/J.UROLOGY.2008.06.054
29. Tomaszewski JJ, Smaldone MC, Schuster T, Jackman SV, Averch TD. Outcomes of percutaneous nephrolithotomy stratified by body mass index. J Endourol. (2010) 24:547–50. doi: 10.1089/END.2009.0431
30. Fuller A, Razvi H, Denstedt JD, Nott L, Pearle M, Cauda F, et al. The CROES percutaneous nephrolithotomy global study: the influence of body mass index on outcome. J Urol. (2012) 188:138–44. doi: 10.1016/J.JURO.2012.03.013
31. Alyami FA, Skinner TAA, Norman RW. Impact of body mass index on clinical outcomes associated with percutaneous nephrolithotomy. Can Urol Assoc J. (2013) 7:1–5. doi: 10.5489/CUAJ.11229
32. Kuntz NJ, Neisius A, Astroza GM, Tsivian M, Iqbal MW, Youssef R, et al. Does body mass index impact the outcomes of tubeless percutaneous nephrolithotomy? BJU Int. (2014) 114:404–11. doi: 10.1111/BJU.12538
33. Torrecilla Ortiz C, Meza Martínez AI, Vicens Morton AJ, Vila Reyes H, Colom Feixas S, Suarez Novo JF, et al. Obesity in percutaneous nephrolithotomy. Is body mass index really important? Urology. (2014) 84:538–43. doi: 10.1016/J.UROLOGY.2014.03.062
34. Şimşek A, Özgör F, Akbulut MF, Küçüktopçu O, Berberoǧlu AY, Sarilar Ö, et al. Does body mass index effect the success of percutaneous nephrolithotomy? Turkish J Urol. (2014) 40:104–9. doi: 10.5152/TUD.2014.66674
35. Neeland IJ, Poirier P, Després JP. Cardiovascular and metabolic heterogeneity of obesity: clinical challenges and implications for management. Circulation. (2018) 137:1391–406. doi: 10.1161/CIRCULATIONAHA.117.029617
36. Nasraway SA, Albert M, Donnelly AM, Ruthazer R, Shikora SA, Saltzman E. Morbid obesity is an independent determinant of death among surgical critically ill patients. Crit Care Med. (2006) 34:964–70. doi: 10.1097/01.CCM.0000205758.18891.70
37. Unruh KR, Bastawrous AL, Kaplan JA, Moonka R, Rashidi L, Simianu VV. The impact of obesity on minimally invasive colorectal surgery: a report from the Surgical Care Outcomes Assessment Program collaborative. Am J Surg. (2021) 221:1211–20. doi: 10.1016/J.AMJSURG.2021.03.019
38. Goyal A, Elminawy M, Kerezoudis P, Victor ML, Yolcu Y, Alvi MA, et al. Impact of obesity on outcomes following lumbar spine surgery: a systematic review and meta-analysis. Clin Neurol Neurosurg. (2019) 177:27–36. doi: 10.1016/J.CLINEURO.2018.12.012
39. Gokce MI, Ozden E, Suer E, Gulpinar B, Gulpinar O, Tangal S. Comparison of imaging modalities for detection of residual fragments and prediction of stone related events following percutaneous nephrolitotomy. Int Braz J Urol. (2015) 41:86–90. doi: 10.1590/S1677-5538.IBJU.2015.01.12
40. Sancak EB, Reşorlu M, Akbas A, Gulpinar MT, Arslan M, Resorlu B. Do Hypertension, diabetes mellitus and obesity increase the risk of severity of nephrolithiasis? Pakistan J Med Sci. (2015) 31:566–71. doi: 10.12669/PJMS.313.7086
41. Taylor EN, Curhan GC. Body size and 24-hour urine composition. Am J Kidney Dis. (2006) 48:905–15. doi: 10.1053/J.AJKD.2006.09.004
42. Daudon M, Lacour B, Jungers P. Influence of body size on urinary stone composition in men and women. Urol Res. (2006) 34:193–9. doi: 10.1007/S00240-006-0042-8
43. Abate N, Chandalia M, Cabo-Chan AV, Moe OW, Sakhaee K. The metabolic syndrome and uric acid nephrolithiasis: novel features of renal manifestation of insulin resistance. Kidney Int. (2004) 65:386–92. doi: 10.1111/J.1523-1755.2004.00386.X
44. Brodsky JB, Oldroyd M, Winfield HN, Kozlowski PM. Morbid obesity and the prone position: a case report. J Clin Anesth. (2001) 13:138–40. doi: 10.1016/S0952-8180(01)00230-6
45. Mourmouris P, Berdempes M, Markopoulos T, Lazarou L, Tzelves L, Skolarikos A. Patient positioning during percutaneous nephrolithotomy: what is the current best practice? Res reports Urol. (2018) 10:189–93. doi: 10.2147/RRU.S174396
46. Mazzucchi E, Vicentini FC, Marchini GS, Danilovic A, Brito AH, Srougi M. Percutaneous nephrolithotomy in obese patients: comparison between the prone and total supine position. J Endourol. (2012) 26:1437–42. doi: 10.1089/END.2012.0257
Keywords: obesity, overweight, renal stones, surgery, complications, nephrolithiasis
Citation: Xu Y and Huang X (2022) Effect of Body Mass Index on Outcomes of Percutaneous Nephrolithotomy: A Systematic Review and Meta-Analysis. Front. Surg. 9:922451. doi: 10.3389/fsurg.2022.922451
Received: 18 April 2022; Accepted: 23 May 2022;
Published: 14 June 2022.
Edited by:
Richard W. Norman, Dalhousie University, CanadaReviewed by:
Widi Atmoko, RSUPN Dr. Cipto Mangunkusumo, IndonesiaPanagiotis Kallidonis, University of Patras, Greece
Copyright © 2022 Xu and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yan Xu QTEzODY4ODA2MzU3QDE2My5jb20=
Specialty section: This article was submitted to Genitourinary Surgery, a section of the journal Frontiers in Surgery
 Yan Xu
Yan Xu Xiaolin Huang
Xiaolin Huang