
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CASE REPORT article
Front. Surg., 24 October 2022
Sec. Orthopedic Surgery
Volume 9 - 2022 | https://doi.org/10.3389/fsurg.2022.917027
This article is part of the Research TopicHip Arthroscopy: Pathologies, surgical techniques and complicationsView all 10 articles
Tendon calcification is a common disease, with the shoulder rotator cuff being the most common site. However, calcific tendinitis of the gluteus medius has rarely been reported. This study reports the case of a 64-year-old woman diagnosed with calcific tendinitis of the gluteus medius and experiencing right lateral hip pain with no apparent trigger. After unsuccessful conservative treatment, hip endoscopy was performed on this patient, allowing for a clear view of a “toothpaste-like” lesion in the gluteus medius tendon. A shaver was used to remove the lesion. After 8 weeks and 14 months of follow-up, the patient could return to regular daily and social activities. This study shows that endoscopic surgery can lead to effective, rapid recovery and minimally invasive clinical outcomes in patients with tendon calcification near the hip joint.
Calcific tendinitis is the deposition of calcium hydroxyapatite crystals in periarticular muscular attachments (1). The etiology of calcific tendinitis is unclear, and the suggested causes include hereditary, metabolic, post-traumatic, and postoperative conditions (2).
Several tendons can become calcified, including those in the shoulder rotator cuffs, near the hip joints, and in hands and wrists (1, 2). However, calcific tendinitis of the gluteus medius, first described by Goldenberg and Leventhal in 1936 (3), is relatively uncommon and sporadically reported (4–8).
Generally, conservative methods for calcific tendinitis are satisfactory, including physiotherapy, non-steroidal anti-inflammatory drugs, local glucocorticoid injection, extracorporeal shock wave therapy, and small needle scalpel therapy (7). However, surgical treatment is usually performed in refractory cases.
Hip endoscopy is minimally invasive and entirely extra-articular, which can help avoid incising the hip capsule fibers, which causes hip joint instability. However, this procedure has been reported only in a few calcific tendinitis cases (2, 6, 9–11). Herein, we report the case of a patient with rare calcific tendinitis of the gluteus medius.
The case of a 64-year-old woman with a history of diabetes mellitus and hypertension is reported here. The patient presented with a 2-year history of right lateral hip pain with no apparent trigger. The pain was aggravated after 10 min of walking and relieved after a break. The pain was predominantly located in the greater trochanter and did not radiate to the lower back or lower extremities. The patient did not experience fever, chills, or limb weakness. However, hip pain was increasingly severe over the past year, hindering hip motion and interfering with sleep. The patient unsuccessfully attempted conservative treatment with oral non-steroidal anti-inflammatory drugs (NSAIDs) and traditional Chinese medicine.
The physical examination revealed an antalgic gait. The Trendelenburg and FABER (flexion abduction external rotation) tests were positive. Moderate tenderness upon palpation of the greater trochanter was experienced. The range of motion was limited compared with the left side. The range of flexion was 90°, extension was 10°, abduction was 25°, and adduction was 20°. The legs were lengthened equally, and neurological examination showed no abnormalities. The initial Harris hip score was 57.45, and the visual analog scale (VAS) score for hip pain in the resting state was 4.
Plain radiography showed a 1.0 × 2.0 cm diameter calcific deposit superomedial to the greater trochanter; this corresponded to the tendinous insertion of the gluteus medius (Figure 1A). Magnetic resonance imaging (MRI) showed evidence of calcific tendinitis (Figure 1B–D); calcific deposits were hypointense on T1- and T2-weighted images. The sedimentation rate and white blood cell count were within normal ranges.
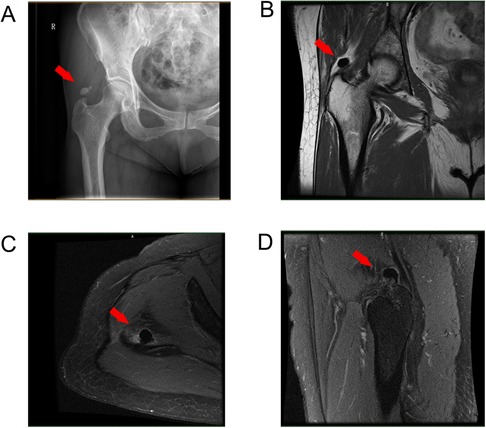
Figure 1. (A) Preoperative plain radiograph, (B) T2 coronal, (C) T1 horizontal, and (D) T1 coronal. View of MRI showing the calcification around the tip of the right greater trochanter (marked with arrows).
As conservative treatment was unsuccessful, hip endoscopy was performed (6, 9, 12). The patient was placed supine on a traction table. A sufficient amount of traction was applied to the operative hip to provide a 10–12 mm distraction of the hip joint. Standard anterolateral, mid-anterior, and distal anterolateral portals were used. An anterolateral approach (ALA) was first performed under fluoroscopic control, which was approximately 1 cm superior and anterior to the anterior edge of the greater trochanter. Next, an anteromedial approach (AMA) was established under endoscopy surveillance (Figure 2A). A 30° hip scope was inserted to visualize the gluteus medius tendon and the tip of the greater trochanter (Figure 2B).

Figure 2. (A) The patient was placed supine on a traction table; an anterolateral approach (ALA) was approximately 1 cm superior and anterior to the anterior edge of the greater trochanter; an anteromedial approach (AMA) was performed at the junction of a sagittal line drawn from the anterior superior iliac spine and a horizontal line drawn from ALA (B) surgical instruments used in hip endoscopic surgery.
Endoscopic imaging confirmed the radio-opacity on plain radiography. A soft white toothpaste-like material was observed when the degenerated gluteus medius tendon was debrided (Figure 3A,B). A motorized shaver was used to remove the material and debride the degenerated tendons. Postoperative radiography revealed that no calcification remained (Figure 3C). The specimen was sent for pathologic examination, which confirmed that the calcified tendon consisted of hydroxyapatite crystals and proliferative tendon fibrous tissue (Figure 3D).
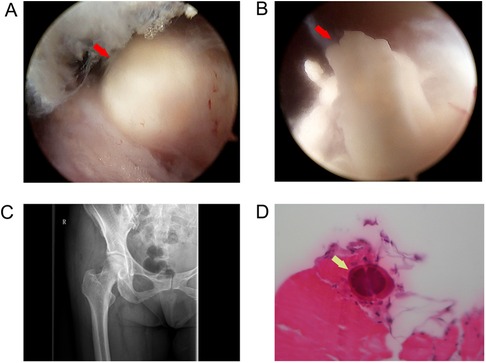
Figure 3. (A) Endoscopic view of a calcified deposit, (B) Endoscopic view showing a soft white toothpaste-like material in the deposit, (C) postoperative plain radiograph view showing complete removal of the calcific deposit, and (D) hydroxyapatite crystals in the specimen confirmed by a pathologic examination (marked with arrows).
The patient was mobilized and allowed to bear weight as tolerated. In addition, straight-leg raise exercises were started on postoperative day one and resisted knee extension strengthening exercises continued for 6 weeks. The Trendelenburg test and Patrick sign were negative at 8 weeks, and no restrictions were imposed on activities due to symptoms. The last recorded Harris hip score was 92.45, and the VAS score was 1 at 14 months after surgery.
In the present case, the patient was diagnosed with calcific tendinitis of the gluteus medius. Deposing focal apatite crystals in the tendon can result in acute or chronic hip pain during daily activities; joint movements may aggravate these symptoms (13). The presenting symptoms, in this case, were chronic pain in the posterolateral region of the right hip and right hip movement limitations.
The most common site of calcific tendinitis is the shoulder, occurring in approximately 3% of adults (1); other sites include the joint tendons such as wrists (14) or knees (15–17). In addition, calcific tendinitis has been reported in tendons near the hip joint, such as the gluteus minimus (6), gluteus medius (18), gluteus maximus (12, 19), gemellus superior, gemellus inferior (2), and rectus femoris (9).
The gluteus medius is located on the lateral side of the iliac wing; it is the main abductor muscle in the hip joint. It plays an important role in both standing and walking. Degeneration and strain of the tendon, in this case, are possible causes of the patient’s calcific tendinitis.
The calcium around the greater trochanter can cause mild to severe pain according to different calcific stages as described in the Uhthoff HK (20). Stage 1: Precalcific phase, fibrocartilaginous transformation within tendon fibers, which is asymptomatic. Stage 2: Formative phase, calcifications formed, usually causing subacute mild pain. Stage 3: Resorptive phase, the tendon develops increased vasculature and calcium deposits are removed by phagocytes; severe acute pain that can be highly disabling and unresponsive to common analgesics is experienced. Stage 4: Postcalcific phase, self-healing, and repair of the tendon fibers over several months, associated with pain and restricted function. Thus, different degrees of pain exist in stages 2–4, which explains why, in some cases, calcium around the greater trochanter can be found incidentally but is not clinically symptomatic.
The treatment for calcific tendinitis of the gluteus medius is summarized in Table 1. Surgical treatment can be adopted in patients with failed conservative treatments or severe symptoms. However, the use of endoscopy to treat the disease is not widespread, as tendon calcification of the hip joint is rare and sporadic, and endoscopic treatment has been reported only in a few cases (2, 6, 9–11). Comba et al. (10). described the surgical technique of endoscopic surgical removal in patients with calcific tendinitis of the rectus femoris. Kandemir et al. (6). and Su et al. (12). described the endoscopic treatment of the gluteus medius and maximus calcified tendinitis and considered it an effective treatment.
In our case, endoscopic surgery was used to treat the patient, which led to effective, rapid recovery and a minimally invasive clinical outcome. Therefore, given the patient's outcome to date, endoscopic treatment of calcific tendinitis of the gluteus medius may be an appropriate treatment option.
Clinically, tendon calcification of the hip joint usually presents pain and tenderness around the hip with movement limitations. These atypical symptoms make it possible to misdiagnose the disease as osteochondroma, gout, ossifying myositis, heterotopic calcification, or lumbar spinal disease.
A thorough medical history and physical examination are essential for diagnosis. For example, patients with heterotopic calcification and myositis ossificans often have a history of trauma (11), while those with gout often have a high uric acid level. Imaging techniques, such as ultrasound, computed tomography (CT) (19, 22), or MRI (5), should be used in cases of diagnostic uncertainty. CT may help evaluate osseous involvement, while MRI can demonstrate tissue edema and rule out bone tumors. In addition, the typical presenting symptoms of lateral hip pain may occasionally mimic lumbar radiculopathy and vice versa. Therefore, obtaining a lumbar MRI may be warranted in select patients (2, 7).
We report a well-documented case of rare calcific tendinitis of the gluteus medius. Endoscopic surgery is considered a feasible and effective option for patients with hip calcific tendinitis who do not respond to conservative treatment, with few risks, rapid recovery, and satisfactory outcomes. However, a longer follow-up time and a large patient sample size are needed to draw reliable conclusions.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
The studies involving human participants were reviewed and approved by Sir Run Shaw Hospital. The patients/participants provided their written informed consent to participate in this study.
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
CJ and WD wrote the draft and revised it. WG collected the data. All authors contributed to the article and approved the submitted version. All authors read and approved the submitted version.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Holt PD, Keats TE. Calcific tendinitis: a review of the usual and unusual. Skeletal Radiol. (1993) 22(1):1–9. doi: 10.1007/BF00191518
2. Yang WB, Xu QK, Liu XH, Bakhshi P, Wang H, Shao ZW, et al. Arthroscopic treatment of calcific tendinitis of gemellus superior and gemellus inferior: a case report and literature review. Orthop Surg. (2022) 14(3):621–7. doi: 10.1111/os.13186
3. Goldenberg RR, Leventhal GS. Supratrochanteric calcification. Journal of Bone and Joint Surgery. (1936) 18:205–11.
4. Yang I, Hayes CW, Biermann JS. Calcific tendinitis of the gluteus medius tendon with bone marrow edema mimicking metastatic disease. Skeletal Radiol. (2002) 31(6):359–61. doi: 10.1007/s00256-002-0516-x
5. Sakai T, Shimaoka Y, Sugimoto M, Koizumi T. Acute calcific tendinitis of the gluteus medius: a case report with serial magnetic resonance imaging findings. J Orthop Sci. (2004) 9(4):404–7. doi: 10.1007/s00776-004-0799-y
6. Kandemir U, Bharam S, Philippon MJ, Fu FH. Endoscopic treatment of calcific tendinitis of gluteus medius and minimus. Arthroscopy. (2003) 19(1):E4. doi: 10.1053/jars.2003.50021
7. Jo H, Kim G, Baek S, Park HW. Calcific tendinopathy of the gluteus medius mimicking lumbar radicular pain successfully treated with barbotage: a case report. Ann Rehabil Med. (2016) 40(2):368–72. doi: 10.5535/arm.2016.40.2.368
8. Almedghio S, Garneti N. The acute and chronic presentation of gluteus medius calcific tendinitis: a case report of two. J Orthop Case Rep. (2014) 4(4):48–50. doi: 10.13107/jocr.2250-0685.225
9. Peng X, Feng Y, Chen G, Yang L. Arthroscopic treatment of chronically painful calcific tendinitis of the rectus femoris. Eur J Med Res. (2013) 18(1):49. doi: 10.1186/2047-783X-18-49
10. Comba F, Piuzzi NS, Zanotti G, Buttaro M, Piccaluga F. Endoscopic surgical removal of calcific tendinitis of the rectus femoris: surgical technique. Arthrosc Tech. (2015) 4(4):e365–369. doi: 10.1016/j.eats.2015.03.022
11. Zini R, Panascì M, Papalia R, Franceschi F, Vasta S, Denaro V. Rectus femoris tendon calcification: arthroscopic excision in 6 top amateur athletes. Orthop J Sports Med. (2014) 2(12):2325967114561585. doi: 10.1177/2325967114561585
12. Su CA, Ina JG, Raji Y, Strony J, Philippon MJ, Salata MJ. Endoscopic treatment of calcific tendinitis of the gluteus maximus: a case report. JBJS Case Connect. (2021) 11:e20.00974-6. doi: 10.2106/JBJS.CC.20.00974
13. Jr MD, Gatter RA. Recurrent acute inflammation associated with focal apatite crystal deposition. Arthritis Rheum. (1966) 9(6):804–19. doi: 10.1002/art.1780090608
14. Torbati SS, Bral D, Geiderman JM. Acute calcific tendinitis of the wrist. J Emerg Med. (2013) 44(2):352–4. doi: 10.1016/j.jemermed.2012.08.028
15. Tennent TD, Goradia VK. Arthroscopic management of calcific tendinitis of the popliteus tendon. Arthroscopy. (2003) 19(4):E35. doi: 10.1053/jars.2003.50124
16. Song K, Dong J, Zhang Y, Chen B, Wang F, Zhao J, et al. Arthroscopic management of calcific tendonitis of the medial collateral ligament. Knee. (2013) 20(1):63–5. doi: 10.1016/j.knee.2012.05.004
17. Tsujii A, Tanaka Y, Yonetani Y, Iuchi R, Shiozaki Y, Horibe S. Symptomatic calcification of the anterior cruciate ligament: a case report. Knee. (2012) 19(3):223–5. doi: 10.1016/j.knee.2011.05.008
18. Lin W, Liu CY, Tang CL, Hsu CH. Acupuncture and small needle scalpel therapy in the treatment of calcifying tendonitis of the gluteus medius: a case report. Acupunct Med. (2012) 30(2):142–3. doi: 10.1136/acupmed-2012-010149
19. Mizutani H, Ohba S, Mizutani M, Otake S, Otsuka T, Nakamura T. Calcific tendinitis of the gluteus maximus tendon with cortical bone erosion: CT findings. J Comput Assist Tomogr. (1994) 18(2):310–2. doi: 10.1097/00004728-199403000-00030
20. Uhthoff HK, Sarkar K. Calcifying tendinitis. Baillieres Clin Rheumatol. (1989) 3:567–81. doi: 10.1016/s0950-3579(89)8000m9-3
21. Vereecke E, Mermuys K, Casselman J. A case of bilateral acute calcific tendinitis of the gluteus medius. Treated by ultrasound-guided needle lavage and corticosteroid injection. J Belg Soc Radiol. (2015) 99(2):16–9. doi: 10.5334/jbr-btr.810
Keywords: calcific tendinitis, gluteus medius, hip pain, minimally invasive (MI), endoscopic treatment
Citation: Jian C, Dan W and Gangliang W (2022) Endoscopic treatment for calcific tendinitis of the gluteus medius: A case report and review. Front. Surg. 9:917027. doi: 10.3389/fsurg.2022.917027
Received: 10 April 2022; Accepted: 27 September 2022;
Published: 24 October 2022.
Edited by:
Carlos Suarez-Ahedo, Hospital Médica Sur, MexicoReviewed by:
Shane J. Nho, Rush University, United States© 2022 Jian, Dan and Gangliang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wang Gangliang d2dsaWFuZ0B6anUuZWR1LmNu
Specialty Section: This article was submitted to Orthopedic Surgery, a section of the journal Frontiers in Surgery
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.