- Department of Gynecology, Optics Valley Affiliated Tongren Hospital, Wuhan University, Wuhan, China
Objective: To investigate the clinical effect of Multi-focused (MF) laser in the treatment of vulvar lichen sclerosus (VLS).
Methods: In this single-center, randomized controlled trial, we compared the effect of fractionated MF laser with other treatments on patients with biopsy-proven VLS. Patients with VLS were enrolled in this study and randomly divided into three groups. Patients in the experimental group were treated with a CO2 laser, control group 1 was treated with radiofrequency, and control group 2 was treated topically with glucocorticoids and soaking with Chinese patent medicine. The pruritus degree, skin elasticity, skin color, lesion scope, and total score were compared before treatment, at one month after treatment, and three months after treatment.
Results: One month after treatment, the pruritus degree, skin elasticity, skin color, lesion scope, and total score decreased in the experimental group, and the differences were statistically significant (P < 0.05). In control group 1, the differences in pruritus degree, skin color, and total score were statistically significant (P < 0.05), but the differences in skin elasticity and lesion scope were not statistically significant (P > 0.05). In control group 2, the differences in pruritus degree and total score were statistically significant (P < 0.05), but the differences in skin elasticity, skin color, and lesion scope were not statistically significant (P > 0.05). At one month after the end of treatment, the differences in pruritus degree, skin elasticity, skin color, lesion scope, and total score among the three groups were not statistically significant. At three months after the end of treatment, the differences in the scores of the five indicators were statistically significant.
Conclusion: For the three treatment methods for VLS, topical corticosteroids + traditional Chinese medicine can quickly relieve itching symptoms in patients, but it cannot significantly improve skin elasticity, skin color, and lesion scope, and VLS easily relapses after treatment. Radiofrequency can improve itching symptoms and skin color but has poor effects on the change of skin elasticity and lesion scope. Multi-focused laser treatment can alleviate the degree of pruritus, improve skin color and elasticity, and narrow the lesion scope, and VLS will not relapse within three months after treatment.
Introduction
Vulvar lichen sclerosus (VLS) is a chronic inflammatory non-neoplastic skin lesion of the vulva in women. The disease is characterized by atrophy and thinning of the skin and mucosa around the vulva and anus, with chronic progression and repeated attacks. Untimely and standardized treatment may lead to vulvar atrophy, adhesion, scar formation, and even loss of normal anatomy and function of the vulva, and the risk of local carcinogenesis will also increase. The disease is easily diagnosed and difficult to treat. Early diagnosis and intervention can improve the long-term prognosis of patients. However, at present, the understanding of VLS in domestic academic circles (including obstetrics, gynecology, and dermatology) is not unified. Approximately 90% of patients seek medical treatment for pruritus, while nearly 10% of asymptomatic patients are missed or misdiagnosed. There are significant regional differences in treatment plans. The effects of routine local applications of glucocorticoids are not lasting, and it is easy to relapse after drug withdrawal, while long-term use of hormones has obvious adverse reactions, and the overall curative effect is limited (1). MF laser is widely used in skin medical cosmetology. It can remove wrinkles, rejuvenate skin, and remove pigmented nevi, but it is rarely used to treat VLS (2).
Subjects and methods
Subjects
Patients with VLS treated at the Guanggu Gynecology Department of Wuhan Third Hospital from November 2020 to November 2021 were enrolled and randomly divided into three groups. In the experimental group, 25 patients with VLS were treated with an MF laser, control group 1 had 13 patients with VLS treated with radiofrequency, and control group 2 had 12 patients with VLS treated with 0.05% clobetasol propionate ointment combined with traditional Chinese medicine.
The inclusion criteria were as follows: (1) Pathologically diagnosed with VLS; (2) the ages ranged between 18 and 75 years old; (3) patients signed informed consent; (4) no other treatment regimen was used to treat VLS within three months. Patients who met the exclusion criteria were excluded from the study: (1) previously treated for intraepithelial neoplasia, carcinoma, or local radiotherapy; (2) with liver or kidney dysfunction; (3) with human immunodeficiency virus or syphilis infections, acute vaginitis, or cervical malignancy; (4) with cardiovascular disease; (5) with blood system diseases; (6) with hypertension or diabetes mellitus; (7) with mental illness; (8) pregnant or lactating women.
Methods
Patients in the experimental group were treated with a CO2 laser, control group 1 was treated with radiofrequency, and control group 2 was treated with glucocorticoids and soaking with Chinese patent medicine.
The experimental group (laser treatment): The manufacturer of the laser therapeutic instrument is Wuhan Leijian Technology Co., Ltd., China, Ligenesis-MC30. Local anesthesia was given after disinfection. The patient was fixed in the lithotomy position. The energy density range was set within 40–50 mJ/pixel according to the location, color, and area of white spots. The front end of the laser hand tool was perpendicular to the white spot surface, and they were treated one by one. The number of image bundles was 81 dots according to the white spot area, peak power could be high, medium, and low, the pulse mode was set on “repeat,” the treatment time was 300–400 µs, and the distance between dots was 250–400 µm. The parameters were adjusted according to the patient's tolerance. Each area was treated with the laser 3–4 times. Local cold compresses were given within 12 h after treatment. The patient was forbidden to take a bath within 24 h or engage in vigorous exercise and hot water baths within 3–4 days, and sexual intercourse was prohibited within seven days after treatment. MF laser were performed once a month for 3 months by the same operator. Patients were administered with topical anesthetics before each MF laser treatment.
Control group 1 (radiofrequency treatment): With 5% 5-aminolevulinic acid (5-ALA) as a photosensitizer, a red light with a wavelength of 635 nm was used for radiofrequency. Each irradiation lasted for 10 min once a week for 10 weeks.
Control group 2: Clobetasol propionate ointment (0.05%) was used topically with traditional Chinese medicine soaking and washing for 3–4 months. Clobetasol propionate ointment was applied once a day for four weeks, then once every other day for four weeks, and, finally, twice a week for four weeks; the treatment course was three months. The dose referred to a fingertip unit (FTU); 1 FTU refers to the amount of medicine (about 0.5 g) extruded from the ointment tube with an opening of 5 mm that can cover the area from the fingertip of the index finger to the first interphalangeal joint. The traditional Chinese medicine consisted of Fructus cnidii and sweet wormwood. The combination of traditional Chinese medicine with Western medicine has been shown to enhance the curative effect, reduce the incidence of adverse reactions, and improve quality of life of patient with VLS (3).
Observation indexes
The scores were recorded before treatment and at one and three months after treatment.
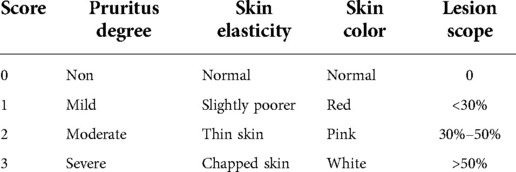
Observation indexes: (i) Clinical symptom evaluation: The curative effect indexes were evaluated according to the Cattaneo scoring system. Details are presented in Table 1.
Statistical data processing
Statistical analysis was performed using SPSS 20.0 software. Normally distributed measurement data were expressed as mean ± standard deviation (mean ± standard deviation), and non-normally distributed measurement data were expressed as median and interquartile ranges. Normally distributed data were evaluated using analysis of variance, and non-normally distributed data were evaluated using the Mann–Whitney U and Kruskal–Wallis nonparametric tests. All statistical tests were conducted using two-sided tests. P < 0.05 was considered statistically significant.
Results
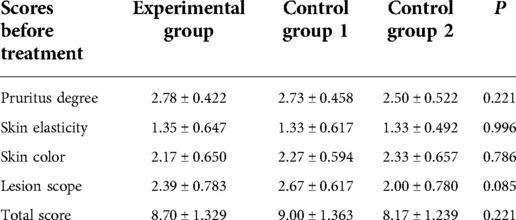
Analysis of conditions among the three groups of patients before treatment
Before treatment, there were no significant differences among the three groups in the mean values of pruritus degree, skin elasticity and color, lesion scope, and total score (Table 2). Figure 1 shows the genital area of a patient with VLS before MF laser treatment.
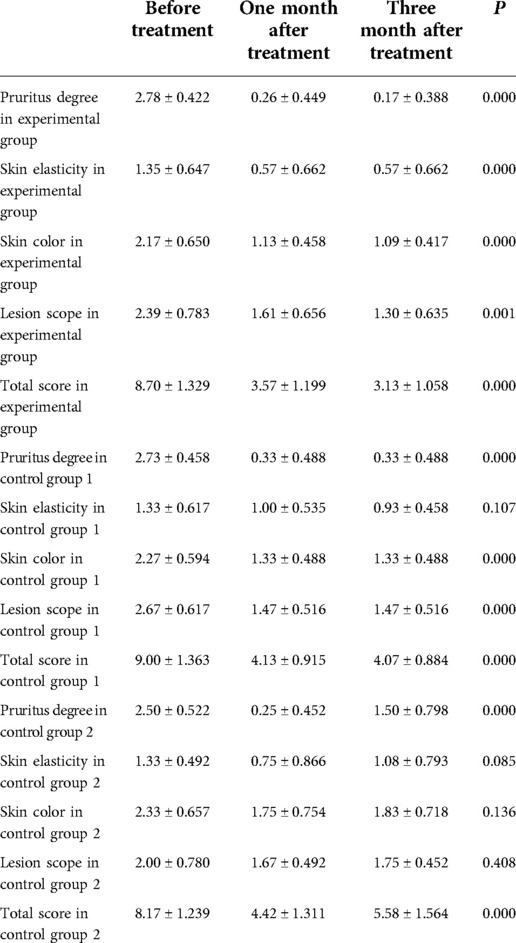
Analysis of conditions among the three groups of patients before and after treatment
The three groups of patients were self-controlled before and after treatment. In the experimental group, the degree of pruritus, skin elasticity and color, lesion scope, and total score decreased; the differences were statistically significant.
In control group 1, the degree of pruritus, skin color, and total score decreased, and the differences were all statistically significant. However, although skin elasticity and lesion scope decreased in control group 1, the differences were not statistically significant. Figure 2 shows the genital area of a patient with VLS after MF laser treatment.
In control group 2, the degree of pruritus and total score decreased, and the differences were statistically significant, but the differences in skin elasticity, color, and lesion scope were not statistically significant.
At three months after treatment, the pruritus degree was higher than one month after treatment, and the difference was statistically significant. At three months after treatment, although the pruritus score was lower than before treatment, the difference was not statistically significant (Table 3).
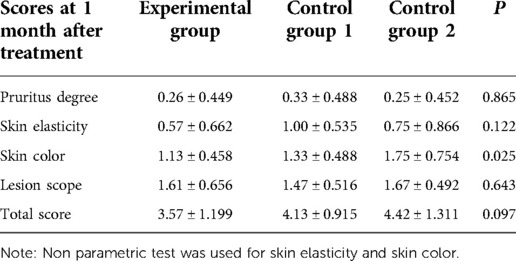
Analysis of conditions among the three groups of patients one month after the End of treatment
One month after the end of treatment, there was a significant difference in skin color among the three groups. There was no significant difference in pruritus degree, skin elasticity, lesion scope, and total scores among the three groups (Table 4).
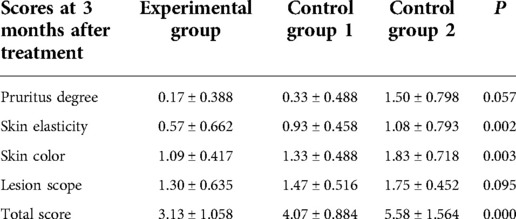
Analysis of conditions among the three groups of patients three months after the end of treatment
At three months after the end of treatment, there were significant differences in pruritus degree, skin elasticity and color, and total scores among the three groups. However, there was no significant difference in lesion scope among the three groups (Table 5).
Discussion
VLS is a chronic inflammatory skin disease. Local lymphocytic infiltration is often observed in skin biopsy pathology. About 90% of patients seek medical treatment due to symptoms. The most common symptom of VLS is intractable pruritus, usually at night. In severe cases, it can affect daily life and sleep. Other accompanying symptoms may include vulvar pain, dysuria, urinary pain, sexual dysfunction, and pain during sexual intercourse and defecation. Nearly 10% of VLS patients are completely asymptomatic and are usually found by chance or by doctors during a gynecological examination. The classic VLS skin texture changes are wrinkled or cellophane-like white patches, which can also be accompanied by irregular hyperkeratosis. The skin lesions mainly involve the labia majora and minora, prepuce of the clitoris, perineal body, and perianal skin, and are mostly symmetrically distributed. The hair growth area of the labia majora is usually not affected. The skin in the vulvar lesion area is fragile and primarily manifests as purpura, erosion, and chapping. If the lesion is not treated properly for a long time, it can cause the invagination of the vulva structure, the loss of the labia minora and the prepuce of the clitoris, or anterior-posterior combined adhesions, and finally, lead to the stenosis of the vaginal orifice and/or anus. Except for the natural remission of some VLS before puberty, most patients with VLS need active intervention and treatment. Furthermore, it is emphasized that even asymptomatic patients should be treated to delay the progression of the disease and improve the long-term prognosis. Currently in China, the local and external use of glucocorticoids is recommended as the first-line treatment of VLS (4–5). Physical therapy or surgical treatment can be chosen for patients with ineffective drug treatment or severe local adhesions. The purpose is to alleviate the itching symptoms, delay lesion progression, prevent complications, and improve the quality of life (6).
Literature reported that the incidence rates of VLS vary widely, from 1/70 to 1/1,000 (7). Since some patients are asymptomatic and do not see doctors in time, the actual incidence rates of VLS may be far underestimated. It is generally considered that there are two peaks in the age of onset of VLS. It usually occurs in postmenopausal women (average age 52.6 years old) and is not uncommon in preadolescent girls (average age 7.6 years old) (8, 9).
At present, the principle of MF lasers in the treatment of VLS is still unclear. The absorption of light energy by water molecules in the dermis achieves the ablation of the dermis and epidermis to reduce the occurrence of hyperkeratosis and lichen-like lesions to treat the disease (10). Therefore, MF laser treatment of VLS can not only improve the symptoms of vulvar pruritus but also improve the skin elasticity and color of lesions and reduce the lesion scope of patients. However, there are few reports on MF laser treatment of VLS. Pagano et al. (11) reported that an MF laser was used to remedy refractory VLS, but this literature failed to set up an effective control and lacked follow-up. No severe complications occurred during or after the treatment. Only a few patients reported red and swollen skin, and burn ointment gave immediate relief. These findings were consistent with the study by Di Donato et al. (12).
Radiofrequency is a type of high-frequency electromagnetic wave that has been widely used to treat tumors in the brain, liver, breast, thyroid, and other tissues in clinical practice. In recent years, its use in the of uterine leiomyomas of less than 5 cm has received satisfactory results (13). Electromagnetic waves act on the dermis and exert a thermal effect, resulting in vasodilation, accelerating blood flow, and increasing the permeability of the vascular endothelial cell membrane, improving the nutritional status of microvessels and nerve endings in the dermis so that the nerve terminals are no longer abnormally excited, and pruritus symptoms do not appear in the vulva. It also improves skin color and elasticity to a certain extent and reduces the lesion scope (14). Yang et al. reported on the therapeutic effect of radiofrequency in patients with VLS (15).
Topical glucocorticoids are currently the first-line treatment for VLS in China. Their local external application can effectively resist inflammation and allergies, promote capillary contraction, regulate immunity, inhibit mitosis, and improve vulvar symptoms with an acceptable short-term curative effect (16). However, its disadvantages are also obvious. The curative effect of this treatment is poor, and there is no significant improvement in skin elasticity, color, and lesion scope. It is easy to relapse after stopping treatment, long-term use brings noticeable adverse reactions to the skin, and the overall curative effect is general.
It is well-known that VLS is a disease that recurs easily. Patients with VLS should be given proper medical follow-up. In our study, the recurrence rate of patients treated with MF laser was lower than those treated with other three treatments. However, it should be noted that the period of this study was short, which is a limitation of the present study. In addition, only a small group of patients were recruited in the three groups. Future investigations with a larger sample size and a multi-center design are needed to validate the current findings.
Conclusion
For these three treatment methods for VLS, topical corticosteroids + traditional Chinese medicine can quickly relieve itching symptoms in patients, but it cannot significantly improve skin elasticity, color, and lesion scope, and VLS easily relapses after treatment. Radiofrequency can improve itching symptoms and skin color but has poor effects on the change of skin elasticity and lesion scope. Multi-focused laser treatment can alleviate the degree of pruritus, improve skin color and elasticity, and narrow the lesion scope, and VLS will not relapse within three months after treatment.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of Optics Valley Affiliated Tongren Hospital (KY2021-016). The patients/participants provided their written informed consent to participate in this study.
Author contributions
Conception and design of the research: ZZY, GJQ, CSY; Acquisition of data: CSY, LJQ; Analysis and interpretation of the data: GJQ, HLN; Statistical analysis: GJQ, SY, LJQ, LHY, HLN; Obtaining financing: ZZY; Writing of the manuscript: GJQ; Critical revision of the manuscript for intellectual content: ZZY, CXM. All authors contributed to the article and approved the submitted version.
Funding
The research projects of Multi-focused laser treatment on gynecology and Pelvic floor dysfunction.
Acknowledgments
We would like to acknowledge the hard and dedicated work of all the staff that implemented the intervention and evaluation components of the study. And acknowledge their contributions of Wen-Xing Song, Huan-Ling Jiang, Huan Huang, Jing Li, Yuan-Ping Xu, Hong-Li Huang,Yu-Ping Lian, Hai-Lan Wang, et al.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Yang M, Chang J. Etiology and clinical manifestations of sclerosing lichen of vulva. Chin J Dermatol. (2015) 48(2):139–41. doi: 10.3760/cma.j.issn.0412-4030.2015.02.022
2. Li J, Yang Y, Xie Y, Wang J. The case study of fractional carbon dioxide laser and triamcinolone acetonide of the patients with vulvar lichen sclerosus. Chin J Clin Obstet Gynecol. (2018) 19(2):107–10. doi: 10.3760/cma.j.issn.0412-4030.2015.02.022
3. Kang W. Clinical observation on vulvar lichen sclerosus treated with red light combined with traditional Chinese and western medicine. Chin J Modern Drug Appl. (2014) 8(17):2. CNKI:SUN:ZWYY.0.2014-17-081
4. Singh N, Ghatage P. Etiology, clinical features, and diagnosis of vulvar lichen sclerosus: a scoping review. Obstet Gynecol Int. (2020) 2020:7480754. doi: 10.19538/j.fk2021010118
5. Marfatia Y, Surani A, Baxi R. Genital lichen sclerosus et atrophicus in females: an update. Indian J Sex Transm Dis AIDS. (2019) 40(1):6–12. doi: 10.4103/ijstd.IJSTD_23_19
6. Van Der Meijden WI, Boffa MJ, Ter Harmsel WA, Kirtschig G, Lewis FM, Moyal-Barracco M, et al. 2016 European guideline for the management of vulval conditions. J Eur Acad Dermatol Venereol. (2017) 31(6):925–41. doi: 10.1111/jdv.14096
7. Fruchter R, Melnick L, Pomeranz MK. Lichenoid vulvar disease: a review. Int J Womens Dermatol. (2017) 3(1):58–64. doi: 10.1016/j.ijwd.2017.02.017
8. Eva LJ. Screening and follow- up of vulval skin disorders. Best Pract Res Clin Obstet Gynaecol. (2012) 26(2):175–88. doi: 10.1016/j.bpobgyn.2011.11.005
9. Singh N, Ghatage P. Etiology, clinical features, and diagnosis of vulvar lichen sclerosus: a scoping Review. Obstet Gynecol Int. (2020) 2020:7480754. doi: 10.1155/2020/7480754
10. Lee A, Lim A, Fischer G. Fractional carbon dioxide laser in recalcitrant vulval lichen sclerosus. Aust J Dermatol. (2016) 57(1):39–43. doi: 10.1111/ajd.12305
11. Pagano T, Conforti A, Buonfantino C, Schettini F, Vallone R, Gallo A, et al. Effect of rescue fractional microablative CO2 laser on symptoms and sexual dysfunction in women affected by vulvar lichen sclerosus resistant to long-term use of topic corticosteroid: a prospective longitudinal study. Menopause. (2020) 27(4):418–22. doi: 10.1097/GME.0000000000001482
12. Di Donato V, D'Oria O, Scudo M, Prata G, Fischetti M, Lecce F, et al. Safety evaluation of fractional CO2 laser treatment in post-menopausal women with vaginal atrophy: a prospective observational study. Maturitas. (2020) 135:34–9. doi: 10.1016/j.maturitas.2020.02.009
13. Kamilos MF, Aguiar LM, Batista VH, Roa CL, Aguiar FN, Soares Júnior JM, et al. Microablative fractional radiofrequency as a therapeutic option for vulvar lichen sclerosus: a pilot study. Clinics (Sao Paulo). (2021) 76:e2567. doi: 10.6061/clinics/2021/e2567
14. Osiecka BJ, Jurczyszyn K, Nockowski P, Murawski M, Ziółkowski P. Photodynamic therapy with green light for the treatment of vulvar lichen sclerosus - preliminary results. Photodiagnosis Photodyn Ther. (2017) 17:185–7. doi: 10.1016/j.pdpdt.2016.11.015
15. Yang H, Tan Z, Zhou X, Yu X, Wan L. Clinical analysis of 70 cases of vulvar leukoplakia treated by radiofrequency. Hainan Med J. (2019) 21:2814–6. CNKI:SUN:HAIN.0.2019-21-028
Keywords: vulvar lichen sclerosus, MF laser, radiofrequency, traditional Chinese medicine, clinical study
Citation: Guo J, Chen S, Chen X, Lu J, Song Y, Liu H, Hu L and Zhu Z (2022) Clinical study on multi-focused laser in the treatment of vulvar lichen sclerosus. Front. Surg. 9:919135. doi: 10.3389/fsurg.2022.919135
Received: 18 May 2022; Accepted: 19 August 2022;
Published: 15 September 2022.
Edited by:
Andrea Rosati, Agostino Gemelli University Polyclinic (IRCCS), ItalyReviewed by:
Alessandra Gallo, Federico II University Hospital, ItalyEdmund Baracat, University of São Paulo, Brazil
© 2022 Guo, Chen, Chen, Lu, Song, Liu, Hu and Zhu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zheng-Yan Zhu emh1emhlbmd5YW56enk2QDEyNi5jb20=
†These authors have contributed equally to this work.
Specialty Section: This article was submitted to Obstetrics and Gynecological Surgery, a section of the journal Frontiers in Surgery
 Jing-Qiu Guo†
Jing-Qiu Guo† Zheng-Yan Zhu
Zheng-Yan Zhu